Factors Influencing Long-Term Care Service Needs among the Elderly Based on the Latest Anderson Model: A Case Study from the Middle and Upper Reaches of the Yangtze River
Abstract
1. Introduction
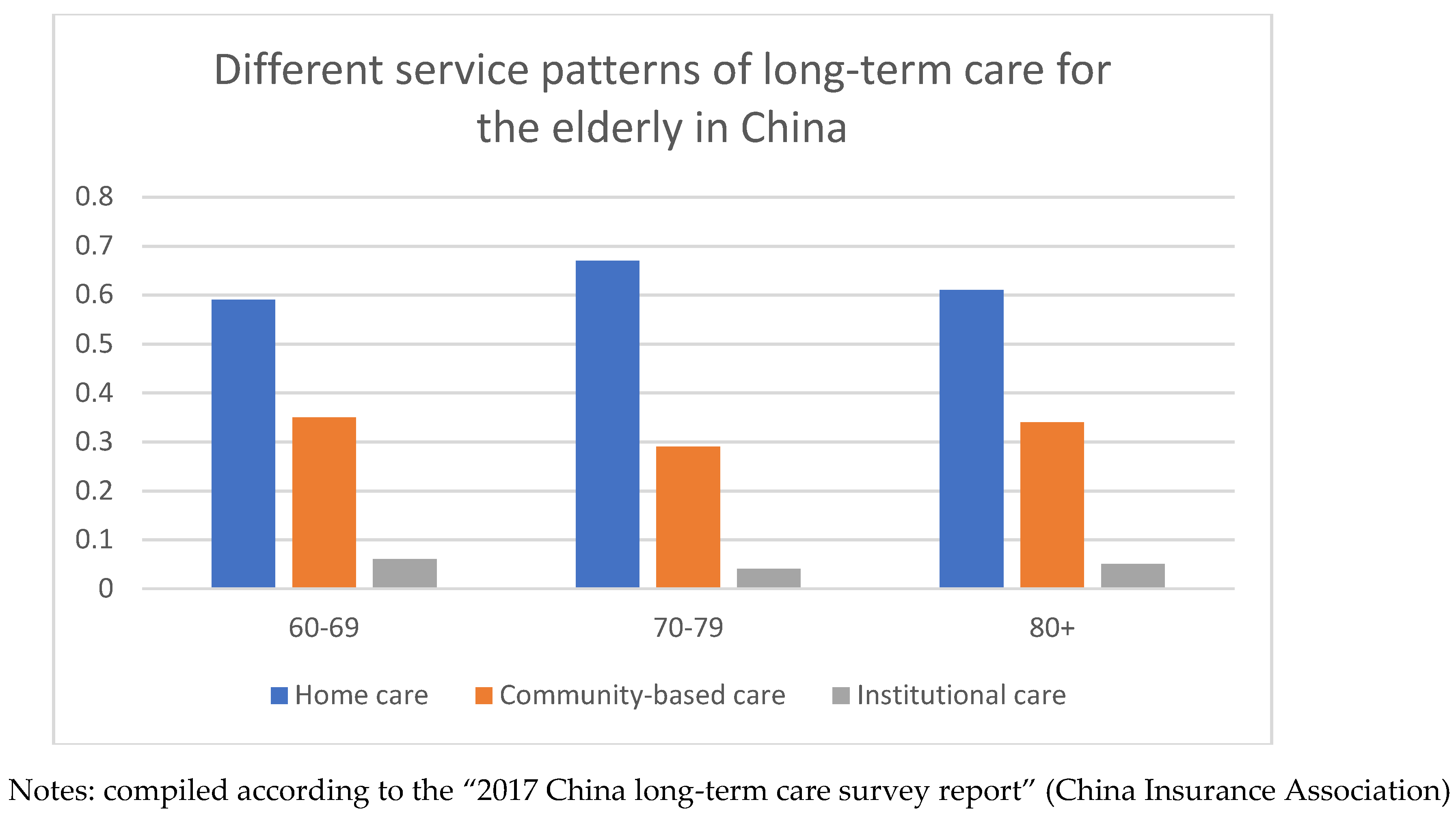
1.1. Current Situation of Long-Term Care in China
1.2. Research on Benchmark Model: Anderson Model
2. Materials and Methods
2.1. Data Source
2.2. Measurement Method
2.2.1. Predisposing Characteristics
2.2.2. Enabling Factors
2.2.3. Need Factors
2.2.4. Psychosocial Factors
3. Results
3.1. Statistical Characteristics Analysis
3.2. Multiple Logistic Analysis
3.3. Sub-Analysis by Gender, by Age, and by Educational Level
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Wang, Q.; Zhou, Y.; Ding, X.; Ying, X. Demand for Long-Term Care Insurance in China. Int. J. Environ. Res. Public Health 2018, 15, 6. [Google Scholar] [CrossRef] [PubMed]
- Lipszyc, B.; Sail, E.; Xavier, A. Long-term Care: Need, Use and Expenditure in the EU-27; Eur Commission: Frankfurt, Germany, 2012. [Google Scholar] [CrossRef]
- Guo, M.; Aranda, M.P.; Silverstein, M. The impact of out-migration on the intergenerational support and psychological wellbeing of older adults in rural China. Ageing Soc. 2009, 29, 1085–1104. [Google Scholar] [CrossRef]
- Hattori, S.; Yoshida, T.; Okumura, Y.; Kondo, K. Effects of Reablement on the Independence of Community-Dwelling Older Adults with Mild Disability: A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2019, 16, 3954. [Google Scholar] [CrossRef] [PubMed]
- Bai, X.; Lai, D.W.L.; Guo, A. Ageism and depression: Perceptions of older people as a burden in China. J. Soc. Issues 2016, 72, 26–46. [Google Scholar] [CrossRef]
- Xu, Q.; Chow, J.C. Exploring the community-based service delivery model: Elderly care in China. Int. Soc. Work 2011, 54, 374–387. [Google Scholar]
- Xu, X.; Chen, L. Projection of Long-Term Care Costs in China, 2020–2050: Based on the Bayesian Quantile Regression Method. Sustainability 2019, 11, 3530. [Google Scholar] [CrossRef]
- Liu, N.; Zeng, L.X.; Li, Z.; Wang, J. Health-related quality of life and long-term care needs among elderly individuals living alone: A cross-sectional study in rural areas of Shaanxi Province, China. BMC Public Health 2013, 13, 313. [Google Scholar] [CrossRef]
- Tokunaga, M.; Hashimoto, H.; Tamiya, N. A gap in formal long-term care use related to characteristics of caregivers and households, under the public universal system in Japan: 2001–2010. Health Policy 2015, 119, 840–849. [Google Scholar] [CrossRef]
- Robison, J.; Shugrue, N.; Fortinsky, R.H.; Gruman, C. Long-term supports and services planning for the future: Implications from a statewide survey of baby boomers and older adults. Gerontologist 2013, 54, 297–313. [Google Scholar] [CrossRef]
- Ye, B.Q. Study on old people’s willingness to select community care mode: An empirical study in Haidian, Beijing. J. Econ. Manag. 2013, 10, 150–153. [Google Scholar]
- Andersen, R.M. Revisiting the behavioral model and access to medical: Does it matter? J. Health Soc. Behav. 1995, 36, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Hsu, H.C. Effects of physical function trajectories on later long-term care utilization among the Taiwanese elderly. Geriatr. Gerontol. Int. 2013, 13, 751–758. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Kwon, S.; Yoon, N.H.; Hyun, K.R. Utilization of long-term care services under the public long-term care insurance program in Korea: Implications of a subsidy policy. Health Policy 2013, 111, 166–174. [Google Scholar] [CrossRef] [PubMed]
- He, A.J.; Chou, K.L. What Affects the Demand for Long-Term Care Insurance? A Study of Middle-Aged and Older Adults in Hong Kong. J. Appl. Gerontol. 2018. [Google Scholar] [CrossRef] [PubMed]
- Yamada, T.; Chen, C.C.; Yamada, T.; Fahs, M.; Fukawa, T. Behavioral analysis of the choice of community-based formal home care, informal home care and nursing home care in Japan. Geneva Pap. Risk Insur. Issues Pract. 2006, 31, 600–632. [Google Scholar] [CrossRef]
- Xu, X.; Xu, Z.; Chen, L.; Li, C. How Does Industrial Waste Gas Emission Affect Health Care Expenditure in Different Regions of China: An Application of Bayesian Quantile Regression. Int. J. Environ. Res. Public Health 2019, 16, 2748. [Google Scholar] [CrossRef] [PubMed]
- Meinow, B.; Kareholt, I.; Lagergren, M. According to need? Predicting the amount of municipal home help allocated to elderly recipients in an urban area of Sweden. Health Soc. Care Community 2005, 13, 366–377. [Google Scholar] [CrossRef]
- Bradley, E.H.; McGraw, S.A.; Curry, L.; Buckser, A.; King, K.L.; Kasl, S.V.; Andersen, R. Expanding the Andersen model: The role of psychosocial factors in longterm care use. J. Health Serv. Res. 2002, 37, 1221–1242. [Google Scholar] [CrossRef] [PubMed]
- Lou, V.W.Q.; Chui, E.W.T.; Leung, A.Y.M.; Kwan, C.W.; Chi, I.; Leung, E.K.S. Characteristics of elderly people who prefer to stay in the community. Asian J. Gerontol. Geriatr. 2009, 4, 36–39. [Google Scholar]
- Montag Schafer, K.; Reidt, S. Assessment of Perceived Barriers to Herpes Zoster Vaccination among Geriatric Primary Care Providers. Pharmacy 2016, 4, 30. [Google Scholar] [CrossRef]
- Tomata, Y.; Watanabe, T.; Tanji, F.; Zhang, S.; Sugawara, Y.; Tsuji, I. The Impact of Psychological Distress on Incident Functional Disability in Elderly Japanese: The Ohsaki Cohort 2006 Study. Int. J. Environ. Res. Public Health. 2018, 15, 2502. [Google Scholar] [CrossRef] [PubMed]
- Chou, R.J.A. Perceived need and actual usage of the family support agreement in rural China: Results from a nationally representative survey. Gerontologist 2010, 51, 295–309. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q. Demands and determinants of community home-based care services for urban elderly: Based on the 2010 National Elderly Survey in China. Popul. Res. 2016, 40, 98–112. [Google Scholar]
- Tian, B.H.; Wang, C.Y. Structural characteristics and determinant factors of the demand of the elderly for social care services: Based on the analysis on the replacement mechanism of family supporting for the elderly. China Rural. Surv. 2014, 4, 2–17. [Google Scholar]
- Komter, A.E.; Vollebergh, W.A.M. Solidarity in Dutch families: Family ties under strain? J. Fam. Issues 2002, 23, 171–188. [Google Scholar] [CrossRef]
- Choi, G.N.; McDougall, G. Unmet needs and depressive symptoms among low-income older adults. J. Gerontol. Soc. Work 2009, 52, 567–583. [Google Scholar] [CrossRef]
- Xu, X.; Chen, L. Influencing factors of disability among the elderly in China, 2003-2016: Application of Bayesian quantile regression. J. Med. Econ. 2019, 22, 605–611. [Google Scholar] [CrossRef]
- Tennstedt, S.; McKinlay, J.; Kasten, L. Unmet need among disabled elders: A problem in access to community long-term care? Soc. Sci. Med. 1994, 38, 915–924. [Google Scholar] [CrossRef]
- Lai, D. Depressive symptoms of elderly Chinese in Guangzhou, Hong Kong, and Taipei. Aging Ment. Health 2009, 13, 725–735. [Google Scholar] [CrossRef]
- Zhang, Y.B.; Harwood, J.; Williams, A.; Ylanne-McEwen, V.; Wadleigh, P.M.; Thimm, C. The portrayal of older adults in advertising: A cross-national review. J. Lang Soc. Psychol. 2006, 25, 264–282. [Google Scholar] [CrossRef]
- Barak, B.; Mathur, A.; Lee, K.; Zhang, Y. Perceptions of age-identity: A cross cultural inner age exploration. Psychol. Mark 2001, 18, 1003–1029. [Google Scholar] [CrossRef]
- Boduroglu, A.; Yoon, C.; Luo, T.; Park, D.C. Age-related stereotypes: A comparison of American and Chinese cultures. Gerontology 2006, 52, 324–333. [Google Scholar] [CrossRef] [PubMed]
- Chiu, S.; Yu, S. An excess of culture: The myth of shared care in the Chinese community in Britain. Aging Soc. 2001, 21, 681–699. [Google Scholar] [CrossRef]
- Chow, N.W.S.; Bai, X. Modernization and its impact on Chinese older people’s perception of their own image and status. Int. Soc. Work 2011, 54, 800–815. [Google Scholar] [CrossRef]
- Wei, X.; Li, Q. The Confucian value of harmony and its influence on Chinese social interaction. Cross Cult. Commun. 2013, 9, 60–66. [Google Scholar] [CrossRef]
- Xu, X.; Huang, X.; Zhang, X.; Chen, L. Family Economic Burden of Elderly Chronic Diseases: Evidence from China. Healthcare 2019, 7, 99. [Google Scholar] [CrossRef]
- Fu, Y.; Guo, Y.; Bai, X.; Chui, E. Factors associated with older people’s longterm care needs: A case study adopting the expanded version of the Anderson Model in China. BMC Geriatr. 2017, 17, 38. [Google Scholar] [CrossRef]
- Bai, X.; Chan, K.S.; Chow, N.W.S. Validation of Self-image evaluation of ageing scale for Chinese elders. Intergener. J. Aging Hum. Dev. 2012, 74, 67–86. [Google Scholar] [CrossRef]
- Zhao, R.F.; Sun, Y.; Lin, X.M. A comparative study of the kinship of the elderly in different geriatric nursing modes. J. Lanzhou Univ. 2015, 1, 120–129. (In Chinese) [Google Scholar]
- Lou, V.W.Q.; Chui, E.W.T.; Leung, A.Y.M.; Tang, K.L.; Chi, I.; Leung, E.K.S.; Kwan, C.W. Factors affecting long-term care use in Hong Kong. Hong Kong Med. J. 2011, 17, 8–12. [Google Scholar]
- Zhan, H.; Liu, G.; Guan, X. Willingness and availability: Explaining new attitudes toward institutional elder care among Chinese elderly parents and their adult children. J. Aging Stud. 2006, 20, 279–290. [Google Scholar] [CrossRef]
- Zhang, Y.; Yu, X. Evaluation of Long-Term Care Insurance Policy in Chinese Pilot Cities. Int. J. Environ. Res. Public Health 2019, 16, 3826. [Google Scholar] [CrossRef] [PubMed]
| Factors | Research Literature | Conclusion |
|---|---|---|
| Intergenerational relationship | Chou (2010) and Wang (2016) [23,24] | Intergenerational relationship had a significant impact on the LTC needs of the elderly |
| Tian & Wang (2014) [25] and Komter & Vollebergh (2002) [26] | Intergenerational relationship had no significant impact on the LTC needs of the elderly | |
| Unmet needs | Choi & McDougall (2009) and Xu & Chen (2019) [27,28] | Unmet needs may negatively affect older adults or their providers, such as increased risk and insecurity of health problems or signs of depression |
| Tennstedt, McKinlay, & Kasten (1994) [29] | Understanding the unmet needs of care services of the elderly can be used as an indicator of future needs of care services | |
| Self-image evaluation | Lai (2009) [30], Zhang. et al. (2006) [31], Barak. et al. (2001) [32], Boduroglu. et al. (2006) [33] | Self-image evaluation of the elderly is rapidly declining |
| Chiu &Y u (2001) [34] and Chow & Bai (2011) [35] | The traditional image of the elderly is now being questioned | |
| Wei & Li (2013) [36] | Negative self-image evaluation that makes the elderly tend to restrain themselves and not express their needs |
| Factors | Total (N = 1308) | Home Care (N = 985) | Community-Based Care (N = 218) | Institutional Care (N = 105) | p | ||||
|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | ||
| Predisposing characteristics | |||||||||
| Age | 0.198 | ||||||||
| 60–69 | 673 | 51.45 | 492 | 49.95 | 122 | 55.96 | 59 | 56.19 | |
| 70 or above | 635 | 48.55 | 493 | 50.05 | 96 | 44.04 | 46 | 43.81 | |
| Gender | 0.206 | ||||||||
| Female | 622 | 47.55 | 453 | 45.99 | 115 | 52.75 | 53 | 50.48 | |
| (Male) | 686 | 52.45 | 532 | 54.01 | 103 | 47.25 | 52 | 49.52 | |
| Educational level | 0.018 | ||||||||
| Below Bachelor’s degree | 954 | 72.94 | 737 | 74.82 | 151 | 69.27 | 66 | 62.86 | |
| (Bachelor’s degree or above) | 354 | 27.06 | 248 | 25.18 | 67 | 30.73 | 39 | 37.14 | |
| Marital status | 0.177 | ||||||||
| Currently not married | 224 | 17.13 | 163 | 16.55 | 36 | 16.51 | 26 | 24.76 | |
| (Currently married) | 1084 | 82.87 | 822 | 83.45 | 182 | 83.49 | 79 | 75.24 | |
| Region | 0.001 | ||||||||
| CQ(Chongqing) | 497 | 38.00 | 358 | 36.35 | 83 | 38.07 | 57 | 54.29 | |
| GZ(Guizhou) | 278 | 21.25 | 198 | 20.10 | 74 | 33.94 | 6 | 5.71 | |
| HB(Hubei) | 283 | 21.64 | 216 | 21.93 | 38 | 17.44 | 29 | 27.62 | |
| (CD)(Chengdu) | 250 | 19.11 | 213 | 21.62 | 23 | 10.55 | 13 | 12.38 | |
| Enabling factors | |||||||||
| Income (thousand, RMB) (mean, SD) | 37.62, 25.12 | 37.40, 25.94 | 38.62, 24.11 | 37.48, 18.67 | 0.040 | ||||
| Number of children (mean, SD) | 2.33, 1.23 | 2.41, 1.24 | 2.10, 1.19 | 2.05, 1.16 | 0.001 | ||||
| Contact frequency with children | <0.001 | ||||||||
| Infrequently | 47 | 3.59 | 25 | 2.54 | 9 | 4.13 | 12 | 11.43 | |
| Sometimes | 150 | 11.47 | 109 | 11.07 | 23 | 10.55 | 18 | 17.14 | |
| (Frequently) | 1111 | 84.94 | 851 | 86.39 | 186 | 85.32 | 75 | 71.43 | |
| Need factors | |||||||||
| IADL (mean, SD) | 7.69, 1.66 | 7.72, 1.61 | 7.59, 1.75 | 7.59, 1.71 | 0.455 | ||||
| Number of chronic diseases (mean, SD) | 1.23, 1.01 | 1.19, 1.04 | 1.36, 1.08 | 1.39, 1.05 | 0.032 | ||||
| Psychosocial factors | |||||||||
| Intergenerational relationships (mean, SD) | 4.94, 0.89 | 4.99, 0.80 | 4.65, 0.88 | 4.36, 1.16 | <0.001 | ||||
| Unmet care service needs (mean, SD) | 4.81, 3.76 | 4.67, 3.57 | 5.42, 3.69 | 4.05, 3.22 | 0.001 | ||||
| Self-image evaluation (mean, SD) | 57.32, 9.02 | 57.66, 8.45 | 53.01, 8.46 | 54.88, 9.77 | 0.019 | ||||
| Factors | Home Care vs. Community-Based Care | Institutional Care vs. Community-Based Care | ||
|---|---|---|---|---|
| p | OR | p | OR | |
| Predisposing characteristics | ||||
| Age | ||||
| 70 or above | 0.7602 | 1.1287 | 0.8011 | 0.9534 |
| (60–69) | ||||
| Gender | ||||
| Female | 0.1270 | 0.7991 | 1.0447 | 1.0521 |
| (Male) | ||||
| Educational level | ||||
| Below Bachelor’s degree | 0.2167 | 1.8923 | 1.0256 | 1.0548 |
| (Bachelor’s degree or above) | ||||
| Marital status | ||||
| Currently not married | 0.8032 | 1.1277 | 0.0168 | 2.4801 |
| (Currently married) | ||||
| Region | ||||
| CQ | 0.0094 | 0.4977 | 0.6573 | 1.3030 |
| GZ | 0.0000 | 1.2782 | 0.0011 | 0.1449 |
| HB | 0.0052 | 0.4011 | 0.9649 | 0.9964 |
| (CD) | ||||
| Enabling factors | ||||
| Income | 0.4809 | 1.0227 | 0.5029 | 0.9996 |
| Number of children | 0.0115 | 1.3314 | 0.6594 | 1.1308 |
| Contact frequency with children | ||||
| Infrequently | 0.4252 | 0.7150 | 0.1207 | 2.5756 |
| Sometimes | 0.2751 | 1.4532 | 0.0609 | 2.2890 |
| (Frequently) | ||||
| Need factors | ||||
| IADL | 0.3843 | 1.1077 | 0.3990 | 0.9681 |
| Number of chronic diseases | 0.1617 | 0.9271 | 0.8232 | 1.0899 |
| Psychosocial factors | ||||
| Intergenerational relationships | 0.7161 | 1.0983 | 0.0199 | 0.7098 |
| Unmet care service needs | 0.0094 | 0.9828 | 0.0283 | 0.9576 |
| Self-image evaluation | 0.0220 | 1.0783 | 0.0273 | 1.0962 |
| Changes in model fits for long-term care needs (*** p < 0.001) | ||||
| Regression models | Pseudo R2 | change | Chi-square | |
| Predisposing | 0.0861 | 73.4034 *** | ||
| Predisposing and enabling | 0.1144 | 0.0283 | 98.6076 *** | |
| Predisposing, enabling, and need | 0.1270 | 0.0126 | 110.039 *** | |
| Predisposing, enabling, need, and psychosocial | 0.1554 | 0.0283 | 136.5735 *** | |
| Factors | Male | Female | ||||||
|---|---|---|---|---|---|---|---|---|
| Home Care vs. Community-Based Care | Institutional Care vs. Community-Based Care | Home Care vs. Community-Based Care | Institutional Care vs. Community-Based Care | |||||
| p | OR | p | OR | p | OR | p | OR | |
| Predisposing characteristics | ||||||||
| Age | ||||||||
| 70 or above | 0.3549 | 1.3891 | 0.7906 | 1.2169 | 0.4924 | 0.8505 | 0.4011 | 0.7003 |
| (60–69) | ||||||||
| Educational level | ||||||||
| Below Bachelor’s degree | 0.3997 | 1.5649 | 0.5047 | 1.2355 | 0.3787 | 1.8864 | 0.3412 | 0.5973 |
| (Bachelor’s degree or above) | ||||||||
| Marital status | ||||||||
| Currently not married | 0.315 | 0.7129 | 0.6489 | 1.4080 | 0.1197 | 1.7493 | 0.0042 | 4.1832 |
| (Currently married) | ||||||||
| Region | ||||||||
| CQ | 0.0430 | 0.3927 | 0.9461 | 0.9607 | 0.1218 | 0.5848 | 0.4578 | 1.6716 |
| GZ | 0.0011 | 0.2058 | 0.0378 | 0.1522 | 0.0042 | 0.3402 | 0.0157 | 0.1155 |
| HB | 0.0168 | 0.2919 | 0.9177 | 0.9250 | 0.1522 | 0.5134 | 1.0206 | 1.0773 |
| (CD) | ||||||||
| Enabling factors | ||||||||
| Income | 0.2016 | 0.9964 | 1.0332 | 1.0510 | 0.5512 | 1.0951 | 0.3003 | 0.9166 |
| Number of children | 0.0094 | 1.5372 | 0.2761 | 1.3555 | 0.2194 | 1.2285 | 0.7644 | 0.9723 |
| Contact frequency with children | ||||||||
| Infrequently | 1.0405 | 1.0584 | 0.0199 | 7.0759 | 0.3969 | 0.6079 | 0.3223 | 0.29295 |
| Sometimes | 0.7654 | 1.2054 | 0.357 | 1.869 | 0.1806 | 1.9246 | 0.0745 | 3.0544 |
| (Frequently) | ||||||||
| Need factors | ||||||||
| IADL | 0.7675 | 1.0153 | 0.1522 | 0.8589 | 0.1543 | 1.1781 | 0.7833 | 1.09725 |
| Number of chronic diseases | 0.5313 | 0.9607 | 0.6457 | 1.1676 | 0.3129 | 0.9261 | 0.7675 | 1.1214 |
| Psychosocial factors | ||||||||
| Intergenerational relationships | 0.5617 | 1.16235 | 0.01995 | 0.59745 | 1.0248 | 1.0458 | 0.3591 | 0.8295 |
| Unmet care service needs | 0.3591 | 1.0122 | 0.8379 | 1.0332 | 0.0042 | 0.9492 | 0.0136 | 0.91035 |
| Self-image evaluation | 0.0304 | 1.0909 | 0.0199 | 1.1235 | 0.3423 | 1.0668 | 0.4788 | 1.071 |
| Factors | 60–69 | 70 or above | ||||||
|---|---|---|---|---|---|---|---|---|
| Home Care vs. Community-Based Care | Institutional Care vs. Community-Based Care | Home Care vs. Community-Based Care | Institutional Care vs. Community-Based Care | |||||
| p | OR | p | OR | p | OR | p | OR | |
| Predisposing characteristics | ||||||||
| Gender | ||||||||
| Female | 0.8232 | 0.9838 | 0.6972 | 1.2432 | 0.0556 | 0.6205 | 0.7801 | 0.9051 |
| (Male) | ||||||||
| Educational level | ||||||||
| Below Bachelor’s degree | 0.0278 | 2.4132 | 0.5977 | 1.0756 | 0.7324 | 0.9018 | 0.6899 | 0.8232 |
| (Bachelor’s degree or above) | ||||||||
| Marital status | ||||||||
| Currently not married | 0.22155 | 1.7598 | 0.00525 | 5.21325 | 0.7497 | 0.9366 | 0.29505 | 1.7934 |
| (Currently married) | ||||||||
| Region | ||||||||
| CQ | 0.0105 | 0.2415 | 0.3549 | 0.5061 | 0.1858 | 0.6541 | 0.273 | 2.0485 |
| GZ | 0.0000 | 0.1092 | 0.0052 | 0.0945 | 0.0136 | 0.3958 | -- | -- |
| HB | 0.0021 | 0.1585 | 0.0861 | 0.2436 | 0.6195 | 0.8064 | 0.0672 | 4.2892 |
| (CD) | ||||||||
| Enabling factors | ||||||||
| Income | 0.7014 | 1.0279 | 0.3717 | 0.9471 | 0.6667 | 1.0206 | 0.7885 | 1.0857 |
| Number of children | 0.1638 | 1.3041 | 0.4882 | 0.8599 | 0.0073 | 1.4731 | 0.2079 | 1.3555 |
| Contact frequency with children | ||||||||
| Infrequently | 0.0535 | 0.3496 | 0.9051 | 0.9219 | 0.4389 | 2.5956 | 0.0252 | 17.5087 |
| Sometimes | 0.8589 | 0.9649 | 0.6835 | 0.8032 | 0.1134 | 2.4108 | 0.0021 | 8.0860 |
| (Frequently) | ||||||||
| Need factors | ||||||||
| IADL | 0.4977 | 0.9397 | 1.0101 | 1.0363 | 0.6982 | 1.0825 | 0.5029 | 0.9712 |
| Number of chronic diseases | 0.0997 | 0.8368 | 0.1743 | 1.4038 | 0.42 | 0.9471 | 0.3895 | 0.8673 |
| Psychosocial factors | ||||||||
| Intergenerational relationships | 0.8526 | 1.0878 | 0.0252 | 0.63 | 0.9555 | 1.0699 | 0.4315 | 0.8263 |
| Unmet care service needs | 0.0283 | 0.9670 | 0.0126 | 0.9009 | 0.147 | 0.9964 | 0.6079 | 1.0143 |
| Self-image evaluation | 0.462 | 1.0626 | 0.0336 | 1.1119 | 0.0294 | 1.092 | 0.4284 | 1.0762 |
| Factors | Below Bachelor’s Degree | Bachelor’s Degree or Above | ||||||
|---|---|---|---|---|---|---|---|---|
| Home Care vs. Community-Based Care | Institutional Care vs. Community-Based Care | Home Care vs. Community-Based Care | Institutional Care vs. Community-Based Care | |||||
| p | OR | p | OR | p | OR | p | OR | |
| Predisposing characteristics | ||||||||
| Age | ||||||||
| 70 or above | 0.0726 | 1.4586 | 0.8301 | 1.2777 | 0.5170 | 0.8930 | 0.4211 | 0.7353 |
| (60–69) | ||||||||
| Gender | ||||||||
| Female | 0.0644 | 1.4464 | 0.5865 | 0.6879 | 0.1036 | 2.1520 | 0.1940 | 0.4178 |
| (Male) | ||||||||
| Marital status | ||||||||
| Currently not married | 0.0307 | 0.7485 | 0.6813 | 1.4784 | 0.1256 | 1.8367 | 0.0044 | 1.3923 |
| (Currently married) | ||||||||
| Region | ||||||||
| CQ | 0.0452 | 0.9123 | 0.9933 | 1.2087 | 0.1278 | 0.9140 | 0.4806 | 1.3551 |
| GZ | 0.0011 | 0.7160 | 0.0396 | 0.7598 | 0.0044 | 0.7572 | 0.0165 | 0.8212 |
| HB | 0.0176 | 0.8064 | 0.9635 | 0.9113 | 0.1598 | 0.8391 | 1.0716 | 0.9311 |
| (CD) | ||||||||
| Enabling factors | ||||||||
| Income | 0.2116 | 1.0462 | 1.0848 | 1.1036 | 0.5788 | 1.1499 | 0.3153 | 0.9624 |
| Number of children | 0.0099 | 1.6140 | 0.2899 | 1.4233 | 0.2304 | 1.2899 | 0.8026 | 1.0209 |
| Contact frequency with children | ||||||||
| Infrequently | 1.0925 | 1.1113 | 0.0209 | 7.4297 | 0.4167 | 0.6383 | 0.3384 | 0.3075 |
| Sometimes | 0.8037 | 1.2656 | 0.3748 | 1.9624 | 0.1896 | 2.0208 | 0.0782 | 3.2071 |
| (Frequently) | ||||||||
| Need factors | ||||||||
| IADL | 0.3059 | 1.0661 | 0.1598 | 0.9018 | 0.1620 | 1.2370 | 0.8224 | 1.0521 |
| Number of chronic diseases | 0.1578 | 1.0087 | 0.6780 | 1.2259 | 0.3285 | 0.9724 | 0.8059 | 1.1774 |
| Psychosocial factors | ||||||||
| Intergenerational relationships | 0.4898 | 1.2204 | 0.0209 | 0.6273 | 1.0760 | 1.0980 | 0.3770 | 0.8709 |
| Unmet care service needs | 0.3770 | 1.0628 | 0.8797 | 1.0848 | 0.0044 | 0.9966 | 0.0143 | 1.9558 |
| Self-image evaluation | 0.0319 | 1.1454 | 0.0209 | 1.1796 | 0.3594 | 1.1201 | 0.5027 | 1.5245 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zeng, L.; Xu, X.; Zhang, C.; Chen, L. Factors Influencing Long-Term Care Service Needs among the Elderly Based on the Latest Anderson Model: A Case Study from the Middle and Upper Reaches of the Yangtze River. Healthcare 2019, 7, 157. https://doi.org/10.3390/healthcare7040157
Zeng L, Xu X, Zhang C, Chen L. Factors Influencing Long-Term Care Service Needs among the Elderly Based on the Latest Anderson Model: A Case Study from the Middle and Upper Reaches of the Yangtze River. Healthcare. 2019; 7(4):157. https://doi.org/10.3390/healthcare7040157
Chicago/Turabian StyleZeng, Liao, Xiaocang Xu, Chunxun Zhang, and Linhong Chen. 2019. "Factors Influencing Long-Term Care Service Needs among the Elderly Based on the Latest Anderson Model: A Case Study from the Middle and Upper Reaches of the Yangtze River" Healthcare 7, no. 4: 157. https://doi.org/10.3390/healthcare7040157
APA StyleZeng, L., Xu, X., Zhang, C., & Chen, L. (2019). Factors Influencing Long-Term Care Service Needs among the Elderly Based on the Latest Anderson Model: A Case Study from the Middle and Upper Reaches of the Yangtze River. Healthcare, 7(4), 157. https://doi.org/10.3390/healthcare7040157





