Effects of Vibration Foam Rolling on Pain, Fatigue, and Range of Motion in Individuals with Muscle Fatigue: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Eligibility Criteria
2.3. Search Strategy
2.4. Study Selection and Data Extraction
2.5. Methodological Quality Assessment
3. Results
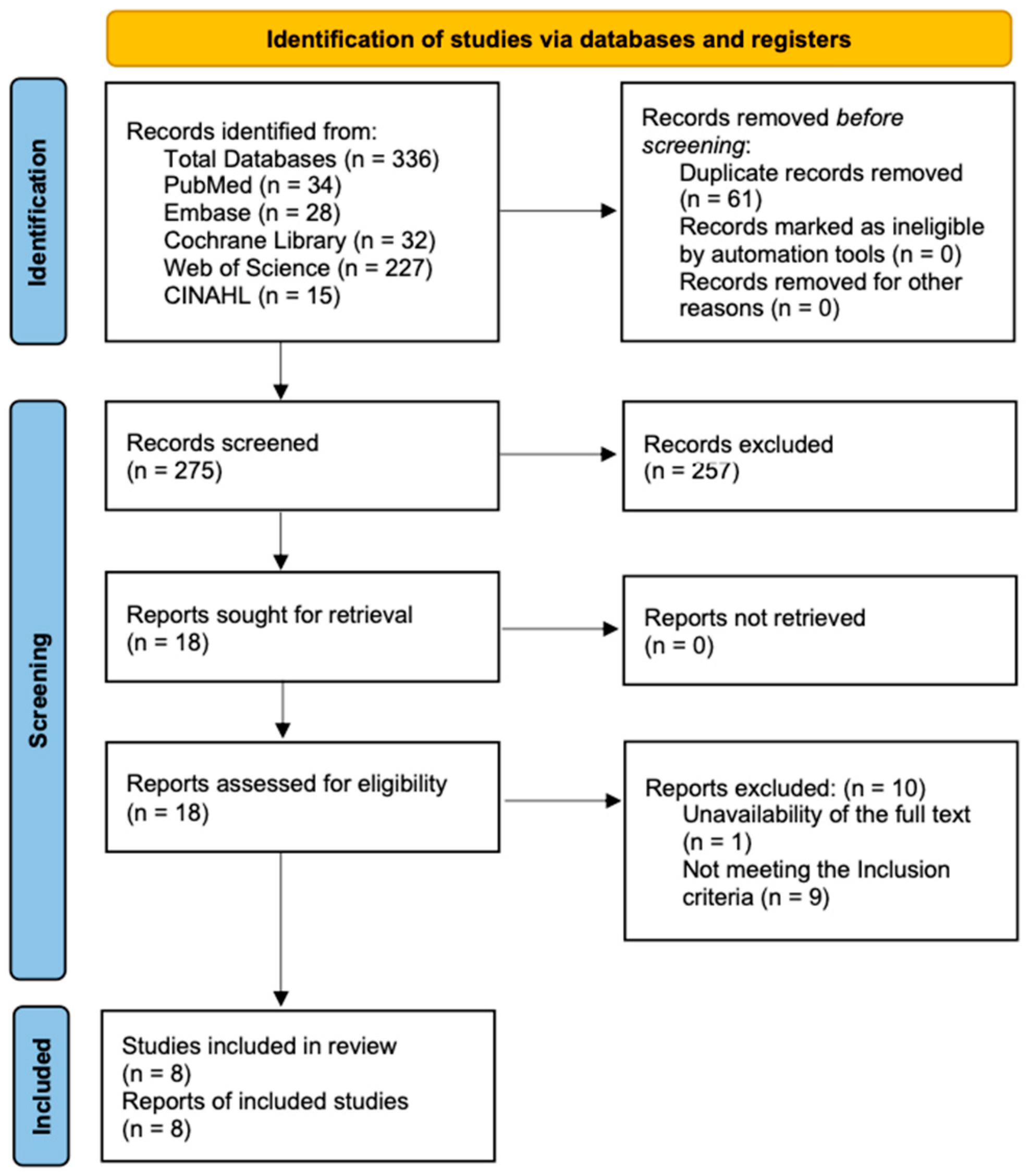
3.1. Search Results
3.2. Characteristics of Included Studies
3.3. Methodological Quality
3.4. Effects on Pain
3.5. Effects on Fatigue
3.6. Effects on Range of Motion
4. Discussion
4.1. Effects on Pain
4.2. Effects on Fatigue
4.3. Effects on Range of Motion
4.4. Clinical Implications
4.5. Limitations and Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ROM | Range of motion |
| VFR | Vibration foam roller |
| NVFR | Non-vibration foam roller |
| RCT | Randomized controlled trial |
| JBI | Joanna Briggs Institute |
| VAS | Visual analog scale |
| PPT | Pressure pain threshold |
| SmO2 | Muscle oxygen saturation |
| DOMS | Delayed onset muscle soreness |
References
- Enoka, R.M.; Duchateau, J. Muscle fatigue: What, why and how it influences muscle function. J. Phys. 2008, 586, 11–23. [Google Scholar] [CrossRef]
- Whittaker, R.L.; Sonne, M.W.; Potvin, J.R. Ratings of perceived fatigue predict fatigue induced declines in muscle strength during tasks with different distributions of effort and recovery. J. Electromyogr. Kinesiol. 2019, 47, 88–95. [Google Scholar] [CrossRef] [PubMed]
- Mastaglia, F.L. The relationship between muscle pain and fatigue. Neuromuscul. Disord 2012, 22, S178–S180. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Yang, H.; Ma, G.; Gong, M.; Niu, W.; Lu, T. Grey Relational Analysis of Lower Limb Muscle Fatigue and Pedalling Performance Decline of Elite Athletes during a 30-Second All-Out Sprint Cycling Exercise. J. Healthc. Eng. 2021, 2021, 6755767. [Google Scholar] [CrossRef]
- Tang, Y.; Li, Y.; Yang, M.; Zheng, X.; An, B.; Zheng, J. The effect of hip abductor fatigue on knee kinematics and kinetics during normal gait. Front. Neurosci. 2022, 16, 1003023. [Google Scholar] [CrossRef] [PubMed]
- Bhati, P.; Singla, D.; Masood, S.; Hussain, M.E. Type 2 Diabetes Mellitus Patients Manifest Greater Muscle Fatigability Than Healthy Individuals During Dynamic Fatigue Protocol. J. Manip. Phys. Ther. 2021, 44, 205–220. [Google Scholar] [CrossRef]
- Tajali, S.; Roozbehfar, N.; Mehravar, M.; Goharpey, S.; Gayem, K. Effects of back extensor and hip abductor fatigue on dynamic postural stability in patients with nonspecific chronic low back pain: A case-control study. Physiother. Theory Pract. 2022, 38, 1987–1995. [Google Scholar] [CrossRef]
- Cheatham, S.W.; Kolber, M.J.; Cain, M.; Lee, M. The Effects of Self-Myofascial Release Using A Foam Roll or Roller Massager on Joint Range of Motion, Muscle Recovery, and Performance: A Systematic Review. Int. J. Sports Phys. Ther. 2015, 10, 827–838. [Google Scholar]
- Michalak, B.; Kopiczko, A.; Gajda, R.; Adamczyk, J.G. Recovery effect of self-myofascial release treatment using different type of a foam rollers. Sci. Rep. 2024, 14, 15762. [Google Scholar] [CrossRef]
- França, M.E.D.; Amorim, M.D.S.; Sinhorim, L.; Santos, G.M.; do Nascimento, I.B. Myofascial release strategies and technique recommendations for athletic performance: A systematic review. J. Bodyw. Mov. Ther. 2023, 36, 30–37. [Google Scholar] [CrossRef]
- Alonso-Calvete, A.; Padrón-Cabo, A.; Lorenzo-Martínez, M.; Rey, E. Acute Effects of Foam Rolling on Blood Flow Measured by Ultrasonography in Soccer Players. J. Strength Cond. Res. 2021, 35, 3256–3259. [Google Scholar] [CrossRef] [PubMed]
- Park, S.J.; Lee, S.I.; Jeong, H.J.; Kim, B.G. Effect of vibration foam rolling on the range of motion in healthy adults: A systematic review and meta-analysis. J. Exerc. Rehabil. 2021, 17, 226–233. [Google Scholar] [CrossRef] [PubMed]
- Alonso-Calvete, A.; Lorenzo-Martínez, M.; Padrón-Cabo, A.; Pérez-Ferreirós, A.; Kalén, A.; Abelairas-Gómez, C.; Rey, E. Does Vibration Foam Roller Influence Performance and Recovery? A Systematic Review and Meta-analysis. Sports Med. Open 2022, 8, 32. [Google Scholar] [CrossRef] [PubMed]
- Padrón-Cabo, A.; Alonso-Calvete, A.; Radzimiński, Ł.; Rey, E.; Lorenzo-Martínez, M. Acute Effects of Foam Rolling vs. Vibration Foam Rolling on Blood Flow Parameters in Professional Soccer Players: A Randomized Crossover Design. J. Strength Cond. Res. 2024, 38, 1885–1890. [Google Scholar]
- Park, S.J.; Jeong, H.J.; Kim, B.G. Effects of vibration rolling on ankle range of motion and ankle muscle stiffness in stroke patients: A randomized crossover study. J. Int. Acad. Phys. Ther. Res. 2021, 12, 2272–2278. [Google Scholar] [CrossRef]
- Kasahara, K.; Yoshida, R.; Yahata, K.; Sato, S.; Murakami, Y.; Aizawa, K.; Konrad, A.; Nakamura, M. Comparison of the Acute Effects of Foam Rolling with High and Low Vibration Frequencies on Eccentrically Damaged Muscle. J. Sports Sci. Med. 2022, 21, 112–119. [Google Scholar] [CrossRef]
- Nakamura, M.; Kasahara, K.; Yoshida, R.; Murakami, Y.; Koizumi, R.; Sato, S.; Takeuchi, K.; Nishishita, S.; Ye, X.; Konrad, A. Comparison of The Effect of High- and Low-Frequency Vibration Foam Rolling on The Quadriceps Muscle. J. Sports Sci. Med. 2022, 21, 376–382. [Google Scholar] [CrossRef]
- Kim, S.Y.; Lim, J.H.; Park, C.B.; Kim, B.G. Immediate effects of a vibrating foam roller on dorsiflexion rom, balance, and gait in stroke patients: A randomized controlled trial. J. Exerc. Rehabil. 2024, 20, 76–82. [Google Scholar] [CrossRef]
- Park, C.B.; Cho, W.S.; Kim, B.G. Effects of Intervention Using Vibration Stimulation on Balance and Gait in Total Hip Replacement Elderly Patients. J. Int. Acad. Phys. Ther. Res. 2022, 13, 2670–2675. [Google Scholar]
- Romero-Moraleda, B.; González-García, J.; Cuéllar-Rayo, Á.; Balsalobre-Fernández, C.; Muñoz-García, D.; Morencos, E. Effects of Vibration and Non-Vibration Foam Rolling on Recovery after Exercise with Induced Muscle Damage. J. Sports Sci. Med. 2019, 18, 172–180. [Google Scholar]
- Lai, Y.H.; Wang, A.Y.; Yang, C.C.; Guo, L.Y. The Recovery Benefit on Skin Blood Flow Using Vibrating Foam Rollers for Postexercise Muscle Fatigue in Runners. Int. J. Environ. Res. Public Health 2020, 17, 9118. [Google Scholar] [CrossRef] [PubMed]
- de Benito, A.M.; Valldecabres, R.; Ceca, D.; Richards, J.; Barrachina Igual, J.; Pablos, A. Effect of vibration vs non-vibration foam rolling techniques on flexibility, dynamic balance and perceived joint stability after fatigue. PeerJ 2019, 7, e8000. [Google Scholar] [CrossRef] [PubMed]
- Haddaway, N.R.; Page, M.J.; Pritchard, C.C.; McGuinness, L.A. PRISMA2020: An R package and Shiny app for producing PRISMA 2020-compliant flow diagrams, with interactivity for optimised digital transparency and Open Synthesis. Campbell Syst. Rev. 2022, 18, e1230. [Google Scholar] [CrossRef]
- Barker, T.H.; Stone, J.C.; Sears, K.; Klugar, M.; Tufanaru, C.; Leonardi-Bee, J.; Aromataris, E.; Munn, Z. The revised JBI critical appraisal tool for the assessment of risk of bias for randomized controlled trials. JBI. Evid. Synth. 2023, 21, 494–506. [Google Scholar] [CrossRef] [PubMed]
- Barker, T.H.; Habibi, N.; Aromataris, E.; Stone, J.C.; Leonardi-Bee, J.; Sears, K.; Hasanoff, S.; Klugar, M.; Tufanaru, C.; Moola, S.; et al. The revised JBI critical appraisal tool for the assessment of risk of bias for quasi-experimental studies. JBI. Evid. Synth. 2024, 22, 378–388. [Google Scholar] [CrossRef]
- Zhu, M. Fatigue and physical recovery in basketball under covid-19. Revista. Bras. Med. Esporte 2023, 29, e2022_0695. [Google Scholar] [CrossRef]
- Chang, Y.C.; Tseng, W.C.; Chiu, C.H.; Hsieh, T.Y.; Chang, C.K.; Dai, X.; Chen, C.H. The effects of a preconditioning vibration rolling warm-up on multidirectional repeated sprinting-induced muscle damage. Eur. J. Sport. Sci. 2024, 24, 36–44. [Google Scholar] [CrossRef]
- Nakamura, M.; Kasahara, K.; Yoshida, R.; Yahata, K.; Sato, S.; Murakami, Y.; Aizawa, K.; Konrad, A. The Effect of Static Compression via Vibration Foam Rolling on Eccentrically Damaged Muscle. Int. J. Environ. Res. Public Health 2022, 19, 1823. [Google Scholar] [CrossRef]
- Nakamura, M.; Kasahara, K.; Yoshida, R.; Yahata, K.; Sato, S.; Murakami, Y.; Aizawa, K.; Konrad, A. Cross-education effect of vibration foam rolling on eccentrically damaged muscles. J. Musculoskelet. Neuronal Interact. 2022, 22, 369–374. [Google Scholar]
- Alonso-Calvete, A.; Lage-Rey, A.; Lorenzo-Martínez, M.; Rey, E. Does a short intervention with vibration foam roller recover lifeguards better after a water rescue? A pilot study. Am. J. Emerg. Med. 2021, 49, 71–75. [Google Scholar] [CrossRef]
- Meechan, J.G. Intraoral topical anesthesia. Periodontology 2008, 46, 56–79. [Google Scholar] [CrossRef] [PubMed]
- Melzack, R.; Wall, P.D. Pain mechanisms: A new theory. Science 1965, 150, 971–979. [Google Scholar] [CrossRef] [PubMed]
- Porritt, J.; Marshman, Z.; Rodd, H.D. Understanding children’s dental anxiety and psychological approaches to its reduction. Int. J. Paediatr. Dent. 2012, 22, 397–405. [Google Scholar] [CrossRef] [PubMed]
- Kime, R.; Hamaoka, T.; Sako, T.; Murakami, M.; Homma, T.; Katsumura, T.; Chance, B. Delayed reoxygenation after maximal isometric handgrip exercise in high oxidative capacity muscle. Eur. J. Appl. Phys. 2003, 89, 34–41. [Google Scholar] [CrossRef]
| Author (Year) | Study Design | Sample | Fatigue Protocol | VFR Intervention (Freq, Site, Duration) | Comparison Group | Outcome Measures |
|---|---|---|---|---|---|---|
| Romero-Moraleda et al., 2019 [20] | RCT | n = 38 healthy adults (19 VFR, 19 NVFR), VFR: 21.9(3.7) y, 1.77(0.07) m, 75.3(8.0) kg; NVFR: 22.2(3.2) y, 1.74(0.07) m, 69.7(11.4) kg | Eccentric squats | 18 Hz, Bilateral quadriceps, 5 min per leg, applied 48 h post-exercise | NVFR | VAS↓ (−30.2%, p = 0.033); PPT↑ (notably vastus medialis, p < 0.01); SmO2↑ (no between-group difference); ROM↑ (VFR > NVFR in hip extension, p < 0.05) |
| Lai et al., 2020 [21] | Quasi -experimental | n = 23 healthy adults (Male: 26.2(5.2) y, 169.5(3.9) cm; Female: 26.6(7.8) y, 156.8(5.1) cm) | 50 min treadmill | 20–40 Hz (mixed), Bilateral gastrocnemius, 3 min per | NVFR | VAS↓ in VFR (5.72 vs. 6.2, p = 0.327; 48% preferred VFR); SBF↑ in VFR (NS vs. FR); BFO↑ (endothelial, neurogenic, myogenic components all not significant) |
| de Benito et al., 2019 [22] | Quasi -experimental | n = 24 Male (n = 17): 22.5 y, 177.03 cm, 73.43 kg Female (n = 7): 20.43 y, 160.86 cm, 56.64 kg | Repetitive lunges at 30 reps/min until volitional fatigue | 30 Hz, bilateral quadriceps and hamstrings, 2 × 60 s per muscle with 30 s rest | NVFR, No treatment | Ankle ROM↑ in both groups (p < 0.001); flexibility (sit-and-reach)↑ (p = 0.074, clinically meaningful) |
| Zhu, 2023 [26] | RCT | 36 male college basketball players (19.8–20.4 y); EXP n = 18, CON n = 18 | Simulated game drills | Main muscle groups, 15 min per session, 3 times per week, for 9 weeks | Walking and stretching for 15 min | Lactic acid↓ (p < 0.05); subjective fatigue↓ (p < 0.05), supporting fatigue recovery |
| Chang et al., 2024 [27] | RCT | VFR group and General Warm-up group, 24 male college athletes (handball and rugby players). 20.21(1.15) y, 175.92(5.57) cm, 76.25(9.13) kg | 15 sets of maximal multidirectional repeated sprints | 48 Hz, Quadriceps and hamstrings, 30 s/set at 30 rolls/min, 4 sets, Total 8 min | General Warm-up group | VAS↓ at 48/72 h post-ex (quad, ham; p < 0.01); CK returned to baseline at 72 h in VFR (vs. elevated in control, p = 0.001); hip ROM: no significant change (p = 0.43) |
| Nakamura et al., 2022 [28] | Quasi -experimental | n = 14 healthy young male, 20.4(0.8) y, 170.9(6.8) cm, 65.1(9.3) kg | Eccentric knee extensions | 35 Hz, Midpoint of the dominant-side quadriceps, 3 × 30 s with 30 s rest, Total 90 s | - | Muscle soreness↓ (p < 0.01); PPT↑ across multiple conditions (p < 0.01); knee flexion ROM↑ by 6.5% (p < 0.01) |
| Nakamura et al., 2022 [29] | Quasi -experimental | n = 14 healthy young male, 21.4(0.7) y, 171.0(5.8) cm, 65.3(8.2) kg | Eccentric contraction of the dominant leg knee extensors | 35 Hz, Quadriceps of the nondamaged leg, 3 × 30 s with 30 s rest, Total 90 s | - | Pain↓ and PPT↑ on affected side (p < 0.05) despite VFR applied to opposite limb; knee flexion ROM↑ on contralateral side (p < 0.01), suggesting cross-education effect |
| Alonso-Calvete et al., 2021 [30] | Quasi -experimental | n = 7 certified lifeguards (2 Female, 5 Male), mean age 23.29(1.11) y, 173.43(8.6) cm, 76.57(5.94) kg | Simulated 100 m water rescue (swimming with fins, towing manikin, extracting to shore) | 18 Hz, quadriceps and hamstrings (both legs), 2 × 30 s per muscle with 15 s rest | Passive recovery (seated), non-vibrating foam roller | Lactate↓ (p = 0.001); perceived lower-limb fatigue↓ (RPE, p = 0.001) |
| Author (Year) | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | Q12 | Q13 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Romero-Moraleda et al., 2019 [20] | Y | U | Y | N | N | Y | Y | Y | Y | Y | Y | Y | Y |
| Lai et al., 2020 [21] | Y | N | Y | Y | Y | Y | Y | Y | Y | - | - | - | - |
| de Benito et al., 2019 [22] | Y | Y | Y | Y | Y | Y | Y | Y | Y | - | - | - | - |
| Zhu, 2023 [26] | Y | U | Y | N | N | U | Y | Y | Y | Y | Y | Y | Y |
| Chang et al., 2024 [27] | Y | U | Y | N | N | U | Y | Y | Y | Y | Y | Y | Y |
| Nakamura et al., 2022 [28] | Y | N | Y | Y | Y | Y | Y | Y | Y | - | - | - | - |
| Nakamura et al., 2022 [29] | Y | N | Y | Y | Y | Y | Y | Y | Y | - | - | - | - |
| Alonso-Calvete et al., 2021 [30] | Y | Y | Y | Y | Y | Y | Y | Y | Y | - | - | - | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, S.; Kim, B. Effects of Vibration Foam Rolling on Pain, Fatigue, and Range of Motion in Individuals with Muscle Fatigue: A Systematic Review. Healthcare 2025, 13, 1391. https://doi.org/10.3390/healthcare13121391
Park S, Kim B. Effects of Vibration Foam Rolling on Pain, Fatigue, and Range of Motion in Individuals with Muscle Fatigue: A Systematic Review. Healthcare. 2025; 13(12):1391. https://doi.org/10.3390/healthcare13121391
Chicago/Turabian StylePark, Seju, and Byeonggeun Kim. 2025. "Effects of Vibration Foam Rolling on Pain, Fatigue, and Range of Motion in Individuals with Muscle Fatigue: A Systematic Review" Healthcare 13, no. 12: 1391. https://doi.org/10.3390/healthcare13121391
APA StylePark, S., & Kim, B. (2025). Effects of Vibration Foam Rolling on Pain, Fatigue, and Range of Motion in Individuals with Muscle Fatigue: A Systematic Review. Healthcare, 13(12), 1391. https://doi.org/10.3390/healthcare13121391








