Interprofessional Education and Collaboration in Healthcare: An Exploratory Study of the Perspectives of Medical Students in the United States
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Survey Design
2.3. Data Collection
2.4. Statistical Analysis
2.5. Ethical Considerations
3. Results
3.1. Demographics
3.2. Attitudes
3.2.1. Attitudes Toward IPE Coursework
3.2.2. Attitudes Toward IPC in Patient Care
3.2.3. Attitudes Toward IPC with Healthcare Team
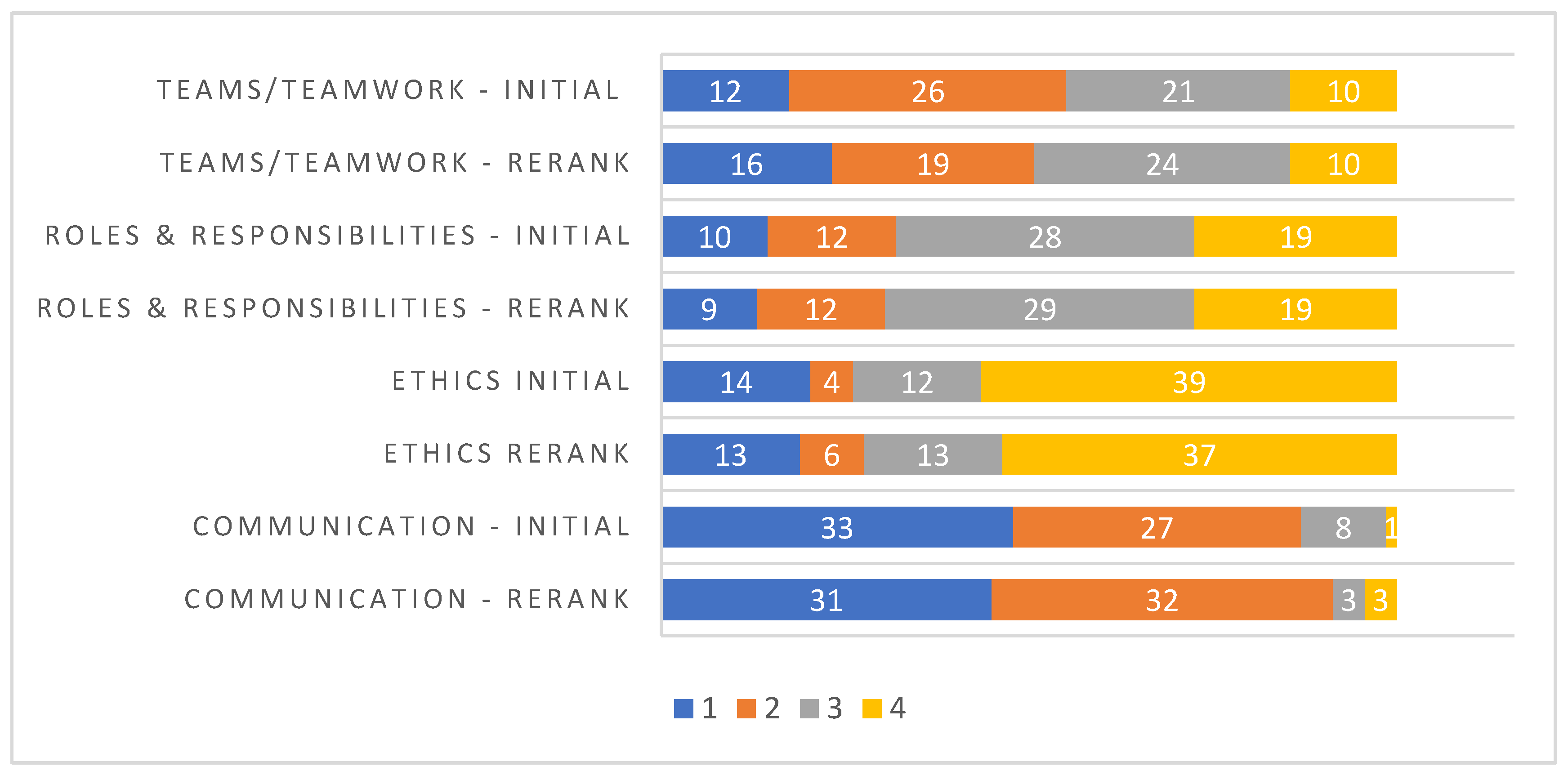
3.3. IPE Definition and Ranking of IPEC Competencies
3.4. Interprofessional Barriers and Opportunities
4. Discussion
Study Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Buring, S.M.; Bhushan, A.; Broeseker, A.; Conway, S.; Duncan-Hewitt, W.; Hansen, L.; Westberg, S. Interprofessional Education: Definitions, Student Competencies, and Guidelines for Implementation. Am. J. Pharm. Educ. 2009, 73, 59. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Framework for Action on Interprofessional Education & Collaborative Practice; WHO/HRH/HPN/10.3; WHO: Geneva, Switzerland, 2010. [Google Scholar]
- Institute of Medicine. Health Professions Education: A Bridge to Quality; National Academies Press: Washington, DC, USA, 2003. [Google Scholar]
- Reeves, S.; Perrier, L.; Goldman, J.; Freeth, D.; Zwarenstein, M. Interprofessional education: Effects on professional practice and healthcare outcomes (update). Cochrane Database Syst. Rev. 2013. [Google Scholar] [CrossRef] [PubMed]
- Wheelan, S.A.; Burchill, C.N.; Tilin, F. The link between teamwork and patients’ outcomes in intensive care units. Am. J. Crit. Care 2003, 12, 527–534. [Google Scholar] [PubMed]
- Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century; National Academy Press: Washington, DC, USA, 2001. [Google Scholar]
- Asmirajanti, M.; Hamid, A.Y.S.; Hariyati, T.S. Clinical care pathway strenghens interprofessional collaboration and quality of health service: A literature review. Enfermería Clínica 2018, 28, 240–244. [Google Scholar] [CrossRef]
- Interprofessional Education Collaborative. Expert Panel Core Competencies for Interprofessional Collaborative Practice: Report of an Expert Panel; Interprofessional Education Collaborative: Washington, DC, USA, 2011. [Google Scholar]
- WHO Study Group on Multiprofessional Education of Health Personnel. Learning Together to Work Together for Health; Report of a WHO Study Group on Multiprofessional Education of Health Personnel: The Team Approach; WHO: Geneva, Switzerland, 1988; Volume 769, pp. 1–72. [Google Scholar]
- Chen, L.; Evans, D.; Evans, T.; Sadana, R.; Stilwell, B.; Travis, P.; Van Lerberghe, W.; Zurn, P. Working Together for Health: The World Health Report 2006; World Health Organization: Geneva, Switzerland, 2006. [Google Scholar]
- Thistlethwaite, J. Interprofessional education: A review of context, learning and the research agenda. Med. Educ. 2012, 46, 58–70. [Google Scholar] [CrossRef]
- Herrmann, G.; Woermann, U.; Schlegel, C. Interprofessional education in anatomy: Learning together in medical and nursing training. Anat. Sci. Educ. 2015, 8, 324–330. [Google Scholar] [CrossRef]
- Kirch, D.G.; Ast, C. Interprofessionalism: Educating to meet patient needs. Anat. Sci. Educ. 2015, 8, 296–298. [Google Scholar] [CrossRef]
- Harden, R.M. Interprofessional education: The magical mystery tour now less of a mystery. Anat. Sci. Educ. 2015, 8, 291–295. [Google Scholar] [CrossRef]
- Association of American Medical Colleges Interprofessional Education. Available online: https://www.aamc.org/initiatives/meded/486536/interprofessionaleducation.html (accessed on 13 September 2018).
- Blue, A.V.; Zoller, J.; Stratton, T.D.; Elam, C.L.; Gilbert, J. Interprofessional education in US medical schools. J. Interprof. Care 2010, 24, 204–206. [Google Scholar] [CrossRef]
- Parsell, G.; Bligh, J. The development of a questionnaire to assess the readiness of health care students for interprofessional learning (RIPLS). Med. Educ. 1999, 33, 95–100. [Google Scholar] [CrossRef]
- Wong, R.L.; Fahs, D.B.; Talwalkar, J.S.; Colson, E.R.; Desai, M.M.; Kayingo, G.; Balanda, M.; Luczak, A.G.; Rosenthal, M.S. A longitudinal study of health professional students’ attitudes towards interprofessional education at an American university. J. Interprof. Care 2016, 30, 191–200. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, M.I.; Chan, S.W.-C.; Wong, L.L.; Tan, M.L.; Liaw, S.Y. Are first-year healthcare undergraduates at an Asian university ready for interprofessional education? J. Interprof. Care 2013, 27, 341–343. [Google Scholar] [CrossRef] [PubMed]
- American Medical Student Association (AMSA). Available online: www.amsa.org (accessed on 23 February 2018).
- Curran, V.R.; Sharpe, D.; Forristall, J. Attitudes of health sciences faculty members towards interprofessional teamwork and education. Med. Educ. 2007, 41, 892–896. [Google Scholar] [CrossRef] [PubMed]
- Vernon, M.M.; Moore, N.M.; Cummins, L.-A.; E Reyes, S.; Mazzoli, A.J.; Heboyan, V.; De Leo, G. Respiratory Therapy Faculty Knowledge of and Attitudes toward Interprofessional Education. Respir. Care 2017, 62, 873–881. [Google Scholar] [CrossRef] [PubMed]
- Patton, Z.; Vernon, M.; Haymond, K.; Anglin, J.; Heboyan, V.; De Leo, G. Evaluation of Interprofessional Education Implementation among Nutrition Program Directors in the United States. Top. Clin. Nutr. 2018, 33, 196–204. [Google Scholar] [CrossRef]
- Ruebling, I.; Pole, D.; Breitbach, A.P.; Frager, A.; Kettenbach, G.; Westhus, N.; Kienstra, K.; Carlson, J. A comparison of student attitudes and perceptions before and after an introductory interprofessional education experience. J. Interprof. Care 2014, 28, 23–27. [Google Scholar] [CrossRef]
- Sytsma, T.T.; Haller, E.P.; Youdas, J.W.; Krause, D.A.; Hellyer, N.J.; Pawlina, W.; Lachman, N. Long-term effect of a short interprofessional education interaction between medical and physical therapy students. Anat. Sci. Educ. 2015, 8, 317–323. [Google Scholar] [CrossRef]
- Hepp, S.L.; Suter, E.; Jackson, K.; Deutschlander, S.; Makwarimba, E.; Jennings, J.; Birmingham, L. Using an interprofessional competency framework to examine collaborative practice. J. Interprof. Care 2015, 29, 131–137. [Google Scholar] [CrossRef]
- Gilbert, J.H. Interprofessional learning and higher education structural barriers. J. Interprof. Care 2005, 19, 87–106. [Google Scholar] [CrossRef]
- Vernon, M.M.; Moore, N.; Mazzoli, A.; De Leo, G. Respiratory therapy faculty perspectives on interprofessional education: Findings from a cross-sectional online survey. J. Interprof. Care 2018, 32, 235–238. [Google Scholar] [CrossRef]
- Groessl, J.M.; Vandenhouten, C.L. Examining Students’ Attitudes and Readiness for Interprofessional Education and Practice. Educ. Res. Int. 2019, 2019, 2153292. [Google Scholar] [CrossRef]
- Pinto, A.; Lee, S.; Lombardo, S.; Salama, M.; Ellis, S.; Kay, T.; Davies, R.; Landry, M.D. The Impact of Structured Inter-professional Education on Health Care Professional Students’ Perceptions of Collaboration in a Clinical Setting. Physiother. Can. 2012, 64, 145–156. [Google Scholar] [CrossRef] [PubMed]
- Visser, C.L.F.; Kusurkar, R.A.; Croiset, G.; Ten Cate, O.; Westerveld, H.E. Students’ motivation for interprofessional collaboration after their experience on an IPE ward: A qualitative analysis framed by self-determination theory. Med. Teach. 2019, 41, 44–52. [Google Scholar] [CrossRef] [PubMed]

| Variable | n = 69 | % |
|---|---|---|
| Gender | ||
| Males | 42 | 61 |
| Females | 27 | 39 |
| Age in Years | ||
| >20 | 1 | 1.4 |
| 20–29 | 59 | 85.5 |
| 30–39 | 9 | 13 |
| Ethnic Background | ||
| White, non-Hispanic | 48 | 69.6 |
| Black, non-Hispanic | 7 | 10.1 |
| Hispanic | 5 | 7.2 |
| Asian/non-Pacific Islander, non-Hispanic | 7 | 10.1 |
| Multiple races | 2 | 2.9 |
| Year in medical school | ||
| Year 1 | 17 | 24.6 |
| Year 2 | 15 | 21.7 |
| Year 3 | 22 | 31.9 |
| Year 4 | 15 | 21.7 |
| (a) | |||||
| Strongly Agree | Agree | Neither | Disagree | Strongly Disagree | |
| n (%) | n (%) | n (%) | n (%) | n (%) | |
| I am interested in coursework with other disciplines because it is important for interprofessional collaboration | 31 (44.9) | 26 (37.7) | 7 (10.1) | 4 (5.8) | 1 (1.4) |
| I am interested in attending coursework that includes nurse practitioners and physician assistant students | 27 (39.1) | 26 (37.7) | 8 (11.6) | 6 (8.7) | 2 (2.9) |
| I am interested in attending coursework that includes nursing students (not nurse practitioners) | 26 (37.7) | 35 (50.7) | 1 (1.4) | 4 (5.8) | 3 (4.3) |
| I am interested in attending coursework that includes allied health professional students | 25 (36.2) | 32 (46.4) | 7 (10.1) | 3 (4.3) | 2 (2.9) |
| Interprofessional education helps students think positively about other healthcare professionals | 35 (50.7) | 22 (31.9) | 9 (13) | 2 (2.9) | 1 (1.4) |
| Medical students would benefit from working on group projects with students from other health care professions | 31 (44.9) | 22 (31.9) | 9 (13) | 4 (5.8) | 3 (4.3) |
| IPE with other disciplines improves interprofessional communication | 38 (55.1) | 24 (34.8) | 6 (8.7) | 1 (1.4) | 0 (0) |
| Integrated learning with students in other disciplines helps students to become more effective members of the healthcare team | 31 (44.9) | 27 (39.1) | 6 (8.7) | 3 (4.3) | 2 (2.9) |
| Clinical problem solving can only be learned effectively when students are taught within their individual department/ school | 10 (14.5) | 8 (11.6) | 15 (21.7) | 27 (39.1) | 9 (13) |
| Interprofessional learning among healthcare students will increase their ability to understand clinical problems | 3 (4.3) | 12 (17.4) | 29 (42) | 25 (36.2) | 0 (0) |
| Interprofessional learning will help students to understand their own professional limitations | 28 (40.6) | 38 (55.1) | 3 (4.3) | 0 (0) | 0 (0) |
| (b) | |||||
| Strongly Agree | Agree | Neither | Disagree | Strongly Disagree | |
| n (%) | n (%) | n (%) | n (%) | n (%) | |
| Interprofessional collaboration increases the healthcare team’s ability to understand clinical problems | 32 (46.4) | 28 (40.6) | 6 (8.7) | 2 (2.9) | 1 (1.4) |
| Patients receiving interprofessional care are more likely than others to be treated as a whole person | 38 (55.1) | 18 (26.1) | 11 (15.9) | 2 (2.9) | 0 (0) |
| The interprofessional approach makes the delivery of patient care more efficient | 36 (52.2) | 22 (31.9) | 10 (14.5) | 1 (1.4) | 0 (0) |
| Patients would ultimately benefit if health care professionals worked together to solve patient problems | 46 (66.7) | 20 (29) | 3 (4.3) | 0 (0) | 0 (0) |
| The ‘give and take’ among team members helps providers make better patient care decisions | 28 (40.6) | 32 (46.4) | 7 (10.1) | 2 (2.9) | 0 (0) |
| Reporting observations to a multi-disciplinary team helps team members better understand the role of other healthcare professionals | 32 (46.4) | 32 (46.4) | 4 (5.8) | 1 (1.4) | 0 (0) |
| (c) | |||||
| Strongly Agree | Agree | Neither | Disagree | Strongly Disagree | |
| n (%) | n (%) | n (%) | n (%) | n (%) | |
| Interprofessional collaboration helps healthcare professionals think positively about the healthcare team | 28 (40.6) | 29 (42) | 9 (13) | 2 (2.9) | 1 (1.4) |
| Communication skills are critical for the healthcare team for improved patient outcomes | 57 (82.6) | 12 (17.4) | 0 (0) | 0 (0) | 0 (0) |
| Interprofessional collaboration allows healthcare professionals to understand their role limitations | 27 (39.1) | 36 (52.2) | 5 (7.2) | 1 (1.4) | 0 (0) |
| For interprofessional collaboration to be effective, the healthcare team needs to trust and respect each other | 47 (68.1) | 20 (29) | 1 (1.4) | 1 (1.4) | 0 (0) |
| Team meetings foster communication among members from different professionals or disciplines | 38 (55.1) | 22 (31.9) | 6 (8.7) | 3 (4.3) | 0 (0) |
| Working in an interprofessional environment keeps health professionals enthusiastic and interested in their jobs | 22 (31.9) | 20 (29) | 19 (27.5) | 5 (7.2) | 3 (4.3) |
| Working in an interprofessional manner requires additional time | 20 (29) | 16 (23.2) | 19 (27.5) | 14 (20.3) | 0 (0) |
| For interprofessional collaboration to be effective, members of the healthcare team must work within their scope of practice | 26 (37.7) | 23 (33.3) | 14 (20.3) | 6 (8.7) | 0 (0) |
| Training to work on interprofessional teams is critical to the future of medicine | 35 (50.7) | 25 (36.2) | 8 (11.6) | 1 (1.4) | 0 (0) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zechariah, S.; Ansa, B.E.; Johnson, S.W.; Gates, A.M.; Leo, G.D. Interprofessional Education and Collaboration in Healthcare: An Exploratory Study of the Perspectives of Medical Students in the United States. Healthcare 2019, 7, 117. https://doi.org/10.3390/healthcare7040117
Zechariah S, Ansa BE, Johnson SW, Gates AM, Leo GD. Interprofessional Education and Collaboration in Healthcare: An Exploratory Study of the Perspectives of Medical Students in the United States. Healthcare. 2019; 7(4):117. https://doi.org/10.3390/healthcare7040117
Chicago/Turabian StyleZechariah, Sunitha, Benjamin E. Ansa, Stephanie W. Johnson, Amy M. Gates, and Gianluca De Leo. 2019. "Interprofessional Education and Collaboration in Healthcare: An Exploratory Study of the Perspectives of Medical Students in the United States" Healthcare 7, no. 4: 117. https://doi.org/10.3390/healthcare7040117
APA StyleZechariah, S., Ansa, B. E., Johnson, S. W., Gates, A. M., & Leo, G. D. (2019). Interprofessional Education and Collaboration in Healthcare: An Exploratory Study of the Perspectives of Medical Students in the United States. Healthcare, 7(4), 117. https://doi.org/10.3390/healthcare7040117






