Effects of Immersive Virtual Reality on Physical Function, Fall-Related Outcomes, Fatigue, and Quality of Life in Older Adults: A Randomized Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
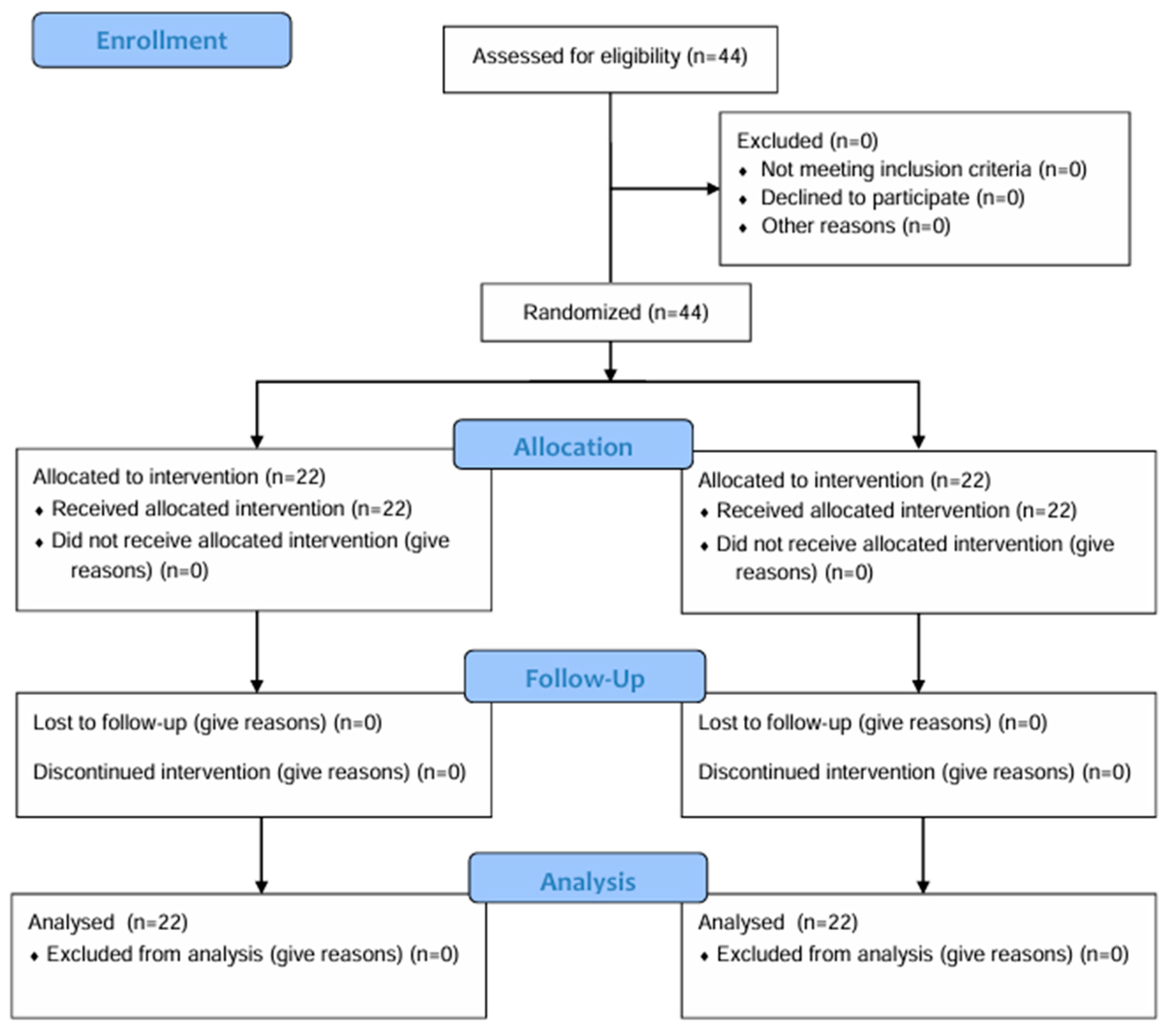
2.1. Study Design
2.2. Participants
2.3. Assessments
2.3.1. Cognitive Status
2.3.2. Balance
2.3.3. Physical Fitness
2.3.4. Risk of Falling
2.3.5. Fear of Falling
2.3.6. Fatigue
2.3.7. Quality of Life
2.3.8. Treatment Satisfaction
2.3.9. Virtual Reality Sickness
2.4. Intervention
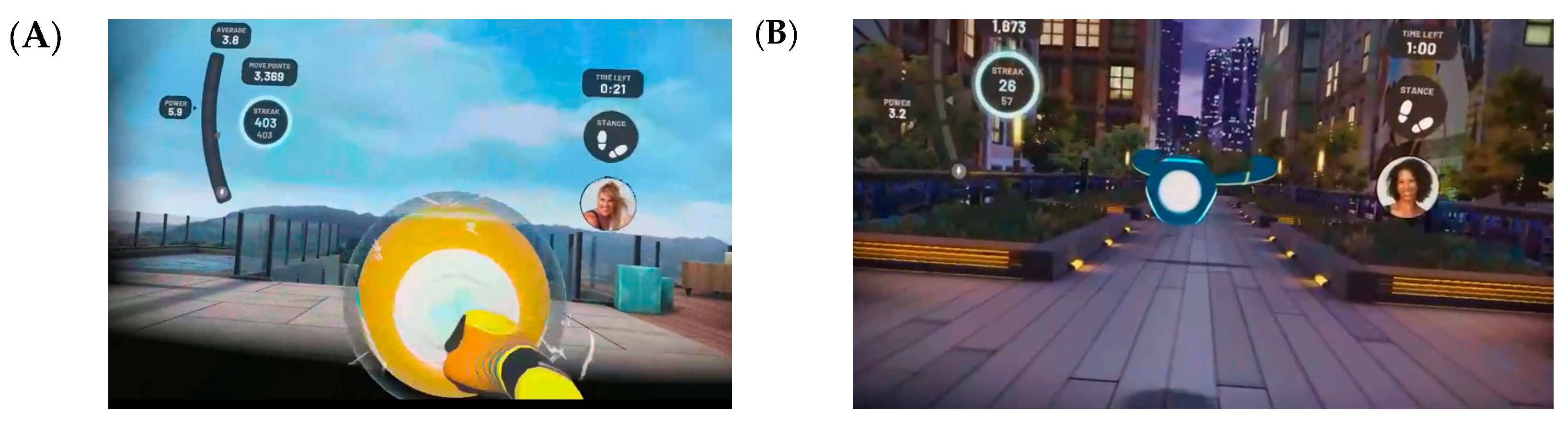
2.4.1. Immersive Virtual Reality
- Warm-up = 3 min;
- FIT-XR BOX mode = 5 min;
- Rest = 3 min;
- FIT-XR BOX mode = 5 min;
- Rest = 3 min;
- FIT-XR SLAM mode = 5 min;
- Rest = 3 min;
- FIT-XR SLAM mode = 5 min;
- Cool-down = 3 min.
- Each session lasted 35 min.
2.4.2. Active Control Group
2.5. Statistical Analysis
3. Results
4. Discussion
4.1. Balance
4.2. Physical Fitness
4.3. Risk of Falling and Fear of Falling
4.4. Fatigue
4.5. Quality of Life
4.6. Treatment Satisfaction
4.7. Virtual Reality Sickness
4.8. Limitations and Strengths
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| IVR | Immersive Virtual Reality |
| ACG | Active Control Group |
| MMST | Mini-Mental State Test |
| SFT | Senior Fitness Test |
| FAB-T | Fullerton Advanced Balance Test |
| MFS | Morse Fall Scale |
| FES-I | International Fall Efficacy Scale |
| FACIT | Fatigue Scale |
| MCDI | Minimal Clinically Important Difference |
| WHOQOL-OLD | World Health Organization Quality of Life Instrument—Older Adults Module |
| VAS | Visual Analog Scale |
| VRSQ | Virtual Reality Sickness Questionnaire |
References
- Kowal, P.; Dowd, J.E. Definition of an Older Person: Proposed Working Definition of an Older Person in Africa for the MDS Project; World Health Organization: Geneva, Switzerland, 2001. [Google Scholar] [CrossRef]
- Lutz, W.; Sanderson, W.; Scherbov, S. The coming acceleration of global population ageing. Nature 2008, 451, 716–719. [Google Scholar] [CrossRef] [PubMed]
- Sanderson, W.C.; Scherbov, S. Remeasuring aging. Science 2010, 329, 1287–1288. [Google Scholar] [CrossRef] [PubMed]
- United Nations. Decade of Healthy Ageing: 2021–2030; United Nations: New York, NY, USA, 2020; Available online: https://social.desa.un.org/sdn/decade-of-healthy-ageing-2021-2030 (accessed on 10 October 2024).
- World Health Organization. Ageing and Health Unit; World Health Organization: Geneva, Switzerland, 2020; Available online: https://www.who.int/teams/maternal-newborn-child-adolescent-health-and-ageing/ageing-and-health/research-evidence-and-data (accessed on 10 October 2024).
- Barbaccia, V.; Bravi, L.; Murmura, F.; Savelli, E.; Viganò, E. Mature and Older Adults’ Perception of Active Ageing and the Need for Supporting Services: Insights from a Qualitative Study. Int. J. Environ. Res. Public Health 2022, 19, 7660. [Google Scholar] [CrossRef] [PubMed]
- Mandıracıoğlu, A. Demographic characteristics of older adults in the world and in Turkey. Ege J. Med. 2010, 49, 39–45. [Google Scholar]
- Rikli, R.E.; Jones, C.J. Development and Validation of a Functional Fitness Test for Community-Residing Older Adults. J. Aging Phys. Act. 1999, 7, 129–161. [Google Scholar] [CrossRef]
- Toraman, A.; Yıldırım, N.Ü. The falling risk and physical fitness in older people. Arch. Gerontol. Geriatr. 2010, 51, 222–226. [Google Scholar] [CrossRef]
- Zijlstra, G.A.R.; van Haastregt, J.C.M.; van Eijk, J.T.M.; van Rossum, E.; Stalenhoef, P.A.; Kempen, G.I.J.M. Prevalence and correlates of fear of falling, and associated avoidance of activity in the general population of community-living older people. Age Ageing 2007, 36, 304–309. [Google Scholar] [CrossRef]
- Fay, B.; Horak, F. Postural control. In Encyclopedia of Neuroscience; Binder, M.D., Hirokawa, N., Windhorst, U., Eds.; Springer: Berlin/Heidelberg, Germany, 2009; pp. 3212–3219. [Google Scholar]
- Viswanathan, A.; Sudarsky, L. Balance and gait problems in the elderly. In Handbook of Clinical Neurology; Aminoff, M.J., Boller, F., Swaab, D.F., Eds.; Elsevier: Amsterdam, The Netherlands, 2012; pp. 623–634. [Google Scholar] [CrossRef]
- EuroSafe. Falls Among Older Adults in the EU-28: Key Facts from the Available Statistics. 2015. Available online: https://eupha.org/repository/sections/ipsp/Factsheet_falls_in_older_adults_in_EU.pdf (accessed on 10 January 2025).
- Muir, S.W.; Berg, K.; Chesworth, B.; Klar, N.; Speechley, M. Application of a fall screening algorithm stratified fall risk but missed preventive opportunities in community-dwelling older adults: A prospective study. J. Geriatr. Phys. Ther. 2010, 33, 165–172. [Google Scholar] [CrossRef]
- Lamb, S.E.; McCabe, C.; Becker, C.; Fried, L.P.; Guralnik, J.M. The optimal sequence and selection of screening test items to predict fall risk in older disabled women: The Women’s Health and Aging Study. J. Gerontol. A Biol. Sci. Med. Sci. 2008, 63, 1082–1088. [Google Scholar] [CrossRef]
- Gazibara, T.; Kurtagic, I.; Kisic-Tepavcevic, D.; Nurkovic, S.; Kovacevic, N.; Gazibara, T.; Pekmezovic, T. Falls, risk factors and fear of falling among persons older than 65 years of age. Psychogeriatrics 2017, 17, 215–223. [Google Scholar] [CrossRef]
- Rosenberg, D.E.; Bellettiere, J.; Gardiner, P.A.; Villarreal, V.N.; Crist, K.; Kerr, J. Independent Associations Between Sedentary Behaviors and Mental, Cognitive, Physical, and Functional Health Among Older Adults in Retirement Communities. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2015, 71, 78–83. [Google Scholar] [CrossRef] [PubMed]
- Bashkireva, A.S.; Bogdanova, D.Y.; Bilyk, A.Y.; Shishko, A.V.; Kachan, E.Y.; Arutyunov, V.A. Quality of life and physical activity among elderly and old people. Adv. Gerontol. 2018, 31, 743–750. [Google Scholar] [CrossRef] [PubMed]
- Drewnowski, A.; Evans, W.J. Nutrition, physical activity, and quality of life in older adults: Summary. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2001, 56, 89–94. [Google Scholar] [CrossRef] [PubMed]
- Hupin, D.; Roche, F.; Gremeaux, V.; Chatard, J.C.; Oriol, M.; Gaspoz, J.M.; Barthélémy, J.C.; Edouard, P. Even a low-dose of moderate-to-vigorous physical activity reduces mortality by 22% in adults aged ≥60 years: A systematic review and meta-analysis. Br. J. Sports Med. 2015, 49, 1262–1267. [Google Scholar] [CrossRef]
- Wen, C.P.; Wai, J.P.M.; Tsai, M.K.; Yang, Y.C.; Cheng, T.Y.D.; Lee, M.C.; Chan, H.T.; Tsao, C.K.; Tsai, S.P.; Wu, X. Minimum amount of physical activity for reduced mortality and extended life expectancy: A prospective cohort study. Lancet 2011, 378, 1244–1253. [Google Scholar] [CrossRef]
- Chen, W.C.; Li, Y.T.; Tung, T.H.; Chen, C.; Tsai, C.Y. The relationship between falling and fear of falling among community-dwelling elderly. Medicine 2021, 100, e26492. [Google Scholar] [CrossRef]
- Pelletier, C.; White, N.; Duchesne, A.; Sluggett, L. Rural-urban differences in individual and environmental correlates of physical activity in Canadian adults. Prev. Med. Rep. 2022, 30, 102061. [Google Scholar] [CrossRef]
- Sadrollahi, A.; Khalili, Z.; Nazari, R.P.; Mohammadi, M.; Khatir, M.A.; Mossadegh, N. Survey of the relationship between activity energy expenditure metabolic equivalents and barrier factors of physical activity in the elderly in Kashan. Iran. Red Crescent Med. J. 2016, 18, e31455. [Google Scholar] [CrossRef]
- Mäkilä, P.; Hirvensalo, M.; Parkatti, T. Changes in physical activity involvement and attitude to physical activity in a 16-year follow-up study among the elderly. J. Aging Res. 2010, 2010, 174290. [Google Scholar] [CrossRef]
- Schutzer, K.A.; Graves, B.S. Barriers and motivation to exercise in older adults. Prev. Med. 2004, 39, 1056–1061. [Google Scholar] [CrossRef]
- Aro, A.; Agbo, S.; Omole, O. Factors influencing regular physical exercise among the elderly in residential care facilities in a south african health district. Afr. J. Prim. Health Care Fam. Med. 2018, 10, a1493. [Google Scholar] [CrossRef]
- Shaikh, A.; Dandekar, S. Perceived benefits and barriers to exercise among physically active and non-active elderly people. Disabil. CBR Incl. Dev. 2019, 30, 73. [Google Scholar] [CrossRef]
- Mappanasingam, A.; Madigan, K.; Kalu, M.E.; Maximos, M.; Dal Bello-Haas, V. Engaging in and Sustaining Physical Activity and Exercise: A Descriptive Qualitative Study of Adults 65 Years and Older Using the Self-Determination Theory. J. Ageing Longev. 2024, 4, 156–176. [Google Scholar] [CrossRef]
- Hayre, C.M.; Muller, D.J.; Scherer, M.J. (Eds.) Virtual Reality in Health and Rehabilitation, 1st ed.; CRC Press: Boca Raton, FL, USA, 2020; pp. 3–6. [Google Scholar]
- Straudi, S.; Basaglia, N. Neuroplasticity-Based Technologies and Interventions for Restoring Motor Functions in Multiple Sclerosis. In Multiple Sclerosis: Bench to Bedside; Springer: Berlin/Heidelberg, Germany, 2017; pp. 171–185. [Google Scholar]
- Vilas Boas, Y.A.G. Overview of Virtual Reality Technologies. Presented at Interactive Multimedia Conference, Southampton, UK. 2012, pp. 20–26. Available online: https://static1.squarespace.com/static/537bd8c9e4b0c89881877356/t/5383bc16e4b0bc0d91a758a6/1401142294892/yavb1g12_25879847_finalpaper.pdf (accessed on 10 January 2025).
- Cacciata, M.; Stromberg, A.; Lee, J.-A.; Sorkin, D.; Lombardo, D.; Clancy, S.; Nyamathi, A.; Evangelista, L.S. Effect of exergaming on health-related quality of life in older adults: A systematic review. Int. J. Nurs. Stud. 2019, 93, 30–40. [Google Scholar] [CrossRef] [PubMed]
- Appel, L.; Appel, E.; Bogler, O.; Wiseman, M.; Cohen, L.; Ein, N.; Abrams, H.B.; Campos, J.L. Older adults with cognitive and/or physical impairments can benefit from immersive virtual reality experiences: A feasibility study. Front. Med. 2020, 6, 329. [Google Scholar] [CrossRef] [PubMed]
- Toulotte, C.; Toursel, C.; Olivier, N. Wii Fit® training vs. adapted physical activities: Which one is the most appropriate to improve the balance of independent senior subjects? A randomized controlled study. Clin. Rehabil. 2012, 26, 827–835. [Google Scholar] [CrossRef] [PubMed]
- İnal, S.H.; Subaşı, F. Geriartric rehabilitation. In New Horizons in Geriatric Medicine; Isik, A.T., Ed.; Nova Science Publishers: Hauppauge, NY, USA, 2014; Chapter 15. [Google Scholar]
- Agbangla, N.F.; Séba, M.-P.; Bunlon, F.; Snacktivity, T.M. Giant games and immersive virtual reality exercises: A rapid narrative review of these new physical activity practices among older people living in nursing homes and long-term care facilities. Healthcare 2022, 10, 1897. [Google Scholar] [CrossRef]
- Dinet, J.; Nouchi, R. Promoting physical activity for elderly people with immersive virtual reality (IVR). Hum. Factors Aging Spec. Needs 2022, 38, 206–211. [Google Scholar] [CrossRef]
- Dilanchian, A.T.; Andringa, R.; Boot, W.R. A pilot study exploring age differences in presence, workload, and cybersickness in the experience of immersive virtual reality environments. Front. Virtual Real. 2021, 2, 736793. [Google Scholar] [CrossRef]
- Gao, Y.; Wang, N.; Liu, Y.; Liu, N. Effectiveness of virtual reality in preventing falls in non-disabled older adults: A meta-analysis and systematic review. Geriatr. Nurs. 2024, 58, 15–25. [Google Scholar] [CrossRef]
- Ren, Y.; Lin, C.; Zhou, Q.; Yingyuan, Z.; Wang, G.; Lu, A. Effectiveness of virtual reality games in improving physical function, balance and reducing falls in balance-impaired older adults: A systematic review and meta-analysis. Arch. Gerontol. Geriatr. 2023, 108, 104924. [Google Scholar] [CrossRef]
- Lin, C.; Ren, Y.; Lu, A. The effectiveness of virtual reality games in improving cognition, mobility, and emotion in elderly post-stroke patients: A systematic review and meta-analysis. Neurosurg. Rev. 2023, 46, 167. [Google Scholar] [CrossRef] [PubMed]
- D’Cunha, N.; Nguyen, D.; Naumovski, N.; McKune, A.J.; Kellett, J.; Georgousopoulou, E.N.; Frost, J.; Isbel, S. A mini-review of virtual reality-based interventions to promote well-being for people living with dementia and mild cognitive impairment. Gerontology 2019, 65, 430–440. [Google Scholar] [CrossRef] [PubMed]
- Zahedian-Nasab, N.; Jaberi, A.; Shirazi, F.; Kavousipor, S. Effect of virtual reality exercises on balance and fall in elderly people with fall risk: A randomized controlled trial. BMC Geriatr. 2021, 21, 509. [Google Scholar] [CrossRef] [PubMed]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. Mini-mental state. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Güngen, C.; Ertan, T.; Eker, E.; Yaşar, R.; Engin, F. Reliability and validity of the Standardized Mini-Mental State Examination in the diagnosis of mild dementia in the Turkish population. Turk. Psikiyatri Derg. 2002, 13, 273–281. [Google Scholar]
- Rose, D.J.; Lucchese, N.; Wiersma, L.D. Development of a multidimensional balance scale for use with functionally independent older adults. Arch. Phys. Med. Rehabil. 2006, 87, 1478–1485. [Google Scholar] [CrossRef]
- Iyigun, G.; Kirmizigil, B.; Angin, E.; Oksuz, S.; Can, F.; Eker, L. The reliability and validity of the Turkish version of the Fullerton Advanced Balance (FAB-T) Scale. Arch. Gerontol. Geriatr. 2018, 78, 38–44. [Google Scholar] [CrossRef]
- Yoosefinejad, A.K.; Hadadi, M.; Eslamloo, P. Evaluating the responsiveness of the fullerton advanced balance scale in patients with lymphedema secondary to breast cancer surgery. Lymphology 2019, 52, 61–70. [Google Scholar] [CrossRef]
- Rikli, R.E.; Jones, C.J. Senior Fitness Test Manual, 2nd ed.; Human Kinetics: Champaign, IL, USA, 2013. [Google Scholar]
- Wright, A.A.; Cook, C.E.; Baxter, G.D.; Dockerty, J.D.; Abbott, J.H. A comparison of 3 methodological approaches to defining major clinically important improvement of 4 performance measures in patients with hip osteoarthritis. J. Orthop. Sports Phys. Ther. 2011, 41, 319–327. [Google Scholar] [CrossRef]
- Morse, J.M.; Morse, R.M.; Tylko, S.J. Development of a scale to identify the fall-prone patient. Can. J. Aging 1989, 8, 366–377. [Google Scholar] [CrossRef]
- Yılmaz Demir, N.; Seren İntepeler, S. Turkish adaptation of the Morse Fall Scale and determination of its sensitivity and specificity levels. Ege Univ. Nurs. Fac. J. 2012, 28, 57–71. [Google Scholar]
- Yardley, L.; Beyer, N.; Hauer, K.; Kempen, G.; Piot-Ziegler, C.; Todd, C. Development and initial validation of the Falls Efficacy Scale-International (FES-I). Age Ageing 2005, 34, 614–619. [Google Scholar] [CrossRef] [PubMed]
- Ulus, Y.; Durmuş, D.; Akyol, Y.; Terzi, Y.; Bilgici, A.; Kuru, O. Reliability and validity of the Turkish version of the Falls Efficacy Scale International (FES-I) in community-dwelling older persons. Arch. Gerontol. Geriatr. 2012, 54, 429–433. [Google Scholar] [CrossRef]
- Frith, J.; Newton, J. Fatigue Impact Scale. Occup. Med. 2010, 60, 159. [Google Scholar] [CrossRef]
- Çınar, D.; Yavaş, A. Validity and reliability of functional assessment of chronic illness treatment-fatigue scale in Turkish patients with type 2 diabetes. Endocrinol. Diabetes Nutr. (Engl. Ed.) 2018, 65, 409–417. [Google Scholar]
- Pouchot, J.; Kherani, R.B.; Brant, R.; Lacaille, D.; Lehman, A.J.; Ensworth, S.; Kopec, J.; Esdaile, J.M.; Liang, M.H. Determination of the minimal clinically important difference for seven fatigue measures in rheumatoid arthritis. J. Clin. Epidemiol. 2008, 61, 705–713. [Google Scholar] [CrossRef]
- Power, M.; Quinn, K.; Schmidt, S.; WHOQOL-OLD Group. Development of the WHOQOL-Old module. Qual. Life Res. 2005, 14, 2197–2214. [Google Scholar] [CrossRef]
- Eser, S.; Saatli, G.; Eser, E.; Baydur, H.; Fidaner, C. The World Health Organization Quality of Life Instrument-Older Adults Module (WHOQOL-OLD): Turkish version study validity and reliability results. Turk. Psikiyatri Derg. 2010, 21, 37–48. [Google Scholar]
- Kim, H.K.; Park, J.; Choi, Y.; Choe, M. Virtual reality sickness questionnaire (VRSQ): Motion sickness measurement index in a virtual reality environment. Appl. Ergon. 2018, 69, 66–73. [Google Scholar] [CrossRef]
- Çetin, H.; Zengin, H.Y.; Köse, N. Reliability and validity of the Turkish version of Virtual Reality Sickness Questionnaire: Methodological study. Turkiye Klinikleri J. Health Sci. 2024, 9, 108–117. [Google Scholar] [CrossRef]
- Slater, M.; Spanlang, B.; Sanchez-Vives, M.V.; Blanke, O. First person experience of body transfer in virtual reality. PLoS ONE 2010, 5, e10564-9. [Google Scholar] [CrossRef] [PubMed]
- Kourtesis, P.; Korre, D.; Collina, S.; Doumas, L.A.A.; MacPherson, S.E. Validation of the virtual reality everyday assessment lab (VR-EAL): An immersive virtual reality neuropsychological battery with enhanced ecological validity. J. Int. Neuropsychol. Soc. 2020, 1, 181–196. [Google Scholar] [CrossRef] [PubMed]
- Fregna, G.; Schincaglia, N.; Baroni, A.; Straudi, S.; Casile, A. A novel immersive virtual reality environment for the motor rehabilitation of stroke patients: A feasibility study. Front. Robot. AI 2022, 9, 906424. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J. Statistical Power Analysis for the Behavioural Sciences; Lawrence Erlbaum Associates: Mahwah, NJ, USA, 1988. [Google Scholar]
- Rodríguez-Almagro, D.; Achalandabaso-Ochoa, A.; Ibáñez-Vera, A.; Góngora-Rodríguez, J.; Rodríguez-Huguet, M. Effectiveness of virtual reality therapy on balance and gait in the elderly: A systematic review. Healthcare 2024, 12, 158. [Google Scholar] [CrossRef]
- Bieryla, K.A. Xbox Kinect training to improve clinical measures of balance in older adults: A pilot study. Aging Clin. Exp. Res. 2016, 28, 451–457. [Google Scholar] [CrossRef]
- Sadeghi, H.; Jehu, D.A.; Daneshjoo, A. Effects of 8 weeks of balance training, virtual training, and combined exercise on lower limb muscle strength balance, and functional mobility among older men: A randomized controlled trial: Response. Sports Health A Multidiscip. Approach 2023, 16, 667–669. [Google Scholar] [CrossRef]
- Bacha, J.M.R.; Gomes, G.C.V.; de Freitas, T.B.; Viveiro, L.A.P.; da Silva, K.G.; Bueno, G.C.; Varise, E.M.; Torriani-Pasin, C.; Alonso, A.C.; Luna, N.M.S.; et al. Effects of Kinect adventures games versus conventional physical therapy on postural control in elderly people: A randomized controlled trial. Games Health J. 2018, 7, 24–36. [Google Scholar] [CrossRef]
- Mao, Y.; Chen, P.; Li, L.; Huang, D. Virtual reality training improves balance function. Neural Regen. Res. 2014, 9, 1628–1634. [Google Scholar] [CrossRef]
- Bersotti, F.M.; Da Silva, R.P.; Vieira-Yano, B.C.D.S.; Simcsik, A.O.; Lima, D.M.T.; Barbanera, M.; Franciulli, P.M.; Caperuto, É.C.; Tanaka, C.; Ervilha, U.F.; et al. Virtual rehabilitation is better than conventional physical therapy to improve the functionality of the gait in elderly people? systematic review and meta-analysis. Mot. Rev. Educ. Física 2024, 30, e10220112. [Google Scholar] [CrossRef]
- Campo-Prieto, P.; Cancela-Carral, J.M.; Rodríguez-Fuentes, G. Feasibility and effects of an immersive virtual reality exergame program on physical functions in institutionalized older adults: A randomized clinical trial. Sensors 2022, 22, 6742. [Google Scholar] [CrossRef]
- Hong, S. A study on the effectiveness of home-based virtual reality rehabilitation training content for elderly individuals with degenerative arthritis. Phys. Ther. Rehabil. Sci. 2023, 12, 522–528. [Google Scholar] [CrossRef]
- Peng, X.; Menhas, R.; Dai, J.; Younas, M. The COVID-19 pandemic and overall well-being: Mediating role of virtual reality fitness for physical-psychological health and physical activity. Psychol. Res. Behav. Manag. 2022, 15, 1741–1756. [Google Scholar] [CrossRef] [PubMed]
- Lee, G. Effects of virtual reality exercise program on balance, emotion and quality of life in patients with cognitive decline. J. Korean Phys. Ther. 2016, 28, 355–363. [Google Scholar] [CrossRef]
- Jansons, P.; Fyfe, J.; Via, J.; Daly, R.; Scott, D. Barriers and enablers associated with participation in a home-based pragmatic exercise snacking program in older adults delivered and monitored by amazon alexa: A qualitative study. Aging Clin. Exp. Res. 2023, 35, 561–569. [Google Scholar] [CrossRef] [PubMed]
- Broderick, L.; McCullagh, R.; White, E.B.; Savage, E.; Timmons, S. Perceptions, expectations, and informal supports influence exercise activity in frail older adults. SAGE Open 2015, 5, 2158244015580850. [Google Scholar] [CrossRef]
- Duque, G.; Boersma, D.; Loza-Diaz, G.; Hassan, S.; Suarez, H.; Geisinger, D.; Suriyaarachchi, P.; Sharma, A.; Demontiero, O. Effects of balance training using a virtual-reality system in older fallers. Clin. Interv. Aging 2013, 8, 257–263. [Google Scholar] [CrossRef]
- Parijat, P.; Lockhart, T.E.; Liu, J. EMG and kinematic responses to unexpected slips after slip training in virtual reality. IEEE Trans. Biomed. Eng. 2015, 62, 593–599. [Google Scholar] [CrossRef]
- Mascarenhas, C. Effects of conventional proprioceptive training and virtual reality on functionality and fear of falling in elderly women: Randomized clinical trial. J. Clin. Med. Surg. 2023, 3, 1074. [Google Scholar] [CrossRef]
- Tavares, G.M.S.; Pacheco, B.P.; Gottlieb, M.G.V.; Müller, D.V.K.; Santos, G.M. Interaction between cognitive status, fear of falling, and balance in elderly persons. Clinics 2020, 75, e1612. [Google Scholar] [CrossRef]
- Neri, S.G.; Cardoso, J.R.; Cruz, L.; Lima, R.M.; de Oliveira, R.J.; Iversen, M.D.; Carregaro, R.L. Do virtual reality games improve mobility skills and balance measurements in community-dwelling older adults? Systematic review and meta-analysis. Clin. Rehabil. 2017, 31, 1292–1304. [Google Scholar] [CrossRef] [PubMed]
- Sánchez, Y.M.S.; Sánchez, M.A.L.; Soto, G.F.F.; Reinoso, A.R.M.; Tapia, M.A.S. Promoting elderly mobility and fall prevention through virtual reality: A sustainable approach to gait balance training. Ibero-Am. J. Educ. Soc. Res. 2024, 4, 37–45. [Google Scholar] [CrossRef]
- Kwok, B.C.; Pua, Y.H. Effects of WiiActive exercises on fear of falling and functional outcomes in community-dwelling older adults: A randomised control trial. Age Ageing 2016, 45, 621–627. [Google Scholar] [CrossRef] [PubMed]
- Park, W.; Jang, S.; Kim, Y.; Kim, G.; Son, W.; Kim, Y. A study on cyber sickness reduction by oculo-motor exercise performed immediately prior to viewing virtual reality (vr) content on head mounted display (hmd). Vibroeng. Procedia 2017, 14, 260–264. [Google Scholar] [CrossRef]
- Alhusamiah, B.; Aldiqs, M.; Zeilani, R.S. The Effectiveness of Immersive Virtual Reality as A Complementary Approach and a New Direction in Cancer Related Fatigue Management. Integr. Cancer Ther. 2024, 23, 15347354241280272. [Google Scholar] [CrossRef]
- Gani, H.; Gunawan, H.; Gunawan, I. Effectiveness of virtual reality on fatigue and life quality in geriatric patients at Kasih nursing home Cirebon, Indonesia. Glob. Health Manag. J. 2024, 7, 245–253. [Google Scholar] [CrossRef]
- Jeon, S.; Kim, J. Effects of augmented-reality-based exercise on muscle parameters, physical performance, and exercise self-efficacy for older adults. Int. J. Environ. Res. Public Health 2020, 17, 3260. [Google Scholar] [CrossRef]
- Huang, W.; Wu, C. Predict the exercise behavior intention of the older adults in Taipei City to promote exercise behavior. Sci. Prog. 2021, 104 (Suppl. S3), 00368504211042468. [Google Scholar] [CrossRef]
- Hughes, S.; Warren-Norton, K.; Spadafora, P.; Tsotsos, L. Supporting optimal aging through the innovative use of virtual reality technology. Multimodal Technol. Interact. 2017, 1, 23. [Google Scholar] [CrossRef]
- He, X. The application and improvement of virtual reality technology in the field of pension. In Proceedings of the 2023 2nd International Conference on Educational Innovation and Multimedia Technology (EIMT 2023), Nanchang, China, 17–19 March 2023; Atlantis Highlights in Social Sciences, Education and Humanities. Atlantis Press: Dordrecht, The Netherlands, 2023; pp. 551–556. [Google Scholar] [CrossRef]
- Mosadeghi, S.; Reid, M.; Martinez, B.; Rosen, B.; Spiegel, B. Feasibility of an immersive virtual reality intervention for hospitalized patients: An observational cohort study. JMIR Ment. Health 2016, 3, e28. [Google Scholar] [CrossRef]
- Seran, E.; Haryanto, J.; Ulfiana, E. The effect of virtual reality on cognitive functions in ladies with dementia: Literature review. J. Vocat. Nurs. 2021, 2, 1–9. [Google Scholar] [CrossRef]
- Manera, V.; Chapoulie, E.; Bourgeois, J.; Guerchouche, R.; David, R.; Ondrej, J.; Drettakis, G.; Robert, P.; Chao, L. A feasibility study with image-based rendered virtual reality in patients with mild cognitive impairment and dementia. PLoS ONE 2016, 11, e0151487. [Google Scholar] [CrossRef]
- Monteagudo, P.; Cordellat, A.; Roldán, A.; Pesce, C.; Blasco-Lafarga, C. Assessing health-related quality of life in older adults: Euroqol five-dimensional questionnaire vs the short form health survey. Sport Mont. 2020, 18, 117–120. [Google Scholar] [CrossRef]
- Bilika, P.; Karampatsou, N.; Stavrakakis, G.; Paliouras, A.; Theodorakis, Y.; Strimpakos, N.; Kapreli, E. Virtual reality-based exercise therapy for patients with chronic musculoskeletal pain: A scoping review. Healthcare 2023, 11, 2412. [Google Scholar] [CrossRef] [PubMed]
- Rakesh, V.; Ramachandran, A.; Vasanthi, R. Challenges and practical considerations in applying virtual reality among Tamil geriatric patients with periarthritis shoulder—A qualitative study. J. Ecophysiol. Occup. Health 2024, 24, 449–453. [Google Scholar] [CrossRef]
- Dockx, K.; Alcock, L.; Bekkers, E.; Ginis, P.; Reelick, M.; Pelosin, E.; Lagravinese, G.; Hausdorff, J.M.; Mirelman, A.; Rochester, L.; et al. Fall-Prone Older People’s Attitudes towards the Use of Virtual Reality Technology for Fall Prevention. Gerontology 2017, 63, 590–598. [Google Scholar] [CrossRef] [PubMed]
- Hsiang, E.L.; Yang, Z.; Yang, Q.; Lai, P.C.; Lin, C.L.; Wu, S.T. AR/VR light engines: Perspectives and challenges. Adv. Opt. Photonics 2022, 14, 783–861. [Google Scholar] [CrossRef]
- Yin, K.; Hsiang, E.L.; Zou, J.; Li, Y.; Yang, Z.; Yang, Q.; Lai, P.C.; Lin, C.L.; Wu, S.T. Advanced liquid crystal devices for augmented reality and virtual reality displays: Principles and applications. Light Sci. Appl. 2022, 11, 161. [Google Scholar] [CrossRef]
- Kang, S.; Yang, Y.; Kim, G.; Kim, H. BalanceVR: VR-based balance training to increase tolerance to vr sickness. Virtual Real. 2025, 29, 39. [Google Scholar] [CrossRef]



| IVR Group (n = 22) | ACG (n = 22) | Total | t/X2 | p | ||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |||
| Gender | ||||||||
| Female | 18 | 81.82 | 18 | 81.82 | 36 | 81.82 | 0.000 | 1.000 |
| Male | 4 | 18.18 | 4 | 18.18 | 8 | 18.18 | ||
| Age | 71.14 ± 4.83 | 75.36 ± 9.16 | 73.25 ± 7.55 | −1.914 | 0.062 | |||
| Employment Status | ||||||||
| Not Working | 0 | 0.00 | 1 | 4.55 | 1 | 2.27 | - | - |
| Retired | 1 | 4.55 | 5 | 22.73 | 6 | 13.64 | ||
| Housewife | 16 | 72.73 | 15 | 68.18 | 31 | 70.45 | ||
| Other | 5 | 22.73 | 1 | 4.55 | 6 | 13.64 | ||
| Smoking | ||||||||
| Yes | 5 | 22.73 | 7 | 31.82 | 12 | 27.27 | 0.458 | 0.498 |
| No | 17 | 77.27 | 15 | 68.18 | 32 | 72.73 | ||
| Alcohol Consumption | ||||||||
| No | 22 | 100.00 | 22 | 100.00 | 44 | 100.00 | ||
| Any Illness | ||||||||
| Yes | 16 | 72.73 | 16 | 72.73 | 32 | 72.73 | 0.000 | 1.000 |
| No | 6 | 27.27 | 6 | 27.27 | 12 | 27.27 | ||
| Illness | ||||||||
| Hypertension | 14 | 63.64 | 12 | 54.55 | 26 | 59.09 | - | - |
| Diabetes | 5 | 22.73 | 8 | 36.36 | 13 | 29.55 | - | - |
| Medications | ||||||||
| Yes | 15 | 68.18 | 16 | 72.73 | 31 | 70.45 | 0.109 | 0.741 |
| No | 7 | 31.82 | 6 | 27.27 | 13 | 29.55 | ||
| History of Falls | ||||||||
| No | 5 | 22.73 | 6 | 27.27 | 11 | 25.00 | 0.158 | 0.924 |
| 1–2 times | 9 | 40.91 | 9 | 40.91 | 18 | 40.91 | ||
| More than 2 | 8 | 36.36 | 7 | 31.82 | 15 | 34.09 | ||
| Intervention Group | n | s | t | p | ||
|---|---|---|---|---|---|---|
| Height (cm) | IVR | 22 | 161.55 | 7.95 | 0.702 | 0.487 |
| ACG | 22 | 159.86 | 7.94 | |||
| Weight (kg) | IVR | 22 | 73.77 | 13.12 | 0.784 | 0.437 |
| ACG | 22 | 70.50 | 14.53 | |||
| Body Mass Index (kg/m2) | IVR | 22 | 28.37 | 5.51 | 0.544 | 0.590 |
| ACG | 22 | 27.52 | 4.80 |
| Group | Pre-Test | Post-Test | F | p3 | η2 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| s | p1 | s | p2 | |||||||
| MMST | IVR | 25.86 | 1.55 | 0.866 | 26.59 | 1.22 | 0.239 | 2.923 | 0.095 | 0.067 |
| ACG | 25.95 | 1.96 | 26.05 | 1.76 | ||||||
| Group | Pre-Test | Post-Test | F | p3 | η2 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| s | p1 | s | p2 | |||||||
| FAB-T | IVR | 28.77 | 4.68 | 0.403 | 34.50 | 3.81 | 0.008 * | 14.336 | 0.000 * | 0.259 |
| ACG | 27.32 | 6.59 | 30.18 | 6.13 | ||||||
| Group | Pre-Test | Post-Test | F | p3 | η2 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| s | p1 | s | p2 | |||||||
| Sit-to-stand test | IVR | 12.09 | 3.21 | 0.147 | 13.86 | 2.38 | 0.010 * | 5.301 | 0.026 * | 0.114 |
| ACG | 10.73 | 2.91 | 11.82 | 2.67 | ||||||
| Weightlifting | IVR | 14.73 | 2.21 | 0.901 | 17.09 | 1.60 | 0.000 * | 30.683 | 0.000 * | 0.428 |
| ACG | 14.64 | 2.59 | 14.82 | 1.97 | ||||||
| Two-minute step test | IVR | 59.14 | 9.79 | 0.533 | 63.86 | 10.61 | 0.822 | 2.586 | 0.116 | 0.059 |
| ACG | 61.55 | 15.06 | 63.05 | 13.27 | ||||||
| Sit-and-reach test | IVR | 3.55 | 7.24 | 0.084 | 4.73 | 7.03 | 0.032 * | 6.733 | 0.013 * | 0.141 |
| ACG | 0.23 | 4.97 | 0.50 | 5.48 | ||||||
| Back scratch test | IVR | −12.95 | 9.57 | 0.774 | −11.82 | 8.92 | 0.600 | 1.719 | 0.197 | 0.040 |
| ACG | −13.70 | 7.48 | −13.14 | 7.57 | ||||||
| Eight-step walk test | IVR | 5.86 | 0.90 | 0.497 | 5.59 | 0.92 | 0.623 | 0.006 | 0.937 | 0.000 |
| ACG | 6.07 | 1.12 | 5.74 | 1.08 | ||||||
| Group | Pre-Test | Post-Test | F | p3 | η2 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| s | p1 | s | p2 | |||||||
| MFS | IVR | 18.18 | 14.19 | 0.821 | 13.64 | 11.25 | 0.463 | 1.692 | 0.201 | 0.040 |
| ACG | 17.27 | 12.22 | 16.14 | 11.12 | ||||||
| FES-I | IVR | 21.95 | 5.46 | 0.486 | 19.32 | 5.06 | 0.106 | 2.727 | 0.106 | 0.062 |
| ACG | 23.41 | 8.02 | 21.82 | 4.98 | ||||||
| Group | Pre-Test | Post-Test | F | p3 | η2 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| s | p1 | s | p2 | |||||||
| FACIT | IVR | 11.77 | 9.70 | 0.689 | 7.50 | 5.93 | 0.072 | 5.172 | 0.028 * | 0.112 |
| ACG | 12.91 | 8.99 | 10.82 | 6.00 | ||||||
| Group | Pre-Test | Post-Test | F | p3 | η2 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| s | p1 | s | p2 | |||||||
| Sensory functions | IVR | 8.41 | 1.71 | 0.125 | 8.64 | 1.71 | 0.073 | 1.110 | 0.298 | 0.026 |
| ACG | 9.32 | 2.12 | 9.55 | 1.57 | ||||||
| Autonomy | IVR | 15.95 | 2.61 | 0.055 | 16.68 | 2.80 | 0.027 * | 2.344 | 0.133 | 0.054 |
| ACG | 14.09 | 3.57 | 14.18 | 4.27 | ||||||
| Past, present, and future activities | IVR | 15.82 | 2.15 | 0.059 | 16.45 | 2.24 | 0.320 | 0.283 | 0.598 | 0.007 |
| ACG | 14.09 | 3.58 | 15.45 | 4.09 | ||||||
| Social participation | IVR | 14.68 | 3.62 | 0.015 * | 15.14 | 2.38 | 0.009 * | 1.551 | 0.220 | 0.036 |
| ACG | 11.91 | 3.65 | 12.64 | 3.58 | ||||||
| Dying and death | IVR | 8.55 | 3.71 | 0.582 | 8.41 | 3.39 | 0.498 | 0.162 | 0.689 | 0.004 |
| ACG | 9.18 | 3.89 | 9.14 | 3.66 | ||||||
| Closeness | IVR | 16.73 | 2.76 | 0.305 | 16.95 | 2.63 | 0.958 | 0.689 | 0.411 | 0.017 |
| ACG | 15.82 | 3.03 | 16.91 | 3.05 | ||||||
| WHOQOL-OLD Total | IVR | 80.27 | 8.18 | 0.039 * | 83.86 | 9.81 | 0.055 | 0.896 | 0.349 | 0.021 |
| ACG | 74.41 | 9.97 | 77.64 | 11.04 | ||||||
| Group | n | s | t | p | ||
|---|---|---|---|---|---|---|
| VAS | IVR | 22 | 9.32 | 1.09 | 4.649 | 0.000 * |
| ACG | 22 | 7.45 | 1.54 |
| n | s | Min | Max | ||
|---|---|---|---|---|---|
| VRSQ | 22 | 0.09 | 0.29 | 0 | 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Parmak, D.; Angın, E.; Iyigun, G. Effects of Immersive Virtual Reality on Physical Function, Fall-Related Outcomes, Fatigue, and Quality of Life in Older Adults: A Randomized Controlled Trial. Healthcare 2025, 13, 1800. https://doi.org/10.3390/healthcare13151800
Parmak D, Angın E, Iyigun G. Effects of Immersive Virtual Reality on Physical Function, Fall-Related Outcomes, Fatigue, and Quality of Life in Older Adults: A Randomized Controlled Trial. Healthcare. 2025; 13(15):1800. https://doi.org/10.3390/healthcare13151800
Chicago/Turabian StyleParmak, Damla, Ender Angın, and Gozde Iyigun. 2025. "Effects of Immersive Virtual Reality on Physical Function, Fall-Related Outcomes, Fatigue, and Quality of Life in Older Adults: A Randomized Controlled Trial" Healthcare 13, no. 15: 1800. https://doi.org/10.3390/healthcare13151800
APA StyleParmak, D., Angın, E., & Iyigun, G. (2025). Effects of Immersive Virtual Reality on Physical Function, Fall-Related Outcomes, Fatigue, and Quality of Life in Older Adults: A Randomized Controlled Trial. Healthcare, 13(15), 1800. https://doi.org/10.3390/healthcare13151800





