Rates and Associated Factors of Secondary Mental Health Care Utilisation among Ex-Military Personnel in the United States: A Narrative Review
Abstract
1. Introduction
1.1. Background
1.2. Objectives
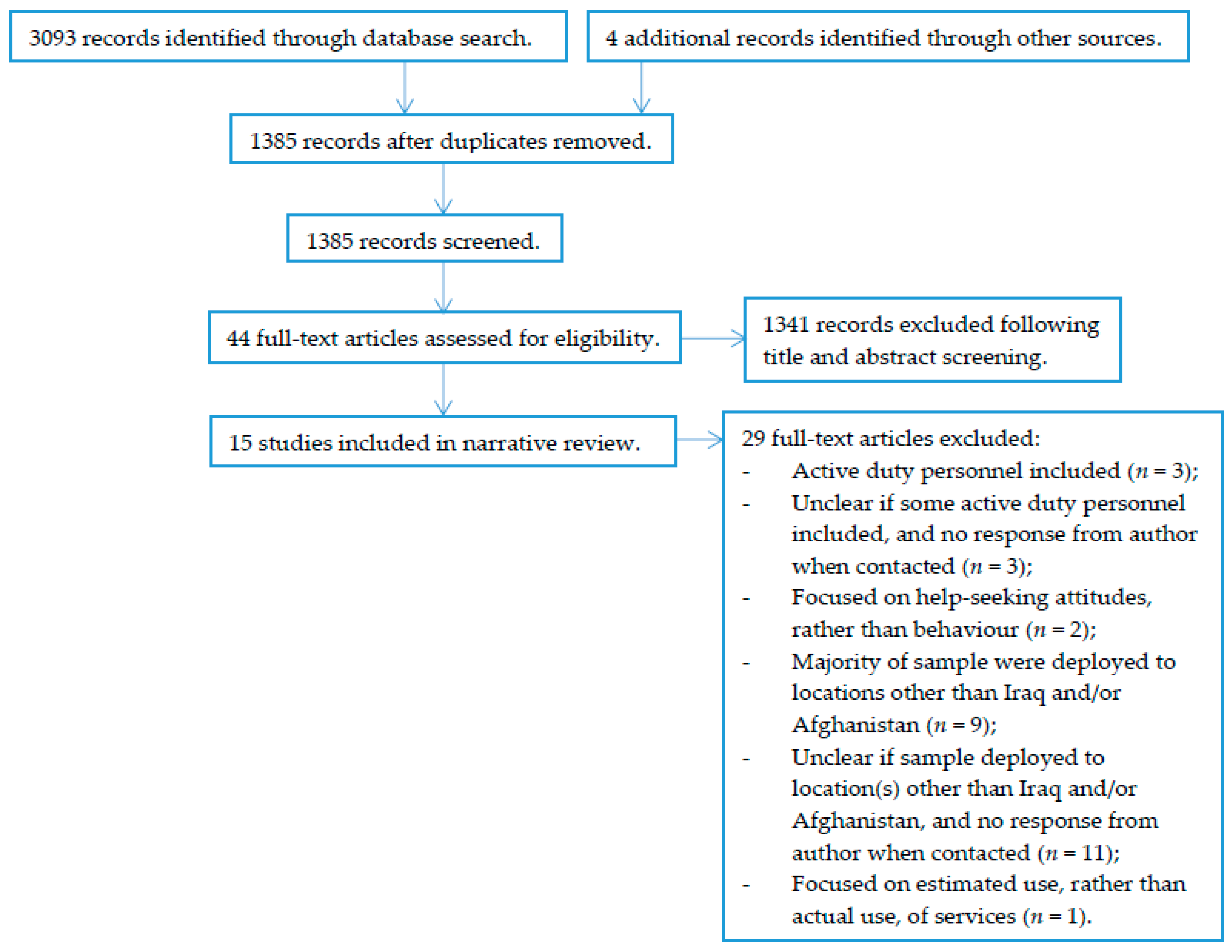
2. Materials and Methods
2.1. Search Strategy
2.2. Eligibility Criteria
3. Results
3.1. Study Characteristics
3.2. Measures
3.3. Rates of Mental Health Care Utilisation
3.4. Associated Factors
4. Discussion
4.1. Key Findings
4.2. Comparison to Previous Research
4.3. Associated Factors
4.4. Strengths and Limitations
4.5. Implications and Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- United States Department of Veterans Affairs. National Center for Veterans Analysis and Statistics. 2017. Available online: https://www.va.gov/vetdata/veteran_population.asp (accessed on 21 August 2018).
- Eisen, S.V.; Schultz, M.R.; Vogt, D.; Glickman, M.E.; Elwy, A.R.; Drainoni, M.L.; Osei-Bonsu, P.E.; Martin, J. Mental and physical health status and alcohol and drug use following return from deployment to Iraq or Afghanistan. Am. J. Public Health 2012, 102, 66–73. [Google Scholar] [CrossRef] [PubMed]
- Hoge, C.W.; Auchterlonie, J.L.; Milliken, C.S. Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Aghanistan. JAMA 2006, 295, 1023–1032. [Google Scholar] [CrossRef] [PubMed]
- Kang, H.K.; Hyams, K.C. Mental health care needs among recent war veterans. N. Engl. J. Med. 2005, 352, 1289. [Google Scholar] [CrossRef] [PubMed]
- Hoge, C.W.; Castro, C.A.; Messer, S.C.; McGurk, D.; Cotting, D.I.; Koffman, R.L. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N. Engl. J. Med. 2004, 351, 13–22. [Google Scholar] [CrossRef] [PubMed]
- Hom, M.A.; Stanley, I.H.; Schneider, M.E.; Joiner, T.E., Jr. A systematic review of help-seeking and mental health service utilization among military service members. Clin. Psychol. Rev. 2017, 53, 59–78. [Google Scholar] [CrossRef] [PubMed]
- Stevelink, S.A.M.; Jones, M.; Hull, L.; Pernet, D.; MacCrimmon, S.; Goodwin, L.; MacManus, D.; Murphy, D.; Jones, N.; Greenberg, N.; et al. Mental health outcomes at the end of the British involvement in the Iraq and Afghanistan conflicts: a cohort study. Br. J. Psychiatry 2018, 213, 690–697. [Google Scholar] [CrossRef]
- Iversen, A.C.; van Staden, L.; Hughes, J.H.; Greenberg, N.; Hotopf, M.; Rona, R.J.; Thonicraft, G.; Wessely, S.; Fear, N.T. The stigma of mental health problems and other barriers to care in the UK Armed Forces. BMC Health Serv. Res. 2011, 11, 31. [Google Scholar] [CrossRef]
- Jones, N.; Twardzicki, M.; Fertout, M.; Jackson, T.; Greenberg, N. Mental health, stigmatising beliefs, barriers to care and help-seeking in a non-deployed sample of UK Army Personnel. J. Psychol. Psychother. 2013, 3, 129. [Google Scholar] [CrossRef]
- Sharp, M.L.; Fear, N.T.; Rona, R.J.; Wessely, S.; Greenberg, N.; Jones, N.; Goodwin, L. Stigma as a barrier to seeking health care among military personnel with mental health problems. Epidemiol. Rev. 2015, 37, 144–162. [Google Scholar] [CrossRef]
- Rafferty, L.; Stevelink, S.; Greenberg, N.; Wessely, S. Stigma and Barriers to Care in Service Leavers with Mental Health Problems. Available online: https://www.fim-trust.org/wp-content/uploads/2017/11/20171102-FinalReport.pdf (accessed on 25 March 2018).
- Johnson, E.M.; Barrie, K.A.; Possemato, K.; Wade, M.; Eaker, A.; Ouimette, P.C. Predictors of mental health care utilization in veterans with post-traumatic stress disorder symptoms and hazardous drinking. Mil. Med. 2016, 181, 1200–1206. [Google Scholar] [CrossRef]
- Whealin, J.M.; Pietrzak, R.H.; Shore, J.; Vogt, D.; Shore, J.; Morland, L.; Southwick, S.M. Deployment-related sequalae and treatment utilization in rural and urban war veterans in Hawaii. Psychol. Serv. 2014, 11, 114–123. [Google Scholar] [CrossRef] [PubMed]
- United States Department of Veterans Affairs. Veterans Health Administration. Available online: https://www.va.gov/health/ (accessed on 10 October 2018).
- Blais, R.K.; Hoerster, K.D.; Malte, C. Unique PTSD clusters predict intention to seek mental health care and subsequent utilization in US veterans with PTSD symptoms. J. Trauma. Stress 2014, 27, 168–174. [Google Scholar] [CrossRef] [PubMed]
- DeViva, J.C. Treatment utilization among OEF/OIF veterans referred for psychotherapy for PTSD. Psychol. Serv. 2014, 11, 179–184. [Google Scholar] [CrossRef] [PubMed]
- DeViva, J.C.; Sheerin, C.M.; Southwick, S.M.; Roy, A.M.; Pietrzak, R.H.; Harpaz-Rotem, I. Correlates of VA mental health treatment utilization among OEF/OIF/OND veterans: Resilience, stigma, social support, personality, and beliefs about treatment. Psychol. Trauma Theory Res. Pract. Policy 2016, 8, 310–318. [Google Scholar] [CrossRef] [PubMed]
- Harpaz-Rotem, I.; Rosenheck, R.A.; Pietrzak, R.H.; Southwick, S.M. Determinants of prospective engagement in mental health treatment among symptomatic Iraq/Afghanistan veterans. J. Nerv. Ment. Dis. 2014, 202, 97–104. [Google Scholar] [CrossRef] [PubMed]
- Hearne, C.R.M. Predictors of operation enduring freedom/operation Iraqi freedom veterans’ engagement in mental health treatment. Mil. Med. 2013, 178, 1183–1187. [Google Scholar] [CrossRef] [PubMed]
- Hoerster, K.D.; Malte, C.A.; Imel, Z.E.; Ahmad, Z.; Hunt, S.C.; Jakupcak, M. Association of perceived barriers with prospective use of VA mental health care among Iraq and Afghanistan veterans. Psychiatr. Serv. 2012, 63, 380–382. [Google Scholar] [CrossRef] [PubMed]
- Hudson, T.J.; Fortney, J.C.; Williams, J.S.; Austen, M.A.; Pope, S.K.; Hayes, C.J. Effect of rural residence on use of VHA mental health care among OEF/OIF veterans. Psychiatr. Serv. 2014, 65, 1420–1425. [Google Scholar] [CrossRef]
- Kaier, E.; Possemato, K.; Lantinga, L.J. Associations between PTSD and healthcare utilization among OEF/OIF veterans with hazardous alcohol use. Traumatology 2014, 20, 142–149. [Google Scholar] [CrossRef]
- Koo, K.H.; Madden, E.; Maguen, S. Race-ethnicity and gender differences in VA health care service utilization among U.S. veterans of recent conflicts. Psychiatr. Serv. 2015, 66, 507–513. [Google Scholar] [CrossRef]
- Maguen, S.; Cohen, B.; Cohen, G.; Madden, E.; Bertenthal, D.; Seal, K. Gender differences in health service utilization among Iraq and Afghanistan veterans with posttraumatic stress disorder. J. Women’s Health 2012, 21, 666–673. [Google Scholar] [CrossRef] [PubMed]
- McGinn, M.M.; Hoerster, K.D.; Stryczek, K.C.; Malte, C.A.; Jakupcak, M. Relationship satisfaction, PTSD symptom severity, and mental healthcare utilization among OEF/OIF veterans. J. Fam. Psychol. 2017, 31, 111–116. [Google Scholar] [CrossRef] [PubMed]
- Naragon-Gainey, K.; Hoerster, K.D.; Malte, C.A.; Jakupcak, M. Distress symptoms and high-risk behaviors prospectively associated with treatment among returning veterans. Psychiatr. Serv. 2012, 12, 942–944. [Google Scholar] [CrossRef] [PubMed]
- Kehle-Forbes, S.M.; Meis, L.A.; Spoont, M.R. Treatment initiation and dropout from prolonged exposure and cognitive processing therapy in a VA outpatient clinic. Psychol. Trauma Theory Res. Pract. Policy 2016, 8, 107–114. [Google Scholar] [CrossRef] [PubMed]
- Keller, S.M.; Tuerk, P.W. Evidence-based psychotherapy (EBP) non-initiation among veterans offered an EBP for posttraumatic stress disorder. Psychol. Serv. 2016, 13, 42–48. [Google Scholar] [CrossRef] [PubMed]
- Kessler, R.; Demler, O.; Frank, R.G.; Olfson, M.; Pincus, H.A.; Walters, E.E.; Wang, P.; Wells, K.B.; Zaslavsky, A.M. Prevalence and treatment of metal disorders, 1990 to 2003. N. Engl. J. Med. 2005, 352, 2515–2523. [Google Scholar] [CrossRef] [PubMed]
- Thornicroft, G. Most people with mental illness are not treated. Lancet 2007, 370, 807–808. [Google Scholar] [CrossRef]
- Wittchen, H.; Jacobi, F. Size and burden of mental disorders in Europe: A critical review and appraisal of 27 studies. Eur. Neuropsychopharmacol. 2005, 15, 357–376. [Google Scholar] [CrossRef] [PubMed]
- Iversen, A.C.; Van Staden, L.; Hughes, J.H.; Browne, T.; Greenberg, N.; Hotopf, M.; Rona, R.J.; Wessely, S.; Thornicroft, G.; Fear, N.T. Help-seeking and receipt of treatment among UK service personnel. Br. J. Psychiatry 2010, 197, 149–155. [Google Scholar] [CrossRef]
- Kehle, S.M.; Polusny, M.A.; Murdoch, M.; Erbes, C.R.; Arbisi, P.A.; Thuras, P.; Meis, L.A. Early mental health treatment-seeking among US national guard soldiers deployed to Iraq. J. Trauma. Stress 2010, 23, 23–40. [Google Scholar]
- Held, P.; Owens, G.P. Stigmas and attitudes toward seeking mental health treatment in a sample of veterans and active duty service members. Traumatology 2012, 19, 136–143. [Google Scholar] [CrossRef]
- Elbogen, E.B.; Wagner, H.R.; Johnson, P.; Kinneer, P.; Kang, H.; Vasterling, J.J.; Timko, C.; Beckham, J.C. Are Iraq and Afghanistan veterans using mental health services? New data from a national random-sample survey. Psychiatr. Serv. 2013, 64, 134–141. [Google Scholar] [CrossRef] [PubMed]
- Di Leone, B.A.; Vogt, D.; Gradus, J.L.; Street, A.E.; Giasson, H.L.; Resick, P.A. Predictors of mental health care use among male and female veterans deployed in support of the wars in Afghanistan and Iraq. Psychol. Serv. 2013, 10, 145–151. [Google Scholar] [CrossRef] [PubMed]
- Fikretoglu, D.; Elhai, J.D.; Liu, A.; Richardson, J.D.; Pedlar, D.J. Predictors of likelihood and intensity of past-year mental health service use in an active Canadian military sample. Psychiatr. Serv. 2009, 60, 358–366. [Google Scholar] [CrossRef] [PubMed]
- Brown, M.C.; Creel, A.H.; Engel, C.C.; Herrell, R.K.; Hoge, C.W. Factors associated with interest in receiving help for mental health problems in combat veterans returning from deployment to Iraq. J. Nerv. Ment. Dis. 2011, 199, 797–801. [Google Scholar] [CrossRef] [PubMed]
- Possemato, K.; Wade, M.; Andersen, J.; Ouimette, P. The impact of PTSD, depression, and substance use disorders on disease burden and health care utilization among OEF/OIF veterans. Psychol. Trauma Theory Res. Pract. Policy 2010, 2, 218–223. [Google Scholar] [CrossRef]
- Hines, L.A.; Goodwin, L.; Jones, M.; Hull, L.; Wessely, S.; Fear, N.T.; Rona, R.J. Factors affecting help seeking for mental health problems after deployment to Iraq and Afghanistan. Psychiatr. Serv. 2014, 65, 98–105. [Google Scholar] [CrossRef]
- Seal, K.H.; Maguen, S.; Cohen, B.; Gima, K.S.; Metzler, T.J.; Ren, L.; Bertenthal, D.; Marmar, C.R. VA mental health services utilization in Iraq and Afghanistan veterans in the first year of receiving new mental health diagnoses. J. Trauma. Stress 2010, 23, 5–16. [Google Scholar] [CrossRef]
- Lu, M.W.; Carlson, K.F.; Duckart, J.P.; Dobscha, S.K. The effects of age on initiation of mental health treatment after positive PTSD screen among Veterans Affairs primary care patients. Gen. Hosp. Psychiatry 2012, 34, 654–659. [Google Scholar] [CrossRef]
- Durai, U.N.; Chopra, M.P.; Coakley, E.; Llorente, M.D.; Kirchner, J.E.; Cook, J.M.; Levkoff, S.E. Exposure to trauma and posttraumatic stress disorder symptoms in older veterans attending primary care: Comorbid conditions and self-rated health status. J. Am. Geriatr. Soc. 2011, 59, 1087–1092. [Google Scholar] [CrossRef]
- Stewart, R. The big case register. Acta Psychiatr. Scand. 2014, 130, 83–86. [Google Scholar] [CrossRef] [PubMed]
- Collen, M.F. Clinical research databases: A historical review. J. Med. Syst. 1990, 14, 323–344. [Google Scholar] [CrossRef] [PubMed]
- Mark, K.M.; Pernet, D.; Murphy, D.; Stevelink, S.A.M.; Fear, N.T. Identifying veterans using electronic health records in the United Kingdom: A feasibility study. Unpublished work. 2019. [Google Scholar]
- Wu, C.Y.; Chang, C.K.; Hayes, R.D.; Broadbent, M.; Hotopf, M.; Stewart, R. Clinical risk assessment rating and all-cause mortality in secondary mental healthcare: The South London and Maudsley NHS foundation trust biomedical research centre (SLaM BRC) case register. Psychol. Med. 2012, 42, 1581–1590. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, A.C.; Cloete, D.; Broadbent, M.T.; Hayes, R.D.; Chang, C.-K.; Jackson, R.G.; Roberts, A.; Tsang, J.; Soncul, M.; Liebscher, J.; et al. Development and evaluation of a de-identification procedure for a case register sourced from mental health electronic records. BMC Med. Inform. Decis. Mak. 2013, 13, 71. [Google Scholar] [CrossRef] [PubMed]
| Reference | N | Sample | Outcomes | Time Frame for Outcomes |
|---|---|---|---|---|
| Samples deployed to Afghanistan/Iraq only | ||||
| Blais et al. [15] | 173 | Ex-serving personnel with PTSD, enrolled in a VA post-deployment clinic for an initial evaluation. | Yes/No for attendance of two or more outpatient mental health care visits, for individual psychotherapy, group psychotherapy, and psychiatric visits. Number of outpatient mental health care visits, for individual psychotherapy, group psychotherapy, and psychiatric visits. | 12 months, following initial assessment at clinic. |
| DeViva [16] | 200 | Ex-serving personnel with PTSD, referred to a PTSD specialist at one specific VA outpatient clinic. | Yes/No for attendance of outpatient mental health care visits, for psychotherapy sessions only. Number of outpatient mental health care visits, for psychotherapy sessions only. Number of days from referral to first scheduled outpatient visit. | No time frame specified. |
| DeViva et al. [17] | 97 | Ex-serving personnel with PTSD, referred to mental health services at one specific VA outpatient clinic. | Yes/No for attendance of outpatient mental health care visits, for psychotherapy sessions only. Yes/No for prescription of medication. Number of outpatient mental health care visits, for psychotherapy sessions only. | Six months, following referral to clinic. |
| Harpaz-Rotem et al. [18] | 137 | Ex-serving personnel, assessed at an initial scheduled screening appointment at one specific VA outpatient clinic. | Yes/No for attendance of outpatient mental health care visits. Number of outpatient mental health care visits. | 12 months, following initial assessment at clinic. |
| Hearne [19] | 429 | Ex-serving personnel with any DSM axis 1 disorder, enrolled in a VA post-deployment clinic for an initial evaluation. | Yes/No for attendance of outpatient mental health care visits. | 12 months, following initial assessment at clinic. |
| Hoerster et al. [20] | 305 | Ex-serving personnel with depression, PTSD, or alcohol misuse, enrolled in a VA post-deployment clinic for an initial evaluation. | Yes/No for attendance of nine or more outpatient mental health care visits, in line with minimally adequate treatment. Number of outpatient mental health care visits (including any in primary care VA settings). | 12 months, following initial assessment at clinic. |
| Hudson et al. [21] | 4782 | Ex-serving personnel assessed at an initial scheduled appointment at a VA outpatient clinic. | Yes/No for attendance of outpatient mental health care visits, for psychotherapy sessions only. Yes/No for prescription of medication. | Three months, following initial assessment at clinic. |
| Kaier et al. [22] | 124 | Ex-serving personnel with PTSD or alcohol misuse, referred to study by primary care provider or VA case management team. | Yes/No for attendance of outpatient mental health care visits. Yes/No for prescription of medication. Number of outpatient mental health care visits. Number of days taking medication. | Six months, prior to referral to study. |
| Koo et al. [23] | 309,050 | Ex-serving personnel with PTSD, depression, anxiety, adjustment disorders, or alcohol or drug disorders, entered into VA care. | Yes/No for attendance of outpatient mental health care visits, and psychiatric inpatient stays. Number of outpatient mental health care visits, and psychiatric inpatient stays. | 12 months, following initial assessment at clinic. |
| Maguen et al. [24] | 159,705 | Ex-serving personnel with PTSD, assessed at an initial scheduled appointment at a VA outpatient clinic. | Yes/No for attendance of outpatient mental health care visits, and psychiatric inpatient stays. Number of outpatient mental health care visits, and psychiatric inpatient stays. | 12 months, following initial assessment at clinic. |
| McGinn et al. [25] | 130 | Ex-serving personnel in a committed relationship, enrolled in a VA post-deployment clinic for an initial evaluation. | Yes/No for attendance of mental health care visits, for outpatient psychiatric, and psychotherapy sessions (including any in primary care VA settings). Number of mental health care visits, for outpatient psychiatric, and psychotherapy sessions (including any in primary care VA settings). | 12 months, following initial assessment at clinic. |
| Naragon-Gainey et al. [26] | 618 | Ex-serving personnel, assessed at an initial scheduled appointment at a VA outpatient clinic. | Number of mental health care visits, for mental health with primary health care visits, outpatient mental health care visits, and psychiatric inpatient stays. | 24 months, following initial assessment at clinic. |
| Whealin et al. [13] | 233 | Ex-serving personnel from Hawaii, identified through an Iraq/Afghanistan era ex-serving program roster. | Yes/No for attendance of mental health care visits, for VA psychotherapy sessions, VA mental health care visits, and community mental health care visits. Yes/No for VA prescription of medication. | Three months, prior to entry into study. |
| Samples deployed to Afghanistan/Iraq, as well as to other locations | ||||
| Kehle-Forbes et al. [27] | 427 | Ex-serving personnel with PTSD, referred to, attended an initial assessment at, and put forward for further treatment at one specific VA outpatient clinic. | Yes/No for attendance of outpatient mental health care visits. Number of outpatient mental health care visits. | 36 months, following referral to clinic. |
| Keller & Tuerk [28] | 324 | Ex-serving personnel with PTSD, assessed at an initial intake evaluation in one specific VA outpatient clinic, offered psychotherapy, and assigned a therapist to begin. | Yes/No for attendance of outpatient mental health care visits, for evidence-based PTSD treatment. | 8 months, following assessment at clinic. |
| Classification | Outpatient MH Care Visits | Inpatient Psychiatric Hospital Stays | MH Medication Use | |||
|---|---|---|---|---|---|---|
| Reference | Rate (%) /Number | Reference | Rate (%) /Number | Reference | Rate (%) /Number | |
| Dichotomous MH care outcome | (1) | (2) | (3) | |||
| Blais et al. [15] | 90% * | Koo et al. [23] | 13% | DeViva et al. [17] | 32% | |
| DeViva [16] | 62% | Maguen et al. [24] | 12% | Hudson et al. [19] | 77% | |
| DeViva et al. [17] | 33% | Kaier et al. [20] | 50% | |||
| Harpaz-Rotem et al. [18] | 73% | Whealin et al. [13] | 15% | |||
| Hearne [19] | 53% | |||||
| Hoerster et al. [20] | 25% * | |||||
| Hudson et al. [21] | 52% | |||||
| Kaier et al. [22] | 68% | |||||
| Kehle-Forbes et al. [27] | 82% | |||||
| Keller & Tuerk [28] | 72% | |||||
| Koo et al. [23] | 93% | |||||
| Maguen et al. [24] | 96% | |||||
| McGinn et al. [25] | 50% * | |||||
| Whealin et al. [13] | 36% | |||||
| Overall mean rate | 63.2% | 12.5% | 43.5% | |||
| Continuous MH care outcome | (4) | (5) | (6) | |||
| Blais et al. [15] | 8.6 | Koo et al. [23] | 0 | Kaier et al. [22] | 247 * | |
| DeViva [16] | 7.0 | Maguen et al. [24] | 0.1 | |||
| DeViva et al. [17] | 9.5 | Naragon-Gainey et al. [26] | 0.1 | |||
| Harpaz-Rotem et al. [18] | 14.7 * | |||||
| Hoerster et al. [20] | 7.5 | |||||
| Kaier et al. [22] | 7.8 | |||||
| Kehle-Forbes et al. [27] | 8.9 | |||||
| Koo et al. [23] | 2.2 | |||||
| Maguen et al. [24] | 6.4 | |||||
| McGinn et al. [25] | 6.6 | |||||
| Naragon-Gainey et al. [26] | 7.6 | |||||
| Overall mean rate (SD) | 7.9 (12.7) | 0.1 (0.4) | 247 (188) | |||
| Associated Factors | Significant Positive Associations | Non-Significant Associations | Significant Negative Associations |
|---|---|---|---|
| Mental health factors | |||
| PTSD severity | DeViva et al. [17] 1 Harpaz-Rotem et al. [18] 1 Hoerster et al. [20] 1 McGinn et al. [25] 4 Naragon-Gainey et al. [26] 4,5 Whealin et al. [13] 1 | Kehle-Forbes et al. [27] 1 Keller & Tuerk [28] 1 | |
| Avoidance cluster | Harpaz-Rotem et al. [18] 1 Kaier et al. [22] 4,6 | Blais et al. [15] 4 | |
| Dysphoria cluster | Blais et al. [15] 4 | ||
| Hyperarousal cluster | Blais et al. [15] 4 Harpaz-Rotem et al. [18] 1 Kaier et al. [22] 4,6 | ||
| Numbing cluster | Harpaz Rotem et al. [18] 1 | ||
| Re-experiencing cluster | Blais et al. [15] 4 Harpaz-Rotem et al. [18] 1 Kaier et al. [22] 4,6 | ||
| Depression | Hoerster et al. [20] 1 Maguen et al. [24] 4,5 | Harpaz-Rotem et al. [18] 1,4 Kaier et al. [22] 4,6 Naragon-Gainey et al. [26] 4,5 | DeViva [16] 1 |
| Substance use disorder | DeViva [16] 1 Hearne [19] 1 | ||
| Alcohol use disorder | Maguen et al. [24] 4,5 | Hearne [19] 1 Kaier et al. [22] 4,6 Naragon-Gainey et al. [26] 4 Whealin et al. [13] 1 | |
| Traumatic brain injury | DeViva [16] 1 Whealin et al. [13] 1 | ||
| Comorbidity | Hearne [19] 1 Maguen et al. [24] 4,5 | ||
| Distress | Kaier et al. [22] 4,6 | ||
| Aggression | Naragon-Gainey et al. [26] 4 | ||
| Panic | Naragon-Gainey et al. [26] 4 | ||
| Associated Factors | Significant Positive Associations | Non-Significant Associations | Significant Negative Associations |
|---|---|---|---|
| Sociodemographic factors | |||
| Female gender | Blais et al. [15] 4 Hoerster et al. [20] 1 | DeViva [16] 1 Hearne [19] 1 Hudson et al. [21] 1,3 Kehle-Forbes et al. [27] 1 Keller & Tuerk [28] 1 Maguen et al. [24] 5 Whealin et al. [13] 1 | |
| White ethnicity | Blais et al. [15] 4 | DeViva [16] 1 Hearne [19] 1 Hudson et al. [21] 1,3 Keller & Tuerk [28] 1 Whealin et al. [13] 1 | Koo et al. [23] 1,2 |
| Older age | DeViva [16] 1 Kehle-Forbes et al. [27] 1 Keller & Tuerk [28] 1 | Hearne [19] 1 Hudson et al. [21] 1,3 Whealin et al. [13] 1 | |
| Married status | DeViva [16] 1 | Whealin et al. [13] 1 | |
| Employed status | DeViva [16] 1 | ||
| Non-student status | DeViva [16] 1 | ||
| Higher education level | Whealin et al. [13] 1 | Harpaz-Rotem et al. [18] 4 | |
| Urban living location | Hudson et al. [21] 1 Whealin et al. [13] 1 | ||
| Being a parent | Kaier et al. [22] 4,6 | ||
| Higher annual income | McGinn et al. [25] 4 | ||
| Military factors | |||
| Combat exposure | Blais et al. [15] 4 | Harpaz-Rotem et al. [18] 1 | |
| Number of traumas experienced | Hearne [19] 1 | ||
| Military status (regular vs reserve) | Blais et al. [15] 4 DeViva [16] 4 | ||
| Branch of service | Hoerster et al. [20] 1 | ||
| Time since last deployment | Hearne [19] 1 | DeViva [16] 1 | |
| Number of deployments | DeViva [16] 1 | ||
| Service connection | Hudson et al. [21] 1,3 | ||
| Unit social support | Harpaz-Rotem et al. [18] 1 | ||
| Post-deployment social support | DeViva et al. [17] 1 Harpaz-Rotem et al. [18] 1 | ||
| Combat era | Keller & Tuerk [28] 1 | ||
| Fear of losing military-based vigilance | Harpaz-Rotem et al. [18] 1 | ||
| Personality factors | |||
| Personality | DeViva et al. [16] 1 | ||
| Resilience | DeViva et al. [17] 1 Harpaz-Rotem et al. [18] 1,4 | ||
| Associated Factors | Significant Positive Associations | Non-Significant Associations | Significant Negative Associations |
|---|---|---|---|
| Treatment factors | |||
| Medication use | DeViva [16] 1 | ||
| Positive beliefs about mental health care | DeViva et al. [17] 1 | ||
| Barriers to mental health care | Hoerster et al. [20] 1 | ||
| Stigma regarding mental health care | DeViva et al. [17] 1 | Hoerster et al. [20] 1 Whealin et al. [13] 1 | |
| Type of treatment facility | Hudson et al. [21] 1,3 | ||
| Type of referral facility | Keller & Tuerk [28] 1 | DeViva [18] 1 | |
| Delivery of therapy | Kehle-Forbes et al. [27] 1 | ||
| Type of therapy | Kehle-Forbes et al. [27] 1 | ||
| Training level of treatment provider | Keller & Tuerk [28] 1 | ||
| Engagement in treatment outside VA | Hearne [19] 1 | ||
| Expressed interest in treatment outside VA | Hearne [19] 1 | ||
| Distance to the nearest VA clinic | Whealin et al. [13] 1 | ||
| Functioning factors | |||
| Legal problems | DeViva [16] 1 | ||
| Social impairment | Kaier et al. [22] 4,6 | ||
| Relationship satisfaction | McGinn et al. [25] 4 | ||
| Occupational impairment | Kaier et al. [22] 4,6 | ||
| Sleep quality | Harpaz-Rotem et al. [18] 1 | ||
| Pain | DeViva [16] 1 Naragon-Gainey et al. [26] 4,5 | ||
| Quality of life | Whealin et al. [13] 1 | ||
| Life satisfaction | Harpaz-Rotem et al. [18] 1 | ||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mark, K.M.; Murphy, D.; Stevelink, S.A.M.; Fear, N.T. Rates and Associated Factors of Secondary Mental Health Care Utilisation among Ex-Military Personnel in the United States: A Narrative Review. Healthcare 2019, 7, 18. https://doi.org/10.3390/healthcare7010018
Mark KM, Murphy D, Stevelink SAM, Fear NT. Rates and Associated Factors of Secondary Mental Health Care Utilisation among Ex-Military Personnel in the United States: A Narrative Review. Healthcare. 2019; 7(1):18. https://doi.org/10.3390/healthcare7010018
Chicago/Turabian StyleMark, Katharine M., Dominic Murphy, Sharon A.M. Stevelink, and Nicola T. Fear. 2019. "Rates and Associated Factors of Secondary Mental Health Care Utilisation among Ex-Military Personnel in the United States: A Narrative Review" Healthcare 7, no. 1: 18. https://doi.org/10.3390/healthcare7010018
APA StyleMark, K. M., Murphy, D., Stevelink, S. A. M., & Fear, N. T. (2019). Rates and Associated Factors of Secondary Mental Health Care Utilisation among Ex-Military Personnel in the United States: A Narrative Review. Healthcare, 7(1), 18. https://doi.org/10.3390/healthcare7010018





