Towards Differentiated Management: The Role of Organizational Type and Work Position in Shaping Employee Engagement Among Slovak Healthcare Professionals
Abstract
1. Introduction
2. Materials and Methods
3. Results
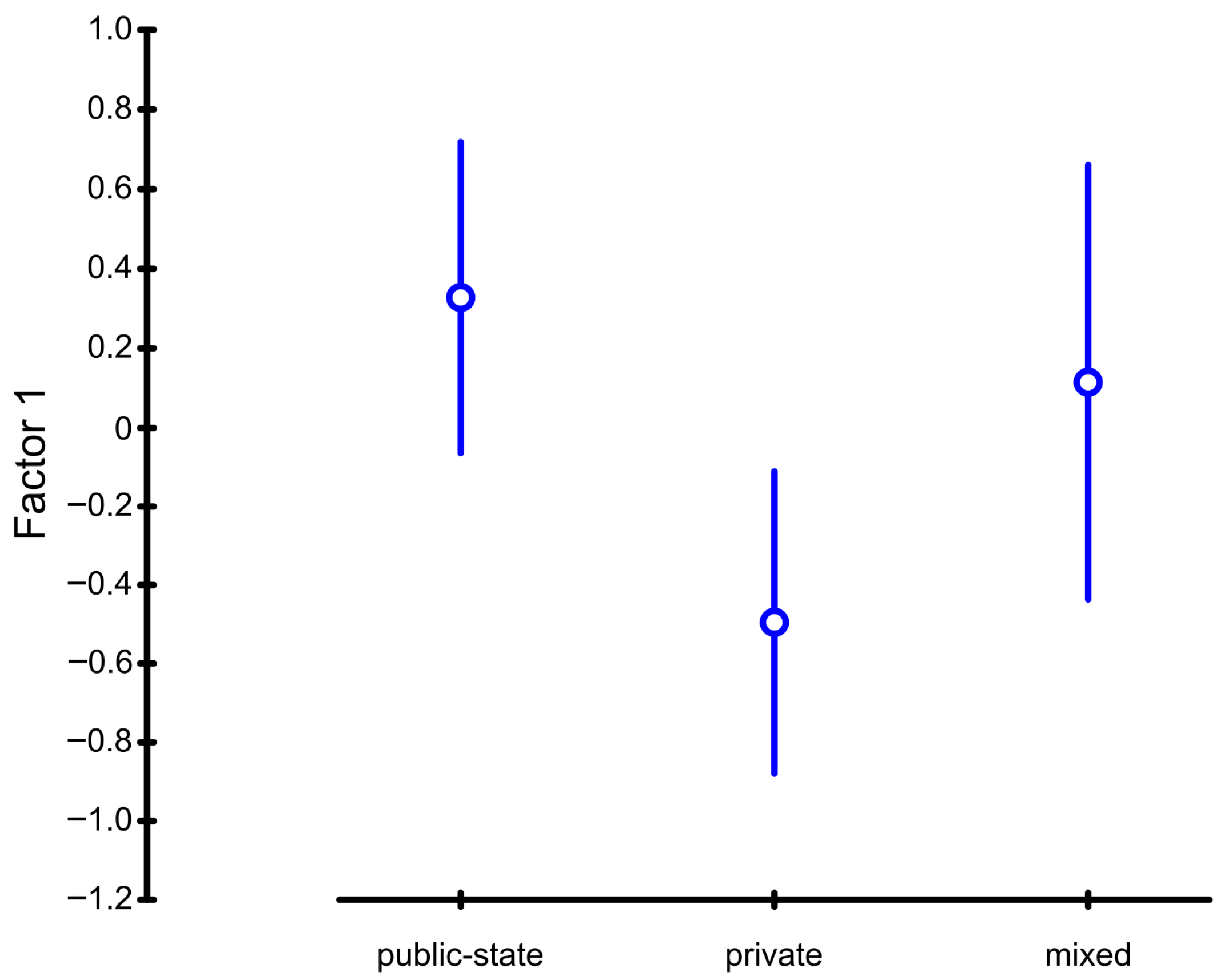
- Factor 1: Organizational Commitment and Identity.
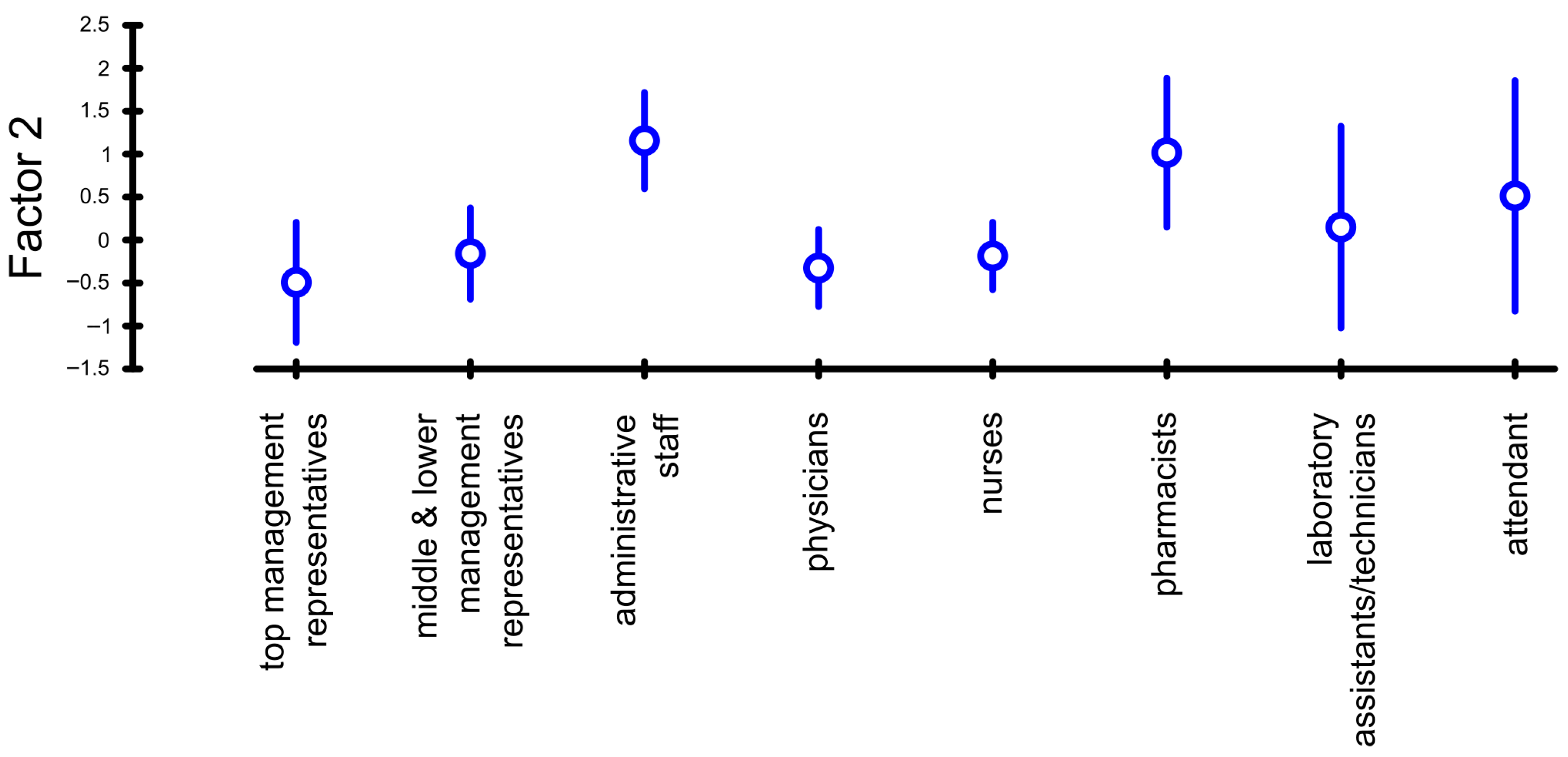
- Factor 2: Meaningful involvement and Job satisfaction (the factor corresponds to Kahn’s psychological meaningfulness);
- Factor 3: Organizational Citizenship and Retention Intent.
4. Discussion
4.1. Factor 1: Organizational Commitment and Identity
4.2. Factor 2: Meaningful Involvement and Job Satisfaction
4.3. Factor 3—Organizational Citizenship and Retention Intent
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ozorovský, V.; Vojteková a kolektív, I. Zdravotnícky Manažment a Financovanie; Wolters Kluwer: Alphen aan den Rijn, The Netherlands, 2016; pp. 168–178. ISBN 978-80-8168-522-4. [Google Scholar]
- Townsend, K.; Wilkinson, A.; Allan, C.; Bamber, G. All we need is a miracle: Using a solution-based approach to human resource management in hospitals. Asia Pac. J. Hum. Resour. 2011, 49, 165–179. [Google Scholar] [CrossRef]
- Inštitút Zdravotných Analýz (IZA). Komentár: Viac peňazí a Stability Pre Zdravotníctvo je Investíciou (More Money and Stability for Healthcare Is an Investment). Bratislava, Slovensko. 2024. Available online: https://analyzy.gov.sk/files/archiv/29/Komentar_Viac-penazi-a-stability-pre-zdravotnictvo-je-investiciou.pdf (accessed on 15 November 2025).
- National Health Information Centre. Healthcare Workers in the Slovak Republic 2024. Bratislava, Slovensko. 2024. Available online: https://www.nczisk.sk/Statisticke_vystupy/Tematicke_statisticke_vystupy/Pracovnici_zdravotnictve/Pages/default.aspx (accessed on 15 November 2025).
- Su, Y.; Jiang, Z.; Meng, R.; Lu, G.; Chen, C. The effect of organizational justice on young nurses’ turnover intention: The mediating roles of organizational climate and emotional labour. Nurse Educ. Pract. 2023, 72, 103723. [Google Scholar] [CrossRef] [PubMed]
- Ainy, A.; Sarri, M.N.; Fujiyanti, P.; Inaku, H.; Tembo, T. Job Satisfaction Among Health Workers at Primary Health Care in Palembang City, Indonesia. Kesmas 2025, 20, 104–111. [Google Scholar] [CrossRef]
- Kitsios, F.; Kamariotou, M. Job satisfaction behind motivation: An empirical study in public health workers. Heliyon 2021, 7, e06857. [Google Scholar] [CrossRef]
- Cohen, C.; Pignata, S.; Bezak, E.; Tie, M.; Childs, J. Workplace interventions to improve well-being and reduce burnout for nurses, physicians and allied healthcare professionals: A systematic review. BMJ Open 2023, 13, e071203. [Google Scholar] [CrossRef]
- Paganin, G.; De Angelis, M.; Pische, E.; Violante, F.S.; Guglielmi, D.; Pietrantoni, L. The Impact of Mental Health Leadership on Teamwork in Healthcare Organizations: A Serial Mediation Study. Sustainability 2023, 15, 7337. [Google Scholar] [CrossRef]
- Wang, L.; Dong, X.; Shang, S. The Relationship Between Perceived Staffing and Quality of Care: The Mediating Roles of Job Satisfaction and Work Engagement. J. Nurs. Res. 2025, 33, e376. [Google Scholar] [CrossRef]
- Janes, G.; Mills, T.; Budworth, L.; Johnson, J.; Lawton, R. The Association Between Health Care Staff Engagement and Patient Safety Outcomes: A Systematic Review and Meta-Analysis. J. Patient Saf. 2021, 17, 207–216. [Google Scholar] [CrossRef]
- Slåtten, T.; Lien, G.; Mutonyi, B. Precursors and outcomes of work engagement among nursing professionals—A cross-sectional study. BMC Health Serv. Res. 2022, 22, 21. [Google Scholar] [CrossRef]
- Bleier, H.; Lützerath, J.; Schaller, A. Organizational facilitators and barriers for participation in workplace health promotion in healthcare: A qualitative interview study among nurses. Front. Psychol. 2023, 14, 1101235. [Google Scholar] [CrossRef]
- Grossmeier, J.; Castle, P.H.; Pitts, J.S.; Saringer, C.; Jenkins, K.R.; Imboden, M.T.; Mangen, D.J.; Johnson, S.S.; Noeldner, S.P.; Mason, S.T. Workplace well-being factors that predict employee participation, health and medical cost impact, and perceived support. Am. J. Health Promot. 2020, 34, 349–358. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Mohamed, R.; Mahomed, A.; Khan, H. The effect of perceived organizational support and employee care on turnover intention and work engagement: A mediated moderation model using age in the post pandemic period. Sustainability 2022, 14, 9125. [Google Scholar] [CrossRef]
- Demirović Bajrami, D.; Terzić, A.; Petrović, M.D.; Radovanović, M.M.; Tretiakova, T.N.; Hadoud, A. Will we have the same employees in hospitality after all? The impact of COVID-19 on employees’ work attitudes and turnover intentions. Int. J. Hosp. Manag. 2020, 94, 102754. [Google Scholar] [CrossRef] [PubMed]
- Winter, P.D.; Chico, T.J.A. Using the non-adoption, abandonment, scale-up, spread, and sustainability (NASSS) framework to identify barriers and facilitators for the implementation of digital twins in cardiovascular medicine. Sensors 2023, 23, 6333. [Google Scholar] [CrossRef]
- Angus, R.; Hattingh, L.; Weir, K.A. The health service perspective on determinants of success in allied health student research project collaborations: A qualitative study guided by the consolidated framework for implementation research. BMC Health Serv. Res. 2024, 24, 143. [Google Scholar] [CrossRef]
- Zemplenyi, A.; Tachkov, K.; Balkanyi, L.; Nemeth, B.; Petykó, Z.I.; Petrova, G.; Czech, M.; Dawoud, D.; Goettsch, W.; Ibarluzea, I.G.; et al. Recommendations to overcome barriers to the use of artificial intelligence-driven evidence in health technology assessment. Front. Public Health 2023, 11, 1088121. [Google Scholar] [CrossRef]
- World Health Organization. Constitution of the World Health Organization. Basic Documents; World Health Organization: Geneva, Switzerland, 2006. [Google Scholar]
- Bakker, A.B.; Demerouti, E. Job demands-resources theory: Taking stock and looking forward. J. Occup. Health Psychol. 2017, 22, 273–285. [Google Scholar] [CrossRef]
- Dimunová, L.; Nagyová, I. Relation between burnout syndrome and employment duration in nurses and midwives in Slovakia. Profese Online 2012, 5, 23–35. [Google Scholar] [CrossRef]
- Galasová, M.; Uhrecký, B.; Kaššaiová, Z. So many negatives, but it still has meaning: A mixed-design cross-sectional study reflecting health professionals’ perceptions of the Slovak health system. Cent. Eur. J. Nurs. Midwifery 2023, 14, 968–979. [Google Scholar] [CrossRef]
- Liona, R.; Yurniardi, M. The contribution of work engagement and job satisfaction to workers’ psychological well-being. Humanitas 2020, 17, 94–103. [Google Scholar] [CrossRef]
- Bogaert, P.; Wouters, K.; Willems, R.; Mondelaers, M.; Clarke, S. Work engagement supports nurse workforce stability and quality of care: Nursing team-level analysis in psychiatric hospitals. J. Psychiatr. Ment. Health Nurs. 2013, 20, 679–686. [Google Scholar] [CrossRef] [PubMed]
- Morales-García, W.; Vallejos, M.; Sairitupa-Sanchez, L.; Morales-García, S.; Rivera-Lozada, O.; Morales-García, M. Depression, professional self-efficacy, and job performance as predictors of life satisfaction: The mediating role of work engagement in nurses. Front. Public Health 2024, 12, 1268336. [Google Scholar] [CrossRef] [PubMed]
- Jim, E.; Pio, R.; Asaloei, S.; Leba, S.; Angelianawati, D.; Werang, B. Work-Related Stress, Emotional Exhaustion, Job Satisfaction, and Organizational Commitment of Indonesian Healthcare Workers. Int. J. Relig. 2024, 5, 308–316. [Google Scholar] [CrossRef]
- Zajac, S.; Woods, A.; Tannenbaum, S.; Salas, E.; Holladay, C.L. Overcoming Challenges to Teamwork in Healthcare: A Team Effectiveness Framework and Evidence-Based Guidance. Front. Commun. 2021, 6, 606445. [Google Scholar] [CrossRef]
- Gubler, T.; Larkin, I.; Pierce, L. Doing well by making well: The impact of corporate wellness programs on employee productivity. Manag. Sci. 2018, 64, 4967–4987. [Google Scholar] [CrossRef]
- Schaller, A.; Gernert, M.; Klas, T.; Lange, M. Workplace health promotion interventions for nurses in Germany: A systematic review based on the RE-AIM framework. BMC Nurs. 2022, 21, 65. [Google Scholar] [CrossRef]
- Geta, A.; Biks, G.A.; Dellie, E.; Yazachew, L. Job Satisfaction and Associated Factors among Health Professionals Working at Public and Private Hospitals in Bahir Dar City, Northwest Ethiopia: A Comparative Cross-Sectional Study. BioMed Res. Int. 2021, 2021, 6632585. [Google Scholar] [CrossRef]
- Notarnicola, I.; Duka, B.; Lommi, M.; Grosha, E.; De Maria, M.; Iacorossi, L.; Mastroianni, C.; Ivziku, D.; Rocco, G.; Stievano, A. Transformational leadership and its impact on job satisfaction and personal mastery for nursing leaders in healthcare organizations. Nurs. Rep. 2024, 14, 3561–3574. [Google Scholar] [CrossRef]
- Klarenbeek, S.; Schuurbiers-Siebers, O.C.J.; van den Heuvel, M.; Prokop, M.; Tummers, M. Barriers and facilitators for implementation of a computerized clinical decision support system in lung cancer multidisciplinary team meetings-a qualitative assessment. Biology 2020, 10, 9. [Google Scholar] [CrossRef]
- Ni, Y.; Wang, Y.; Wen, Z.; Fang, J.; Xu, J.; Wu, S.; Sawmadal, J.D.; Jama, H.A. Optimization path of primary public health service talent team construction: A large-scale survey in Huaihai Economic Zone, China. Front. Public Health 2024, 12, 1399857. [Google Scholar] [CrossRef]
- Albrecht, S.L.; Marty, A. Personality, self-efficacy and job resources and their associations with employee engagement, affective commitment and turnover intentions. Int. J. Hum. Resour. Manag. 2020, 31, 657–681. [Google Scholar] [CrossRef]
- Pandhi, N.; Jacobson, N.; Crowder, M.; Quanbeck, A.; Hass, M.; Davis, S. Engaging Patients in Primary Care Quality Improvement Initiatives: Facilitators and Barriers. Am. J. Med. Qual. 2020, 35, 52–62. [Google Scholar] [CrossRef] [PubMed]
- Gkliati, A.; Saiti, A. Work engagement and job satisfaction in the medical sector: Two Aspects of Psychological Well-being Among Medical Staff. Int. J. Health Sci. 2022, 6, 7753–7761. [Google Scholar] [CrossRef]
- Wei, H.; Horsley, L.; Cao, Y.; Haddad, L.; Hall, K.; Robinson, R.; Powers, M.; Anderson, D. The associations among nurse work engagement, job satisfaction, quality of care, and intent to leave: A national survey in the United States. Int. J. Nurs. Sci. 2023, 10, 476–484. [Google Scholar] [CrossRef] [PubMed]
- Nowakowska, I.; Rasińska, R. Związek wybranych czynników socjodemograficznych z wypaleniem zawodowym wśród pielęgniarek. Pielęgniarka Pol. 2014, 1, 26–33. [Google Scholar]
- Antczak-Komoterska, A.; Polak, M.; Haor, B.; Kochman, D.; Fidecki, W.; Wysokiński, M. Analiza czynników wpływających na występowanie depresji. Pielęgniarstwo Neurol. I Neurochir. 2021, 10, 126–132. [Google Scholar] [CrossRef]
- Hitka, M.; Kozubíková, Ľ.; Potkány, M. Education and gender-based differences in employee motivation. J. Bus. Econ. Manag. 2018, 19, 80–95. [Google Scholar] [CrossRef]
- Krick, A.; Felfe, J.; Hauff, S.; Renner, K.-H. Facilitating health-oriented leadership from a leader’s perspective: Antecedents at the organizational, workplace, and individual level. Z. Für Arb.-Und Organ. 2022, 66, 213–225. [Google Scholar] [CrossRef]
- Patrick, H.; Mukherjee, U. Work Engagement: A Cross Sectional Study of Employees in the Healthcare Sector. Contemp. Manag. Res. 2018, 12, 60. Available online: https://www.researchgate.net/publication/326173184_WORK_ENGAGEMENT_A_CROSS_SECTIONAL_STUDY_OF_EMPLOYEES_IN_THE_HEALTHCARE_SECTOR (accessed on 15 November 2025).
- Ceballos-Vásquez, P.; Rolo-González, G.; Hérnandez-Fernaud, E.; Díaz-Carera, D.; Paravic-Klijn, T.; Burgos-Moreno, M. Psychosocial factors and mental work load: A reality perceived by nurses in intensive care units. Rev. Lat. Am. De Enferm. 2015, 23, 315–322. [Google Scholar] [CrossRef]
- Umansky, J.; Rantanen, E. Workload in Nursing. Proc. Hum. Factors Ergon. Soc. Annu. Meet. 2016, 60, 551–555. [Google Scholar] [CrossRef]
- Werner, N.S.; Bültmann, M.; Möckel, L. Perceived stress, workload and psychosomatic complaints in inpatient and outpatient care nurses. Pflege 2023, 36, 220–227. [Google Scholar] [CrossRef] [PubMed]
- Ge, J.; He, J.; Liu, Y.; Zhang, J.; Pan, J.; Zhang, X.; Liu, D. Effects of effort-reward imbalance, job satisfaction, and work engagement on self-rated health among healthcare workers. BMC Public Health 2021, 21, 195. [Google Scholar] [CrossRef] [PubMed]
- Shuck, B.; Adelson, J.L.; Reio, T.G. The Employee Engagement Scale: Initial Evidence for Construct Validity and Implications for Theory and Practice. Hum. Resour. Manag. 2017, 56, 953–977. [Google Scholar] [CrossRef]
- Xu, J.; Thomas, H.C. How can leaders achieve high employee engagement? Leadersh. Organ. Dev. J. 2011, 32, 399–416. [Google Scholar] [CrossRef]
- Rich, B.L.; Lepine, J.A.; Crawford, E.R. Job engagement: Antecedents and effects on job performance. Acad. Manag. J. 2010, 53, 617–635. [Google Scholar] [CrossRef]
- May, D.R.; Gilson, R.L.; Harter, L.M. The psychological conditions of meaningfulness, safety and availability and the engagement of the human spirit at work. J. Occup. Organ. Psychol. 2004, 77, 11–37. [Google Scholar] [CrossRef]
- Poškiené, E.; Coudounaris, D.N.; Kazlauskaité, R. The Relationship between Caring for Employees and the Well-being of the Organisation. Manag. Organ. Syst. Res. 2020, 84, 46–60. [Google Scholar] [CrossRef]
- Top, M.; Akdere, M.; Tarcan, M. Examining transformational leadership, job satisfaction, organizational commitment and organizational trust in Turkish hospitals: Public servants versus private sector employees. Int. J. Hum. Resour. Manag. 2015, 26, 1259–1282. [Google Scholar] [CrossRef]
- Paparisabet, M.; Jalalpour, A.; Farahi, F.; Gholami, Z.; Shaygani, F.; Jalili, N.; Beigi, S.; Marzaleh, A.; Elyaderani, H. Investigating the organizational commitment and its associated factors among the staff of the health sector: A cross-sectional research. BMC Health Serv. Res. 2024, 24, 1373. [Google Scholar] [CrossRef]
- Reigas, V.; Šimanskiené, L.; Frungiliené, D.; Davidavičiené, V. The Impact of quality management practice implementatition in an organization on the psycho-emotional well-being of employees. J. Secur. Sustain. Issues 2020, 10, 593–604. [Google Scholar] [CrossRef]
- Lee, D. Impact of organizational culture and capabilities on employee commitment to ethical behavior in the healthcare sector. Serv. Bus. 2020, 14, 47–72. [Google Scholar] [CrossRef]
- Kridaningsih, A.; Agustina, R.; Nuraeni, E. Between Loyalty and Integrity: The Paradox of Organizational Support and Employee Behavior in Healthcare. INVEST J. Inov. Bisnis dan Akunt. 2025, 6, 25–34. [Google Scholar] [CrossRef]
- Qureshi, S.; Larik, A.; Bukhari, S. Role of Organizational Culture in Improving Employee Psychological Ownership. Pak. J. Appl. Soc. Sci. 2023, 14, 107–131. [Google Scholar] [CrossRef]
- Susaeta Erburu, L.; Duque, C.M.; Padilla, Y.R.; Suarez, E.; Susaeta, L. Organizational Commitment and Well-Being HR Practices: A Gender Bias Perspective for the Hospitality Industry in Spain. Tour. Int. Interdiscip. J. 2024, 72, 551–565. [Google Scholar] [CrossRef]
- Senjaya, V.; Anindita, R. The role of transformational leadership and organizational culture towards organizational commitment through job satisfaction among mining industry employees. J. Apl. Manaj. 2020, 18, 767–782. [Google Scholar] [CrossRef]
- Cramarenco, R.E.; Burcâ-Voicu, M.I.; Dabija, D.C. The impact of artificial intelligence (AI) on employees’ skills and well-being in global labor markets: A systematic review. Oeconomia Copernic. 2023, 3, 731–767. [Google Scholar] [CrossRef]
- Abuselidze, G.; Mamaladze, L. The impact of artificial intelligence on employment before and during pandemic: A comparative analysis. J. Phys. Conf. Ser. 2021, 18, 012040. [Google Scholar] [CrossRef]
- Al-Jubari, I.; Mosbah, A.; Salem, S.F. Employee well-being during COVID-19 pandemic: The role of adaptability, work-family conflict, and organizational response. Sage Open 2022, 12, 1096142. [Google Scholar] [CrossRef]
- Bellmann, L.; Hübler, O. Working from home, job satisfaction and work–life balance—Robust or heterogeneous links? Int. J. Manpow. 2020, 42, 424–441. [Google Scholar] [CrossRef]
- Davenport, T.H.; Mittal, N. How companies can prepare for the coming “AI-first” world. Strategy & Leadership. Int. J. Organ. Anal. 2023, 51, 26–30. [Google Scholar] [CrossRef]
- Dicuonzo, G.; Donofrio, F.; Fusco, A.; Shini, M. Healthcare system: Moving forward with artificial intelligence. Technovation 2023, 120, 102510. [Google Scholar] [CrossRef]
- Chatterji, M. Caring Management in the New Economy, Socially Responsible Behaviour Through Spirituality. J. Manag. Spirit. Relig. 2020, 17, 292–297. [Google Scholar] [CrossRef]
- Argyriou, C.; Dimitriadou, I.; Saridi, M.; Toska, A.; Lavdaniti, M.; Fradelos, E.C. Assessment of the relation between depression, frailty, nutrition and quality of life among older adults: Findings from a cross-sectional study in Greece. Psychogeriatrics 2024, 24, 1065–1074. [Google Scholar] [CrossRef] [PubMed]
- LaMontagne, A.D.; Martin, A.; Page, K.M.; Reavley, N.J.; Noblet, A.J.; Milner, A.J.; Keegel, T.; Smith, P.M. Workplace mental health: Developing an integrated intervention approach. BMC Psychiatry 2014, 14, 131. [Google Scholar] [CrossRef]
- Kahn, W.A. Psychological conditions of personal engagement and disengagement at work. Acad. Manag. J. 1990, 33, 692–724. [Google Scholar] [CrossRef]
- Benishek, L.E.; Kachalia, A.; Biddison, L.D. Improving Clinician Well-being and patient safety through human-centered design. JAMA J. Am. Med. Assoc. 2023, 329, 1149–1150. [Google Scholar] [CrossRef]
- Hall, L.; Johnson, J.; Watt, I.; Tsipa, A.; O’Connor, D.B. Healthcare Staff Wellbeing, Burnout, and Patient Safety: A Systematic Review. PLoS ONE 2016, 11, e0159015. [Google Scholar] [CrossRef]
- Akdere, M.; Top, M.; Tekingündüz, S. Examining patient perceptions of service quality in Turkish hospitals: The SERVPERF model. Total Qual. Manag. Bus. Excell. 2020, 31, 342–352. [Google Scholar] [CrossRef]
- Babic, A.; Gillis, N.; Hansez, I. Work-to-family interface and well-being: The role of workload, emotional load, support and recognition from supervisors. SA J. Ind. Psychol. 2020, 46, a1628. [Google Scholar] [CrossRef]
- Fatima, T.; Malik, S.A.; Shabbir, A. Hospital healthcare service quality, patient satisfaction and loyalty: An investigation in context of private healthcare systems. Int. J. Qual. Reliab. Manag. 2018, 35, 1195–1214. [Google Scholar] [CrossRef]
- Hasan, H.; Aljunid, S.M. Job satisfaction among Community-Based Rehabilitation (CBR) workers in caring for disabled persons in the east coast region of Peninsular Malaysia. BMC Public Health 2019, 19, 208. [Google Scholar] [CrossRef]
- Hurtado, D.A.; Dumet, L.M.; Greenspan, S.A.; Rodríguez, Y.I.; Heinonen, G.A. Identifying safety peer leaders with social network analysis. Occup. Health Sci. 2018, 2, 437–450. [Google Scholar] [CrossRef]
- Paillé, P. Organizational citizenship behaviour and employee retention: How important are turnover cognitions? Int. J. Hum. Resour. Manag. 2013, 24, 768–790. [Google Scholar] [CrossRef]
- de Geus, C.J.C.; Ingrams, A.; Tummers, L.; Pandey, S.K. Organizational citizenship behavior in the public sector: A systematic literature review and future research agenda. Public Adm. Rev. 2020, 80, 259–270. [Google Scholar] [CrossRef]
- Gan, J.L.; Yusof, H.M. A global research trend on organizational citizenship behaviour: A bibliometric analysis. Sustain. Bus. Soc. Emerg. Econ. 2020, 2, 55–71. [Google Scholar] [CrossRef]
- Poon, Y.S.R.; Lin, Y.P.; Griffiths, P.; Yong, K.K.; Seah, B.; Liaw, S.Y. A global overview of healthcare workers’ turnover intention amid COVID-19 pandemic: A systematic review with future directions. Hum. Resour. Health 2022, 20, 70. [Google Scholar] [CrossRef]
- Yang, S.; Zhang, L.; Wang, L. Key factors of sustainable development of organization: Bibliometric analysis of organizational citizenship behavior. Sustainability 2023, 15, 8261. [Google Scholar] [CrossRef]
- Mohamad, A.R.; Ali, K.; Mohd Noor, K. Organisational Citizenship Behaviour and Healthcare Employees’ Turnover Intention: A Bibliometric Analysis of Research Trajectories in the 21st Century. Int. J. Entrep. Manag. Pract. 2024, 7, 263–280. [Google Scholar] [CrossRef]
- Callado, A.; Teixeira, G.; Lucas, P. Turnover Intention and Organizational Commitment of Primary Healthcare Nurses. Healthcare 2023, 11, 521. [Google Scholar] [CrossRef]
- Obeng, H.; Atan, T. Understanding Turnover Intentions: The Interplay of Organizational Politics, Employee Resilience, and Person-Job Fit in Ghana’s Healthcare Sector. Sustainability 2024, 16, 9980. [Google Scholar] [CrossRef]
- Bayati, M.; Sadeghi, A.; Jamasbi, M.; Tapak, L. Servant leadership, work-life quality, and organizational citizenship behavior in nurses: A cross-sectional design. BMC Nurs. 2025, 24, 561. [Google Scholar] [CrossRef]
- Hidayat, W.; Tannady, H. Analysis of Organizational Citizenship Behavior (OCB) Variables, Work Stress, Work Communication, Work Climate Affecting Employee Performance and Turnover Intention at PT. Bank Tabungan Negara (Persero) Tbk. Cabang Gresik. Int. J. Sci. Technol. Manag. 2023, 4, 688–696. [Google Scholar] [CrossRef]
- Basu, E.; Pradhan, R.; Tewari, H. Impact of organizational citizenship behavior on job performance in Indian healthcare industries: The mediating role of social capital. Int. J. Product. Perform. Manag. 2017, 66, 780–796. [Google Scholar] [CrossRef]
- Štefko, R.; Jenčová, S.; Litavcová, E.; Vašaničová, P. Management and funding of the healthcare system. Pol. J. Manag. Stud. 2017, 16, 266–277. [Google Scholar] [CrossRef]
| Value Number | Eigenvalues of Correlation Matrix, and Related Statistics (Active Variables Only) | |||
|---|---|---|---|---|
| Eigenvalue | % Total Variance | Cumulative Eigenvalue | Cumulative % | |
| 1 | 9.853468 | 54.74149 | 9.85347 | 54.7415 |
| 2 | 1.271232 | 7.06240 | 11.12470 | 61.8039 |
| 3 | 1.019160 | 5.66200 | 12.14386 | 67.4659 |
| 4 | 0.837035 | 4.65020 | 12.98090 | 72.1161 |
| 5 | 0.726384 | 4.03547 | 13.70728 | 76.1516 |
| 6 | 0.597913 | 3.32174 | 14.30519 | 79.4733 |
| 7 | 0.483610 | 2.68672 | 14.78880 | 82.1600 |
| 8 | 0.451173 | 2.50652 | 15.23998 | 84.6665 |
| 9 | 0.405256 | 2.25142 | 15.64523 | 86.9180 |
| 10 | 0.375205 | 2.08447 | 16.02044 | 89.0024 |
| 11 | 0.336487 | 1.86937 | 16.35692 | 90.8718 |
| 12 | 0.313145 | 1.73969 | 16.67007 | 92.6115 |
| 13 | 0.296283 | 1.64602 | 16.96635 | 94.2575 |
| 14 | 0.243122 | 1.35068 | 17.20947 | 95.6082 |
| 15 | 0.226035 | 1.25575 | 17.43551 | 96.8639 |
| 16 | 0.210046 | 1.16692 | 17.64555 | 98.0309 |
| 17 | 0.189132 | 1.05073 | 17.83469 | 99.0816 |
| 18 | 0.165314 | 0.91841 | 18.00000 | 100.0000 |
| Variable | Factor Loadings (Varimax Normalized) Extraction: Principal Components (Marked Loadings Are > 0.700000) | ||
|---|---|---|---|
| Factor 1 | Factor 2 | Factor 3 | |
| PA_1 | 0.571540 | 0.464758 | 0.319909 |
| PA_2 | 0.511910 | 0.592615 | 0.271631 |
| PA_3 | 0.645115 | 0.431292 | 0.052068 |
| PA_4 | 0.333800 | 0.751369 | 0.133296 |
| PA_5 | 0.352668 | 0.756873 | 0.048166 |
| PA_6 | 0.394348 | 0.747626 | 0.135004 |
| PA_7 | 0.112367 | 0.768509 | 0.303793 |
| PA_8 | 0.737008 | 0.411117 | 0.069006 |
| PA_9 | 0.802443 | 0.244463 | 0.145500 |
| PA_10 | 0.766068 | 0.263942 | 0.215896 |
| PA_11 | 0.354525 | 0.631954 | 0.329894 |
| PA_12 | 0.741196 | 0.283659 | 0.316683 |
| PA_13 | 0.660605 | 0.313888 | 0.443738 |
| PA_14 | 0.579889 | 0.123383 | 0.553935 |
| PA_15 | 0.403600 | 0.077617 | 0.709121 |
| PA_16 | 0.500003 | 0.373187 | 0.191714 |
| PA_17 | 0.670308 | 0.346721 | 0.298616 |
| PA_18 | 0.046534 | 0.343964 | 0.780606 |
| Expl.Var | 5.494874 | 4.316013 | 2.332973 |
| Prp.Totl | 0.305271 | 0.239778 | 0.129610 |
| Effect | Univariate Tests of Significance for Factor 1. Sigma-Restricted Parameterization Effective Hypothesis Decomposition; Std. Error of Estimate: 0.8923 | ||||
|---|---|---|---|---|---|
| SS | Degr. of Freedom | MS | F | p | |
| Intercept | 0.0109 | 1 | 0.010904 | 0.013696 | 0.906990 |
| Gender | 2.0235 | 1 | 2.023514 | 2.541655 | 0.112929 |
| Age | 2.6787 | 5 | 0.535745 | 0.672929 | 0.644569 |
| Education | 5.2363 | 3 | 1.745448 | 2.192387 | 0.091199 |
| Organizational size | 0.4449 | 2 | 0.222436 | 0.279393 | 0.756625 |
| Type of the organization | 9.0504 | 2 | 4.525191 | 5.683911 | 0.004153 |
| Work position | 10.0030 | 7 | 1.428994 | 1.794903 | 0.091964 |
| Error | 122.6056 | 154 | 0.796140 | ||
| Effect | Univariate Tests of Significance for Factor 2. Sigma-Restricted Parameterization Effective Hypothesis Decomposition; Std. Error of Estimate: 0.9280 | ||||
|---|---|---|---|---|---|
| SS | Degr. of Freedom | MS | F | p | |
| Intercept | 1.3751 | 1 | 1.375097 | 1.596731 | 0.208277 |
| Gender | 0.3960 | 1 | 0.396042 | 0.459874 | 0.498700 |
| Age | 1.7611 | 5 | 0.352216 | 0.408985 | 0.842022 |
| Education | 1.2669 | 3 | 0.422298 | 0.490363 | 0.689480 |
| Organizational size | 1.4851 | 2 | 0.742551 | 0.862234 | 0.424246 |
| Type of the organization | 0.3459 | 2 | 0.172955 | 0.200832 | 0.818264 |
| Work position | 30.3089 | 7 | 4.329838 | 5.027708 | 0.000037 |
| Error | 132.6241 | 154 | 0.861195 | ||
| Effect | Univariate Tests of Significance for Factor 3. Sigma-Restricted Parameterization Effective Hypothesis Decomposition; Std. Error of Estimate: 0.9639 | ||||
|---|---|---|---|---|---|
| SS | Degr. of Freedom | MS | F | p | |
| Intercept | 0.7481 | 1 | 0.748080 | 0.805097 | 0.370983 |
| Gender | 0.0773 | 1 | 0.077284 | 0.083175 | 0.773431 |
| Age | 9.7708 | 5 | 1.954165 | 2.103107 | 0.067970 |
| Education | 0.9701 | 3 | 0.323354 | 0.348000 | 0.790645 |
| Organizational size | 1.7743 | 2 | 0.887145 | 0.954761 | 0.387185 |
| Type of organization | 2.4792 | 2 | 1.239622 | 1.334103 | 0.266441 |
| Work position | 8.5259 | 7 | 1.217982 | 1.310814 | 0.248712 |
| Error | 142.1645 | 153 | 0.929180 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Juran, V.; Kolesárová, S.; Ali Taha, V. Towards Differentiated Management: The Role of Organizational Type and Work Position in Shaping Employee Engagement Among Slovak Healthcare Professionals. Healthcare 2026, 14, 7. https://doi.org/10.3390/healthcare14010007
Juran V, Kolesárová S, Ali Taha V. Towards Differentiated Management: The Role of Organizational Type and Work Position in Shaping Employee Engagement Among Slovak Healthcare Professionals. Healthcare. 2026; 14(1):7. https://doi.org/10.3390/healthcare14010007
Chicago/Turabian StyleJuran, Veronika, Stela Kolesárová, and Viktória Ali Taha. 2026. "Towards Differentiated Management: The Role of Organizational Type and Work Position in Shaping Employee Engagement Among Slovak Healthcare Professionals" Healthcare 14, no. 1: 7. https://doi.org/10.3390/healthcare14010007
APA StyleJuran, V., Kolesárová, S., & Ali Taha, V. (2026). Towards Differentiated Management: The Role of Organizational Type and Work Position in Shaping Employee Engagement Among Slovak Healthcare Professionals. Healthcare, 14(1), 7. https://doi.org/10.3390/healthcare14010007


_Rachiotis.png)



