Maternal Health and Green Spaces in China: A Longitudinal Analysis of MMR Based on Spatial Panel Model
Abstract
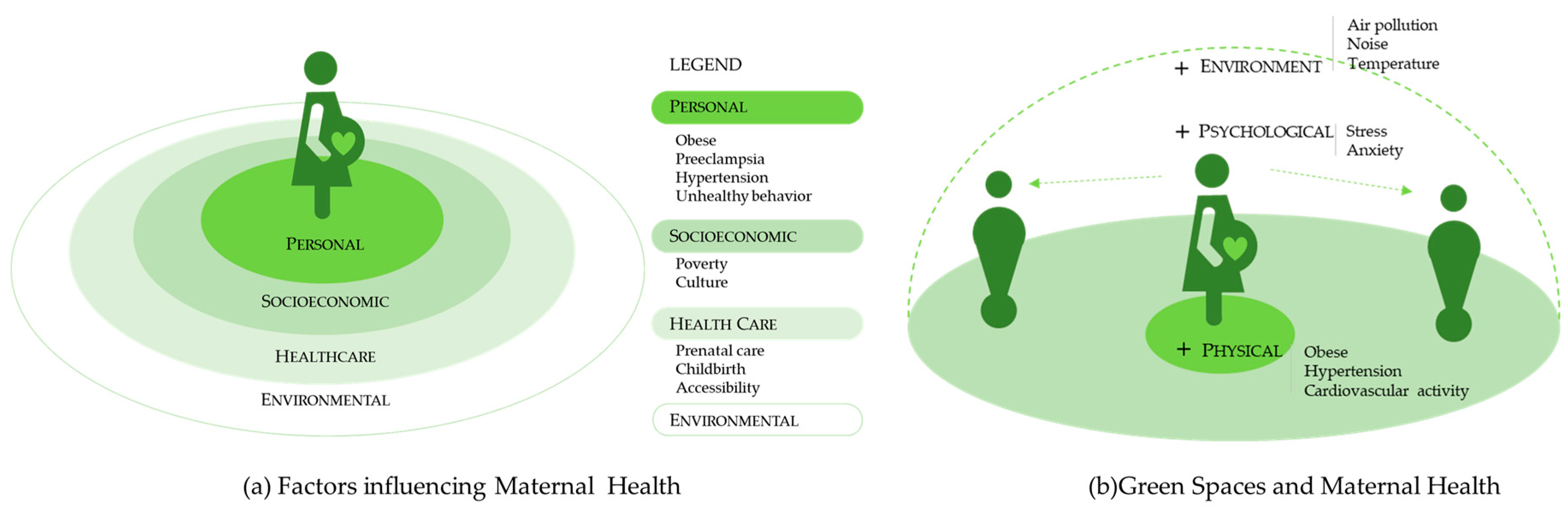
1. Introduction
2. Materials and Methods
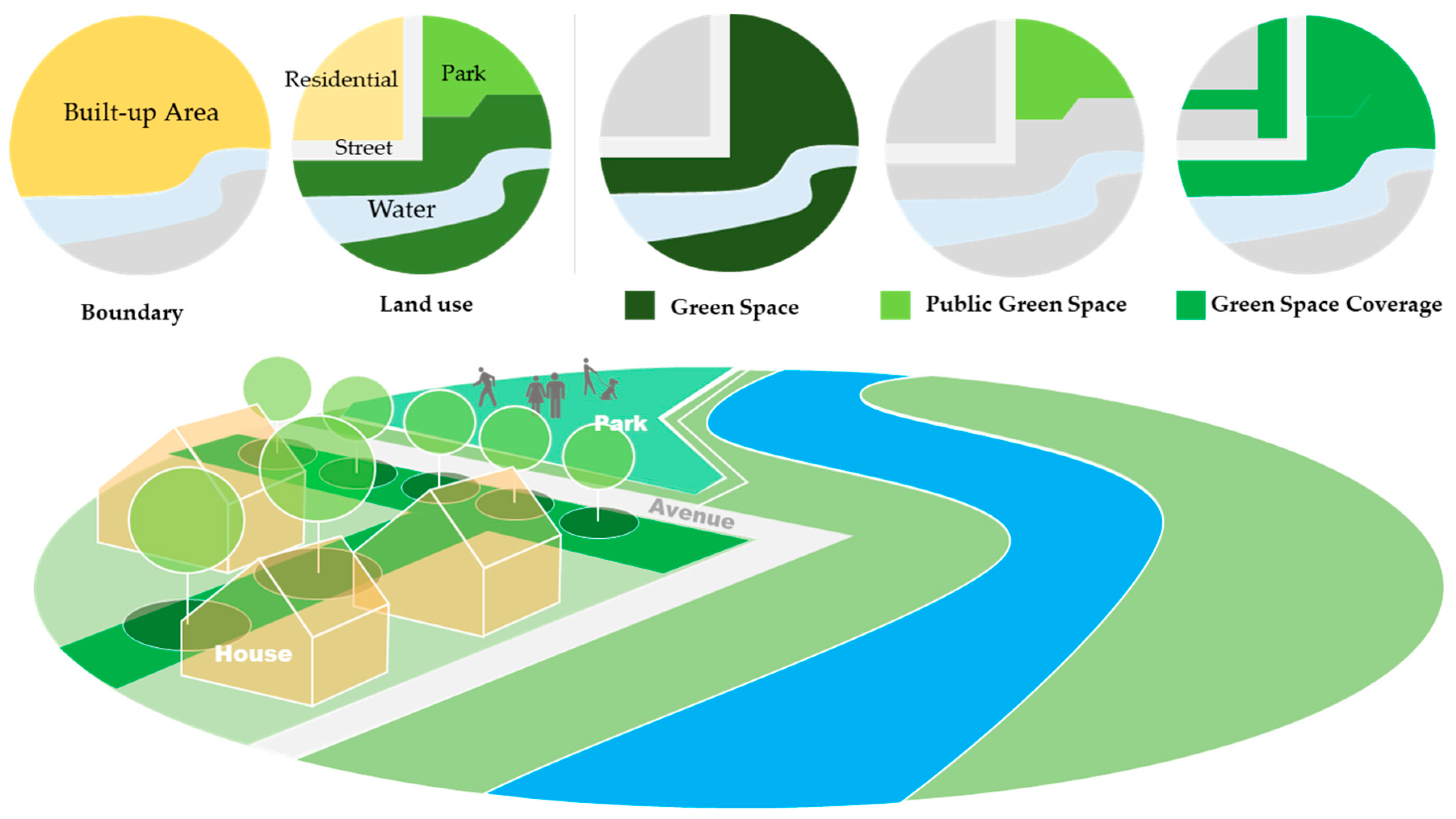
2.1. Variables and Data Source
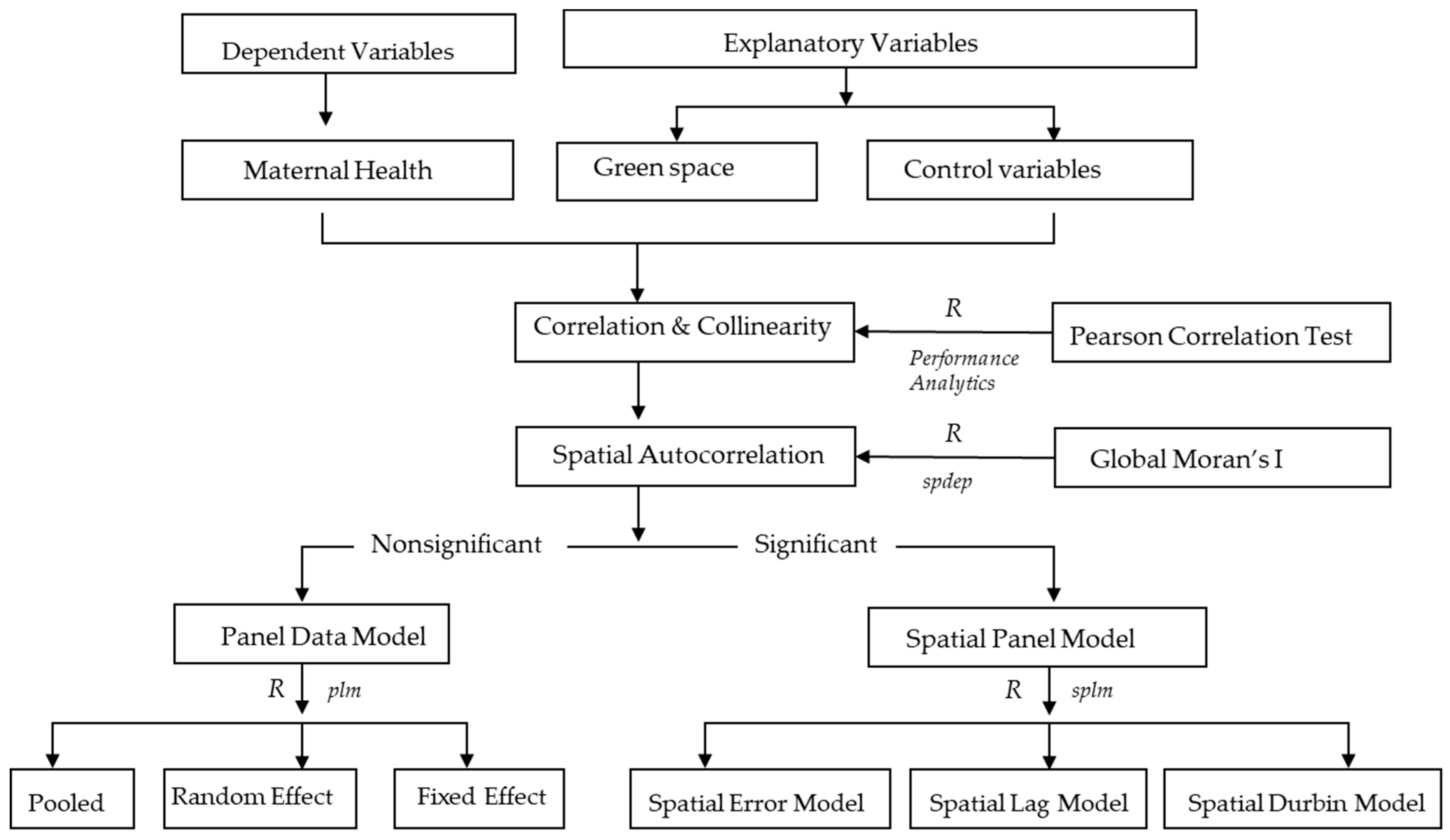
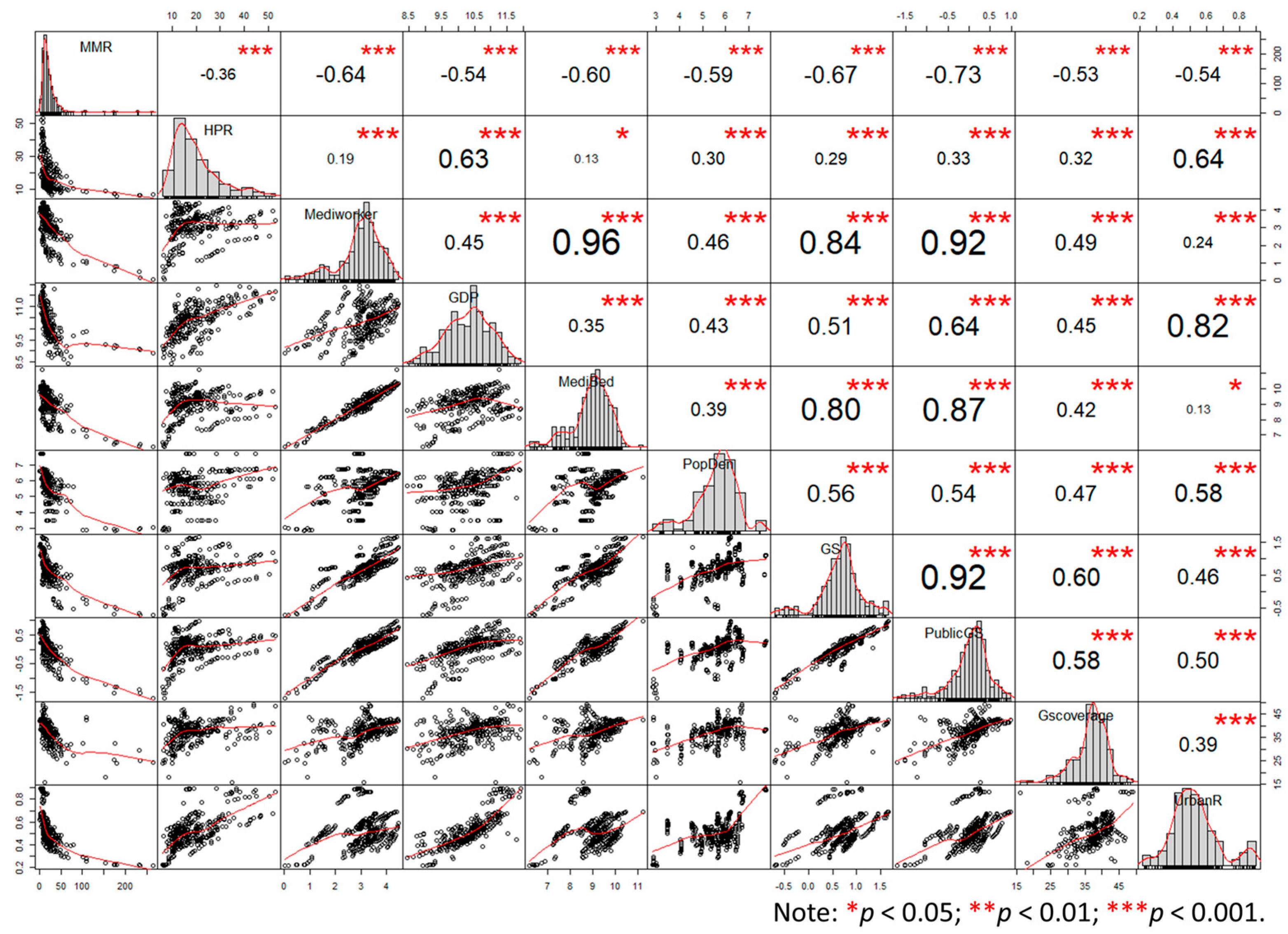
2.2. Methods
3. Results
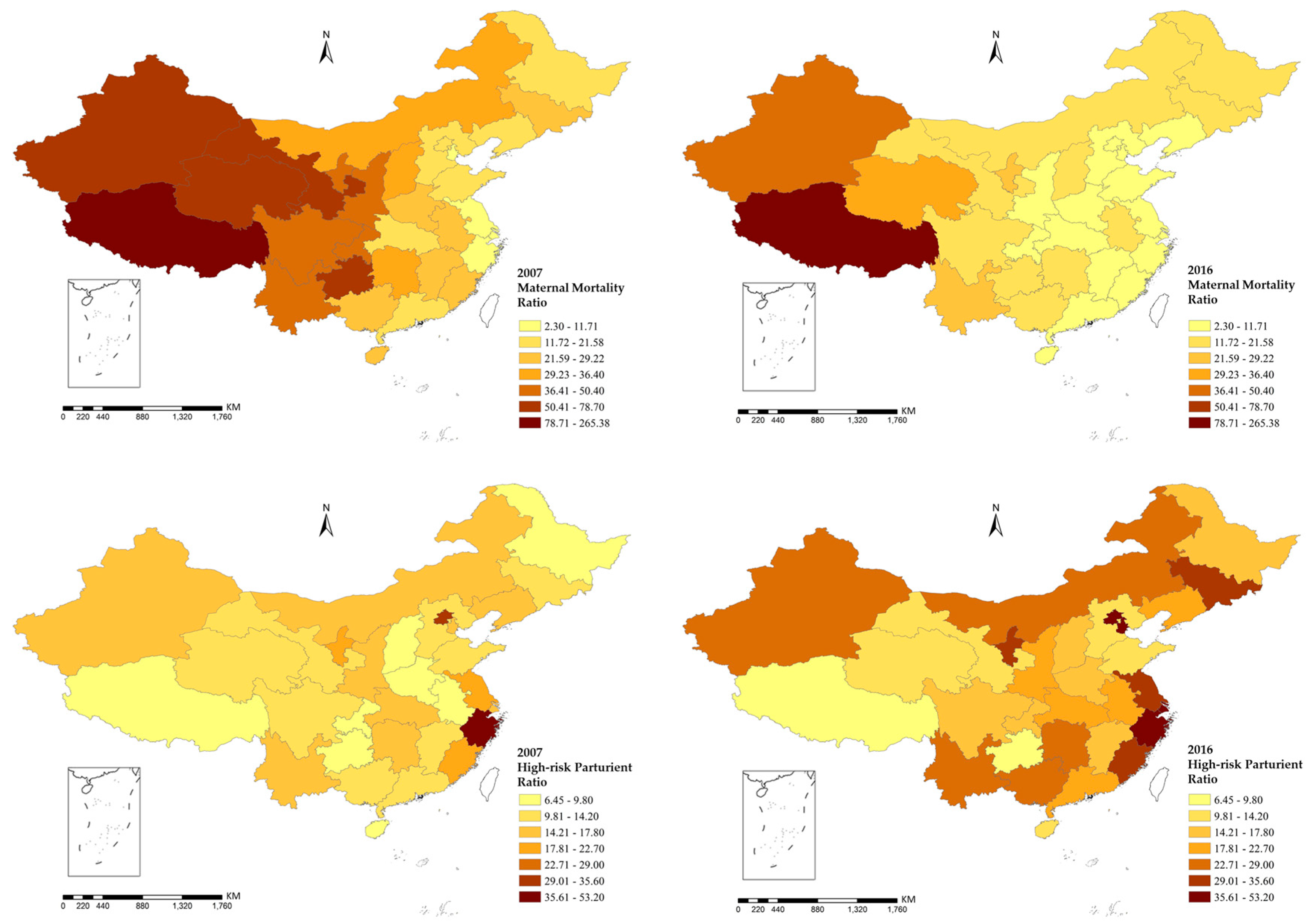
3.1. Description Analysis
3.2. Global Moran’s I Statistics
3.3. Panel Data Model
3.4. Spatial Panel Model
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Beaglehole, R.; Bonita, R. Global public health: A scorecard. Lancet 2008, 372, 1988–1996. [Google Scholar] [CrossRef]
- Singh, K.; Story, W.T.; Moran, A.C. Assessing the continuum of care pathway for maternal health in South Asia and sub-Saharan Africa. Matern. Child Health J. 2016, 20, 281–289. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, S.; Creanga, A.A.; Gillespie, D.G.; Tsui, A.O. Economic status, education and empowerment: Implications for maternal health service utilization in developing countries. PLoS ONE 2010, 5, e11190. [Google Scholar] [CrossRef] [PubMed]
- Feng, X.L.; Zhu, J.; Zhang, L.; Song, L.; Hipgrave, D.; Guo, S.; Ronsmans, C.; Guo, Y.; Yang, Q. Socio-economic disparities in maternal mortality in China between 1996 and 2006. BJOG Int. J. Obstet. Gynecol. 2010, 117, 1527–1536. [Google Scholar] [CrossRef]
- Liang, J.; Li, X.; Kang, C.; Wang, Y.; Kulikoff, X.R.; Coates, M.M.; Ng, M.; Luo, S.; Mu, Y.; Wang, X.; et al. Maternal mortality ratios in 2852 Chinese counties, 1996–2015, and achievement of Millennium Development Goal 5 in China: A subnational analysis of the Global Burden of Disease Study 2016. Lancet 2019, 393, 241–252. [Google Scholar] [CrossRef]
- Huang, Y.; Shallcross, D.; Pi, L.; Tian, F.; Pan, J.; Ronsmans, C. Ethnicity and maternal and child health outcomes and service coverage in western China: A systematic review and meta-analysis. Lancet Glob. Health 2018, 6, e39–e56. [Google Scholar] [CrossRef]
- Liang, J.; Zhu, J.; Dai, L.; Li, X.; Li, M.; Wang, Y. Maternal mortality in China, 1996–2005. Int. J. Obstet. Gynecol. 2010, 110, 93–96. [Google Scholar] [CrossRef]
- Li, Y.; Zhang, Y.; Fang, S.; Liu, S.; Liu, X.; Li, M.; Liang, H.; Fu, H. Analysis of inequality in maternal and child health outcomes and mortality from 2000 to 2013 in China. Int. J. Equity Health 2017, 16, 66. [Google Scholar] [CrossRef]
- Dadvand, P.; Wright, J.; Martinez, D.; Basagaña, X.; Mceachan, R.R.; Cirach, M.; Gidlow, C.J.; De, H.K.; Gražulevičienė, R.; Nieuwenhuijsen, M.J. Inequality, green spaces, and pregnant women: Roles of ethnicity and individual and neighbourhood socioeconomic status. Environ. Int. 2014, 71, 101–108. [Google Scholar] [CrossRef]
- Morellofrosch, R.; Shenassa, E.D. The environmental “riskscape” and social inequality: Implicationsfor explaining maternal and child health disparities. Environ. Health Perspect. 2006, 114, 1150–1153. [Google Scholar] [CrossRef]
- Timmermans, S.; Bonsel, G.J.; Steegers-Theunissen, R.P.M.; Mackenbach, J.P.; Steyerberg, E.W.; Raat, H.; Verbrugh, H.A.; Tiemeier, H.W.; Hofman, A.; Birnie, E.; et al. Individual accumulation of heterogeneous risks explains perinatal inequalities within deprived neighbourhoods. Eur. J. Epidemiol. 2011, 26, 165–180. [Google Scholar] [CrossRef] [PubMed]
- Izugbara, C.O.; Ngilangwa, D.P. Women, poverty and adverse maternal outcomes in Nairobi, Kenya. BMC Women’s Health 2010, 10, 33. [Google Scholar] [CrossRef] [PubMed]
- Dadvand, P.; Nazelle, A.D.; Figueras, F.; Basagaña, X.; Su, J.; Amoly, E.; Jerrett, M.; Vrijheid, M.; Sunyer, J.; Nieuwenhuijsen, M.J. Green space, health inequality and pregnancy. Environ. Int. 2012, 40, 110–115. [Google Scholar] [CrossRef] [PubMed]
- James, P.; Banay, R.F.; Hart, J.E.; Laden, F. A review of the health benefits of greenness. Curr. Epidemiol. Rep. 2015, 2, 131–142. [Google Scholar] [CrossRef]
- Both, M.I.; Overvest, M.A.; Wildhagen, M.F.; Golding, J.; Wildschut, H.I.J. The association of daily physical activity and birth outcome: A population-based cohort study. Eur. J. Epidemiol. 2010, 25, 421–429. [Google Scholar] [CrossRef]
- Hegaard, H.K.; Pedersen, B.K.; Birgitte Bruun, N.; Peter, D. Leisure time physical activity during pregnancy and impact on gestational diabetes mellitus, pre-eclampsia, preterm delivery and birth weight: A review. Acta Obstet. Gynecol. Scand. 2011, 86, 1290–1296. [Google Scholar] [CrossRef]
- Hjortebjerg, D.; Andersen, A.M.N.; Ketzel, M.; Pedersen, M.; Raaschou-Nielsen, O.; Sørensen, M. Associations between maternal exposure to air pollution and traffic noise and newborn’s size at birth: A cohort study. Environ. Int. 2016, 95, 1–7. [Google Scholar] [CrossRef]
- Kingsley, S.L.; Eliot, M.N.; Whitsel, E.A.; Huang, Y.-T.; Kelsey, K.T.; Marsit, C.J.; Wellenius, G.A. Maternal residential proximity to major roadways, birth weight, and placental DNA methylation. Environ. Int. 2016, 92–93, 43–49. [Google Scholar] [CrossRef]
- Rondó, P.H.C.; Ferreira, R.F.; Nogueira, F.; Ribeiro, M.C.N.; Lobert, H.; Artes, R. Maternal psychological stress and distress as predictors of low birth weight, prematurity and intrauterine growth retardation. Eur. J. Clin. Nutr. 2003, 57, 266–272. [Google Scholar] [CrossRef]
- Grote, N.K.; Bridge, J.A.; Gavin, A.R.; Melville, J.L.; Satish, I.; Katon, W.J. A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Arch. Gen. Psychiatry 2010, 67, 1012. [Google Scholar] [CrossRef]
- Gill, S.E.; Handley, J.F.; Ennos, A.R.; Pauleit, S. Adapting cities for climate change: The role of the green infrastructure. Built Environ. 2007, 33, 115–133. [Google Scholar] [CrossRef]
- Scotland, H. Guide to HIA of Greenspace (Greenspace, Scotland). Available online: http://cloud.snappages.com/803c0945dd99f78b94cef59b278fec5244df7b24/HIA%20of%20greenspace%20a%20guide%20-%20GS%20HS%20SNH%20IOM%20Scotland%20-%202008.pdf (accessed on 28 November 2019).
- Lawton, E.; Brymer, E.; Clough, P.; Denovan, A. The relationship between the physical activity environment, nature relatedness, anxiety, and the psychological well-being benefits of regular exercisers. Front. Psychol. 2017, 8, 1058. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.C.; Maheswaran, R. The health benefits of urban green spaces: A review of the evidence. J. Public Health 2011, 33, 212–222. [Google Scholar] [CrossRef] [PubMed]
- Maas, J.; van Dillen, S.M.; Verheij, R.A.; Groenewegen, P.P. Social contacts as a possible mechanism behind the relation between green space and health. Health Place 2009, 15, 586–595. [Google Scholar] [CrossRef]
- Maas, J.; Verheij, R.A.; de Vries, S.; Spreeuwenberg, P.; Schellevis, F.G.; Groenewegen, P.P. Morbidity is related to a green living environment. J. Epidemiol. Community Health 2009, 63, 967–973. [Google Scholar] [CrossRef]
- Nowak, D.J.; Crane, D.E.; Stevens, J.C. Air pollution removal by urban trees and shrubs in the United States. Urban For. Urban Green. 2006, 4, 115–123. [Google Scholar] [CrossRef]
- Whitford, V.; Ennos, A.R.; Handley, J.F. “City form and natural process”—Indicators for the ecological performance of urban areas and their application to Merseyside, UK. Landsc. Urban Plan. 2001, 57, 91–103. [Google Scholar] [CrossRef]
- Martine, V.; David, M.; Sandra, M.; Payam, D.; Anna, S.; Judith, R.; Mark, N. Ambient air pollution and risk of congenital anomalies: A systematic review and meta-analysis. Environ. Health Perspect. 2011, 119, 598–606. [Google Scholar]
- Sapkota, A.; Chelikowsky, A.P.; Nachman, K.E.; Cohen, A.J.; Ritz, B. Exposure to particulate matter and adverse birth outcomes: A comprehensive review and meta-analysis. Air Qual. Atmos. Health 2012, 5, 369–381. [Google Scholar] [CrossRef]
- Rupa, B.; Brian, M.; Bart, O. High ambient temperature and the risk of preterm delivery. Am. J. Epidemiol. 2010, 172, 1108. [Google Scholar]
- Wolch, J.R.; Byrne, J.; Newell, J.P. Urban green space, public health, and environmental justice: The challenge of making cities ‘just green enough’. Landsc. Urban Plan. 2014, 125, 234–244. [Google Scholar] [CrossRef]
- Banay, R.F.; Bezold, C.P.; James, P.; Hart, J.E.; Laden, F. Residential greenness: Current perspectives on its impact on maternal health and pregnancy outcomes. Int. J. Women’s Health 2017, 9, 133–144. [Google Scholar] [CrossRef]
- Payam, D.; Jordi, S.; Xavier, B.A.; Ferran, B.; Aitana, L.; Ana, F.S.; Marisa, E.; Raquel, G.E.; Mendez, M.A.; Nieuwenhuijsen, M.J. Surrounding greenness and pregnancy outcomes in four Spanish birth cohorts. Environ. Health Perspect. 2012, 120, 1481–1487. [Google Scholar]
- Casey, J.A.; James, P.; Rudolph, K.E.; Wu, C.D.; Schwartz, B.S. Greenness and birth outcomes in a range of Pennsylvania communities. Int. J. Environ. Res. Public Health 2016, 13, 311. [Google Scholar] [CrossRef]
- China Health Statistics Yearbook, 2007–2016. Available online: http://data.cnki.net/yearbook/Single/N2019030282 (accessed on 15 June 2018).
- China Statistics Yearbook, 2007–2016. Available online: http://data.cnki.net/yearbook/Single/N2019110002 (accessed on 15 June 2018).
- Liu, L.; Zhong, Y.; Ao, S.; Wu, H. Exploring the relevance of green space and epidemic diseases based on panel data in China from 2007 to 2016. Int. J. Environ. Res. Public Health 2019, 16, 2551. [Google Scholar] [CrossRef]
- Véronique, F.; Carine, R.; Campbell, O.M.R.; Graham, W.J.; Anne, M.; Jo, B.; Marjorie, K.; David, O. Maternal health in poor countries: The broader context and a call for action. Lancet 2006, 368, 1535–1541. [Google Scholar]
- Tunçalp, Ö.; Souza, J.P.; Hindin, M.J.; Santos, C.A.; Oliveira, T.H.; Vogel, J.P.; Togoobaatar, G.; Ha, D.Q.; Say, L.; Gülmezoglu, A.M.; et al. Education and severe maternal outcomes in developing countries: A multicountry cross-sectional survey. BJOG Int. J. Obstet. Gynecol. 2014, 121, 57–65. [Google Scholar] [CrossRef]
- Marmot, M. Social determinants of health inequalities. Lancet 2012, 51, 1–4. [Google Scholar] [CrossRef]
- Levy, L.; Herzog, A.N. Effects of population density and crowding on health on health and social adapation in the Netherlands. J. Health Soc. Behav. 1974, 15, 228–240. [Google Scholar] [CrossRef]
- Gage, A.J. Barriers to the utilization of maternal health care in rural Mali. Soc. Sci. Med. 2007, 65, 1666–1682. [Google Scholar] [CrossRef]
- Cao, Q.; Liang, Y.; Niu, X. China’s air quality and respiratory disease mortality based on the spatial panel model. Int. J. Environ. Res. Public Health 2017, 14, 1081. [Google Scholar] [CrossRef] [PubMed]
- Hystad, P.; Davies, H.W.; Frank, L.; Van Loon, J.; Gehring, U.; Tamburic, L.; Brauer, M. Residential greenness and birth outcomes: Evaluating the influence of spatially correlated built-environment factors. Environ. Health Perspect. 2014, 122. [Google Scholar] [CrossRef] [PubMed]
- Grazuleviciene, R.; Danileviciute, A.; Dedele, A.; Vencloviene, J.; Andrusaityte, S.; Uždanaviciute, I.; Nieuwenhuijsen, M.J. Surrounding greenness, proximity to city parks and pregnancy outcomes in Kaunas cohort study. Int. J. Hyg. Environ. Health 2015, 218, 358–365. [Google Scholar] [CrossRef] [PubMed]
- Davey, G. Happiness and quality of life in the people’s republic of China. In Happiness across Cultures; Springer: Dordrecht, The Netherlands, 2012. [Google Scholar] [CrossRef]
- Harpham, T. Urbanization and mental health in developing countries: A research role for social scientists, public health professionals and social psychiatrists. Soc. Sci. Med. 1994, 39, 233–245. [Google Scholar] [CrossRef]
- Moore, M.; Gould, P.; Keary, B.S. Global urbanization and impact on health. Int. J. Hyg. Environ. Health 2003, 206, 269–278. [Google Scholar] [CrossRef] [PubMed]
- Fuller, R.A.; Gaston, K.J. The scaling of green space coverage in European cities. Biol. Lett. 2009, 5, 352. [Google Scholar] [CrossRef]
- Smith, M.P.; Guarnizo, L.E. Global mobility, shifting borders and urban citizenship. J. Econ. Soc. Geogr. 2010, 100, 610–622. [Google Scholar] [CrossRef]
- Bowler, D.E.; Buyung-Ali, L.M.; Knight, T.M.; Pullin, A.S. A systematic review of evidence for the added benefits to health of exposure to natural environments. BMC Public Health 2010, 10, 1–10. [Google Scholar] [CrossRef]
- Maas, J.; Verheij, R.A.; Groenewegen, P.P.; de Vries, S.; Spreeuwenberg, P. Green space, urbanity, and health: How strong is the relation? J. Epidemiol. Community Health 2006, 60, 587–592. [Google Scholar] [CrossRef]

| 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | |
|---|---|---|---|---|---|---|---|---|---|---|
| MMR (1 death/100,000 livebirth) | ||||||||||
| Min. | 7.86 | 6.57 | 5.20 | 3.60 | 1.20 | 1.40 | 1.90 | 1.90 | 1.90 | 2.30 |
| Mean | 39.87 | 32.11 | 28.84 | 25.81 | 22.15 | 20.66 | 19.78 | 17.72 | 17.72 | 16.32 |
| Max. | 265.38 | 233.96 | 232.20 | 174.80 | 180.70 | 176.10 | 154.50 | 108.90 | 108.90 | 100.90 |
| HPR (1 death/100,000 livebirth) | ||||||||||
| Min. | 6.45 | 6.47 | 6.50 | 7.20 | 5.90 | 7.60 | 8.70 | 8.50 | 8.50 | 8.70 |
| Mean | 14.28 | 16.20 | 17.26 | 18.17 | 18.61 | 19.43 | 20.77 | 22.39 | 22.39 | 24.68 |
| Max. | 38.30 | 41.19 | 41.90 | 42.60 | 42.50 | 44.00 | 46.40 | 46.90 | 46.90 | 53.20 |
| Area of Green Space (100 km2) | ||||||||||
| Min. | 0.20 | 0.20 | 0.22 | 0.21 | 0.29 | 0.34 | 0.36 | 0.42 | 0.53 | 0.62 |
| Mean | 5.56 | 5.69 | 6.43 | 6.89 | 7.24 | 7.64 | 7.83 | 8.15 | 8.61 | 8.99 |
| Max. | 27.47 | 37.70 | 40.16 | 42.04 | 41.06 | 40.17 | 41.20 | 42.19 | 43.84 | 45.27 |
| Area of Public Green Space (100 km2) | ||||||||||
| Min. | 0.02 | 0.03 | 0.04 | 0.03 | 0.05 | 0.05 | 0.06 | 0.07 | 0.09 | 0.09 |
| Mean | 1.09 | 1.18 | 1.30 | 1.42 | 1.56 | 1.67 | 1.77 | 1.86 | 1.98 | 2.11 |
| Max. | 4.76 | 5.02 | 5.32 | 5.85 | 6.80 | 7.40 | 7.89 | 8.32 | 8.96 | 9.75 |
| Green Space Coverage Ratio (%) | ||||||||||
| Min. | 24.10 | 25.10 | 27.30 | 16.00 | 24.10 | 30.00 | 18.10 | 30.80 | 29.80 | 31.10 |
| Mean | 34.18 | 35.32 | 36.70 | 36.33 | 37.75 | 38.46 | 38.13 | 39.34 | 39.11 | 39.17 |
| Max. | 42.80 | 42.60 | 47.70 | 46.60 | 46.80 | 46.20 | 47.10 | 49.10 | 48.40 | 48.40 |
| Urbanization rate (%) | ||||||||||
| Min. | 0.21 | 0.22 | 0.22 | 0.23 | 0.23 | 0.23 | 0.24 | 0.26 | 0.28 | 0.30 |
| Mean | 0.47 | 0.48 | 0.49 | 0.51 | 0.52 | 0.53 | 0.54 | 0.56 | 0.57 | 0.58 |
| Max. | 0.89 | 0.89 | 0.89 | 0.89 | 0.89 | 0.89 | 0.90 | 0.90 | 0.88 | 0.88 |
| Health worker (10,000 persons) | ||||||||||
| Min. | 1.02 | 1.17 | 1.60 | 1.67 | 2.22 | 2.16 | 2.47 | 2.65 | 2.91 | 2.92 |
| Mean | 19.06 | 19.90 | 25.10 | 26.44 | 27.76 | 29.38 | 31.55 | 32.98 | 34.46 | 36.01 |
| Max. | 45.21 | 47.98 | 60.21 | 64.59 | 68.96 | 73.89 | 81.93 | 83.85 | 85.57 | 87.41 |
| Year | Maternal Mortality Ratio (MMR) | High-Risk Parturient Ratio (HPR) | ||||
|---|---|---|---|---|---|---|
| Moran’s I | p | Z | Moran’s I | p | Z | |
| 2007 | 0.162 | <0.001 | 3.552 | −0.064 | 0.678 | −0.415 |
| 2010 | 0.130 | <0.001 | 3.166 | 0.027 | 0.939 | 0.007 |
| 2013 | 0.122 | <0.001 | 3.23 | 0.012 | 0.56 | 0.584 |
| 2016 | 0.114 | <0.001 | 3.209 | 0.032 | 0.402 | 0.838 |
| Variables | Pooled OLS | Fixed Effects | Random Effects |
|---|---|---|---|
| HPR | −0.145 | 0.828 *** | 0.516 ** |
| Mediworker | −5.689 | −37.711 *** | −10.38 |
| GDP | 9.020 * | 0.929 | 0.373 |
| PopDen | −5.603 ** | 5.733 | 0.384 |
| GS | 16.021 * | −16.624 * | −4.442 |
| Public GS | −42.580 *** | −60.312 *** | −46.133 *** |
| Gscoverage | −0.774 * | −0.418 * | −0.747 *** |
| Urban R | −66.523 ** | 184.193 *** | −2.629 |
| R2 | 0.618 | 0.579 | 0.502 |
| Adjusted R2 | 0.608 | 0.52 | 0.489 |
| F Statistic | 60.984 *** (df = 8; 301) | 46.595 *** (df = 8; 271) | 303.620 *** |
| Variables | SDM | SLM | SEM | |||
|---|---|---|---|---|---|---|
| Coef. | p | Coef. | p | Coef. | p | |
| HPR | 0.087381 | 0.645 | 0.82245 | <0.001 *** | 0.82801 | <0.001 *** |
| Mediworker | −10.8043 | 0.024 * | −37.9481 | <0.001 *** | −37.4303 | <0.001 *** |
| GDP | −1.91947 | 0.201 | 0.886 | 0.697 | 0.9084 | 0.68903 |
| PopDen | −2.6407 | 0.333 | 5.71223 | 0.179 | 5.66942 | 0.18136 |
| GS | −2.75892 | 0.688 | −16.841 | <0.05 * | −16.891 | <0.05 * |
| Public GS | −10.1467 | 0.362 | −60.0729 | <0.001 *** | −60.4161 | <0.001 *** |
| Gscoverage | −0.26285 | 0.021 * | −0.42238 | <0.05 * | −0.42398 | <0.05 * |
| Urban R | −73.6624 | 0.004 ** | 183.3074 | <0.001 *** | 184.0643 | <0.001 *** |
| 0.955045 | <0.001 *** | |||||
| 0.065648 | 0.3925 | −0.016712 | 0.8125 | |||
| λ | −0.016370 | 0.8378 | ||||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jin, P.; Gao, Y.; Liu, L.; Peng, Z.; Wu, H. Maternal Health and Green Spaces in China: A Longitudinal Analysis of MMR Based on Spatial Panel Model. Healthcare 2019, 7, 154. https://doi.org/10.3390/healthcare7040154
Jin P, Gao Y, Liu L, Peng Z, Wu H. Maternal Health and Green Spaces in China: A Longitudinal Analysis of MMR Based on Spatial Panel Model. Healthcare. 2019; 7(4):154. https://doi.org/10.3390/healthcare7040154
Chicago/Turabian StyleJin, Ping, Yushu Gao, Lingbo Liu, Zhenghong Peng, and Hao Wu. 2019. "Maternal Health and Green Spaces in China: A Longitudinal Analysis of MMR Based on Spatial Panel Model" Healthcare 7, no. 4: 154. https://doi.org/10.3390/healthcare7040154
APA StyleJin, P., Gao, Y., Liu, L., Peng, Z., & Wu, H. (2019). Maternal Health and Green Spaces in China: A Longitudinal Analysis of MMR Based on Spatial Panel Model. Healthcare, 7(4), 154. https://doi.org/10.3390/healthcare7040154







