The Influence of Recreational Hiking on the Prevalence of Cardiovascular and Psychiatric Diseases Among Population of Republic of Serbia
Abstract
:1. Introduction
- -
- Recreational hikers have fewer risk factors for developing CVDs and PDs than the general population.
- -
- Recreational hikers less frequently report history of pre-existing CVDs and/or PDs than the general population.
- -
- Recreational hikers use fewer drugs (for a shorter time and with fewer side effects) and have a greater quality of life than the general population.
- -
- The presence of socio-demographic and other risk factors for developing CVDs and PDs.
- -
- The prevalence of different clinical entities in people with (pre-existing) CVDs and PDs.
- -
- The frequency, duration, and side effects of chronic CVD and PD pharmacotherapy.
- -
- The quality of life among the general population and recreational hikers in the RS.
2. Materials and Methods
3. Results
- A.
- Demographic data
- B.
- Risk factors for the development of chronic non-communicable diseases
- C.
- Comorbidities
- D.
- Characteristics of the hikers
- E.
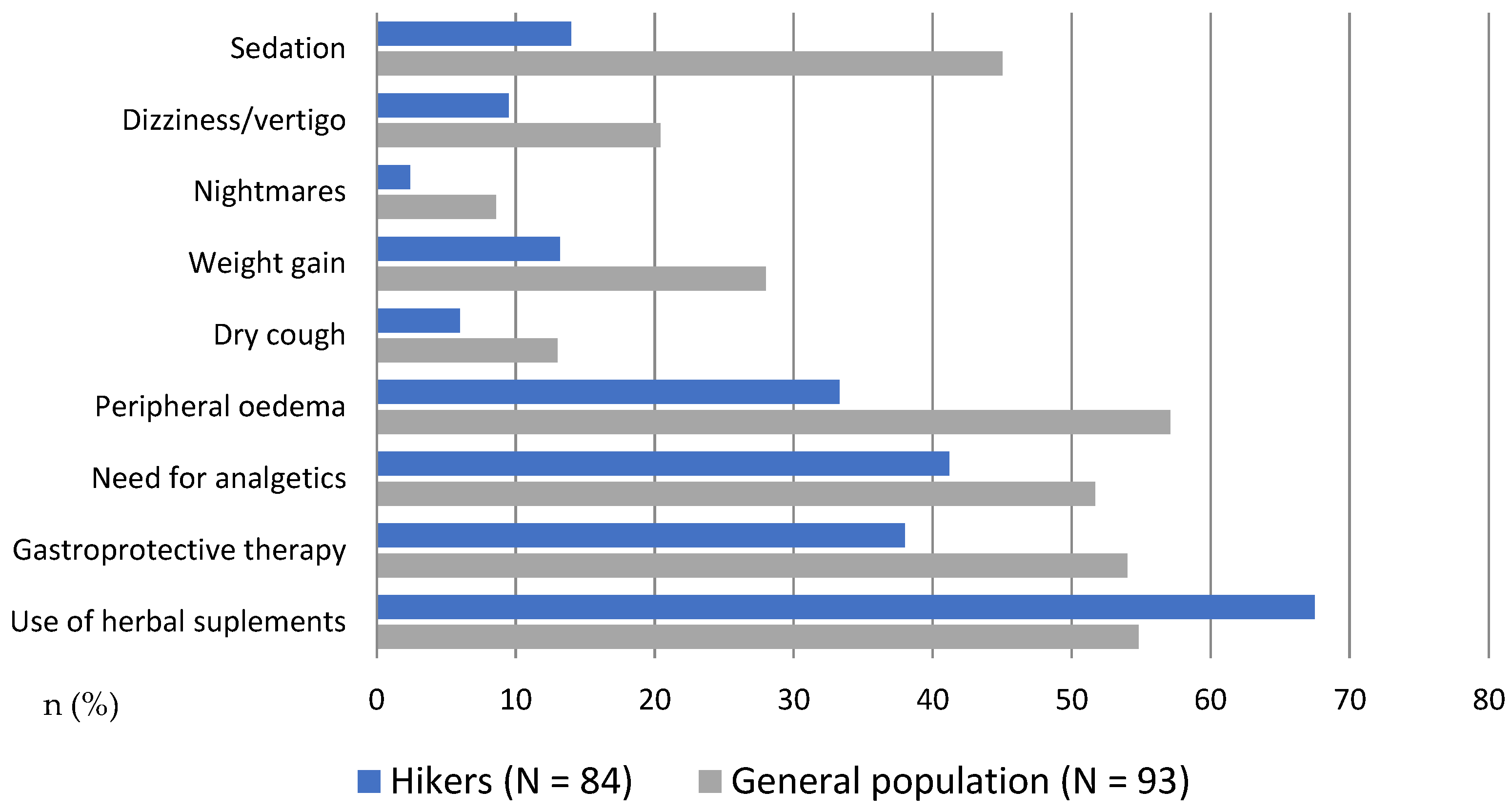
- Pharmacotherapy and side effects
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Nunan, D.; Mahtani, K.R.; Roberts, N.; Heneghan, C. Physical activity for the prevention and treatment of major chronic disease: An overview of systematic reviews. Syst. Rev. 2013, 2, 56. [Google Scholar] [CrossRef] [PubMed]
- Miko, H.C.; Zillmann, N.; Ring-Dimitriou, S.; Dorner, T.E.; Titze, S.; Bauer, R. Effects of Physical Activity on Health. Gesundheitswesen 2020, 82, S184–S195. [Google Scholar]
- Nystoriak, M.A.; Bhatnagar, A. Cardiovascular Effects and Benefits of Exercise. Front. Cardiovasc. Med. 2018, 5, 135. [Google Scholar] [CrossRef]
- Torres, W.; Maillane-Vanegas, S.; Urban, J.B.; Fernandes, R.A. Impact of sports participation on cardiovascular health markers of children and adolescents: Systematic review and meta-analysis. World J. Clin. Pediatr. 2022, 11, 375–384. [Google Scholar] [CrossRef]
- Smith, P.J.; Merwin, R.M. The Role of Exercise in Management of Mental Health Disorders: An Integrative Review. Annu. Rev. Med. 2021, 72, 45–62. [Google Scholar] [CrossRef] [PubMed]
- Park, A.H.; Zhong, S.; Yang, H.; Jeong, J.; Lee, C. Impact of COVID-19 on physical activity: A rapid review. J. Glob. Health 2022, 12, 05003. [Google Scholar] [CrossRef] [PubMed]
- Lloyd-Jones, D.; Adams, R.J.; Brown, T.M.; Carnethon, M.; Dai, S.; De Simone, G.; Ferguson, T.B.; Ford, E.; Furie, K.; Gillespie, C.; et al. Heart disease and stroke statistics—2010 update: A report from the American Heart Association. Circulation 2010, 121, e46–e215. [Google Scholar]
- Croughs, M.; Nyakunga, G.B.; Sakita, F.M.; Kilonzo, K.; Mmbaga, B.T.; Soentjens, P. Incidence and predictors of severe altitude illness symptoms in Mt. Kilimanjaro hikers: A prospective cohort study. J. Travel Med. 2022, 29, taac044. [Google Scholar] [CrossRef] [PubMed]
- Linsell, J.D.; Pelham, E.C.; Hondula, D.M.; Wardenaar, F.C. Hiking Time Trial Performance in the Heat with Real-Time Observation of Heat Strain, Hydration Status and Fluid Intake Behavior. Int. J. Environ. Res. Public Health 2020, 17, 4086. [Google Scholar] [CrossRef] [PubMed]
- Neumayr, G.; Fries, D.; Mittermayer, M.; Humpeler, E.; Klingler, A.; Schobersberger, W.; Spiesberger, R.; Pokan, R.; Schmid, P.; Berent, R. Effects of hiking at moderate and low altitude on cardiovascular parameters in male patients with metabolic syndrome: Austrian Moderate Altitude Study. Wilderness Environ. Med. 2014, 25, 329–334. [Google Scholar] [CrossRef] [PubMed]
- Greie, S.; Humpeler, E.; Gunga, H.C.; Koralewski, E.; Klingler, A.; Mittermayr, M.; Fries, D.; Lechleitner, M.; Hoertnagl, H.; Hoffmann, G.; et al. Improvement of metabolic syndrome markers through altitude specific hiking vacations. J. Endocrinol. Investig. 2006, 29, 497–504. [Google Scholar] [CrossRef] [PubMed]
- Burtscher, M. Risk of cardiovascular events during mountain activities. Adv. Exp. Med. Biol. 2007, 618, 1–11. [Google Scholar] [PubMed]
- Chobanian, A.V.; Bakris, G.L.; Black, H.R.; Cushman, W.C.; Green, L.A.; Izzo, J.L., Jr.; Jones, D.W.; Materson, B.J.; Oparil, S.; Wright, J.T., Jr.; et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003, 42, 1206–1252. [Google Scholar] [CrossRef] [PubMed]
- Andersson, C.; Vasan, R.S. Epidemiology of cardiovascular disease in young individuals. Nat. Rev. Cardiol. 2018, 15, 230–240. [Google Scholar] [CrossRef]
- Batut. Zdravstveno-Statistički Godišnjak Republike Srbije 2021. 2021. Available online: https://www.batut.org.rs/download/publikacije/pub2021a.pdf (accessed on 15 July 2024).
- Jo, C. Cost-of-illness studies: Concepts, scopes, and methods. Clin. Mol. Hepatol. 2014, 20, 327–337. [Google Scholar] [CrossRef]
- WHO. World Heart Federation Global Atlas on Cardiovascular Disease Prevention and Control. Section C: Prevention and Control of CVDs: Policies, Strategies and Interventions; WHO: Geneva, Switzerland, 2011.
- Rossi, V.A.; Schmied, C.; Niebauer, J.; Niederseer, D. Cardiovascular effects and risks of recreational alpine skiing in elderly individuals. J. Sci. Med. Sport 2019, 22 (Suppl. S1), S27–S33. [Google Scholar] [CrossRef]
- Lavie, C.J.; Ozemek, C.; Carbone, S.; Katzmarzyk, P.T.; Blair, S.N. Sedentary Behavior, Exercise, and Cardiovascular Health. Circ. Res. 2019, 124, 799–815. [Google Scholar] [CrossRef] [PubMed]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports 2020, 54, 1451–1462. [Google Scholar] [CrossRef] [PubMed]
- Andrews, G.; Slade, T. Interpreting scores on the Kessler Psychological Distress Scale (K10). Aust. N. Z. J. Public Health 2001, 25, 494–497. [Google Scholar] [CrossRef] [PubMed]
- Salem, M.; Pollack, L.; Zepeda, A.; Tebb, K.P. Utilization of online systems to promote youth participation in research: A methodological study. World J. Methodol. 2023, 13, 210–222. [Google Scholar] [CrossRef] [PubMed]
- Planinarski Savez Srbije. (Official Website). Available online: www.pss.rs (accessed on 15 January 2024).
- Lioret, S.; Campbell, K.J.; McNaughton, S.A.; Cameron, A.J.; Salmon, J.; Abbott, G.; Hesketh, K.D. Lifestyle Patterns Begin in Early Childhood, Persist and Are Socioeconomically Patterned, Confirming the Importance of Early Life Interventions. Nutrients 2020, 12, 724. [Google Scholar] [CrossRef] [PubMed]
- Coler, C.; Hoffman, M.D.; Towle, G.; Hew-Butler, T. Hyponatremia in an 85-year-old hiker: When depletion plus dilution produces delirium. Wilderness Environ. Med. 2012, 23, 153–157. [Google Scholar] [CrossRef]
- Gupta, M.; Lehl, S.S.; Singh, K.; Singh, R. Acute splenic infarction in a hiker with previously unrecognized sickle cell trait. BMJ Case Rep. 2013, 2013, bcr2013008931. [Google Scholar] [CrossRef]
- Gostimirovic, M.; Novakovic, R.; Rajkovic, J.; Djokic, V.; Terzic, D.; Putnik, S.; Gojkovic-Bukarica, L. The influence of climate change on human cardiovascular function. Arch. Environ. Occup. Health 2020, 75, 406–414. [Google Scholar] [CrossRef] [PubMed]
- Faulhaber, M.; Gatterer, H.; Burtscher, M. Preexisting cardiovascular diseases among high-altitude mountaineers in the Alps. J. Travel Med. 2011, 18, 355–357. [Google Scholar] [CrossRef]
- Faulhaber, M.; Flatz, M.; Burtscher, M. Frequency of cardiovascular diseases among ski mountaineers in the Austrian Alps. Int. J. Sports Med. 2007, 28, 78–81. [Google Scholar] [CrossRef]
- Stoltzfus, K.B.; Naylor, D.; Cattermole, T.; Ankeney, A.; Mount, R.; Chang, R.; Gibson, C.A. Blood Pressure Changes While Hiking at Moderate Altitudes: A Prospective Cohort Study. Int. J. Environ. Res. Public Health 2020, 17, 7978. [Google Scholar] [CrossRef]
- Chan You, S.; Krumholz, H.M.; Suchard, M.A.; Schuemie, M.J.; Hripcsak, G.; Chen, R.; Shea, S.; Duke, J.; Pratt, N.; Reich, C.G.; et al. Comprehensive Comparative Effectiveness and Safety of First-Line β-Blocker Monotherapy in Hypertensive Patients: A Large-Scale Multicenter Observational Study. Hypertension 2021, 77, 1528–1538. [Google Scholar] [CrossRef] [PubMed]
- Grigorieva, N.Y.; Ilushina, T.P.; Kolosova, K.S. The possibilities of using beta-blocker bisoprolol in patients with stable angina with concomitant bronchial asthma. Kardiologiia 2022, 62, 32–39. [Google Scholar] [CrossRef]
- Fijałkowski, Ł.; Skubiszewska, M.; Grześk, G.; Koech, F.K.; Nowaczyk, A. Acetylsalicylic Acid-Primus Inter Pares in Pharmacology. Molecules 2022, 27, 8412. [Google Scholar] [CrossRef]
- Turner, J.M.; Kodali, R. Should Angiotensin-Converting Enzyme Inhibitors ever be used for the Management of Hypertension? Curr. Cardiol. Rep. 2020, 22, 95. [Google Scholar] [CrossRef]
- Auer, J.; Sinzinger, H.; Franklin, B.; Berent, R. Muscle- and skeletal-related side-effects of statins: Tip of the iceberg? Eur. J. Prev. Cardiol. 2016, 23, 88–110. [Google Scholar] [CrossRef]
- Li, L.; Zhou, Y.; Zou, S.; Wang, Y. The Effects of High-Altitude Mountaineering on Cognitive Function in Mountaineers: A Meta-Analysis. Int. J. Environ. Res. Public Health 2023, 20, 5101. [Google Scholar] [CrossRef]
- Próchniak, P. Profiles of Wellbeing in Soft and Hard Mountain Hikers. Int. J. Environ. Res. Public Health 2022, 19, 7429. [Google Scholar] [CrossRef]
- Mayer, K.; Lukács, A. Motivation and mental well-being of long-distance hikers: A quantitative and qualitative approach. Heliyon 2021, 7, e06960. [Google Scholar] [CrossRef] [PubMed]
- Mau, M.; Aaby, A.; Klausen, S.H.; Roessler, K.K. Are Long-Distance Walks Therapeutic? A Systematic Scoping Review of the Conceptualization of Long-Distance Walking and Its Relation to Mental Health. Int. J. Environ. Res. Public Health 2021, 18, 7741. [Google Scholar] [CrossRef]
- Stojanović, G.; Jakovljević, B.; Nikolić Turnić, T.; Maričić, M.; Stojanović, S.; Milovanović, O. Potentially inappropriate medication prescribing among elderly patients with cardiovascular diseases. Vojn. Pregl. 2022, 79, 373–382. [Google Scholar] [CrossRef]
- Society, A.G. Updated AGS Beers Criteria® for Potentially Inappropriate Medication Use in Older Adults. J. Am. Geriatr. Soc. 2019, 67, 674–694. [Google Scholar]
- Terzić, Š.Z.; Todorović, J.; Kilibarda, B.; Mravčik, V. Non-medical prescription drug use in Serbia: Results from the national survey on lifestyles: Substance abuse and gambling. Serbian J. Med. Chamb. 2023, 4, 209–221. [Google Scholar] [CrossRef]
- Hüfner, K.; Sperner-Unterweger, B.; Brugger, H. Going to Altitude with a Preexisting Psychiatric Condition. High Alt. Med. Biol. 2019, 20, 207–214. [Google Scholar] [CrossRef] [PubMed]
- Tondo, L.; Alda, M.; Bauer, M.; Bergink, V.; Grof, P.; Hajek, T.; Lewitka, U.; Licht, R.W.; Manchia, M.; Müller-Oerlinghausen, B.; et al. Clinical use of lithium salts: Guide for users and prescribers. Int. J. Bipolar Disord. 2019, 7, 16. [Google Scholar] [CrossRef]
- Haddad, P.M.; Anderson, I.M. Antipsychotic-related QTc prolongation, torsade de pointes and sudden death. Drugs 2002, 62, 1649–1671. [Google Scholar] [CrossRef]
- Windsor, J.S.; Rodway, G.W.; Mukherjee, R.; Firth, P.G.; Shattock, M.; Montgomery, H.E. Prolongation of the corrected QT complex—a cause of sudden cardiac death in the mountain environment? J. R. Army Med. Corps. 2011, 157, 63–67. [Google Scholar] [CrossRef] [PubMed]
- UNICEF The State of the World’s Children 2021. On My Mind: Promoting, Protecting and Caring for Children’s Mental Health. How Adolescents Experience and Perceive Mental Health Around the World; UNICEF: New York, NY, USA, 2021. [Google Scholar]
- Schuch, F.B.; Vancampfort, D. Physical activity, exercise, and mental disorders: It is time to move on. Trends Psychiatry Psychother. 2021, 43, 177–184. [Google Scholar] [CrossRef] [PubMed]
- Puretz, S.L. First-aid supplies for backpacking. Br. J. Sports Med. 1992, 26, 48–50. [Google Scholar] [CrossRef] [PubMed]
- Styne, D.M.; Arslanian, S.A.; Connor, E.L.; Farooqi, I.S.; Murad, M.H.; Silverstein, J.H.; Yanovski, J.A. Pediatric Obesity-Assessment, Treatment, and Prevention: An Endocrine Society Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 2017, 102, 709–757. [Google Scholar] [CrossRef]
- Marković, L.; Đorđić, V.; Trajković, N.; Božić, P.; Halaši, S.; Cvejić, D.; Ostojić, S.M. Childhood Obesity in Serbia on the Rise. Children 2021, 8, 409. [Google Scholar] [CrossRef]
- Abernethy, L.; MacAuley, D. Impact of school sports injury. Br. J. Sports Med. 2003, 37, 354–355. [Google Scholar] [CrossRef]
- Greier, K.; Riechelmann, H. Ballspielverletzungen im Schulsport und Möglichkeiten der Prävention. Dtsch. Z. Sportmed. 2012, 63, 168–172. [Google Scholar] [CrossRef]
- Stoltzfus, K.B.; Arvanitakis, A.V.; Kennedy, L.M.; McGregor, K.R.; Zhang, B.; Hu, J. Factors Associated with Musculoskeletal Injuries While Hiking with a Backpack at Philmont Scout Ranch. Wilderness Environ. Med. 2022, 33, 59–65. [Google Scholar] [CrossRef] [PubMed]
- Bigdon, S.F.; Hecht, V.; Fairhurst, P.G.; Deml, M.C.; Exadaktylos, A.K.; Albers, C.E. Injuries in alpine summer sports—Types, frequency and prevention: A systematic review. BMC Sports Sci. Med. Rehabil. 2022, 14, 79. [Google Scholar] [CrossRef]
- Yang, P.; Dai, S.; Xu, H.; Ju, P. Perceived Environmental, Individual and Social Factors of Long-Distance Collective Walking in Cities. Int. J. Environ. Res. Public Health 2018, 15, 2458. [Google Scholar] [CrossRef] [PubMed]



| Demographic Characteristics | Hikers | General Population |
|---|---|---|
| N (%) | ||
| Age | s | |
| 18–30 | 23 (8.9) | 145 (49.7) |
| 31–40 | 58 (22.4) | 34 (11.6) |
| 41–50 | 79 (30.5) | 64 (21.9) |
| 51–60 | 58 (22.4) | 37 (12.7) |
| 61–70 | 33 (12.7) | 12 (4.1) |
| >70 | 8 (3.1) | 0 |
| Sex (Male/Female) | 107 (41.3)/152 (58.7) | 69 (23.6)/223 (76.4) * |
| Education | ||
| Primary school | 1 (0.4) | 6 (2.1) |
| High school | 61 (23.5) | 152 (52.1) |
| Higher school | 29 (11.2) | 11 (3.8) |
| Faculty | 125 (48.3) | 103 (35.3) |
| PhD studies | 43 (16.6) | 20 (6.8) |
| Employment (Yes/No) | 213 (82.2)/46 (17.8) | 155 (53.1)/137 (46.9) |
| Marriage status | ||
| Unmarried | 83 (32) | 156 (53.4) |
| Married | 103 (39.8) | 92 (31.5) |
| Divorced | 39 (15.1) | 23 (7.9) |
| Widow | 11 (4.2) | 6 (2.1) |
| Extramarital union | 23 (8.9) | 15 (5.1) |
| Living place | ||
| City | 212 (81.9) | 241 (82.5) |
| Suburb | 29 (11.2) | 34 (11.6) |
| Countryside | 18 (6.9) | 17 (5.8) |
| Risk Factors | Hikers | General Population |
|---|---|---|
| N (%) | ||
| Smoking status | ||
| Nonsmoker | 208 (80.3) | 193 (66.1) |
| <1 year | 3 (1.2) | 10 (3.4) |
| Several year | 10 (3.9) | 24 (8.2) |
| More than a decade | 38 (14.7) | 65 (22.3) |
| Alcohol consumption | ||
| Never | 75 (29) | 122 (41.8) |
| Once/week | 71 (27.4) | 76 (26) |
| Several times/week | 55 (21.2) | 30 (10.3) |
| Once/month | 58 (22.4) | 64 (21.9) |
| Unhealthy diet | ||
| No | 40 (15.4) | 27 (9.2) |
| Sometimes | 168 (64.9) | 147 (50.3) |
| Often | 29 (11.2) | 95 (32.6) |
| Every day | 9 (3.5) | 23 (7.9) |
| BMI | ||
| Underweight (<18.5) | 7 (2.7) | 15 (5.2) |
| Normal (18.5–24.9) | 152 (58.7) | 189 (64.7) |
| Overweight (25.0–29.9) | 81 (31.3) | 64 (21.9) |
| Obese (>30.0) | 19 (7.3) | 24 (8.2) |
| Blood pressure measurements | ||
| Rare | 221 (85.3) | 259 (88.7) |
| Once/week | 28 (10.8) | 22 (7.5) |
| Several times/week | 10 (3.9) | 11 (3.8) |
| CBC/serum measurements | ||
| Rare | 173 (66.8) | 136 (46.6) |
| Once/year | 83 (32) | 156 (53.4) |
| Several times/year | 3 (1.2) | 0 |
| Doctor visiting | ||
| None | 96 (46) | 83 (40.7) |
| Once/year | 73 (36.1) | 72 (35.3) |
| Several times/year | 36 (17.9) | 49 (24) |
| Comorbidities | ||
| Cardiovascular diseases | 61 (23.5) | 57 (19.5) |
| Psychiatric diseases | 17 (6.6) | 35 (12) |
| Average duration of the disease (years) ( ± SD) | 11.9 ± 10.5 * | 8.4 ± 8.7 * |
| Drug interactions | ||
| No therapy | 175 (67.6) | 199 (68.2) |
| One drug | 35 (13.5) | 45 (15.4) |
| Two drugs | 34 (13.1) | 30 (10.3) |
| More than three drugs | 15 (5.8) | 18 (6.2) |
| Family history | ||
| Cardiovascular diseases | 134 (51.7) | 157 (53.8) |
| Psychiatric diseases | 14 (5.4) | 33 (11.3) |
| Physical Activities Intensity/Frequency | Light (%) | Moderate (%) | High (%) |
|---|---|---|---|
| Everyday | 71.4/65.1 | 12.7/5.5 | 1.5/0.7 |
| 5–6 days | 11.2/12.7 | 4.6/2.4 | 1.3/1 |
| 3–4 days | 12/11.6 | 25.5/11.3 | 12.7/9.6 |
| <2 days | 4.6/9.2 | 32.8/21.9 * | 29.7/14 * |
| Never | 0.8/1.4 | 24.7/58.9 ** | 54.8/74.7 ** |
| Relevant Characteristics of the Hikers (N = 259 (100%)) | N (%) |
|---|---|
| Average years of hiking experience. n—year (s) | |
| n ≤ 2 | 30 (11.6) |
| 2 < n ≤ 5 | 75 (29) |
| 5 < n ≤ 10 | 64 (24.7) |
| 10 < n ≤ 20 | 45 (17.4) |
| 20 < n ≤ 30 | 23 (8.9) |
| 30 < n ≤ 40 | 11 (4.2) |
| 40 < n ≤ 50 | 8 (3.2) |
| 50 < n ≤ 60 | 3 (1.2) |
| Time of last hiking action | |
| Last week | 123 (47.5) |
| Last month | 57 (22) |
| Several months ago | 66 (25.5) |
| More than a year | 13 (5) |
| Main reason/motivation for hiking | |
| Mental health | 7 (2.7) |
| Physical activity | 12 (4.6) |
| Stay in nature | 46 (17.8) |
| All of the above | 194 (74.9) |
| Participation in high mountaineering (>2500 m) actions during the last year | |
| Once | 65 (25.1) |
| 2–5 | 65 (25.1) |
| More than five times | 26 (10) |
| I do not participate in actions > 2500 m altitudes | 103 (39.8) |
| Health problems during the action | 20 (7.7) |
| Symptoms | |
| Excessive/disturbing tachycardia | 11 (55) |
| Shortness of breath | 7 (35) |
| Excessive sweating | 3 (15) |
| Nausea/vomiting/GIT disturbances | 2 (10) |
| Anxiety | 1 (5) |
| Carrying the drugs on the action | 85 (32.8) |
| Hiking company (alone/group of friends) | 89 (34.4)/170 (65.6) |
| Mood after the hiking (better/same) | 252 (97.3)/7 (2.7) |
| Reduction in stress and anxiety after hiking | 249 (96.1) |
| Keeping in touch with people met on hiking trips | 219 (84.6) |
| More energy at the beginning of the working week | 229 (88.4) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gostimirovic, M.; Rajkovic, J.; Bukarica, A.; Gojkovic-Bukarica, L. The Influence of Recreational Hiking on the Prevalence of Cardiovascular and Psychiatric Diseases Among Population of Republic of Serbia. Healthcare 2025, 13, 680. https://doi.org/10.3390/healthcare13060680
Gostimirovic M, Rajkovic J, Bukarica A, Gojkovic-Bukarica L. The Influence of Recreational Hiking on the Prevalence of Cardiovascular and Psychiatric Diseases Among Population of Republic of Serbia. Healthcare. 2025; 13(6):680. https://doi.org/10.3390/healthcare13060680
Chicago/Turabian StyleGostimirovic, Milos, Jovana Rajkovic, Ana Bukarica, and Ljiljana Gojkovic-Bukarica. 2025. "The Influence of Recreational Hiking on the Prevalence of Cardiovascular and Psychiatric Diseases Among Population of Republic of Serbia" Healthcare 13, no. 6: 680. https://doi.org/10.3390/healthcare13060680
APA StyleGostimirovic, M., Rajkovic, J., Bukarica, A., & Gojkovic-Bukarica, L. (2025). The Influence of Recreational Hiking on the Prevalence of Cardiovascular and Psychiatric Diseases Among Population of Republic of Serbia. Healthcare, 13(6), 680. https://doi.org/10.3390/healthcare13060680







