Oral Health in Pregnant Chinese Women in Singapore: A Call to Go beyond the Traditional Clinical Care
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design, Setting and Participants
2.2. Outcomes and Measurements
2.3. Data Collection Procedure
2.4. Ethical Considerations
2.5. Statistical Analysis
3. Results
3.1. Socio-Demographics and Self-Reported Clinical Characteristics of Participants
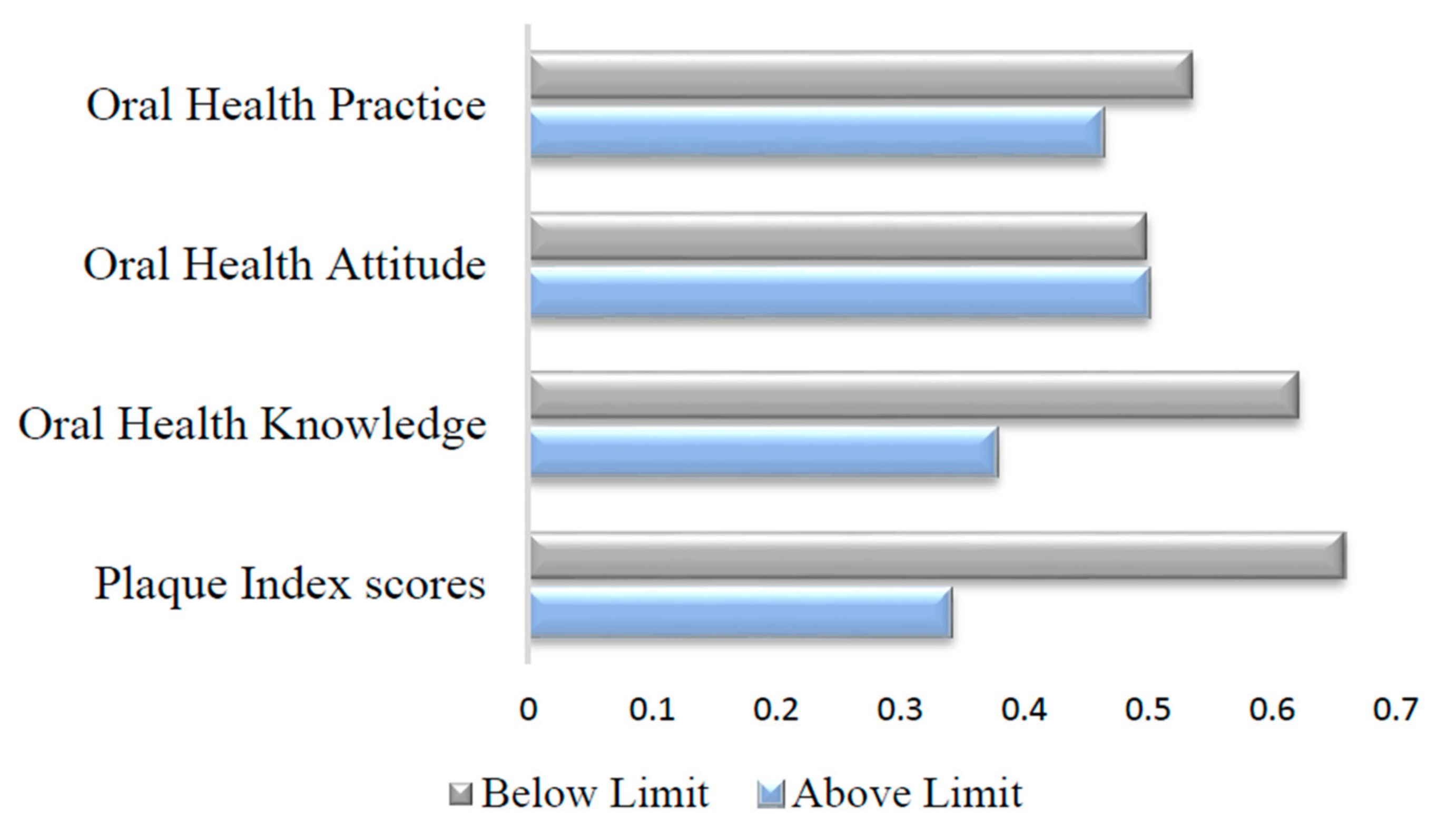
3.2. Levels of Oral Health Determinants among Participants
3.3. Association of Oral Health Status during Pregnancy with the Oral Health Determinant Factors and the Social Demographic Factors
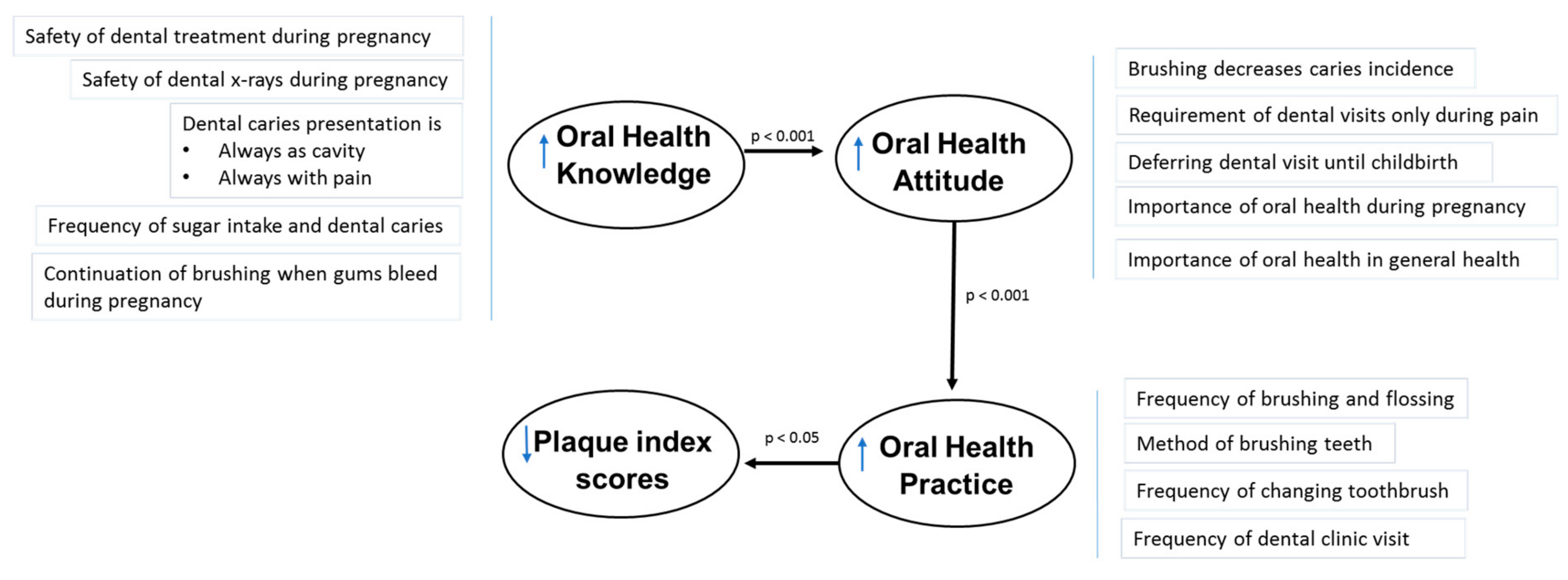
3.4. Correlations among Oral Health Determinants
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Ethics Approval
Appendix A
| SPSS | Statistical Package for the Social Sciences |
| PRAMS | Pregnancy Risk Assessment Monitoring System |
| ROHKI | Rustvold Oral Health Knowledge Inventory |
| OHAQ | Oral Health Attitudes Questionnaire |
| NHG DSRB | National Healthcare Group Domain Specific Review Boards |
| NUHS | National University Health System |
References
- La Marca-Ghaemmaghami, P.; Ehlert, U. Stress during Pregnancy. Eur. Psychol. 2015, 20, 102–119. [Google Scholar] [CrossRef]
- Silk, H.; Douglass, A.B.; Douglass, J.M.; Silk, L. Oral health during pregnancy. Am. Fam. Phys. 2008, 77, 1139–1144. [Google Scholar]
- Hey-Hadavi, J. Women’s oral health issues: Sex differences and clinical implications. Women’s Health Prim. Care Clin. 2002, 5, 189–199. [Google Scholar]
- Sherman, P.W.; Flaxman, S.M. Nausea and vomiting of pregnancy in an evolutionary perspective. Am. J. Obs. Gynecol. 2002, 186, S190–S197. [Google Scholar] [CrossRef]
- Shanthi, V.; Vanka, A.; Bhambal, A.; Saxena, V.; Saxena, S.; Kumar, S.S. Association of pregnant women periodontal status to preterm and low-birth weight babies: A systematic and evidence-based review. Dent. Res. J. 2012, 9, 368–380. [Google Scholar]
- Hom, J.M.; Lee, J.Y.; Divaris, K.; Diane Baker, A.; Vann, W.F. Oral health literacy and knowledge among patients who are pregnant for the first time. J. Am. Dent. Assoc. 2012, 143, 972–980. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.M.; Ren, F.; Chen, L.L.; Sun, W.L.; Liu, J.; Lei, L.H.; Zhang, J.; Cao, Z. Possible socioeconomic and oral hygiene behavioural risk factors for self-reported periodontal diseases in women of childbearing age in a Chinese population. Oral Health Prev. Dent. 2014, 12, 171–181. [Google Scholar] [CrossRef] [PubMed]
- Le, M.; Riedy, C.; Weinstein, P.; Milgrom, P. Barriers to utilization of dental services during pregnancy: A qualitative analysis. J. Dent. Child. 2009, 76, 46–52. [Google Scholar]
- Buerlein, J.K.; Horowitz, A.M.; Child, W.L. Perspectives of Maryland women regarding oral health during pregnancy and early childhood. J. Publ. Health Dent. 2011, 71, 131–135. [Google Scholar] [CrossRef]
- George, A.; Johnson, M.; Blinkhorn, A.; Ajwani, S.; Bhole, S.; Yeo, A.E.; Ellis, S. The oral health status, practices and knowledge of pregnant women in south-western Sydney. Aust. Dent. J. 2013, 58, 26–33. [Google Scholar] [CrossRef] [PubMed]
- Detman, L.A.; Cottrell, B.H.; Denis-Luque, M.F. Exploring dental care misconceptions and barriers in pregnancy. Birth 2010, 37, 318–324. [Google Scholar] [CrossRef] [PubMed]
- Marchi, K.S.; Fisher-Owen, S.A.; Weintraub, J.A.; Yu, Z.; Braveman, P.A. Most pregnant women in California do not receive dental care: Findings from a population-based study. Publ. Health Rep. 2010, 125, 831–842. [Google Scholar] [CrossRef] [PubMed]
- Gilbert, G.H. Racial and socioeconomic disparities in health from population-based research to practice-based research: The example of oral health. J. Dent. Educ. 2005, 69, 1003–1014. [Google Scholar] [PubMed]
- Hunter, L.P.; Yount, S.M. Oral health and oral health care practices among low-income pregnant women. J. Midwifery Women’s Health 2011, 56, 103–109. [Google Scholar] [CrossRef] [PubMed]
- Thompson, T.A.; Cheng, D.; Strobino, D. Dental cleaning before and during pregnancy among Maryland mothers. Matern. Child Health J. 2013, 17, 110–118. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.W.; Low, Y.L.; Fok, D.; Han, W.M.; Chong, Y.S.; Gluckman, P.; Godfrey, K.; Kwek, K.; Saw, S.M.; Soh, S.E.; et al. Dietary changes during pregnancy and the postpartum period in Singaporean Chinese, Malay and Indian women: The GUSTO birth cohort study. Public Health Nutr. 2014, 17, 1930–1938. [Google Scholar] [CrossRef] [PubMed]
- Naser, E.; Mackey, S.; Arthur, D.; Klainin-Yobas, P.; Chen, H.; Creedy, D.K. An exploratory study of traditional birthing practices of Chinese, Malay and Indian women in Singapore. Midwifery 2012, 28, e865–e871. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J. A power primer. Psychol. Bull. 1992, 112, 155–159. [Google Scholar] [CrossRef] [PubMed]
- Pregnancy Risk Assessment Monitoring System (PRAMS) Questionnaires; Division of Reproductive Health, National Center for Chronic Disease Prevention and Health Promotion; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2004–2008.
- Rustvold, S.R. Oral Health Knowledge, Attitudes, and Behaviors: Investigation of an Educational Intervention Strategy with at-Risk Females. Doctoral Thesis, Portland State University, Portland, ON, USA, 2012. [Google Scholar]
- Yuen, H.K.; Wolf, B.J.; Bandyopadhyay, D.; Magruder, K.M.; Salinas, C.F.; London, S.D. Oral health knowledge and behavior among adults with diabetes. Diabetes Res. Clin.Pract. 2009, 86, 239–246. [Google Scholar] [CrossRef] [PubMed]
- Singapore Department of Statistics. Population Trends; Singapore Department of Statistics, Ministry of Trade & Industry: Singapore, 2016; p. 5, ISSN 1793–2424.
- Singapore Department of Statistics. Population Trends; Singapore Department of Statistics: Singapore, 2016; p. 30.
- Wu, M.; Chen, S.W.; Jiang, S.Y. Relationship between gingival inflammation and pregnancy. Med. Inflamm. 2015, 2015. [Google Scholar] [CrossRef] [PubMed]
- Pirie, M.; Cooke, I.; Linden, G.; Irwin, C. Dental manifestations of pregnancy. Obs. Gynaecol. 2007, 9, 21–26. [Google Scholar] [CrossRef]
- Thomas, N.J.; Middleton, P.F.; Crowther, C.A. Oral and dental health care practices in pregnant women in Australia: A postnatal survey. BMC Pregnancy Childbirth 2008, 8, 13. [Google Scholar] [CrossRef] [PubMed]
- Gaffield, M.L.; Gilbert, B.J.; Malvitz, D.M.; Romaguera, R. Oral health during pregnancy: An analysis of information collected by the pregnancy risk assessment monitoring system. J. Am. Dent. Assoc. 2001, 132, 1009–1016. [Google Scholar] [CrossRef] [PubMed]
- Baskaradoss, J.K.; Geevarghese, A.; Al Dosari, A.A.F. Causes of Adverse Pregnancy Outcomes and the Role of Maternal Periodontal Status—A Review of the Literature. Open Dent. J. 2012, 6, 79–84. [Google Scholar] [CrossRef] [PubMed]
- Capasso, F.; Vozza, I.; Capuccio, V.; Vestri, A.R.; Polimeni, A.; Ottolenghi, L. Correlation among periodontal health status, maternal age and pre-term low birth weight. Am. J. Dent. 2016, 29, 197–200. [Google Scholar] [PubMed]
- Amin, M.; ElSalhy, M. Factors affecting utilization of dental services during pregnancy. J. Periodontol. 2014, 85, 1712–1721. [Google Scholar] [CrossRef] [PubMed]
- George, A.; Johnson, M.; Duff, M.; Ajwani, S.; Bhole, S.; Blinkhorn, A.; Ellis, S. Midwives and oral health care during pregnancy: Perceptions of pregnant women in south-western Sydney, Australia. J. Clin. Nurs. 2012, 21, 1087–1096. [Google Scholar] [CrossRef] [PubMed]
- Hullah, E.; Turok, Y.; Nauta, M.; Yoong, W. Self-reported oral hygiene habits, dental attendance and attitudes to dentistry during pregnancy in a sample of immigrant women in North London. Arch. Gynecol. Obs. 2008, 277, 405–409. [Google Scholar] [CrossRef] [PubMed]
- Al Habashneh, R.; Guthmiller, J.M.; Levy, S.; Johnson, G.K.; Squier, C.; Dawson, D.V.; Fang, Q. Factors related to utilization of dental services during pregnancy. J. Clin. Periodontol. 2005, 32, 815–821. [Google Scholar] [CrossRef] [PubMed]
- Committee on Health Care for Underserved Women. Oral health care during pregnancy and through the lifespan. Obs. Gynecol. 2013, 122, 417–422. [Google Scholar] [CrossRef]
- Naseem, M.; Khurshid, Z.; Khan, H.A.; Niazi, F.; Zohaib, S.; Zafar, M.S. Oral health challenges in pregnant women: Recommendations for dental care professionals. Saudi J. Dent. Res. 2016, 7, 138–146. [Google Scholar] [CrossRef]
- Chacko, V.; Shenoy, R.; Prasy, H.E.; Agarwal, S. Self-reported awareness of oral health and infant oral health among pregnant women in Mangalore, India—A prenatal survey. Int. J. Health Rehabilit. Sci. 2013, 2, 109–115. [Google Scholar]
- Saddki, N.; Yusoff, A.; Hwang, Y.L. Factors associated with dental visit and barriers to utilisation of oral health care services in a sample of antenatal mothers in Hospital Universiti Sains Malaysia. BMC Public Health 2010, 10, 75. [Google Scholar] [CrossRef] [PubMed]
- Al-Sufyani, G.A.; Al-Maweri, S.A.; Al-Ghashm, A.A.; Al-Soneidar, W.A. Oral hygiene and gingival health status of children with Down syndrome in Yemen: A cross-sectional study. J. Int. Soc. Prev. Commun. Dent. 2014, 4, 82–86. [Google Scholar] [CrossRef]
- Bressane, L.B.; Costa, L.N.B.D.S.; Vieira, J.M.R.; Rebelo, M.A.B. Oral health conditions among pregnant women attended to at a health care center in Manaus, Amazonas, Brazil. Rev. Odonto Cienc. 2011, 26, 291–296. [Google Scholar] [CrossRef]
- Deinzer, R.; Granrath, N.; Spahl, M.; Linz, S.; Waschul, B.; Herforth, A. Stress, oral health behaviour and clinical outcome. Br. J. Health Psychol. 2005, 10, 269–283. [Google Scholar] [CrossRef] [PubMed]
- Cigna Corporation. 2015 Cigna Corporation Healthy Smiles for Mom and Baby: Insights into Expecting and New Mothers’ Oral Health Habits. 2015. Available online: https://www.cigna.com/assets/docs/newsroom/cigna-study-healthy-smiles-for-mom-and-baby-2015.pdf (accessed on 3 July 2018).
- Tang, Y.; Zhu, Y.Q.; Wang, Y.; He, Y. A survey about knowledge, attitude, practice of oral health in pregnant women of one hospital in Shanghai municipality. Shanghai J. Stomatol. 2011, 20, 531–534. [Google Scholar]
- Ifesanya, J.U.; Ifesanya, A.O.; Asuzu, M.C.; Oke, G.A. Determinants of good oral hygiene among pregnant women in Ibadan, south-western Nigeria. Ann. Ib. Postgrad. Med. 2010, 8, 95–100. [Google Scholar] [CrossRef] [PubMed]
- Beegle, D. Overcoming the Silence of Generational Poverty: Invisible Literacies. 2003. Available online: http://www.combarriers.com/TP0151Overcoming.pdf (accessed on 10 February 2017).
- Steinberg, B.J.; Hilton, I.V.; Iida, H.; Samelson, R. Oral health and dental care during pregnancy. Dent. Clin. North Am. 2013, 57, 195–210. [Google Scholar] [CrossRef] [PubMed]
- Jackson, J.T.; Quinonez, R.B.; Kerns, A.K.; Chuang, A.; Eidson, R.S.; Boggess, K.A.; Weintraub, J.A. Implementing a prenatal oral health program through interprofessional collaboration. J. Dent. Educ. 2015, 79, 241–248. [Google Scholar] [PubMed]
| Sociodemographic and Oral Health Characteristics | Mean ± SD | N (%) |
|---|---|---|
| Sociodemographic characteristics | ||
| Age in years | 31.8 (± 4.5) | |
| Gestational age | 12.1 (± 5.2) | |
| Marital status | ||
| Married | 84 (98.8%) | |
| Single | 1 (1.2%) | |
| Highest educational level | ||
| Secondary school/diploma | 38 (46.3%) | |
| Graduate | 34 (41.4%) | |
| Masters/PhD | 10 (12.2%) | |
| Monthly household income | ||
| Low (≤2999$) | 23 (28.1%) | |
| Medium (3000 to 4999$) | 19 (23.2%) | |
| High (≥5000$) | 40 (48.8%) | |
| Smoking status | ||
| Yes | 0 (0.0%) | |
| No | 82 (100%) | |
| Intentions of practicing confinement | ||
| Yes | 70 (81.7%) | |
| No | 15 (18.3%) | |
| Oral health characteristics | ||
| Dental problems during pregnancy (Self-reported) | ||
| Yes | 20 (24.4%) | |
| No | 62 (75.6%) | |
| Self-reported dental complaints | ||
| Tooth decay | 2 (2.4%) | |
| Bleeding gums | 15 (18.3%) | |
| Gum boil | 0 (0.0%) | |
| Tooth-ache | 5 (6.1%) | |
| Tooth injury | 1 (1.2%) | |
| Bleeding gums within participants with dental problems during pregnancy | ||
| Yes | 15 (75.5%) | |
| No | 5 (25.5%) | |
| Participants who visited dentist for bleeding gums during pregnancy | ||
| Yes | 1 (6.7%) | |
| No | 14 (93.9%) | |
| Self-perception of oral health status | ||
| Good | 22 (26.8%) | |
| Poor/moderate | 60 (73.2%) | |
| Association between adverse pregnancy outcomes and oral health | ||
| Agree | 31(37.8%) | |
| Disagree | 5 (6.1%) | |
| Unsure | 46 (56.1%) | |
| Score | Mean ± SD | Median | Minimum | Maximum |
|---|---|---|---|---|
| Oral health knowledge | 27.5 ± 3.2 | 28 | 16.00 | 37.00 |
| Oral health attitude | 27.7 ± 2.9 | 28 | 22.00 | 34.00 |
| Oral health practice | 4.4 ± 1.8 | 4 | 0.00 | 9.00 |
| Plaque index | 1.4 ± 0.6 | 1 | 1.00 | 3.00 |
| Oral Health Status during Pregnancy | |||
|---|---|---|---|
| Problem present N = 20 (24.4%) | Problem absent N = 62 (75.6%) | p-value | |
| Oral health determinants | |||
| Oral health knowledge score (Mean) a | 38.9 | 42.3 | 0.572 |
| Oral health attitude score (Mean) a | 39.3 | 42.1 | 0.640 |
| Oral health practice score (Mean) a | 40.0 | 41.9 | 0.747 |
| Plaque index (Mean) a | 44.4 | 40.5 | 0.462 |
| Social demographic factors | |||
| Age (Mean) a | 34.3 | 43.8 | 0.121 |
| Income status (N, %) b | |||
| High (5000$–>10,000$) | 5 (12.5) | 35 (87.5) | 0.03 |
| Medium (3000$–4999$) | 7 (36.8) | 12 (63.2) | 0.890 |
| Low (<1000$–2999$) | 8 (34.8) | 15 (65.2) | |
| Educational level (N, %) b | |||
| Masters/PhD | 1 (10.0) | 9 (90.0) | 0.172 |
| Graduate | 7 (20.6) | 27 (79.4) | 0.291 |
| Secondary school/Diploma | 12 (31.6) | 26 (68.4) | |
| 1 | 2 | 3 | 4 | |
|---|---|---|---|---|
| 1.000 | |||
| 0.300 ** | 1.000 | ||
| 0.056 | 0.215 * | 1.000 | |
| −0.108 | −0.081 | −0.200 * | 1.000 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Balan, P.; He, H.-G.; Cao, F.; Wong, M.L.; Chong, Y.-S.; Lopez, V.; Soh, S.-E.; Seneviratne, C.J. Oral Health in Pregnant Chinese Women in Singapore: A Call to Go beyond the Traditional Clinical Care. Healthcare 2018, 6, 77. https://doi.org/10.3390/healthcare6030077
Balan P, He H-G, Cao F, Wong ML, Chong Y-S, Lopez V, Soh S-E, Seneviratne CJ. Oral Health in Pregnant Chinese Women in Singapore: A Call to Go beyond the Traditional Clinical Care. Healthcare. 2018; 6(3):77. https://doi.org/10.3390/healthcare6030077
Chicago/Turabian StyleBalan, Preethi, Hong-Gu He, Fengchunzhi Cao, Mun Loke Wong, Yap-Seng Chong, Violeta Lopez, Shu-E. Soh, and Chaminda Jayampath Seneviratne. 2018. "Oral Health in Pregnant Chinese Women in Singapore: A Call to Go beyond the Traditional Clinical Care" Healthcare 6, no. 3: 77. https://doi.org/10.3390/healthcare6030077
APA StyleBalan, P., He, H.-G., Cao, F., Wong, M. L., Chong, Y.-S., Lopez, V., Soh, S.-E., & Seneviratne, C. J. (2018). Oral Health in Pregnant Chinese Women in Singapore: A Call to Go beyond the Traditional Clinical Care. Healthcare, 6(3), 77. https://doi.org/10.3390/healthcare6030077




