What Motivates Chinese Young Adults to Use mHealth?
Abstract
1. Introduction
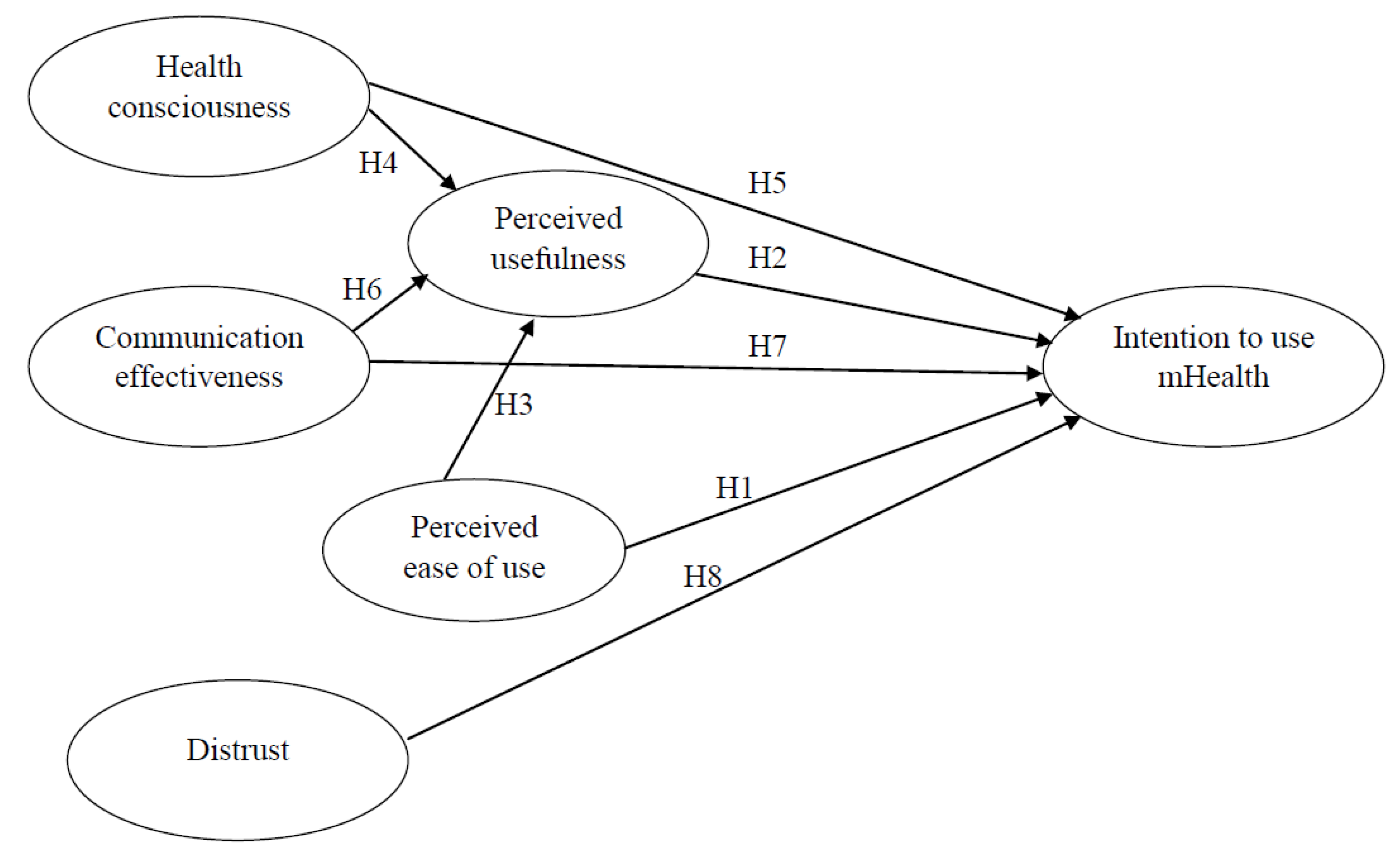
2. Literature Review and Hypothesis Development
3. Materials and Methods
3.1. Study Design and Sample
3.2. Instrument
4. Results
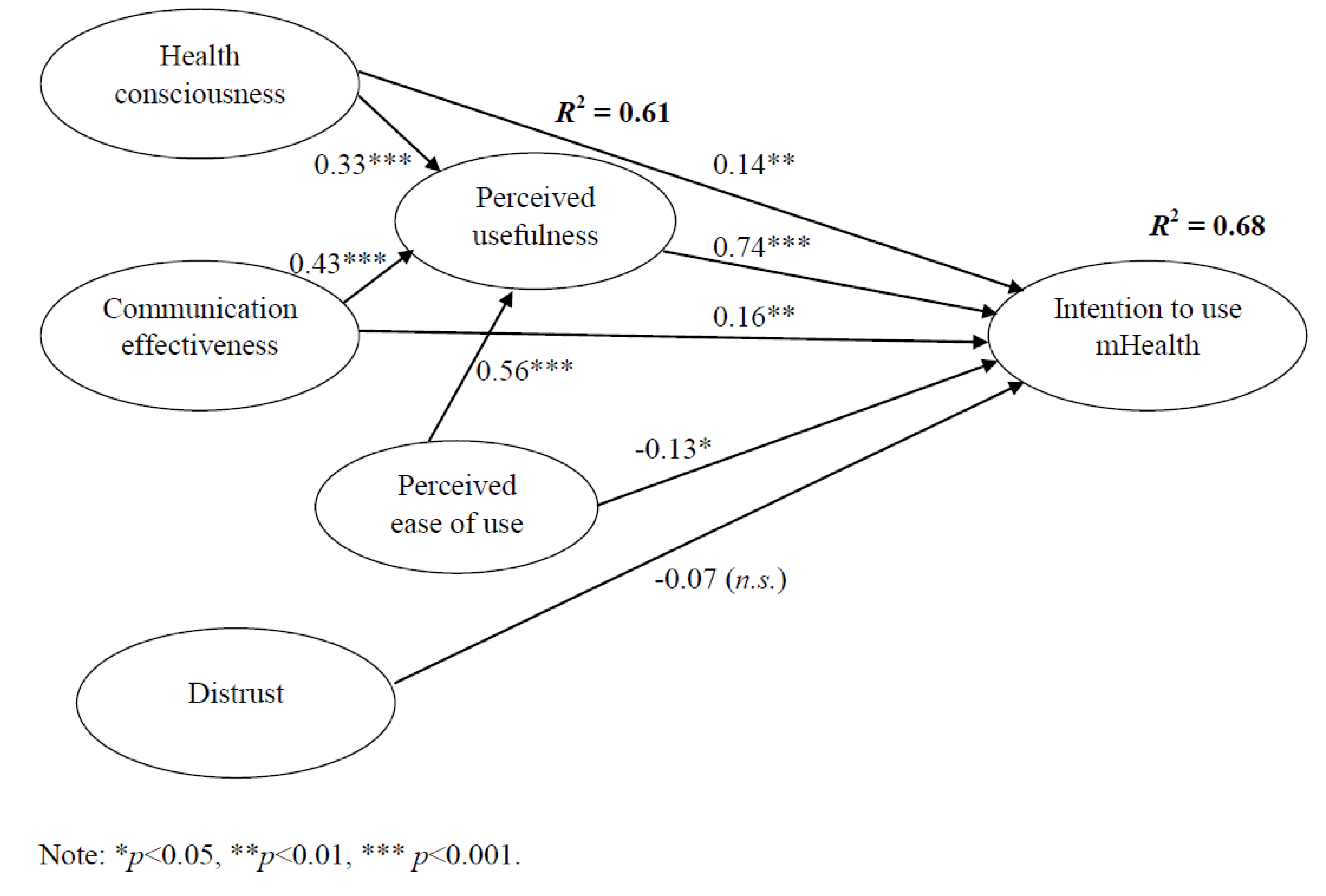
4.1. Confirmatory Factor Analysis and Structural Equation Modeling
4.2. Key Themes from Open-Ended Questions
5. Discussion
5.1. Limitations and Future Research
5.2. Practical Implications
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- The World Health Organization. mHealth: Use of Mobile Wireless Technologies for Public Health; WHO Executive Board Report EB139/8; The World Health Organization: Geneva, Switzerland, 2016; Available online: http://202.171.253.70/apps.who.int/gb/ebwha/pdf_files/EB139/B139_8-en.pdf (accessed on 1 October 2019).
- Sá, J.H.; Rebelo, M.S.; Brentani, A.; Grisi, S.J.; Iwaya, L.H.; Simplício, M.A., Jr.; Carvalho, T.C.M.B.; Gutierrez, M.A. Georeferenced and secure mobile health system for large scale data collection in primary care. Int. J. Med. Inform. 2016, 94, 91–99. [Google Scholar] [CrossRef] [PubMed]
- Sherry, J.M.; Ratzan, S.C. Measurement and evaluation outcomes for mHealth communication: Don’t we have an app for that? J. Health Commun. 2012, 17 (Suppl. 1), 1–3. [Google Scholar] [CrossRef]
- Friederici, N.; Hullin, C.; Yamamichi, M. mHealth. In Information and Communications for Development 2012: Maximizing Mobile; The World Bank: Washington, DC, USA, 2012; Chapter 3; pp. 45–59. [Google Scholar]
- Chan, S.R.; Torous, J.; Hinton, L.; Yellowlees, P. Mobile tele-mental health: Increasing applications and a move to hybrid models of care. Healthcare 2014, 2, 220–233. [Google Scholar] [CrossRef] [PubMed]
- Krupinski, E.; Weinstein, R. Telemedicine, telehealth and m-health: New frontiers in medical practice. Healthcare 2014, 2, 250–252. [Google Scholar] [CrossRef] [PubMed]
- Corpman, D.W. Mobile health in China: A review of research and programs in medical care, health education, and public health. J. Health Commun. 2013, 18, 1345–1367. [Google Scholar] [CrossRef] [PubMed]
- Ni, Z.; Liu, C.; Wu, B.; Yang, Q.; Douglas, C.; Shaw, R.J. An mHealth intervention to improve medication adherence among patients with coronary heart disease in China: Development of an intervention. Int. J. Nurs. Sci. 2018, 5, 322–330. [Google Scholar] [CrossRef]
- Lai, L.S.L.; To, W.M. Internet diffusion in China: Economic and social implications. IT Prof. 2012, 14, 16–21. [Google Scholar] [CrossRef]
- China Internet Network Information Center. The 43rd China Statistical Report on Internet Development; China Internet Network Information Center (CNNIC): Beijing, China, 2019; Available online: http://www.cnnic.cn/hlwfzyj/hlwxzbg/hlwtjbg/201902/P020190318523029756345.pdf (accessed on 1 October 2019). (In Chinese)
- Big Data Research. 2019Q1 Mobile Medical Report; Big Data Research: Beijing, China, 2019; Available online: http://www.bigdata-research.cn/content/201905/964.html (accessed on 1 October 2019).
- Ping An Healthcare and Technology Company Limited. Company Overview; Ping An Healthcare and Technology Company Limited (PAHTG): Shanghai, China, 2019; Available online: http://www.pahtg.com/en/about-us/company-overview/ (accessed on 1 October 2019).
- Hsu, J.; Liu, D.; Yu, Y.M.; Zhao, H.T.; Chen, Z.R.; Li, J.; Chen, W. The top Chinese mobile health apps: A systematic investigation. J. Med. Internet Res. 2016, 18, e222. [Google Scholar] [CrossRef]
- Gagnon, M.P.; Ngangue, P.; Payne-Gagnon, J.; Desmartis, M. m-Health adoption by healthcare professionals: A systematic review. J. Am. Med. Inform. Assoc. 2015, 23, 212–220. [Google Scholar] [CrossRef]
- Hoque, R.; Sorwar, G. Understanding factors influencing the adoption of mHealth by the elderly: An extension of the UTAUT model. Int. J. Med. Inform. 2017, 101, 75–84. [Google Scholar] [CrossRef]
- Jen, W.Y.; Hung, M.C. An empirical study of adopting mobile healthcare service: The family’s perspective on the healthcare needs of their elderly members. Telemed. E-Health 2010, 16, 41–48. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.; Han, S.; Jo, S.H. Consumer choice of on-demand mHealth app services: Context and contents values using structural equation modeling. Int. J. Med. Inform. 2017, 97, 229–238. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Guo, X.; Lai, K.H.; Guo, F.; Li, C. Understanding gender differences in m-health adoption: A modified theory of reasoned action model. Telemed. E-Health 2014, 20, 39–46. [Google Scholar] [CrossRef]
- Lu, C.; Hu, Y.; Xie, J.; Fu, Q.; Leigh, I.; Governor, S.; Wang, C. The use of mobile health applications to improve patient experience: Cross-sectional study in Chinese public hospitals. JMIR Mhealth Uhealth 2018, 6, e126. [Google Scholar] [CrossRef]
- Cheung, M.L.; Chau, K.Y.; Lam, M.H.S.; Tse, G.; Ho, K.Y.; Flint, S.W.; Broom, D.R.; Tso, E.K.H.; Lee, K.Y. Examining consumers’ adoption of wearable healthcare technology: The role of health attributes. Int. J. Environ. Res. Public Health 2019, 16, 2257. [Google Scholar] [CrossRef] [PubMed]
- To, W.M.; Tang, M.N.F. Computer-based course evaluation: An extended technology acceptance model. Educ. Stud. 2019, 45, 131–144. [Google Scholar] [CrossRef]
- Davis, F.D. A Technology Acceptance Model for Empirically Testing New End-User Information Systems: Theory and Results. Ph.D. Thesis, Massachusetts Institute of Technology, Cambridge, MA, USA, 1985. [Google Scholar]
- Davis, F.D. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Q. 1989, 13, 319–340. [Google Scholar] [CrossRef]
- Gefen, D.; Straub, D.W. Gender differences in the perception and use of e-mail: An extension to the technology acceptance model. MIS Q. 1997, 21, 389–400. [Google Scholar] [CrossRef]
- Davis, F.D.; Bagozzi, R.P.; Warshaw, P.R. User acceptance of computer technology: A comparison of two theoretical models. Manag. Sci. 1989, 35, 982–1003. [Google Scholar] [CrossRef]
- Chau, P.Y.K. An empirical assessment of a modified technology acceptance model. J. Manag. Inf. Syst. 1996, 13, 185–204. [Google Scholar] [CrossRef]
- Gefen, D.; Straub, D.W. The relative importance of perceived ease of use in IS adoption: A study of e-commerce adoption. J. Assoc. Inf. Syst. 2000, 1, 8. [Google Scholar] [CrossRef]
- Liu, X.; Wei, K.K. An empirical study of product differences in consumers’ e-commerce adoption behavior. Electron. Commer. Res. Appl. 2003, 2, 229–239. [Google Scholar] [CrossRef]
- Chen, L.; Chin, F.G.; Sun, Y.; Amran, R. Integrating guanxi into technology acceptance: An empirical investigation of WeChat. Telemat. Inform. 2017, 34, 1125–1142. [Google Scholar]
- Kwon, S.J.; Park, E.; Kim, K.J. What drives successful social networking services? A comparative analysis of user acceptance of Facebook and Twitter. Soc. Sci. J. 2014, 51, 534–544. [Google Scholar] [CrossRef]
- Rauniar, R.; Rawski, G.; Yang, Y.; Johnson, B. Technology acceptance model (TAM) and social media usage: An empirical study on Facebook. J. Enterp. Inf. Manag. 2014, 27, 6–30. [Google Scholar] [CrossRef]
- Hur, H.J.; Lee, H.K.; Choo, H.J. Understanding usage intention in innovative mobile app service: Comparison between millennial and mature consumers. Comput. Hum. Behav. 2017, 73, 353–361. [Google Scholar] [CrossRef]
- Vishwanath, A.; Brodsky, L.; Shaha, S. Physician adoption of personal digital assistants (PDA): Testing its determinants within a structural equation model. J. Health Commun. 2009, 14, 77–95. [Google Scholar] [CrossRef]
- Cajita, M.I.; Hodgson, N.A.; Budhathoki, C.; Han, H.R. Intention to use mHealth in older adults with heart failure. J. Cardiovasc. Nurs. 2017, 32, E1. [Google Scholar] [CrossRef]
- Bagozzi, R.P. The legacy of the technology acceptance model and a proposal for a paradigm shift. J. Assoc. Inf. Syst. 2007, 8, 3. [Google Scholar] [CrossRef]
- Benbasat, I.; Barki, H. Quo vadis TAM? J. Assoc. Inf. Syst. 2007, 8, 7. [Google Scholar] [CrossRef]
- Dutta-Bergman, M.J. Primary sources of health information: Comparisons in the domain of health attitudes, health cognitions, and health behaviors. Health Commun. 2004, 16, 273–288. [Google Scholar] [CrossRef] [PubMed]
- Cho, J.; Park, D.; Lee, H.E. Cognitive factors of using health apps: Systematic analysis of relationships among health consciousness, health information orientation, eHealth literacy, and health app use efficacy. J. Med. Internet Res. 2014, 16, e125. [Google Scholar] [CrossRef] [PubMed]
- Ahadzadeh, A.S.; Sharif, S.P.; Ong, F.S.; Khong, K.W. Integrating health belief model and technology acceptance model: An investigation of health-related internet use. J. Med. Internet Res. 2015, 17, e45. [Google Scholar] [CrossRef]
- Yun, E.K.; Park, H.A. Consumers’ disease information–seeking behaviour on the Internet in Korea. J. Clin. Nurs. 2010, 19, 2860–2868. [Google Scholar] [CrossRef]
- Park, J.; Lee, J.; Lee, H.; Truex, D. Exploring the impact of communication effectiveness on service quality, trust and relationship commitment in IT services. Int. J. Inf. Manag. 2012, 32, 459–468. [Google Scholar] [CrossRef]
- Wang, E.T.G.; Chen, J.H.F. Effects of internal support and consultant quality on the consulting process and ERP system quality. Decis. Support Syst. 2006, 42, 1029–1041. [Google Scholar] [CrossRef]
- Lu, Y.; Deng, Z.; Wang, B. Exploring factors affecting Chinese consumers’ usage of short message service for personal communication. Inf. Syst. J. 2010, 20, 183–208. [Google Scholar] [CrossRef]
- Akter, S.; D’Ambra, J.; Ray, P. Trustworthiness in mHealth information services: An assessment of a hierarchical model with mediating and moderating effects using partial least squares (PLS). J. Am. Soc. Inf. Sci. Technol. 2011, 62, 100–116. [Google Scholar] [CrossRef]
- Colledge, B.; Morgan, J.; Tench, R. The concept(s) of trust in late modernity, the relevance of realist social theory. J. Theory Soc. Behav. 2014, 44, 481–503. [Google Scholar] [CrossRef]
- Ou, C.X.; Sia, C.L. Consumer trust and distrust: An issue of website design. Int. J. Hum. Comput. Stud. 2010, 68, 913–934. [Google Scholar] [CrossRef]
- Chang, Y.S.; Fang, S.R. Antecedents and distinctions between online trust and distrust: Predicting high-and low-risk internet behaviors. J. Electron. Commer. Res. 2013, 14, 149–166. [Google Scholar]
- Hasler, G.; Buysse, D.J.; Klaghofer, R.; Gamma, A.; Ajdacic, V.; Eich, D.; Rössler, W.; Angst, J. The association between short sleep duration and obesity in young adults: A 13-year prospective study. Sleep 2004, 27, 661–666. [Google Scholar] [CrossRef] [PubMed]
- Nunnally, J.C.; Bernstein, I.H. Psychometric Theory; McGraw-Hill: New York, NY, USA, 1994. [Google Scholar]
- Brislin, R.W. Back-translation for cross-cultural research. J. Cross Cult. Psychol. 1970, 1, 185–216. [Google Scholar] [CrossRef]
- Cao, Z. Average Chinese Mobile User Installs 56 Apps; China Daily: Beijing, China, 2019; Available online: https://www.chinadaily.com.cn/a/201908/16/WS5d561e4ea310cf3e35566287.html (accessed on 18 November 2019).
- Arbuckle, J.L. IBM SPSS Amos 26 User’s Guide; IBM SPSS: Chicago, IL, USA, 2019. [Google Scholar]
- Hair, J.F., Jr.; Black, W.C.; Babin, B.J.; Anderson, R.E. Multivariate Data Analysis, 7th ed.; Pearson: Essex, UK, 2014. [Google Scholar]
- Hu, L.T.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. A Multidiscip. J. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Fornell, C.; Larcker, D.F. Evaluating structural equation models with unobservable variables and measurement error. J. Mark. Res. 1981, 18, 39–50. [Google Scholar] [CrossRef]
- Kim, K.H.; Kim, K.J.; Lee, D.H.; Kim, M.G. Identification of critical quality dimensions for continuance intention in mHealth services: Case study of onecare service. Int. J. Inf. Manag. 2019, 46, 187–197. [Google Scholar] [CrossRef]
- Le Deu, F.; Parekh, R.; Zhang, F.; Zhou, G. Healthcare in China: Entering Uncharted Waters; McKinsey & Company: Shanghai, China, 2012. [Google Scholar]
- Mellikeche, S.; de Fatima Marin, H.; Elizabeth Benítez, S.; de Lira, A.C.O.; de Quirós, F.G.B.; Degoulet, P. External validation of the Unified Model of Information Systems Continuance (UMISC): An international comparison. Int. J. Med. Inform. 2019. [Google Scholar] [CrossRef]
- Li, A.H. Whom to trust when sick? The Wei Zexi incident, the Chinese Internet and the healthcare system in China. China Perspect. 2016, 4, 79–83. [Google Scholar]
- Podsakoff, P.M.; MacKenzie, S.B.; Lee, J.Y.; Podsakoff, N.P. Common method biases in behavioral research: A critical review of the literature and recommended remedies. J. Appl. Psychol. 2003, 88, 879–903. [Google Scholar] [CrossRef]
| Construct and Items | Factor | CR | AVE |
|---|---|---|---|
| Health consciousness (HC) | 0.90 | 0.76 | |
| HC1—I think it is important to know well about how to stay healthy | 0.91 | ||
| HC2—I think I should take health into account a lot in my life. | 0.96 | ||
| HC3—I ask myself at the time whether the things I eat are healthy for me. | 0.73 | ||
| Communication effectiveness (EC) | 0.80 | 0.57 | |
| CE1—I shall be able to describe my symptoms of illness thoroughly and clearly to doctors through mHealth. | 0.65 | ||
| CE2—Doctors on mHealth are able to diagnose my disease accurately and give me suitable advice according to the information I provide. | 0.86 | ||
| CE3—My communication with doctors on mHealth shall be as effective as going to hospitals and seeing doctors physically. | 0.74 | ||
| Distrust (DIS) | 0.82 | 0.60 | |
| DIS1—mHealth may not have enough professionalism and competence in providing medical service. | 0.69 | ||
| DIS2—I am concerned about the reliability of mHealth. | 0.85 | ||
| DIS3—I am worried about relying on mHealth. | 0.77 | ||
| Perceived ease of use (PEOU) | 0.88 | 0.78 | |
| PEOU1—mHealth is flexible to interact with.1 | 0.49 | ||
| PEOU2—Learning to operate mHealth is easy for me. | 0.85 | ||
| PEOU3—It is easy to become skillful at using mHealth. | 0.94 | ||
| Perceived usefulness (PU) | 0.87 | 0.69 | |
| PU1—Using mHealth is beneficial to my health. | 0.84 | ||
| PU2—The functions of mHealth make my life more convenient. | 0.84 | ||
| PU3—In general, I think that the advantages of mHealth outweigh the disadvantages. | 0.81 | ||
| Intention to use mHealth (INT) | 0.87 | 0.78 | |
| INT1—I am interested in trying to use mHealth. | 0.86 | ||
| INT2—I plan to use mHealth in the near future. | 0.90 |
| Variable | Class | Frequency | Percent |
|---|---|---|---|
| Gender | Male | 211 | 53.4 |
| Female | 275 | 56.6 | |
| Age | 20–24 | 267 | 54.9 |
| 25–29 | 113 | 23.3 | |
| 30–34 | 69 | 14.2 | |
| 35–39 | 37 | 7.6 | |
| Status | Student | 212 | 43.6 |
| Employed | 255 | 52.5 | |
| Self-employed | 12 | 2.5 | |
| Others | 7 | 1.4 | |
| Annual income or family support (in thousands RMB) | <30 | 40 | 8.2 |
| 30–80 | 126 | 25.9 | |
| 80–150 | 144 | 29.7 | |
| 150–800 | 156 | 32.1 | |
| >800 | 20 | 4.1 | |
| Medical insurance | Covered | 408 | 84 |
| Uncovered | 35 | 7.2 | |
| Unclear | 43 | 8.8 | |
| Time spent on mobile phone per day (hours) | <2 | 10 | 2.1 |
| 2–4 | 120 | 24.7 | |
| 4–6 | 165 | 34 | |
| 6–8 | 132 | 27.2 | |
| >8 | 59 | 12.1 |
| Item | Annual Income or Family Support (in Thousand RMB) | ||||
|---|---|---|---|---|---|
| <30 | 30–80 | 80–150 | 150–800 | 800+ | |
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | |
| HC1 | 1.55 (0.597) | 1.48 (0.678) | 1.54 (0.938) | 1.49 (0.807) | 2.25 (1.618) |
| HC2 | 1.43 (0.549) | 1.40 (0.622) | 1.60 (0.956) | 1.52 (0.807) | 2.25 (1.517) |
| HC3 | 1.85 (0.802) | 1.68 (0.876) | 1.99 (0.993) | 1.94 (1.011) | 2.40 (1.353) |
| CE1 | 2.98 (1.097) | 2.78 (0.884) | 2.79 (0.960) | 3.06 (0.883) | 3.60 (0.883) |
| CE2 | 3.03 (0.891) | 2.71 (0.838) | 2.95 (0.847) | 3.04 (0.773) | 3.60 (0.940) |
| CE3 | 3.18 (0.984) | 3.06 (0.851) | 3.10 (0.926) | 3.43 (0.951) | 3.85 (0.754) |
| PEOU2 | 2.45 (0.876) | 2.26 (0.761) | 2.29 (0.860) | 2.10 (0.841) | 2.90 (1.119) |
| PEOU3 | 2.23 (0.800) | 2.17 (0.713) | 2.24 (0.836) | 2.01 (0.884) | 2.85 (1.309) |
| PU1 | 2.48 (0.751) | 2.30 (0.673) | 2.33 (0.802) | 2.27 (0.798) | 2.90 (1.071) |
| PU2 | 2.28 (0.640) | 2.19 (0.654) | 2.29 (0.801) | 2.21 (0.803) | 2.70 (0.865) |
| PU3 | 2.48 (0.816) | 2.33 (0.747) | 2.38 (0.836) | 2.29 (0.887) | 2.80 (1.281) |
| INT1 | 2.40 (0.810) | 2.29 (0.716) | 2.42 (0.920) | 2.58 (0.894) | 3.10 (1.252) |
| INT2 | 2.42 (0.781) | 2.24 (0.686) | 2.33 (0.853) | 2.44 (0.844) | 2.90 (1.210) |
| Construct | Mean (SD) | HC | CE | DIS | PEOU | PU | INT |
|---|---|---|---|---|---|---|---|
| Health consciousness (HC) | 1.66 (0.810) | 0.87 | |||||
| Communication effectiveness (CE) | 3.04 (0.767) | 0.40 ** | 0.75 | ||||
| Distrust (DIS) | 2.18 (0.690) | 0.19 ** | −0.02 | 0.77 | |||
| Perceived ease of use (PEOU) | 2.38 (0.703) | 0.56 ** | 0.45 ** | 0.16 ** | 0.89 | ||
| Perceived usefulness (PU) | 2.32 (0.711) | 0.59 ** | 0.52 ** | 0.09 | 0.71** | 0.83 | |
| Intention to use mHealth (INT) | 2.42 (0.807) | 0.56 ** | 0.53 ** | 0.03 | 0.57 ** | 0.75 ** | 0.88 |
| Relationship | Direct | Indirect | Total |
|---|---|---|---|
| Health consciousness (HC) on PU | 0.33 | 0.00 | 0.33 |
| Communication effectiveness (CE) on PU | 0.43 | 0.00 | 0.43 |
| Perceived ease of use (PEOU) on PU | 0.56 | 0.00 | 0.56 |
| HC on INT | 0.14 | 0.24 | 0.38 |
| CE on INT | 0.16 | 0.32 | 0.48 |
| PEOU on INT | −0.13 | 0.42 | 0.29 |
| PU on INT | 0.74 | 0.00 | 0.74 |
| DIST on INT | −0.07 | 0.00 | −0.07 |
| Hypothesis | Path (Direction) | Standardized Coefficient a | Supported |
|---|---|---|---|
| H1 | PEOU → INT (+) | −0.13 * | No b |
| H2 | PU → INT (+) | 0.74 *** | Yes |
| H3 | PEOU → PU (+) | 0.56 *** | Yes |
| H4 | HC → PU (+) | 0.33 *** | Yes |
| H5 | HC → INT (+) | 0.14 ** | Yes |
| H6 | CE → PU (+) | 0.43 *** | Yes |
| H7 | CE → INT (+) | 0.16 ** | Yes |
| H8 | DIS → INT (-) | −0.07 | No |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
To, W.-M.; Lee, P.K.C.; Lu, J.; Wang, J.; Yang, Y.; Yu, Q. What Motivates Chinese Young Adults to Use mHealth? Healthcare 2019, 7, 156. https://doi.org/10.3390/healthcare7040156
To W-M, Lee PKC, Lu J, Wang J, Yang Y, Yu Q. What Motivates Chinese Young Adults to Use mHealth? Healthcare. 2019; 7(4):156. https://doi.org/10.3390/healthcare7040156
Chicago/Turabian StyleTo, Wai-Ming, Peter K. C. Lee, Jinxuan Lu, Junhao Wang, Yihan Yang, and Qingxin Yu. 2019. "What Motivates Chinese Young Adults to Use mHealth?" Healthcare 7, no. 4: 156. https://doi.org/10.3390/healthcare7040156
APA StyleTo, W.-M., Lee, P. K. C., Lu, J., Wang, J., Yang, Y., & Yu, Q. (2019). What Motivates Chinese Young Adults to Use mHealth? Healthcare, 7(4), 156. https://doi.org/10.3390/healthcare7040156






