1. Introduction
Medication errors have health and economic consequences for patients and health services. It is estimated that 2%–3% of all hospital Australian admissions are medication-related [
1], with 66%–75% of patients having a medication error at time of admission [
2,
3] to an Australian hospital, 30% of which have potential to cause harm [
4,
5]. A recent review conducted by the United Kingdom (UK) National Health Service (NHS) found errors occurred at all stages of medication use, from prescribing and dispensing, through administration and monitoring, and they occurred in primary care (38.3%), care homes (41.7%), and secondary care (20%) [
6]. Errors in primary care may contribute greatly to the burden on health systems due to the size of the sector, with the impact estimated to cost the NHS £98.5 million per year, consuming 181,626 bed-days, causing 712 deaths, and contributing to 1708 deaths during hospitalisation [
6]. The authors suggest UK rates are similar to those in comparable settings. There were, however, few quality studies of error rates during transition of care and most studies pertained to medication errors for patients discharged from hospital care.
Best practice medication management includes reconciling medicines on admission to a health service. A Best Possible Medication History (BPMH) involves a structured patient interview and confirmation with at least one other source and is often undertaken by the hospital pharmacist for admitted patients. High-risk medications include the anti-infectives, potassium and other electrolytes, insulin, narcotics and other sedatives, chemotherapeutic agents, and heparin and other anticoagulant (APINCH) medicines ([
7]. Using the BPMH to compare with the medications listed in General Practitioner (GP) referrals, a multisite study conducted in Australian hospitals in 2008–2009 found 87% of GP referrals had one or more discrepancies in the patients’ regular medications and 62% had one or more regular medication discrepancies of moderate to high significance [
8].
Computerised medication systems or some computerised functionality is regarded as a key component of safer medication management. The purported benefits include auto population of medications into transfer of care documents such as referrals, minimising errors associated with ‘cutting and pasting’, up-to-date and accurate lists, inclusion of new, suspended or changed medications supporting clinical handover communication, support of workflow that prompts medication review when patients are identified as a falls risk, and alerts for prescribers when prescribing look-alike, sound-alike and high-risk medications [
7]. An accurate and complete current medication list is a key component of transfer of care documents such as referrals, discharge summaries, and the shared health summary (SHS) that is a crucial part of the Australian electronic MyHealth record system. A SHS is particularly recommended for patients with chronic medical conditions or following a 75+ health assessment and may be created and uploaded by a medical practitioner, usually the patients’ GP, a registered nurse, or an Aboriginal and Torres Strait Islander Health Practitioner [
9]. With increased focus over the last decade on computerised systems including the MyHealth record to provide the right information, for the right patient, at the right time, we sought to quantify the medication discrepancies for patients referred to an emergency department (ED) who were subsequently admitted to hospital and had a Best Possible Medication History taken by a pharmacist. The overarching aim of this study was to identify where strategies to reduce persisting medication error might be best targeted.
2. Materials and Methods
This was a single-site, observational, diagnostic accuracy study undertaken for patients presenting to the ED of an Australian regional hospital between 1 June 2015 and 30 May 2016. Ethics approval was obtained from the Tasmanian Health and Medical Research Ethics Committee (Ref: H0015862).
Patient records were identified retrospectively from the ED medical information system as being referred to the ED by a GP and subsequently admitted as an inpatient. For each patient record, a medication list provided by the GP was compared to the BPMH taken by the hospital pharmacist. The BPMH did not include any medications commenced in the ED as a discrepancy. Medication discrepancies were recorded as omissions, false inclusions, dose and frequency errors, route of administration error, class discrepancies and dosage or frequency omissions.
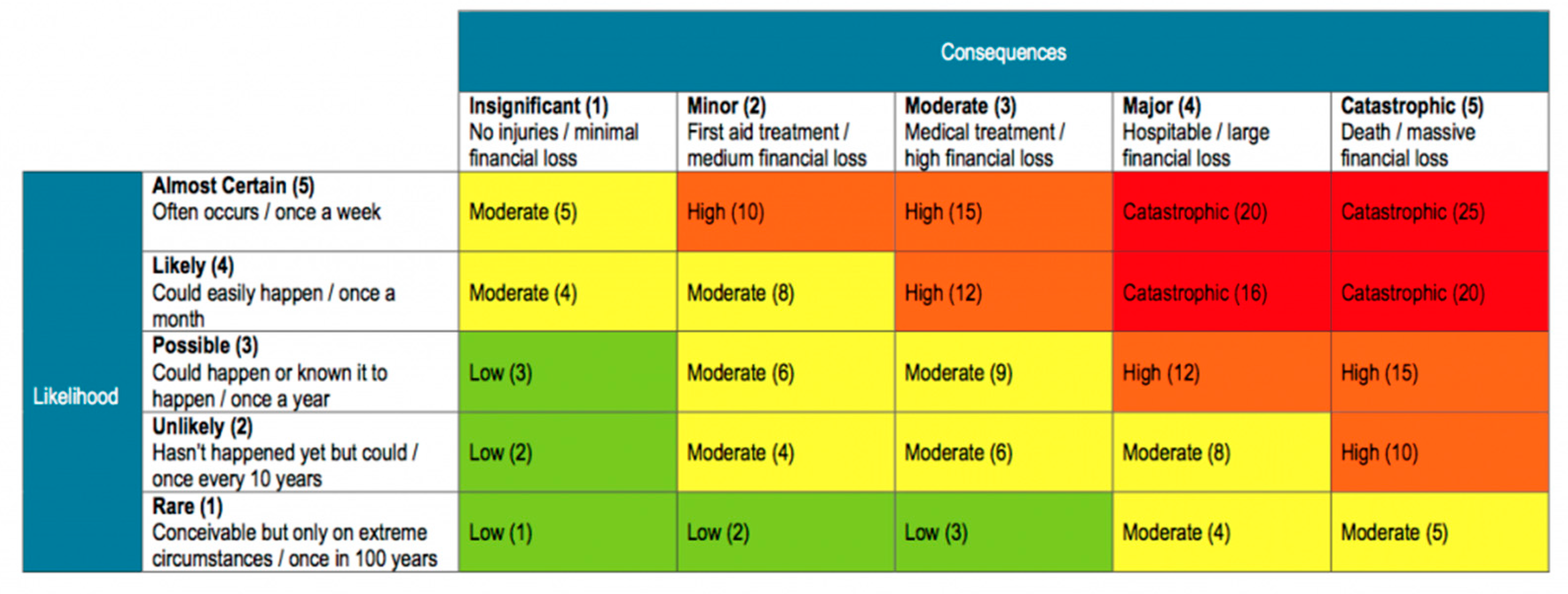
Each discrepancy was given a risk rating by calculating the consequence and likelihood of occurrence using a Risk Assessment Matrix (
Figure 1). The severity of the consequences was assessed by an emergency medicine clinician and rated as insignificant, minor, moderate or major. The likelihood of occurrence was assessed by an emergency medicine clinician and was rated as rare, unlikely, possible, likely, or almost certain.
3. Results
A total of 563 patient records were scrutinised with 143 (25%) of these having both a GP referral and a best possible medication history. Of the 143 patient records, 74 were males and 69 females. A total of 135 (94%) of these histories contained at least one medication discrepancy, all of whom attended ED with computer-generated GP referrals. Inclusions were the most common discrepancy (40%) with omissions being the next most frequent (24.7%) (
Table 1). The rate of medication error (number of medication discrepancies per 100 medications) was 67.18.
3.1. Consequences
Following clinical evaluation of the medication discrepancies, it was found that 94 (15.3%) of discrepancies were of moderate to major consequence (
Table 2). The eight discrepancies of major consequence were seen in three patients. One patient had 13 discrepancies, of which three were of major consequence. One patient had five medications listed on their referral, none of which the patient was taking; the four medications not listed that the patient was found to be taking in the BPMH included an novel oral anticoagulant (NOAC) and a steroid. One patient had one medication listed in the GP referral the patient was not taking, whereas the BPMH found the patient was taking six unlisted medications, including Gliclazide and Metformin. The most common drugs associated with discrepancies of major consequence were insulin and another diabetic medication.
3.2. Likelihood
The likelihood of consequences occurring was almost certain or likely in 28 (4.6%) instances (
Table 3).
3.3. Risk
The consequence and likelihood data were utilised to determine a risk rating for the medication discrepancies. The majority (72.9%) of discrepancies were low risk (
Table 4). However, the risk was high or extreme in 96 (15.6%) instances.
The 13 extreme risk ratings were from discrepancies of major consequence which were likely (n = 7) or almost certain (n = 1) and applied to five patients. One patient presented with hypercalcaemia and the GP referral listed five diabetic medications the patient was not taking, and was missing the apixaban, cholecalciferol, magnesium and prednisone the patient was taking; one patient presented with abdominal pain, tachycardia, and atrial fibrillation and the referral contained one medication the patient was not taking, and was missing six medications the patient was taking; one patient presented with bilateral pulmonary infiltrate for whom the supplements fish oil, glucosamine and magnesium were missing from the GP referral; one patient presented with abdominal pain whose blood pressure medication was not recorded on the GP referral list nor were two medications for depression. In only one of these instances was the referring GP not the patient’s usual GP.
The 78 high-risk ratings related to 35 patients, two of whom also had extreme ratings for some discrepancies. Of the remaining patients, one patient presenting with a diabetic foot ulcer had eight discrepancies rated as high risk, none of the 11 patient’s medications were contained in the referral; one patient presenting with shortness of breath and chest pain had three medications listed, only one of which the patient was taking, together with nine others missing in the referral, including a nitrate, nitrate spray and a vasodilator. In both instances, the referring GP was the patient’s usual GP.
In 48.8% of the high-risk discrepancies the GP authoring the referral was listed as the patients usual GP, and no one GP was represented more than another.
4. Discussion
Medication errors have the potential for significant patient harm and cost to the health system. Computerised medication management is promoted to reduce the likelihood of error. In this study, the rate of medication discrepancies observed in General Practitioner (GP) patient referrals where at least one medication discrepancy occurred was 67% despite the use of computerised systems for medication management. One-quarter of these discrepancies were of a moderate to extreme risk.
The premise of having a nominated provider for the electronic health information summary (Australia), MyHealth record, is that it is critical to have shared health summaries (SHSs) that are clinically useful and effective for a range of different types of healthcare providers who may review them [
9]. The World Health Organisation advocates the use of shared electronic medical records and an intersectoral approach to reorient health systems to person-centered care [
5]. In this study, the important role of the hospital pharmacist in reconciling medications was highlighted. While it is unknown how or why so many medication discrepancies occurred, better medication reconciliation in the community is an opportunity for reducing burden associated with medication error. Whether this can be easily performed by the GP through more frequent medication review, or whether there is a role for the community pharmacist or general practice nurse, may depend on the community and available resources.
This study was conducted at a single regional site; it is known that there are fewer GPs in rural towns per capita than in urban areas, and this area has an older population and a high rate of chronic health issues [
10]. The rate of medication discrepancy was calculated from the number of referrals with at least one discrepancy present. As 6% of the sample did not contain any discrepancies, the overall rate of medication discrepancy is likely to be slightly lower. Nevertheless, that one-quarter of these were of moderate to extreme risk suggests there is considerable opportunity to improve patient health outcomes through better medication reconciliation in the community.
5. Conclusions
This paper presents clinically important data that can contribute to ongoing education, quality assurance and meaningful interaction between medical professionals. Improving medication reconciliation in the community may reduce the burden associated with preventable medication errors. Whether this is achieved by more frequent GP-led medication review or community-based pharmacist medication review may depend on the community and available resources.
Author Contributions
Conceptualization, C.C., S.J.P., D.C., C.E., A.W. and N.S.R.; methodology, C.C., D.C., C.E.; data collection, D.C., C.E., N.S.R. and C.C.; formal analysis, S.J.P., C.C., N.S.R.; investigation, S.J.P., C.C.; resources, S.J.P., C.C.; data curation, S.J.P., C.C., N.S.R.; writing—original draft preparation, C.C., S.J.P.; writing—review and editing, D.C., C.E., N.S.R., A.W.; supervision, C.C., S.J.P.; and project administration, S.J.P., C.C., N.S.R.
Funding
This research received no external funding.
Acknowledgments
The authors would like to acknowledge the assistance in data collection from Edith Lightfoot and Emily Doole.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Roughead, E.E.; Semple, S.J.; Rosenfeld, E. The extent of medication errors and adverse drug reactions throughout the patient journey in acute care in Australia. Int. J. Evid. Based Healthc. 2016, 14, 113–122. [Google Scholar] [CrossRef] [PubMed]
- Tompson, A.; Peterson, G.; Jackson, S.; Hughes, J.D.; Raymond, K. Utilizing community pharmacy dispensing records to disclose errors in hospital admission drug charts. Int. J. Clin. Pharmacol. Ther. 2012, 50, 639–646. [Google Scholar] [CrossRef] [PubMed]
- Vasileff, H.M.; Whitten, L.E.; Pink, J.A.; Goldsworthy, S.J.; Angley, M.T. The effect on medication errors of pharmacists charting medication in an emergency department. Pharm. World Sci. 2009, 31, 373–379. [Google Scholar] [CrossRef] [PubMed]
- Duguid, M. The importance of medication reconciliation for patients and practitioners. Aust. Prescr. 2012, 35, 373–379. [Google Scholar] [CrossRef]
- Azzi, M.; Constantino, M.; Pont, L.; Mcgill, M.; Twigg, S.; Krass, I. Medication Safety: an audit of medication discrepancies in transferring type 2 diabetes mellitus (T2DM) patients from Australian primary care to tertiary ambulatory care. Int. J. Qual. Health C. 2014, 26, 397–403. [Google Scholar] [CrossRef] [PubMed]
- Prevalence and Economic Burden of Medication Errors in The NHS in England. Rapid evidence synthesis and economic analysis of the prevalence and burden of medication error in the UK. Available online: http://www.eepru.org.uk/wp-content/uploads/2018/02/eepru-report-medication-error-feb-2018.pdf (accessed on 16 September 2017).
- Electronic Medication Management Systems: A guide to safe implementation. Available online: https://www.safetyandquality.gov.au/sites/default/files/migrated/Electronic-Medication-Management-Systems-A-guide-to-safe-implementation-third-edition.pdf (accessed on 14 November 2017).
- Shared Health Summaries. Available online: https://www.myhealthrecord.gov.au/for-healthcare-professionals/howtos/shared-health-summaries (accessed on 6 May 2018).
- Taylor, S.; Welch, S.; Harding, A.; Abbott, L.; Riyat, B.; Morrow, M.; Lawrence, D.; Rodda, S.; Heward, S. Accuracy of general practitioner medication histories for patients presenting to the emergency department. Aust. Fam. Physician 2014, 43, 728. [Google Scholar] [PubMed]
- National Health Survey. Available online: https://www.ausstats.abs.gov.au/ausstats/subscriber.nsf/0/CDA852A349B4CEE6CA257F150009FC53/$File/national%20health%20survey%20first%20results,%202014-15.pdf (accessed on 4 April 2018).
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).