Combined Effects of Race and Socioeconomic Status on Cancer Beliefs, Cognitions, and Emotions
Abstract
1. Background
2. Methods
2.1. Design and Setting
2.2. Ethics
2.3. Sampling
2.4. Surveys
2.5. Study Variables
2.5.1. Independent Variable
2.5.2. Covariates
2.5.3. Dependent Variables
2.5.4. Mediators
2.6. Statistical Analysis
3. Results
3.1. Descriptive Statistics
3.2. Bivariate Correlations
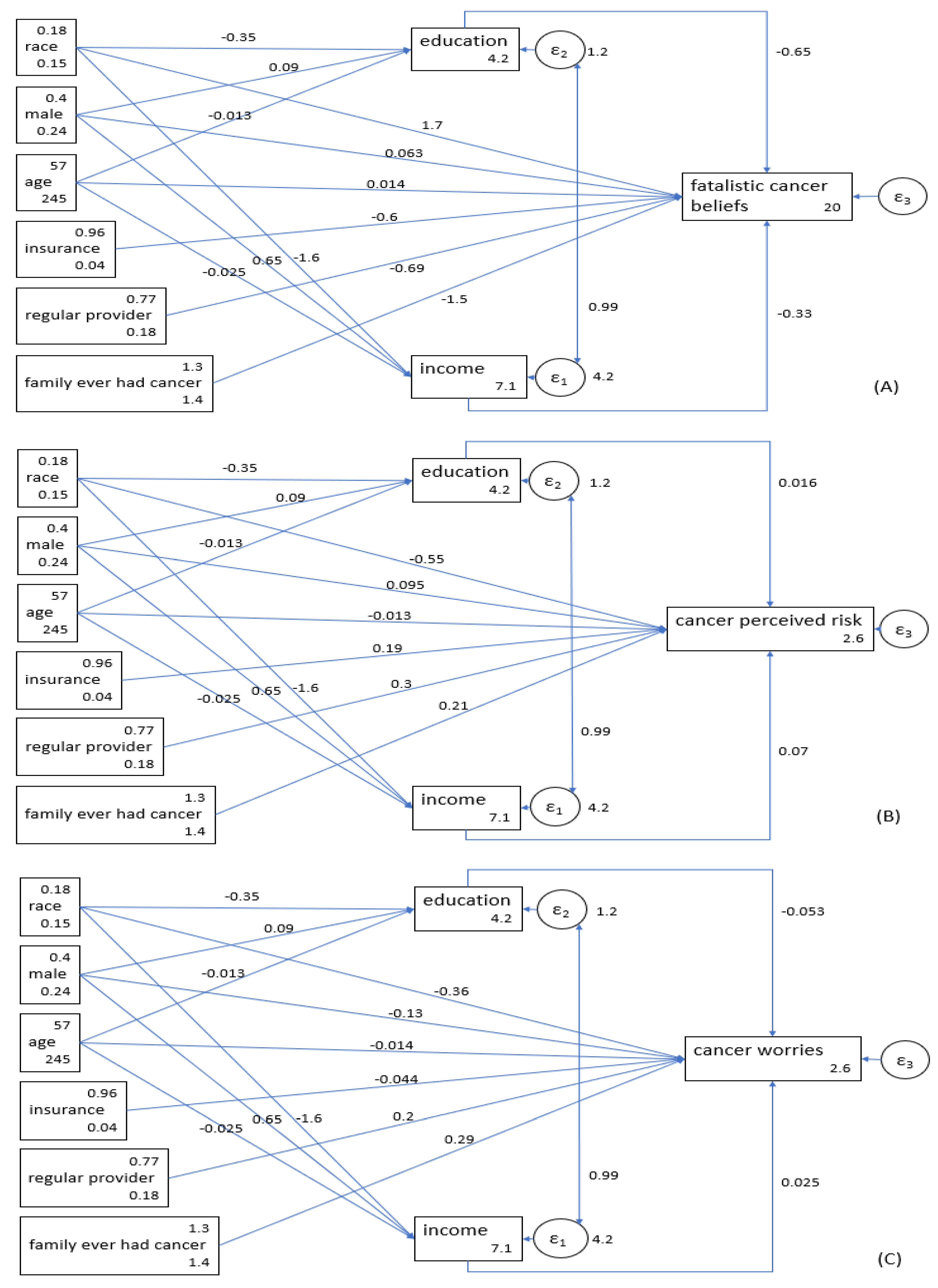
3.3. Fatalistic Cancer Beliefs
3.4. Perceived Risk of Cancer
3.5. Cancer Worries
4. Discussion
4.1. Study Limitations and Future Research
4.2. Implications
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- King, G.; Wlliams, D.R.; Aick, B.C.; Lvin, S.; Wlsh, D.C.; Tarlov, A.R. Race and health: A multidimensional approach to African American Health. In Society and Health; Oxford University Press: Oxford, UK, 1995. [Google Scholar]
- Assari, S. Number of chronic medical conditions fully mediates the effects of race on mortality; 25-year follow-up of a nationally representative sample of Americans. J. Racial Ethn. Health Disparities 2017, 4, 623–631. [Google Scholar] [CrossRef] [PubMed]
- Assari, S. Cross-country variation in additive effects of socio-economics, health behaviors, and comorbidities on subjective health of patients with diabetes. J. Diabetes Metab. Disord. 2014, 13, 36. [Google Scholar] [CrossRef] [PubMed]
- Assari, S.; Lankarani, M.M. Does multi-morbidity mediate the effect of socioeconomics on self-rated health? Cross-country differences. Int. J. Prev. Med. 2015, 6, 85. [Google Scholar] [CrossRef] [PubMed]
- Adler, N.; Boyce, T.; Chesney, M.; Cohen, S.; Folkman, S.; Kahn, R.; Syme, L. Socioeconomic status and health: The challenge of the gradient. Am. Psychol. 1994, 49, 15–24. [Google Scholar] [CrossRef] [PubMed]
- Marmot, M.; Kogevinas, M.; Elston, M. Social/economic status and disease. Annu. Rev. Public Health 1987, 8, 111–135. [Google Scholar] [CrossRef]
- Link, B.G.; Phelan, J. Social conditions as fundamental causes of disease. J. Health Soc. Behav. 1995, 36, 80–94. [Google Scholar] [CrossRef]
- House, J.S.; Lepkowski, J.M.; Kinney, A.M.; Mero, R.P.; Kessler, R.C.; Herzog, A.R. The social stratification of aging and health. J. Health Soc. Behav. 1994, 35, 213–234. [Google Scholar] [CrossRef]
- House, J.S.; Kessler, R.C.; Herzog, A.R. Age, socioeconomic status, and health. Milbank Q. 1990, 68, 383–411. [Google Scholar] [CrossRef]
- Pappas, G.; Qeen, S.; Hdden, W.; Fisher, G. The increasing disparity in mortality between socioeconomic groups in the United States, 1960 and 1986. N. Engl. J. Med. 1993, 329, 103–109. [Google Scholar] [CrossRef] [PubMed]
- Navarro, V. Race or class versus race and class: Mortality differentials in the United States. Lancet 1990, 336, 1238–1240. [Google Scholar] [CrossRef]
- Kaufman, J.S.; Coper, R.S.; McGee, D.L. Socioeconomic status and health in blacks and whites: The problem of residual confounding and the resiliency of race. Epidemiology 1997, 8, 621–628. [Google Scholar] [CrossRef] [PubMed]
- Kawachi, I.; Dniels, N.; Robinson, D.E. Health disparities by race and class: Why both matter. Health Aff. 2005, 24, 343–352. [Google Scholar] [CrossRef] [PubMed]
- Williams, D.R.; Collins, C. U.S. socioeconomic and racial differences in health: Patterns and explanations. Annu. Rev. Sociol. 1995, 21, 349–386. [Google Scholar] [CrossRef]
- Williams, D.R.; Priest, N.; Aderson, N.B. Understanding associations among race, socioeconomic status, and health: Patterns and prospects. Health Psychol. 2016, 35, 407–411. [Google Scholar] [CrossRef] [PubMed]
- Gornick, M.E.; Egers, P.W.; Rilly, T.W.; Mntnech, R.M.; Ftterman, L.K.; Kcken, L.E.; Vladeck, B.C. Effects of race and income on mortality and use of services among Medicare beneficiaries. N. Engl. J. Med. 1996, 335, 791–799. [Google Scholar] [CrossRef]
- Assari, S. Distal, intermediate, and proximal mediators of racial disparities in renal disease mortality in the United States. J. Nephropathol. 2016, 5, 51. [Google Scholar] [CrossRef] [PubMed]
- Hayward, M.D.; Crimmins, E.M.; Miles, T.P.; Yu, Y. The significance of socioeconomic status in explaining the racial gap in chronic health conditions. Am. Sociol. Rev. 2000, 65, 91. [Google Scholar] [CrossRef]
- Blakely, T.; Disney, G.; Valeri, L.; Atkinson, J.; Teng, A.; Wilson, N.; Gurrin, L. Socioeconomic and tobacco mediation of ethnic inequalities in mortality over time: Repeated census-mortality cohort studies, 1981 to 2011. Epidemiology 2018, 29, 506–516. [Google Scholar] [CrossRef]
- Li, C.I.; Mlone, K.E.; Daling, J.R. Differences in breast cancer stage, treatment, and survival by race and ethnicity. Arch. Intern. Med. 2003, 163, 49–56. [Google Scholar] [CrossRef]
- Orom, H.; Kiviniemi, M.T.; Shavers, V.L.; Ross, L.; Underwood, W., 3rd. Perceived risk for breast cancer and its relationship to mammography in Blacks, Hispanics, and Whites. J. Behav. Med. 2013, 36, 466–476. [Google Scholar] [CrossRef]
- Pearlman, D.N.; Rakowski, W.; Erich, B.; Cark, M.A. Breast cancer screening practices among black, Hispanic, and white women: Reassessing differences. Am. J. Prev. Med. 1996, 12, 327–337. [Google Scholar] [CrossRef]
- Smith-Bindman, R.; Miglioretti, D.L.; Lurie, N.; Abraham, L.; Barbash, R.B.; Strzelczyk, J.; Dignan, M.; Barlow, W.E.; Beasley, C.M.; Kerlikowske, K. Does utilization of screening mammography explain racial and ethnic differences in breast cancer? Ann. Intern. Med. 2006, 144, 541–553. [Google Scholar] [CrossRef] [PubMed]
- Newman, L.A.; Mason, J.; Cote, D.; Vin, Y.; Carolin, K.; Bouwman, D.; Colditz, G.A. African-American ethnicity, socioeconomic status, and breast cancer survival: A meta–analysis of 14 studies involving over 10,000 African-American and 40,000 white American patients with carcinoma of the breast. Cancer Interdiscip. Int. J. Am. Cancer Soc. 2002, 94, 2844–2854. [Google Scholar] [CrossRef]
- Morris, G.J.; Naidu, S.; Topham, A.K.; Guiles, F.; Xu, Y.; McCue, P.; Schwartz, G.F.; Park, P.K.; Rosenberg, A.L.; Brill, K.; et al. Differences in breast carcinoma characteristics in newly diagnosed African–American and Caucasian patients: A single-institution compilation compared with the National Cancer Institute’s Surveillance, Epidemiology, and end results database. Cancer: Interdisciplinary International. J. Am. Cancer Soc. 2007, 110, 876–884. [Google Scholar]
- Chlebowski, R.T.; Chen, Z.; Anderson, G.L.; Rohan, T.; Aragaki, A.; Lane, D.; Dolan, N.C.; Paskett, E.D.; McTiernan, A.; Hubbell, F.A.; et al. Ethnicity and breast cancer: Factors influencing differences in incidence and outcome. J. Natl. Cancer Inst. 2005, 97, 439–448. [Google Scholar] [CrossRef]
- Vona-Davis, L.; Rse, D.P. The influence of socioeconomic disparities on breast cancer tumor biology and prognosis: A review. J. Women’s Health 2009, 18, 883–893. [Google Scholar] [CrossRef]
- Curtis, E.; Quale, C.; Haggstrom, D.; Sith-Bindman, R. Racial and ethnic differences in breast cancer survival: How much is explained by screening, tumor severity, biology, treatment, comorbidities, and demographics? Cancer Interdiscip. Int. J. Am. Cancer Soc. 2008, 112, 171–180. [Google Scholar] [CrossRef]
- Cella, D.F.; Oav, E.J.; Krnblith, A.B.; Hlland, J.C.; Slberfarb, P.M.; Le, K.W.; Maurer, L.H. Socioeconomic status and cancer survival. J. Clin. Oncol. 1991, 9, 1500–1509. [Google Scholar] [CrossRef]
- Yost, K.; Prkins, C.; Chen, R.; Mrris, C.; Wright, W. Socioeconomic status and breast cancer incidence in California for different race/ethnic groups. Cancer Causes Control 2001, 12, 703–711. [Google Scholar] [CrossRef]
- Bradley, C.J.; Gven, C.W.; Roberts, C. Race, socioeconomic status, and breast cancer treatment and survival. J. Natl. Cancer Inst. 2002, 94, 490–496. [Google Scholar] [CrossRef]
- Ward, E.; Jmal, A.; Ckkinides, V.; Sngh, G.K.; Crdinez, C.; Gafoor, A.; Thun, M. Cancer disparities by race/ethnicity and socioeconomic status. CA Cancer J. Clin. 2004, 54, 78–93. [Google Scholar] [CrossRef] [PubMed]
- Bennett, C.L.; Frreira, M.R.; Dvis, T.C.; Kplan, J.; Winberger, M.; Kzel, T.; Sartor, O. Relation between literacy, race, and stage of presentation among low-income patients with prostate cancer. J. Clin. Oncol. 1998, 16, 3101–3104. [Google Scholar] [CrossRef]
- Newman, L.A.; Giffith, K.A.; Jtoi, I.; Smon, M.S.; Cowe, J.P.; Colditz, G.A. Meta-analysis of survival in African American and white American patients with breast cancer: Ethnicity compared with socioeconomic status. J. Clin. Oncol. 2006, 24, 1342–1349. [Google Scholar] [CrossRef] [PubMed]
- Clegg, L.X.; Richman, M.E.; Mller, B.A.; Hnkey, B.F.; Sngh, G.K.; Ln, Y.D.; Bernstein, L. Impact of socioeconomic status on cancer incidence and stage at diagnosis: Selected findings from the surveillance, epidemiology, and end results: National Longitudinal Mortality Study. Cancer Causes Control 2009, 20, 417–435. [Google Scholar] [CrossRef] [PubMed]
- Siegel, R.; Wrd, E.; Bawley, O.; Jemal, A. Cancer statistics, 2011: The impact of eliminating socioeconomic and racial disparities on premature cancer deaths. CA Cancer J. Clin. 2011, 61, 212–236. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.Y.; Ju, E.; Vng, P.D.; Lundquist, M. Breast and cervical cancer screening disparity among Asian American women: Does race/ethnicity matter? J. Women’s Health 2010, 19, 1877–1884. [Google Scholar] [CrossRef] [PubMed]
- Paskett, E.D.; Rshing, J.; D’Agostino, R.; Ttum, C.; Velez, R. Cancer screening behaviors of low-income women: The impact of race. Women’s Health (Hillsdalenj) 2014, 3, 203–226. [Google Scholar]
- Barroso, J.; MMillan, S.; Csey, L.; Gbson, W.; Kminski, G.; Meyer, J. Comparison between African-American and white women in their beliefs about breast cancer and their health locus of control. Cancer Nurs. 2000, 23, 268–276. [Google Scholar] [CrossRef]
- Demark-Wahnefried, W.; Srigo, T.; Ctoe, K.; Cnaway, M.; Bunetti, M.; Rmer, B.K.; Robertson, C.N. Knowledge, beliefs, and prior screening behavior among blacks and whites reporting for prostate cancer screening. Urology 1995, 46, 346–351. [Google Scholar] [CrossRef]
- Assari, S. Health disparities due to diminished return among black Americans: Public policy solutions. Soc. Issues Policy Rev. 2018, 12, 112–145. [Google Scholar] [CrossRef]
- Assari, S. Diminished economic return of socioeconomic status for black families. Soc. Sci. 2018, 7, 74. [Google Scholar] [CrossRef]
- Farmer, M.M.; Ferraro, K.F. Are racial disparities in health conditional on socioeconomic status? Soc. Sci. Med. 2005, 60, 191–204. [Google Scholar] [CrossRef] [PubMed]
- Assari, S.; Tomas, A.; Cldwell, C.H.; Mincy, R.B. Blacks’ diminished health return of family structure and socioeconomic status; 15 years of follow-up of a national urban sample of youth. J. Urban Health 2018, 95, 21–35. [Google Scholar] [CrossRef] [PubMed]
- Assari, S. Unequal gain of equal resources across racial groups. Int. J. Health Policy Manag. 2018, 7, 1. [Google Scholar] [CrossRef] [PubMed]
- Baquet, C.R.; Mishra, S.I.; Commiskey, P.; Ellison, G.L.; DeShields, M. Breast cancer epidemiology in blacks and whites: Disparities in incidence, mortality, survival rates and histology. J. Natl. Med. Assoc. 2008, 100, 480–488. [Google Scholar] [CrossRef]
- Baquet, C.R.; Commiskey, P.; Mack, K.; Meltzer, S.; Mishra, S.I. Esophageal cancer epidemiology in blacks and whites: Racial and gender disparities in incidence, mortality, survival rates and histology. J. Natl. Med. Assoc. 2005, 97, 1471–1478. [Google Scholar]
- Baquet, C.R.; Commiskey, P. Colorectal cancer epidemiology in minorities: A review. J. Assoc. Acad. Minor. Phys. 1999, 10, 51–58. [Google Scholar]
- Kendzor, D.E.; Costello, T.J.; Li, Y.; Vidrine, J.I.; Mazas, C.A.; Reitzel, L.R.; Cinciripini, P.M.; Cofta-Woerpel, L.M.; Businelle, M.S.; Wetter, D.W. Race/ethnicity and multiple cancer risk factors among individuals seeking smoking cessation treatment. Cancer Epidemiol. Biomark. Prev. 2008, 17, 2937–2945. [Google Scholar] [CrossRef]
- Wolf, M.S.; Knight, S.J.; Lyons, E.A.; Durazo-Arvizu, R.; Pickard, S.A.; Arseven, A.; Arozullah, A.; Colella, K.; Ry, P.; Bnnett, C.L. Literacy, race, and PSA level among low-income men newly diagnosed with prostate cancer. Urology 2006, 68, 89–93. [Google Scholar] [CrossRef]
- Flynn, J.; Sovic, P.; Mertz, C.K. Gender, race, and perception of environmental health risks. Risk Anal. 1994, 14, 1101–1108. [Google Scholar] [CrossRef]
- Finucane, M.L.; Sovic, P.; Mrtz, C.K.; Fynn, J.; Satterfield, T.A. Gender, race, and perceived risk: The ‘White male’ effect. Health Risk Soc. 2000, 2, 159–172. [Google Scholar] [CrossRef]
- Goel, M.S.; Wee, C.C.; McCarthy, E.P.; Davis, R.B.; Ngo-Metzger, Q.; Pillips, R.S. Racial and ethnic disparities in cancer screening: The importance of foreign birth as a barrier to care. J. Gen. Intern. Med. 2003, 18, 1028–1035. [Google Scholar] [CrossRef] [PubMed]
- Clegg, L.X.; Li, F.P.; Hankey, B.F.; Chu, K.; Ewards, B.K. Cancer survival among US whites and minorities: A SEER (Surveillance, Epidemiology, and End Results) Program population-based study. Arch. Intern. Med. 2002, 162, 1985–1993. [Google Scholar] [CrossRef] [PubMed]
- Hesse, B.W.; Moser, R.P.; Rutten, L.J.; Kreps, G.L. The Health Information National Trends Survey: Research from the Baseline. J. Health Commun. 2006, 11, vii–xvi. Available online: http://www.tandfonline.com/doi/abs/10.1080/10810730600692553 (accessed on 21 November 2018). [CrossRef] [PubMed]
- Chalian, H.; Khoshpouri, P.; Assari, S. Demographic, social, and behavioral determinants of lung cancer perceived risk and worries in a national sample of American adults; does lung cancer risk matter? Medicina 2018, 54, 97. [Google Scholar] [CrossRef] [PubMed]
- Chalian, H.; Khoshpouri, P.; Iranmanesh, A.; Mmmarappallil, J.G.; Assari, S. Lung cancer screening patient-provider discussion. Where do we stand and what are the associates? Sage Open Med. 2019, in press. [Google Scholar]
- Chalian, H.; Khoshpouri, P.; Assari, S. Patients’ age and discussion with doctors about lung cancer screening; Diminished returns of Blacks. Aging Med. 2019, in press. [Google Scholar]
- Niederdeppe, J.; Levy, A.G. Fatalistic beliefs about cancer prevention and three prevention behaviors. Cancer Epidemiol. Prev. Biomark. 2007, 16, 998–1003. [Google Scholar] [CrossRef]
- Orom, H.; O’Quin, K.E.; Reilly, S.; Kiviniemi, M.T. Perceived cancer risk and risk attributions among African-American residents of a low-income, predominantly African-American neighborhood. Ethn. Health 2015, 20, 543–556. [Google Scholar] [CrossRef]
- Chen, Y.; Yng, Q. How do cancer risk perception, benefit perception of quitting, and cancer worry influence quitting intention among current smokers: A study using the 2013 HINTS. J. Subst. Use 2017, 22, 555–560. [Google Scholar] [CrossRef]
- Kline, R.B. Principles and Practice of Structural Equation Modeling, 3rd ed.; Guilford Press: New York, NY, USA, 2010. [Google Scholar]
- Allison, P.D. Missing Data; SAGE: Thousand Oaks, CA, USA, 2002; pp. 7–136. [Google Scholar]
- Arbuckle, J.A. IBM SPSS Amos 20 User’s Guide; IBM Corp.: Armonk, NY, USA, 2012. [Google Scholar]
- Hu, L.; Bntler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. Multidiscip. J. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Lei, M.; Lmax, R.G. The effect of varying degrees of nonnormality in structural equation modeling. Struct. Equ. Model. 2005, 12, 1–27. [Google Scholar] [CrossRef]
- Assari, S. Parental education better helps White than Black families escape poverty: National survey of children’s health. Economies 2018, 6, 30. [Google Scholar] [CrossRef]
- Assari, S.; Preiser, B.; Kelly, M. Education and income predict future emotional well-being of Whites but not Blacks: A ten-year cohort. Brain Sci. 2018, 8, 122. [Google Scholar] [CrossRef] [PubMed]
- Assari, S. Blacks’ diminished return of education attainment on subjective health; mediating effect of income. Brain Sci. 2018, 8, 176. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, K.; Mcco, E.; Crney, A.; Sopfer, J.; Putt, M. Racial differences in the use of BRCA1/2 testing among women with a family history of breast or ovarian cancer. JAMA 2005, 293, 1729–1736. [Google Scholar] [CrossRef]
- Orom, H.; Kviniemi, M.T.; Uderwood, W.; Rss, L.; Shavers, V.L. Perceived cancer risk: Why is it lower among nonwhites than whites? Cancer Epidemiol. Prev. Biomark. 2010, 1055–9965. [Google Scholar] [CrossRef] [PubMed]
- Pagán, J.A.; Su, D.; Li, L.; Amstrong, K.; Asch, D.A. Racial and ethnic disparities in awareness of genetic testing for cancer risk. Am. J. Prev. Med. 2009, 37, 524–530. [Google Scholar] [CrossRef]
- Gwede, C.K.; Wlliam, C.M.; Tomas, K.B.; Trver, W.L.; Qinn, G.P.; Vdaparampil, S.T.; Meade, C.D. Exploring disparities and variability in perceptions and self-reported colorectal cancer screening among three ethnic subgroups of US Blacks. In Oncology Nursing Forum; NIH Public Access: Bethesda, MD, USA, 2010; Volume 37, p. 581. [Google Scholar]
- Vrinten, C.; van Jaarsveld, C.H.; Waller, J.; von Wagner, C.; Wardle, J. The structure and demographic correlates of cancer fear. BMC Cancer 2014, 14, 597. [Google Scholar] [CrossRef]
- Vrinten, C.; Waller, J.; von Wagner, C.; Wrdle, J. Cancer fear: Facilitator and deterrent to participation in colorectal cancer screening. Cancer Epidemiol. Biomark. Prev. 2015, 24, 400–405. [Google Scholar] [CrossRef]
- Vrinten, C.; Wardle, J.; Marlow, L.A. Cancer fear and fatalism among ethnic minority women in the United Kingdom. Br. J. Cancer 2016, 114, 597–604. [Google Scholar] [CrossRef] [PubMed]
- Vrinten, C.; McGregor, L.M.; Heinrich, M.; von Wagner, C.; Waller, J.; Wrdle, J.; Back, G.B. What do people fear about cancer? A systematic review and meta-synthesis of cancer fears in the general population. Psychooncology 2017, 26, 1070–1079. [Google Scholar] [CrossRef] [PubMed]
- Vrinten, C.; Wrdle, J. Is cancer a good way to die? A population-based survey among middle-aged and older adults in the United Kingdom. Eur. J. Cancer 2016, 56, 172–178. [Google Scholar] [CrossRef] [PubMed]
- Murphy, P.J.; Marlow, L.A.; Waller, J.; Vinten, C. What is it about a cancer diagnosis that would worry people? A population-based survey of adults in England. BMC Cancer 2018, 18, 86. [Google Scholar] [CrossRef] [PubMed]
- Vrinten, C.; Boniface, D.; Lo, S.H.; Kobayashi, L.C.; von Wagner, C.; Wller, J. Does psychosocial stress exacerbate avoidant responses to cancer information in those who are afraid of cancer? A population-based survey among older adults in England. Psychol. Health 2018, 33, 117–129. [Google Scholar] [CrossRef] [PubMed]
- Winterich, J.A.; Gzywacz, J.G.; Qandt, S.A.; Cark, P.E.; Mller, D.P.; Auna, J.; Arcury, T.A. Men’s knowledge and beliefs about prostate cancer: Education, race, and screening status. Ethn. Dis. 2009, 19, 199. [Google Scholar] [PubMed]
- Champion, V.L.; Mnahan, P.O.; Sringston, J.K.; Rssell, K.; Zllinger, T.W.; Sywell, R.M., Jr.; Maraj, M. Measuring mammography and breast cancer beliefs in African American women. J. Health Psychol. 2008, 13, 827–837. [Google Scholar] [CrossRef]
- Assari, S.; Moghani Lankarani, M. Poverty Status and Childhood Asthma in White and Black Families: National Survey of Children’s Health. Healthcare 2018, 6, 62. [Google Scholar] [CrossRef]
- Assari, S.; Nikahd, A.; Malekahmadi, M.R.; Lankarani, M.M.; Zamanian, H. Race by gender group differences in the protective effects of socioeconomic factors against sustained health problems across five domains. J. Racial Ethn. Health Disparities 2017, 414, 884–894. [Google Scholar] [CrossRef]
- Hudson, D.L.; Bllard, K.M.; Nighbors, H.W.; Gronimus, A.T.; Yng, J.; Jackson, J.S. Are benefits conferred with greater socioeconomic position undermined by racial discrimination among African American men? J. Men’s Health 2012, 9, 127–136. [Google Scholar] [CrossRef]
- Krieger, N. Epidemiology and the web of causation: Has anyone seen the spider? Soc. Sci. Med. 1994, 39, 887–903. [Google Scholar] [CrossRef]
- Krieger, N.; Sdney, S.; Coakley, E. Racial discrimination and skin color in the CARDIA study: Implications for public health research. Coronary Artery Risk Development in Young Adults. Am. J. Public Health 1998, 88, 1308–1313. [Google Scholar] [CrossRef] [PubMed]
- Williams, D.R.; Mohammed, S.A. Racism and health I: Pathways and scientific evidence. Am. Behav. Sci. 2013, 57, 1152–1173. [Google Scholar] [CrossRef] [PubMed]
- Williams, D.R.; Whitfield, K.E. Racism and Health. Closing the Gap: Improving the Health of Minority Elders in the New Millennium; Gerontological Society of America: Washington, DC, USA, 2004. [Google Scholar]
- Harris, R.; Tbias, M.; Jffreys, M.; Wldegrave, K.; Krlsen, S.; Nazroo, J. Racism and health: The relationship between experience of racial discrimination and health in New Zealand. Soc. Sci. Med. 2006, 63, 1428–1441. [Google Scholar] [CrossRef] [PubMed]
- Nazroo, J.Y. The structuring of ethnic inequalities in health: Economic position, racial discrimination, and racism. Am. J. Public Health 2003, 93, 277–284. [Google Scholar] [CrossRef]
- Meade, C.D.; MKinney, W.P.; Barnas, G.P. Educating patients with limited literacy skills: The effectiveness of printed and videotaped materials about colon cancer. Am. J. Public Health 1994, 84, 119–121. [Google Scholar] [CrossRef]
- Lee-Lin, F.; Ptt, M.; Mnon, U.; Le, S.; Nil, L.; Money, K.; Itano, J. Cervical cancer beliefs and pap test screening practices among Chinese American immigrants. Oncol. Nurs. Forum 2007, 34, 6. [Google Scholar] [CrossRef]
- Simon, C.E. Breast cancer screening: Cultural beliefs and diverse populations. Health Soc. Work 2006, 31, 36–43. [Google Scholar] [CrossRef]
- Freeman, H.P. Poverty, culture, and social injustice: Determinants of cancer disparities. CA Cancer J. Clin. 2004, 54, 72–77. [Google Scholar] [CrossRef]
- Shankar, S.; Slvin, E.; Alberg, A.J. Perceptions of cancer in an African-American community: A focus group report. Ethn. Dis. 2002, 12, 276–283. [Google Scholar]
- Pascoe, E.A.; Smart Richman, L. Perceived discrimination and health: A meta-analytic review. Psychol. Bull. 2009, 135, 531–554. [Google Scholar] [CrossRef] [PubMed]
- Mays, V.M.; Cochran, S.D.; Barnes, N.W. Race, race-based discrimination, and health outcomes among African Americans. Annu. Rev. Psychol. 2007, 58, 201–225. [Google Scholar] [CrossRef] [PubMed]
- Umutyan, A.; Ciechi, C.; Bckett, L.A.; Pterniti, D.A.; Trrell, C.; Gndara, D.R.; Lara, P.N., Jr. Overcoming barriers to cancer clinical trial accrual: Impact of a mass media campaign. Cancer Interdiscip. Int. J. Am. Cancer Soc. 2008, 112, 212–219. [Google Scholar] [CrossRef] [PubMed]
- Gerend, M.A.; Pai, M. Social determinants of Black-White disparities in breast cancer mortality: A review. Cancer Epidemiol. Prev. Biomark. 2008, 17, 2913–2923. [Google Scholar] [CrossRef] [PubMed]
- Allen, H.; Wight, B.J.; Hrding, K.; Broffman, L. The role of stigma in access to health care for the poor. Milbank Q. 2014, 92, 289–318. [Google Scholar] [CrossRef] [PubMed]
- Hall, M.A.; Dgan, E.; Zeng, B.; Mishra, A.K. Trust in physicians and medical institutions: What is it, can it be measured, and does it matter? Milbank Q. 2001, 79, 613–639. [Google Scholar] [CrossRef] [PubMed]
- Chambers, S.K.; Dnn, J.; Ochipinti, S.; Hghes, S.; Bade, P.; Snclair, S.; O’Connell, D.L. A systematic review of the impact of stigma and nihilism on lung cancer outcomes. BMC Cancer 2012, 12, 184. [Google Scholar] [CrossRef]
| Variables | % (SE) | 95% CI |
| Race | ||
| Non-Hispanic Whites | 86.66 (0.01) | 85.48–87.85 |
| Non-Hispanic Blacks | 13.34 (0.01) | 12.15–14.52 |
| Gender | ||
| Male | 47.89 (0.01) | 46.57–49.21 |
| Female | 52.11 (0.01) | 5.79–53.43 |
| Health Insurance | ||
| No | 7.87 (0.01) | 6.40–9.35 |
| Yes | 92.13 (0.01) | 9.65–93.60 |
| Variables | Mean (SE) | 95% CI |
| Age (Years) | 48.88 (0.34) | 48.19–49.56 |
| Income | 5.60 (0.05) | 5.49–5.70 |
| Educational Attainment | 3.12 (0.02) | 3.08–3.16 |
| Fatalistic Cancer Beliefs | ||
| Perceived Risk of Cancer | 2.93 (0.02) | 2.83–3.03 |
| Cancer Worries | 2.54 (0.04) | 2.45–2.62 |
| Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|---|
| 1. Race (Non-Hispanic Blacks) | 1.00 | ||||||||
| 2. Gender (Male) | −0.11 * | 1.00 | |||||||
| 3. Age | −0.07 * | 0.07 * | 1.00 | ||||||
| 4. Health Insurance | −0.02 | −0.01 | 0.07 * | 1.00 | |||||
| 5. Educational Attainment | −0.10 * | 0.01 | −0.15 * | 0.12 * | 1.00 | ||||
| 6. Income | −0.28 * | 0.15 * | −0.14 * | 0.14 * | 0.46 * | 1.00 | |||
| 7. Fatalistic Cancer Beliefs | 0.12 * | −0.01 | 0.04 | −0.03 | −0.18 * | −0.15 * | 1.00 | ||
| 8. Perceived Risk of Cancer | −0.14 * | 0.04 | −0.09 * | 0.02 | 0.02 | 0.08 * | −0.01 | 1.00 | |
| 9. Cancer Worries | −0.06 * | −0.05 | −0.11 * | −0.03 | −0.02 | 0.00 | 0.05 | 0.29 * | 1.00 |
| Variables | B(SE) | 95% CI | z | p |
|---|---|---|---|---|
| Fatalistic Cancer Beliefs | ||||
| Income | −0.33 (0.09) | (−0.50, −0.15) | −3.73 | <0.001 |
| Educational Attainment | −0.65 (0.15) | (−0.94, −0.35) | −4.31 | <0.001 |
| Race (Non-Hispanic Black) | 1.68 (0.40) | (0.90, 2.45) | 4.23 | <0.001 |
| Gender (Male) | 0.06 (0.32) | (−0.56, 0.69) | 0.20 | 0.843 |
| Age (Years) | 0.01 (0.01) | (−0.01, 0.04) | 1.29 | 0.196 |
| Family Member with Cancer | −1.52 (0.12) | (−1.76, −1.28) | −12.55 | <0.001 |
| Any Health Insurance | −0.60 (0.74) | (−2.04, 0.85) | −0.81 | 0.417 |
| Having a Regular Source of Health Care | −0.69 (0.36) | (−1.41, 0.02) | −1.90 | 0.057 |
| Intercept | 19.68 (1.06) | (17.61, 21.76) | 18.58 | <0.001 |
| Educational Attainment | ||||
| Race (Non-Hispanic Black) | −0.35 (0.06) | (−0.47, −0.23) | −5.70 | <0.001 |
| Gender (Male) | 0.09 (0.05) | (0.00, 0.18) | 1.86 | 0.063 |
| Age | −0.01 (0.00) | (−0.02, −0.01) | −8.47 | <0.001 |
| Intercept | 4.15 (0.09) | (3.97, 4.33) | 45.63 | <0.001 |
| Income | ||||
| Race (Non-Hispanic Black) | −1.65 (0.12) | (−1.87, −1.42) | −14.19 | <0.001 |
| Gender (Male) | 0.65 (0.09) | (0.47, 0.83) | 7.12 | <0.001 |
| Age (Years) | −0.03 (0.00) | (−0.03, −0.02) | −8.79 | <0.001 |
| Intercept | 7.12 (0.17) | (6.78, 7.46) | 4.94 | <0.001 |
| Variables | b (SE) | 95% CI | z | p |
|---|---|---|---|---|
| Perceived Risk of Cancer | ||||
| Income | 0.07 (0.02) | (0.02, 0.12) | 2.81 | 0.005 |
| Educational Attainment | 0.02 (0.04) | (−0.07, 0.10) | 0.37 | 0.714 |
| Race (Non-Hispanic Black) | −0.55 (0.11) | (−0.77, −0.33) | −4.84 | <0.001 |
| Gender (Male) | 0.10 (0.09) | (−0.08, 0.27) | 1.07 | 0.283 |
| Age (Years) | −0.01 (0.00) | (−0.02, −0.01) | −4.31 | <0.001 |
| Family Member with Cancer | 0.21 (0.03) | (0.14, 0.28) | 5.99 | <0.001 |
| Any Health Insurance | 0.19 (0.21) | (−.23, 0.60) | 0.88 | 0.380 |
| Having a Regular Source of Health Care | 0.30 (0.10) | (0.10, 0.50) | 2.90 | 0.004 |
| Intercept | 2.63 (0.30) | (2.04, 3.21) | 8.78 | <0.001 |
| Educational Attainment | ||||
| Race (Non-Hispanic Black) | −0.35 (0.06) | (−0.47, −0.23) | −5.73 | <0.001 |
| Gender (Male) | 0.09 (0.05) | (0.00, 0.18) | 1.87 | 0.062 |
| Age (Years) | −0.01 (0.00) | (−0.02, −0.01) | −8.47 | <0.001 |
| Intercept | 4.15 (0.09) | (3.97, 4.33) | 45.66 | <0.001 |
| Income | ||||
| Race (Non-Hispanic Black) | −1.64 (0.12) | (−1.87, −1.41) | −14.15 | <0.001 |
| Gender (Male) | 0.65 (0.09) | (0.47, 0.83) | 7.07 | <0.001 |
| Age (Years) | −0.03 (0.00) | (−0.03, −0.02) | −8.81 | <0.001 |
| Intercept | 7.12 (0.17) | (6.78, 7.46) | 41.02 | <0.001 |
| Variables | b (SE) | 95% CI | z | p |
|---|---|---|---|---|
| Cancer Worries | ||||
| Income | 0.02 (0.02) | (−0.02, 0.07) | 1.20 | 0.232 |
| Educational Attainment | −0.05 (0.03) | (−0.12, 0.02) | −1.53 | 0.126 |
| Race (Non-Hispanic Black) | −0.36 (0.09) | (−0.54, −0.18) | −3.85 | <0.001 |
| Gender (Male) | −0.13 (0.07) | (−0.27, 0.01) | −1.83 | 0.068 |
| Age (Years) | −0.01 (0.00) | (−0.02, −0.01) | −5.52 | <0.001 |
| Family Member with Cancer | 0.29 (0.03) | (0.24, 0.35) | 1.28 | <0.001 |
| Any Health Insurance | −0.04 (0.17) | (−0.38, 0.29) | −0.25 | 0.799 |
| Having a Regular Source of Health Care | 0.20 (0.08) | (0.04, 0.37) | 2.42 | 0.016 |
| Intercept | 2.87 (0.25) | (2.38, 3.35) | 11.58 | <0.001 |
| Educational Attainment | ||||
| Race (Non-Hispanic Black) | −0.35 (0.06) | (−0.47, −0.23) | −5.72 | <0.001 |
| Gender (Male) | 0.09 (0.05) | (0.00, 0.19) | 1.89 | 0.058 |
| Age (Years) | −0.01 (0.00) | (−0.02, −0.01) | −8.51 | <0.001 |
| Intercept | 4.15 (0.09) | (3.97, 4.33) | 45.73 | <0.001 |
| Income | ||||
| Race (Non-Hispanic Black) | −1.64 (0.12) | (−1.87, −1.41) | −14.17 | <0.001 |
| Gender (Male) | 0.65 (0.09) | (0.47, 0.83) | 7.09 | <0.001 |
| Age (Years) | −0.03 (0.00) | (−0.03, −0.02) | −8.91 | <0.001 |
| Intercept | 7.14 (0.17) | (6.80, 7.48) | 41.17 | <0.001 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Assari, S.; Khoshpouri, P.; Chalian, H. Combined Effects of Race and Socioeconomic Status on Cancer Beliefs, Cognitions, and Emotions. Healthcare 2019, 7, 17. https://doi.org/10.3390/healthcare7010017
Assari S, Khoshpouri P, Chalian H. Combined Effects of Race and Socioeconomic Status on Cancer Beliefs, Cognitions, and Emotions. Healthcare. 2019; 7(1):17. https://doi.org/10.3390/healthcare7010017
Chicago/Turabian StyleAssari, Shervin, Pegah Khoshpouri, and Hamid Chalian. 2019. "Combined Effects of Race and Socioeconomic Status on Cancer Beliefs, Cognitions, and Emotions" Healthcare 7, no. 1: 17. https://doi.org/10.3390/healthcare7010017
APA StyleAssari, S., Khoshpouri, P., & Chalian, H. (2019). Combined Effects of Race and Socioeconomic Status on Cancer Beliefs, Cognitions, and Emotions. Healthcare, 7(1), 17. https://doi.org/10.3390/healthcare7010017






