A Study on the Development of Information and Communication Technology-Based Oral Functional Rehabilitation Exercise Program Content for Elderly People
Abstract
1. Introduction
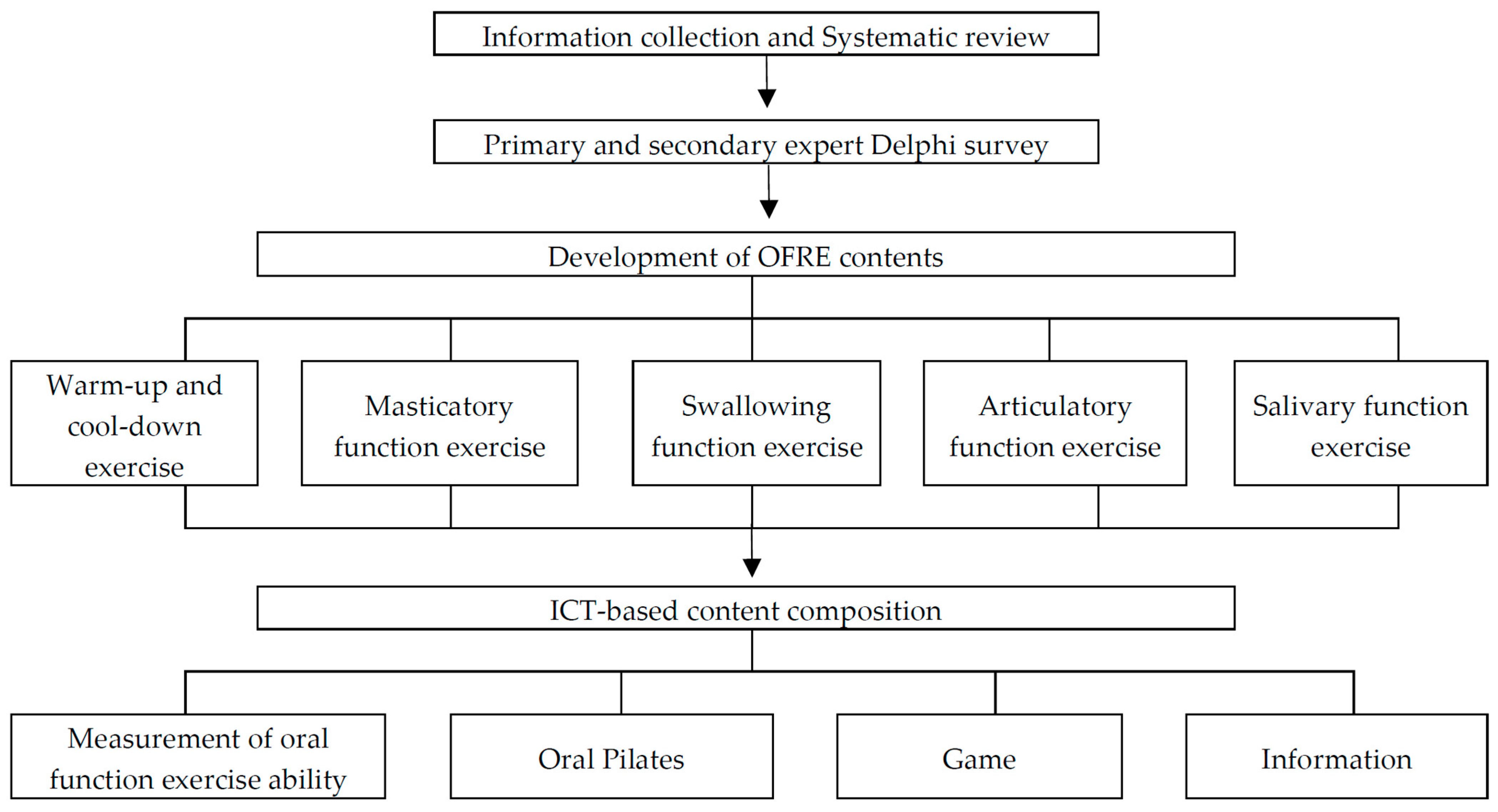
2. Materials and Methods
2.1. Study Model and Period
2.2. ICT-Based Content Development Process 1: OFRE App Content Survey
2.3. Process 2: Evidence-Based OFRE Content Categorization through Systematic Review
2.4. Process 3: Validity Evaluation of the Detailed OFRE Content through the Expert Delphi Survey
2.5. Process 4: Composition of the Final ICT-Based OFRE Contents
3. Results
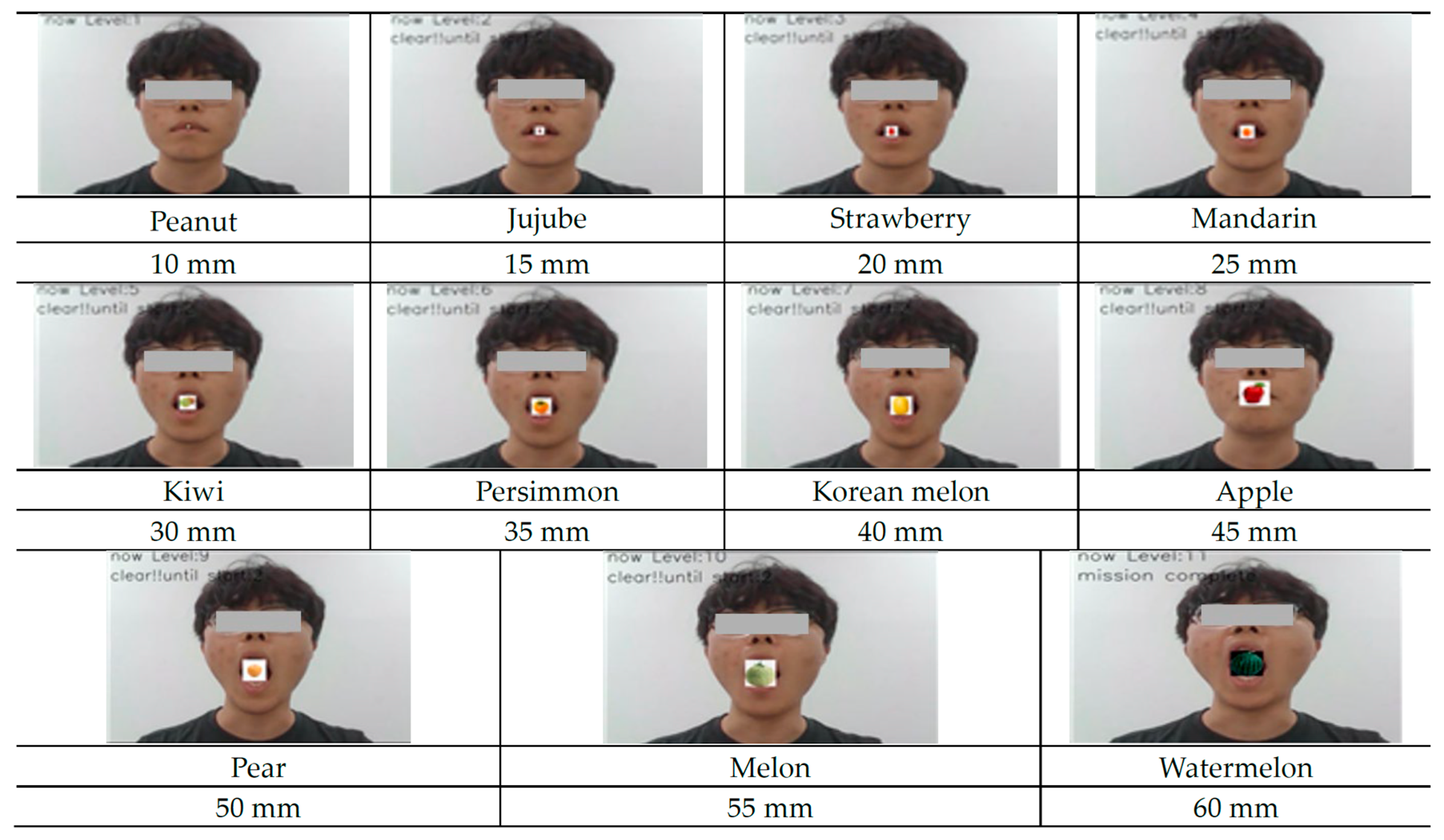
3.1. Content of ICT-Based OFRE for Measuring Oral Function Exercise Ability Using Facial Recognition
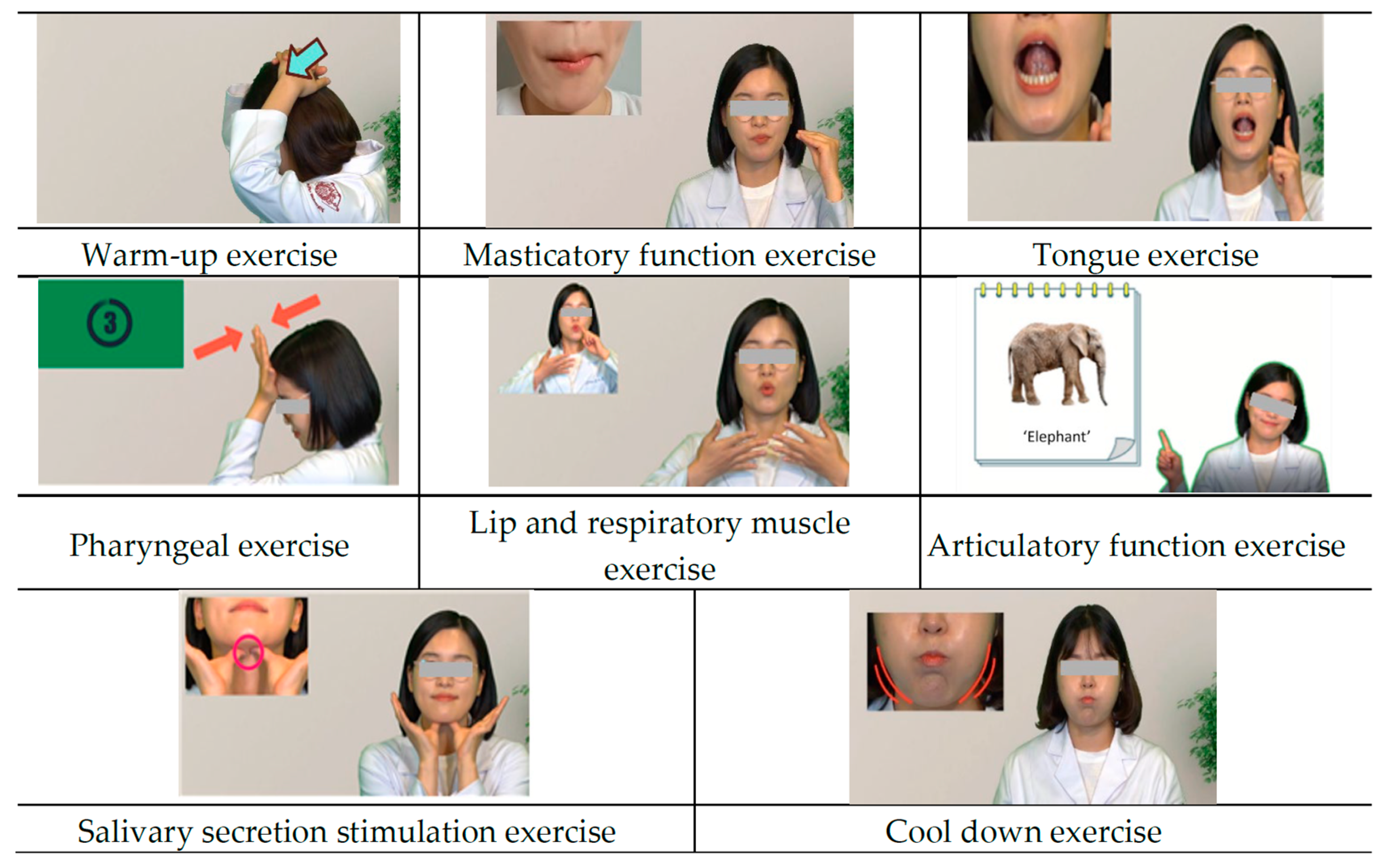
3.2. ICT-Based OFRE Oral Pilates Content
3.3. ICT-Based OFRE Game Content
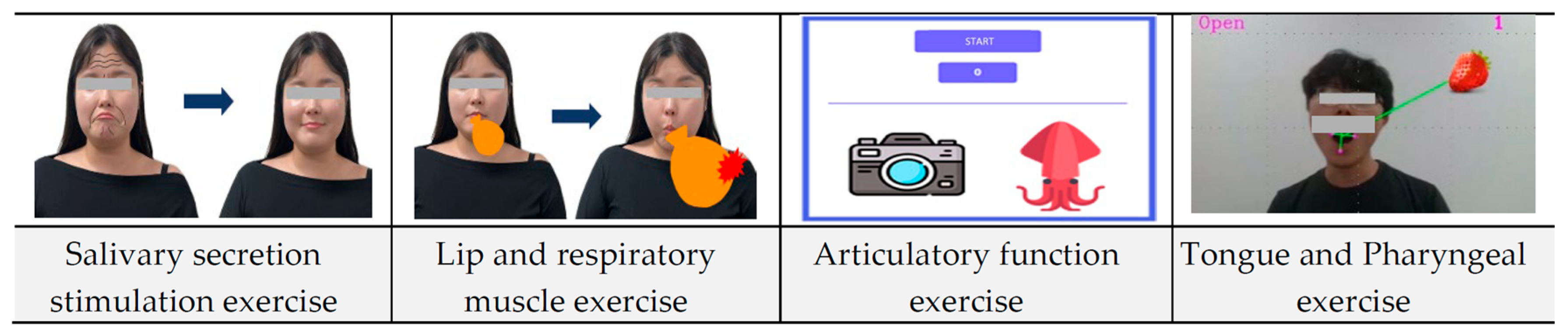
3.3.1. Salivary Secretion Stimulation Game
- A virtual wrinkle pattern was displayed on the user’s facial image. As the user performed a salivary gland stimulation massage, the wrinkle pattern’s reduction was tracked in real-time. The complete disappearance of the wrinkles (100% reduction) indicated successful game completion. This method objectively assessed the accuracy and duration of the massage technique in stimulating salivary secretion.
3.3.2. Lip and Respiratory Muscle Exercise Game
- Users virtually inflated an on-screen balloon by puffing out their cheeks. Balloon size was measured in pixels. The balloon’s inflation to a predetermined size (causing it to “burst”) marked successful game completion. This measured the intensity and duration of lip and respiratory muscle engagement.
3.3.3. Articulatory Function Exercise Game
- Users pronounced words corresponding to images displayed on the screen. Voice recognition technology analyzed pronunciation accuracy and duration. Successful game completion was achieved upon the correct pronunciation of a predetermined number of words. This assessed the accuracy and speed of articulatory exercises.
3.3.4. Tongue and Pharyngeal Exercise Game
- Using facial recognition, the accuracy of the user’s tongue contact with an on-screen target (simulating food) was measured. This provided an objective assessment of tongue and pharyngeal muscle function.
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bjering, H.; Curry, J.; Maeder, A. Gerontechnology: The importance of user participation in ICT development for older adults. In Investing in E-Health: People, Knowledge and Technology for a Healthy Future; IOS Press: Amsterdam, The Netherlands, 2014; pp. 7–12. [Google Scholar]
- Europe, A.P. Certification for Ageing in Place: The New European Project “HOMES4LIFE” Kick Off. 2023. Available online: https://www.age-platform.eu/certification-for-ageing-in-place-the-new-european-project-homes4life-kicks-off/ (accessed on 7 August 2023).
- Yoshimoto, T.; Nawa, N.; Uemura, M.; Sakano, T.; Fujiwara, T. The impact of interprofessional communication through ICT on health outcomes of older adults receiving home care in Japan—A retrospective cohort study. J. Gen. Fam. Med. 2022, 23, 233–240. [Google Scholar] [CrossRef] [PubMed]
- Waldman, S.A.; Terzic, A. Healthcare evolves from reactive to proactive. Clin. Pharmacol. Ther. 2019, 105, 10. [Google Scholar] [CrossRef] [PubMed]
- Ching Yuen Luk, S. Technologies and the Wellness of Older Adults. In Healthy Ageing in Singapore: Opportunities, Challenges and the Way Forward; Springer: Berlin/Heidelberg, Germany, 2023; pp. 89–122. [Google Scholar]
- Hänninen, R.; Taipale, S.; Luostari, R. Exploring heterogeneous ICT use among older adults: The warm experts’ perspective. New Media Soc. 2021, 23, 1584–1601. [Google Scholar] [CrossRef]
- Sheng, Y.; Doyle, J.; Bond, R.; Jaiswal, R.; Gavin, S.; Dinsmore, J. Home-based digital health technologies for older adults to self-manage multiple chronic conditions: A data-informed analysis of user engagement from a longitudinal trial. Digit. Health 2022, 8, 20552076221125957. [Google Scholar] [CrossRef]
- Yutong, T.; Yan, Z.; Qingyun, C.; Lixue, M.; Mengke, G.; Shanshan, W. Information and Communication Technology Based Integrated Care for Older Adults: A Scoping Review. Int. J. Integr. Care 2023, 23, 2. [Google Scholar] [CrossRef]
- Kim, J.; Song, J.; Kim, D.; Park, J. The development of ICT-based exercise rehabilitation service contents for patients with musculoskeletal disorders and stroke. Int. J. Environ. Res. Public Health 2022, 19, 5022. [Google Scholar] [CrossRef] [PubMed]
- Barisch-Fritz, B.; Bezold, J.; Scharpf, A.; Trautwein, S.; Krell-Roesch, J.; Woll, A. ICT-based individualized training of institutionalized individuals with dementia. Evaluation of usability and trends toward the effectiveness of the InCoPE-App. Front. Physiol. 2022, 13, 921105. [Google Scholar] [CrossRef]
- Nagatomi, Y.; Ide, T.; Higuchi, T.; Nezu, T.; Fujino, T.; Tohyama, T.; Nagata, T.; Higo, T.; Hashimoto, T.; Matsushima, S. Home-based cardiac rehabilitation using information and communication technology for heart failure patients with frailty. ESC Heart Fail. 2022, 9, 2407–2418. [Google Scholar] [CrossRef]
- Assis, M.A.L.; Tavares, L.D.F.; Bernardino, A.P.; Rocha, B.A.; Abreu, L.G.; Oliveira, D.D.; Pithon, M.M.; Soares, R.V. Information and Communications Technology in Dentistry: An informative and educational approach for patients with fixed orthodontic appliances. Dental Press J. Orthod. 2022, 27, e22spe3. [Google Scholar] [CrossRef]
- Brenčič, N.S.; Muntianu, L.S.; Piotrowicz, K.; Mocanu, I.; Rudel, D.; Lupu, I. Oral health education for elderly through ICT technology. In Proceedings of the EDULEARN21 Proceedings, Online, 5–6 July 2021; pp. 5452–5457. [Google Scholar]
- Hakeem, F.F.; Bernabe, E.; Sabbah, W. Association between oral health and frailty: A systematic review of longitudinal studies. Gerodontology 2019, 36, 205–215. [Google Scholar] [CrossRef]
- Koyama, Y.; Sugimoto, A.; Hamano, T.; Kasahara, T.; Toyokura, M.; Masakado, Y. Proposal for a modified jaw opening exercise for dysphagia: A randomized, controlled trial. Tokai J. Exp. Clin. Med. 2017, 42, 71–78. [Google Scholar] [PubMed]
- Iwao-Kawamura, Y.; Shigeishi, H.; Uchida, S.; Kawano, S.; Maehara, T.; Sugiyama, M.; Ohta, K. Changes in physical and oral function after a long-term care prevention program in community-dwelling Japanese older adults: A 12-month follow-up study. Healthcare 2021, 9, 719. [Google Scholar] [CrossRef] [PubMed]
- Takano, S.; Yamaguchi, K.; Nakagawa, K.; Yoshimi, K.; Nakane, A.; Okumura, T.; Tohara, H. Effect of isometric exercises on the masseter muscle in older adults with missing dentition: A randomized controlled trial. Sci. Rep. 2021, 11, 7285. [Google Scholar] [CrossRef]
- Kim, M.J.; Hong, J.Y.; Lee, G.; Yoon, T.; Hwang, S.H.; Kim, H.H.; Jung, Y.; Park, J.S. Effects of chewing exercises on the occlusal force and masseter muscle thickness in community-dwelling Koreans aged 65 years and older: A randomised assessor-blind trial. J. Oral. Rehabil. 2020, 47, 1103–1109. [Google Scholar] [CrossRef] [PubMed]
- Shirobe, M.; Watanabe, Y.; Tanaka, T.; Hirano, H.; Kikutani, T.; Nakajo, K.; Sato, T.; Furuya, J.; Minakuchi, S.; Iijima, K. Effect of an oral frailty measures program on community-dwelling elderly people: A cluster-randomized controlled trial. Gerontology 2022, 68, 377–386. [Google Scholar] [CrossRef]
- Mansoor, D.E. Full Mouth Rehabilitation versus Full Body Rehabilitation. 2023. Available online: https://www.fdiworlddental.org/full-mouth-rehabilitation-versus-full-body-rehabilitation (accessed on 9 December 2023).
- Choi, Y.; Yun, J.; Park, H.; Cha, E. A Study on the Status of Contents Related to Oral Functional Rehabilitation Exercise Based on Application. J. Korean Soc. Oral. Healh Sci. 2022, 10, 55–61. [Google Scholar] [CrossRef]
- Kwon, H.; Maeng, H.; Chung, J. Development of an ICT-based exergame program for children with developmental disabilities. J. Clin. Med. 2022, 11, 5890. [Google Scholar] [CrossRef]
- Yun, J.H. Development and Validation of a Conceptual Framework of ICF-Based Oral Function Rehabilitation Exercise Intervention for Community-Dwelling Older Adults. Ph.D. Thesis, Ajou University, Suwon, Republic of Korea, 2023. [Google Scholar]
- Li, X.-Y.; Jia, C.; Zhang, Z.-C. The normal range of maximum mouth opening and its correlation with height or weight in the young adult Chinese population. J. Dent. Sci. 2017, 12, 56–59. [Google Scholar] [CrossRef]
- Peel, N.M.; McClure, R.J.; Bartlett, H.P. Behavioral determinants of healthy aging. Am. J. Prev. Med. 2005, 28, 298–304. [Google Scholar] [CrossRef]
- Haumschild, M.S.; Haumschild, R.J. The importance of oral health in long-term care. J. Am. Med. Dir. Assoc. 2009, 10, 667–671. [Google Scholar] [CrossRef]
- Suzuki, M.; Koyama, S.; Kimura, Y.; Ishiyama, D.; Otobe, Y.; Nishio, N.; Ichikawa, T.; Kunieda, Y.; Ohji, S.; Ito, D. Relationship between characteristics of skeletal muscle and oral function in community-dwelling older women. Arch. Gerontol. Geriatr. 2018, 79, 171–175. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, Y.; Hirano, H.; Arai, H.; Morishita, S.; Ohara, Y.; Edahiro, A.; Murakami, M.; Shimada, H.; Kikutani, T.; Suzuki, T. Relationship between frailty and oral function in community-dwelling elderly adults. J. Am. Geriatr. Soc. 2017, 65, 66–76. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, M.; Hiyama, A.; Miura, T.; Asakawa, C.; Hirose, M.; Ifukube, T. Elderly user evaluation of mobile touchscreen interactions. In Proceedings of the Human-Computer Interaction—INTERACT, Lisbon, Portugal, 5–9 September 2011; pp. 83–99. [Google Scholar]
- Mariño, R.J.; Marwaha, P.; Barrow, S.-y. Web-based oral health promotion program for older adults: Development and preliminary evaluation. Int. J. Med. Inform. 2016, 91, e9–e15. [Google Scholar] [CrossRef] [PubMed]
- Wongworasun, S.; Hunsrisakhun, J.; Watanapa, A. Effectiveness of oral exercise programs on oral function among independent elderly people: A cluster randomized controlled trial. J. Int. Oral Health 2022, 14, 363–369. [Google Scholar]
- Lee, J.; Kwon, H.; Lee, Y.; Lee, M.H.; Lee, H.K. Effect of regular oral exercise on oral function in elderly patients with long-term care. J. Korean Acad. Oral. Health 2010, 34, 422–429. [Google Scholar]
- Jang, K.; Hwang, I. Effects of mouth exercise on the improvements of oral function in elderly men. J. Dent. Hyg. Sci. 2011, 11, 257–263. [Google Scholar]
- Lee, J.W.; Park, S.J. A study on interface design of serious game for the elderly. Adv. Sci. Technol. Lett. 2013, 39, 159–163. [Google Scholar]
- Resnick, B.; Vogel, A.; Luisi, D. Motivating minority older adults to exercise. Cultur. Divers. Ethnic Minor. Psychol. 2006, 12, 17. [Google Scholar] [CrossRef]
- Ki, J.Y.; Jo, S.R.; Cho, K.S.; Park, J.E.; Cho, J.W.; Jang, J.H. Effect of oral health education using a mobile app (OHEMA) on the oral health and swallowing-related quality of life in community-based integrated care of the elderly: A randomized clinical trial. Int. J. Environ. Res. Public Health 2021, 18, 11679. [Google Scholar] [CrossRef]
- Ohara, Y.; Yoshida, N.; Kono, Y.; Hirano, H.; Yoshida, H.; Mataki, S.; Sugimoto, K. Effectiveness of an oral health educational program on community-dwelling older people with xerostomia. Geriatr. Gerontol. Int. 2015, 15, 481–489. [Google Scholar] [CrossRef]
- Sánchez-Mena, A.; Martí-Parreño, J. Drivers and barriers to adopting gamification: Teachers’ perspectives. Electron. J. e-Learn. 2017, 15, 434–443. [Google Scholar]
- Kim, d. A Literature review of domestic research on gamification of education in Korea: Research trends and critical analysis. Korean Assoc. Learn.-Centered Curric. Instr. 2020, 20, 457. [Google Scholar] [CrossRef]
- Johnson, L.; Becker, S.A.; Estrada, V.; Freeman, A. NMC Horizon Report: 2014 K-12 Edition. The New Media Consortium. 2014. Available online: https://files.eric.ed.gov/fulltext/ED559369.pdf (accessed on 10 August 2023).
| Operating System | Purpose | Application Name | Cost |
|---|---|---|---|
| IOS | Education | Smart Oral Motor | No |
| Train My Tongue | No | ||
| Health | Dysfagi træning | No | |
| Swallow RehApp | Yes | ||
| Medical | Small Talk Oral Motor Exercises | No | |
| Android | Lifestyle | Oral Health and Dementia | No |
| Medical | Speech Companion | Yes | |
| Both | Education | Oroeasy | No |
| VAST Pre-Speech Motor Planning | Yes | ||
| Tongue Thrust Therapy | No |
| Intervention Domain | Detailed Content | |
|---|---|---|
| Warm-up and cool-down exercise | Orofacial muscle-stretching exercise | |
| Masticatory function exercise | Chewing exercise using noncariogenic foods or tools Masseter muscle-strengthening exercise | |
| Swallowing function exercise | Tongue exercise | Tongue-strengthening exercise Swallowing exercise |
| Pharyngeal exercise | Head-flexing exercise | |
| Lip and respiratory muscle exercise | Lip-strengthening exercise Expiratory muscle-strength exercise | |
| Articulatory function exercise | Syllable-articulation exercise | |
| Salivary function exercise | Salivary gland massage | |
| Name | Menu | Contents | Details |
|---|---|---|---|
| OFRE | Oral-function exercise ability evaluation | Maximum mouth-opening measurement | Measure oral-function exercise ability before and after exercise (measure maximum opening amount) |
| Oral Pilates | Warm-up exercise | Warm-up and cool-down are the same exercise | |
| Cool-down exercise | |||
| Masticatory function exercise | Eight exercises provided in video format | ||
| Tongue exercise | |||
| Pharyngeal exercise | |||
| Lip exercise | |||
| Respiratory muscle exercise | |||
| Articulatory function exercise | |||
| Salivary function exercise | |||
| Game | Salivary secretion stimulation exercise | Perform oral functional rehabilitation exercises in a fun way like a motion recognition game. | |
| Lip and respiratory muscle exercise | |||
| Articulatory function exercise | |||
| Tongue and pharyngeal exercise |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choi, Y.-K.; Yun, J.-H.; Lee, H.; Cha, E.-G.; Park, H.-A. A Study on the Development of Information and Communication Technology-Based Oral Functional Rehabilitation Exercise Program Content for Elderly People. Healthcare 2024, 12, 2058. https://doi.org/10.3390/healthcare12202058
Choi Y-K, Yun J-H, Lee H, Cha E-G, Park H-A. A Study on the Development of Information and Communication Technology-Based Oral Functional Rehabilitation Exercise Program Content for Elderly People. Healthcare. 2024; 12(20):2058. https://doi.org/10.3390/healthcare12202058
Chicago/Turabian StyleChoi, Yong-Keum, Ji-Hye Yun, Hyun Lee, Eun-Gyeong Cha, and Hyang-Ah Park. 2024. "A Study on the Development of Information and Communication Technology-Based Oral Functional Rehabilitation Exercise Program Content for Elderly People" Healthcare 12, no. 20: 2058. https://doi.org/10.3390/healthcare12202058
APA StyleChoi, Y.-K., Yun, J.-H., Lee, H., Cha, E.-G., & Park, H.-A. (2024). A Study on the Development of Information and Communication Technology-Based Oral Functional Rehabilitation Exercise Program Content for Elderly People. Healthcare, 12(20), 2058. https://doi.org/10.3390/healthcare12202058






