Co-Creation in Health 4.0 as a New Solution for a New Era
Abstract
1. Introduction
2. Co-Creation in Health 4.0
2.1. Health 4.0 Solutions
2.2. Co-Creation in Healthcare Services
2.3. Co-Creation and Service Management Phases
2.4. Co-Creation and Actors
3. Materials and Methods
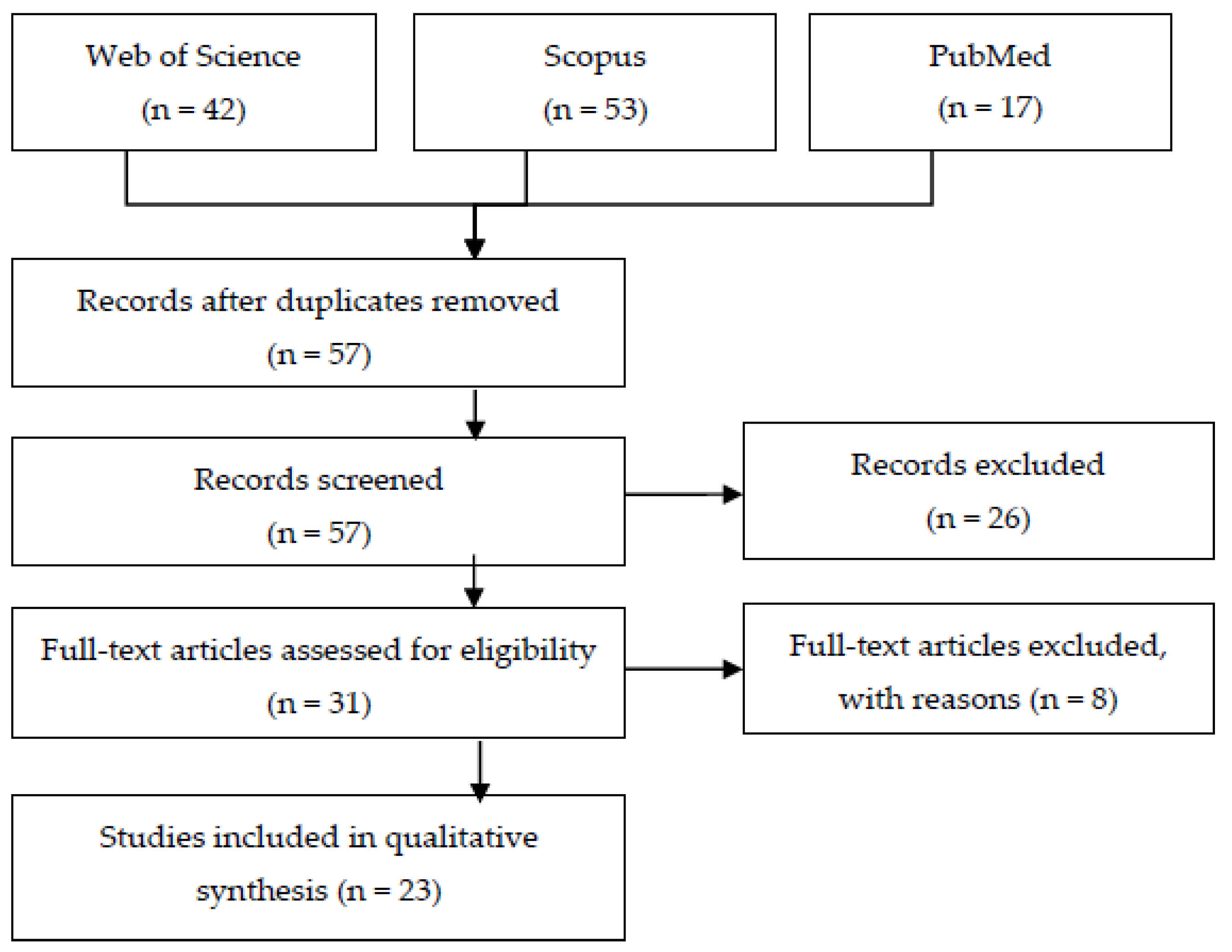
3.1. The Identification of Already Investigated Cases
3.2. The Selection of the Most Informative Example
- -
- the process—phases of creating a solution (12 articles);
- -
- the entity—actors (16 articles);
- -
- results—products/services (12 articles);
- -
- health policy and implementation (9 articles);
- -
- solution and/or health system effectiveness (17 articles);
- -
- current knowledge synthesis (literature review or case presentations) (6 articles).
3.3. The Assessment of the Scope and Scale of Co-creation in Health 4.0 Ventures
4. Results
4.1. Description
4.2. Actors
4.3. Co-Creation Mechanisms/Areas
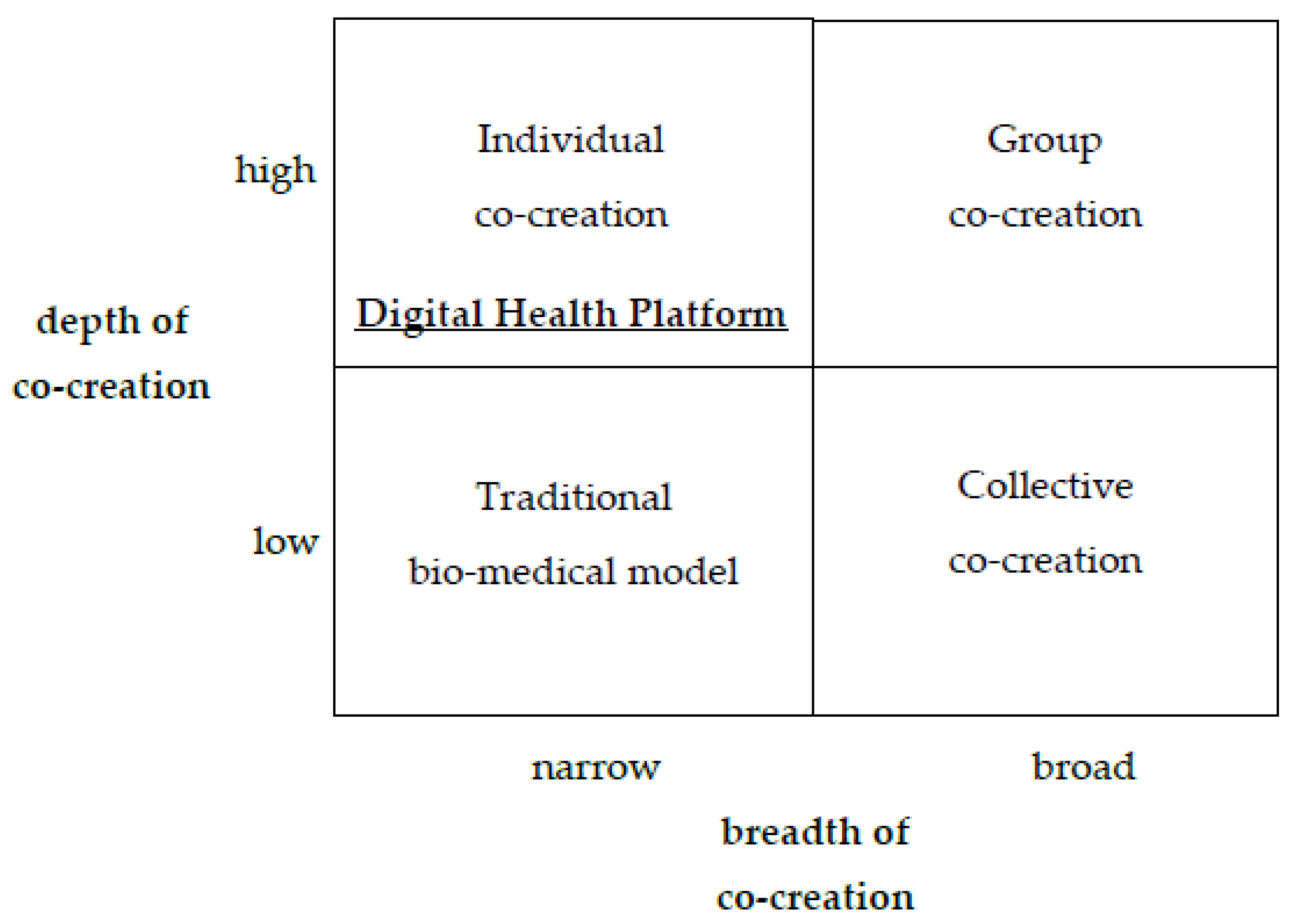
4.4. Co-Creation Matrix
5. Conclusions
5.1. Theoretical Implications
5.2. Practical Implications
5.3. Study Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Palumbo, R. Contextualizing Co-production of Health Care. A Systematic Literature Review. Int. J. Public Sect. Manag. 2016, 29, 72–90. [Google Scholar] [CrossRef]
- Bashshur, R.; Shannon, G.; Krupinski, E.; Grigsby, J. The Taxonomy of Telemedicine. Telemed. J. E-Health Off. J. Am. Telemed. Assoc. 2011, 17, 484–494. [Google Scholar] [CrossRef] [PubMed]
- Palumbo, R. The Bright Side and the Dark Side of Patient Empowerment. Co-Creation and Co-Destruction of Value in the Healthcare Environment; Springer International Publishing A&G: New York, USA, 2017; p. 104. [Google Scholar]
- Thuemmler, C.; Bai, C. Health 4.0: How Virtualization and Big Data Are Revolutionizing Healthcare; Springer International Publishing A&G: New York, USA, 2017; p. 254. [Google Scholar]
- Liao, Y.; Deschamps, F.; Loures, E.d.F.R.; Ramos, L.F.P. Past, present and future of Industry 4.0—A systematic literature review and research agenda proposal. Int. J. Prod. Res. 2017, 55, 3609–3629. [Google Scholar] [CrossRef]
- Valderas, J.M.; World Health Organization, Department of Service Delivery and Safety. Patient Engagement; World Health Organization: Geneva, Switzerland, 2016. [Google Scholar]
- Anderson, R.M.; Funnell, M.M. Patient empowerment: Myths and misconceptions. Patient Educ. Couns. 2009, 79, 277–282. [Google Scholar] [CrossRef] [PubMed]
- Klich, J. The fourth industrial revolution and the healthcare system. In The Digital Transformation of Healthcare—Health 40; Routledge: New York, NY, USA, 2022. [Google Scholar]
- Li, J.; Carayon, P. Health Care 4.0: A vision for smart and connected health care. IISE Trans. Healthc. Syst. Eng. 2021, 11, 171–180. [Google Scholar] [CrossRef]
- Carayon, P.; Wooldridge, A.R. Improving Patient Safety in the Patient Journey: Contributions from Human Factors Engineering. In Women in Industrial and Systems Engineering; Smith, A.E., Ed.; Springer International Publishing: Cham, Switzerland, 2020; pp. 275–299. [Google Scholar] [CrossRef]
- Karlöf, B.; Östblom, S. Benchmarking: A Signpost to Excellence in Quality and Productivity; John Wiley & Sons: New York, NY, USA, 1994. [Google Scholar]
- Schwab, K. The Fourth Industrial Revolution; World Economic Forum: New York, NY, USA, 2016; 184p. [Google Scholar]
- Schwab, K.; Zahidi, S. The Future of Jobs Report 2020. World Economic Forum. 2020. Available online: https://www.voced.edu.au/content/ngv:83213 (accessed on 20 September 2022).
- Klöcker, P.N.; Bernnat, R.; Veit, D.J. Stakeholder behavior in national eHealth implementation programs. Health Policy Technol. 2015, 4, 113–120. [Google Scholar] [CrossRef]
- Brynjolfsson, E.; Mcafee, A. The Second Machine Age: Work, Progress, and Prosperity in a Time of Brilliant Technologies, Illustrated ed.; W. W. Norton & Company: New York, NY, USA, 2014; 320p. [Google Scholar]
- Ford, M. Rise of the Robots; Basic Books: New York, NY, USA, 2015. [Google Scholar]
- Morgan, J. The Future of Work: Attract New Talent, Build Better Leaders, and Create a Competitive Organization; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2014; 234p. [Google Scholar]
- Cresswell, K.; Cunningham-Burley, S.; Sheikh, A. Health Care Robotics: Qualitative Exploration of Key Challenges and Future Directions. J. Med. Internet Res. 2018, 20, e10410. [Google Scholar] [CrossRef]
- Tse, Z.T.H.; Chen, Y.; Hovet, S.; Ren, H.; Cleary, K.; Xu, S.; Wood, B.; Monfaredi, R. Soft Robotics in Medical Applications. J. Med. Robot. Res. 2018, 3, 1841006. [Google Scholar] [CrossRef]
- Honigmann, P.; Sharma, N.; Okolo, B.; Popp, U.; Msallem, B.; Thieringer, F.M. Patient-Specific Surgical Implants Made of 3D Printed PEEK: Material, Technology, and Scope of Surgical Application. BioMed Res. Int. 2018, 10, 3563. [Google Scholar] [CrossRef]
- Milligan, C.; Roberts, C.; Mort, M. Telecare and older people: Who cares where? Soc. Sci. Med. 2011, 72, 347–354. [Google Scholar] [CrossRef]
- Willemsen, K.; Nizak, R.; Noordmans, H.J.; Castelein, R.M.; Weinans, H.; Kruyt, M.C. Challenges in the design and regulatory approval of 3D-printed surgical implants: A two-case series. Lancet Digit. Health 2019, 1, e163–e171. [Google Scholar] [CrossRef]
- Aceto, G.; Persico, V.; Pescapé, A. The role of Information and Communication Technologies in healthcare: Taxonomies, perspectives, and challenges. J. Netw. Comput. Appl. 2018, 107, 125–154. [Google Scholar] [CrossRef]
- Kerr, D.; Klonoff, D.C. Digital Diabetes Data and Artificial Intelligence: A Time for Humility Not Hubris. J. Diabetes Sci. Technol. 2019, 13, 123–127. [Google Scholar] [CrossRef]
- Okamura, A.M.; Mataric, M.J.; Christensen, H.I. Medical and Health-Care Robotics. IEEE Robot. Autom. Mag. 2010, 17, 26–37. [Google Scholar] [CrossRef]
- Joyia, G.J.; Liaqat, R.M.; Farooq, A.; Rehman, S. Internet of Medical Things (IOMT): Applications, Benefits and Future Challenges in Healthcare Domain. J. Commun. 2017, 12, 240–247. [Google Scholar] [CrossRef]
- Basatneh, R.; Najafi, B.; Armstrong, D.G. Health Sensors, Smart Home Devices, and the Internet of Medical Things: An Oppor-tunity for Dramatic Improvement in Care for the Lower Extremity Complications of Diabetes. J. Diabetes Sci. Technol. 2018, 12, 577–586. [Google Scholar] [CrossRef] [PubMed]
- Keeys, L.A.; Huemann, M. Project benefits co-creation: Shaping sustainable development benefits. Int. J. Proj. Manag. 2017, 35, 1196–1212. [Google Scholar] [CrossRef]
- Chambers, R.; Schmid, M. Making technology-enabled health care work in general practice. Br. J. Gen. Pract. 2018, 68, 108–109. [Google Scholar] [CrossRef] [PubMed]
- Bryson, J. What to do when Stakeholders matter. Public Manag. Rev. 2004, 6, 21–53. [Google Scholar] [CrossRef]
- Kaplan, R.M.; Babad, Y.M. Balancing influence between actors in healthcare decision making. BMC Health Serv. Res. 2011, 11, 85. [Google Scholar] [CrossRef]
- Stabell, C.B.; Fjeldstad, Ø.D. Configuring value for competitive advantage: On chains, shops, and networks. Strateg. Manag. J. 1998, 19, 413–437. [Google Scholar] [CrossRef]
- Prahalad, C.K.; Ramaswamy, V. Co-creation experiences: The next practice in value creation. J. Interact. Mark. 2004, 18, 5–14. [Google Scholar] [CrossRef]
- Ramaswamy, V.; Gouillart, F. Build the co-creative enterprise. Harv. Bus. Rev. 2010, 88, 150. [Google Scholar]
- Galvagno, M.; Dalli, D. Theory of value co-creation: A systematic literature review. Manag. Serv. Qual. Int. J. 2014, 24, 643–683. [Google Scholar] [CrossRef]
- Vargo, S.L.; Maglio, P.P.; Akaka, M.A. On value and value co-creation: A service systems and service logic perspective. Eur. Manag. J. 2008, 26, 145–152. [Google Scholar] [CrossRef]
- Vargo, S.L.; Lusch, R.F. Evolving to a New Dominant Logic for Marketing. J. Mark. 2004, 68, 1–17. [Google Scholar] [CrossRef]
- Laurisz, N. Co-creation in Health 4.0. In The Digital Transformation of Healthcare—Health 40; Routledge: New York, NY, USA, 2022. [Google Scholar]
- Bhalla, G. Collaboration and Co-Creation: New Platforms for Marketing and Innovation, 2011th ed.; Springer International Publishing A&G: New York, NY, USA, 2010; 205p. [Google Scholar]
- Mair, F.S.; May, C.; O’Donnell, C.; Finch, T.; Sullivan, F.; Murray, E. Factors that promote or inhibit the implementation of e-health systems: An explanatory systematic review. Bull. World Health Organ. 2012, 90, 357–364. [Google Scholar] [CrossRef]
- Eysenbach, G. Medicine 2.0: Social Networking, Collaboration, Participation, Apomediation, and Openness. J. Med. Internet Res. 2008, 10, e22. [Google Scholar] [CrossRef]
- Herzlinger, R.E. Why innovation in health care is so hard. Harv. Bus. Rev. 2006, 84(5), 58–66. [Google Scholar]
- Oh, H.; Jadad, A.; Rizo, C.; Enkin, M.; Powell, J.; Pagliari, C. What Is eHealth (3): A Systematic Review of Published Definitions. J. Med. Internet Res. 2005, 7, e1. [Google Scholar] [CrossRef]
- Palumbo, R.; Nicola, C.; Adinolfi, P. Addressing health literacy in the digital domain: Insights from a literature review. Kybernetes 2021, 51, 82–97. [Google Scholar] [CrossRef]
- Lo Presti, L.; Testa, M.; Marino, V.; Singer, P. Engagement in Healthcare Systems: Adopting Digital Tools for a Sustainable Ap-proach. Sustainability 2019, 11, 220. [Google Scholar] [CrossRef]
- Gouillart, F.J. The race to implement co-creation of value with stakeholders: Five approaches to competitive advantage. Strat. Leadersh. 2014, 42, 2–8. [Google Scholar] [CrossRef]
- Hsu, Y. A value cocreation strategy model for improving product development performance. J. Bus. Ind. Mark. 2016, 31, 695–715. [Google Scholar] [CrossRef]
- Kim, J. Use of Robots as a Creative Approach in Healthcare ICT. Healthc. Inform. Res. 2018, 24, 155–156. [Google Scholar] [CrossRef] [PubMed]
- Pinho, N.; Beirão, G.; Patrício, L.; Fisk, R.P. Understanding value co-creation in complex services with many actors. J. Serv. Manag. 2014, 25, 470–493. [Google Scholar] [CrossRef]
- Ramaswamy, V.; Ozcan, K. The Co-Creation Paradigm; Stanford University Press: Redwood City, CA, USA, 2014; 356p. [Google Scholar]
- Voorberg, W.H.; Bekkers, V.J.J.M.; Tummers, L.G. A Systematic Review of Co-Creation and Co-Production: Embarking on the social innovation journey. Public Manag. Rev. 2015, 17, 1333–1357. [Google Scholar] [CrossRef]
- Freeman, R.E. Strategic Management; Cambridge University Press: Cambridge, UK, 2010; 292p. [Google Scholar]
- Bryson, J.; Sancino, A.; Benington, J.; Sørensen, E. Towards a multi-actor theory of public value co-creation. Public Manag. Rev. 2017, 19, 640–654. [Google Scholar] [CrossRef]
- Ross, J.; Stevenson, F.; Lau, R.; Murray, E. Exploring the challenges of implementing e-health: A protocol for an update of a sys-tematic review of reviews. BMJ Open 2015, 5, e006773. [Google Scholar] [CrossRef]
- Harrison, J.S. Strategic Management of Healthcare Organizations: A Stakeholder Management Approach; Business Expert Press: Hampton, NJ, USA, 2014; 180p. [Google Scholar]
- Alkhaldi, B.; Sahama, T.; Huxley, C.; Gajanayake, R. Barriers to Implementing eHealth: A Multi-dimensional Perspective. Stud. Health Technol. Inform. 2014, 205, 875–879. [Google Scholar] [CrossRef]
- Hill, G.M. The Complete Project Management Methodology and Toolkit; CRC Press: Boca Raton, FL, USA, 2009. [Google Scholar] [CrossRef]
- Bengtsson, M. A Method for Implementing Condition Based Maintenance in Industrial Settings. In Proceedings of the International Conference on Flexible Automation and Intelligent Manufacturing, Skövde, Sweden, 30 June–2 July 2008. [Google Scholar]
- Black, A.; Sahama, T.; Gajanayake, R. eHealth-as-a-Service (eHaaS): A data-driven decision making approach in Australian context. Stud. Health Technol. Inform. 2014, 205, 915–919. [Google Scholar]
- Zhang, P.; Carey, J.; Te’eni, D.; Tremaine, M. Integrating Human-Computer Interaction Development into the Systems Develop-ment Life Cycle: A Methodology. Commun. AIS 2005, 15, 512–543. [Google Scholar]
- Hamilton, A.B.; Brunner, J.; Cain, C.; Chuang, E.; Luger, T.M.; Canelo, I.; Rubenstein, L.; Yano, E.M. Engaging multilevel stakeholders in an implementation trial of evidence-based quality improvement in VA women’s health primary care. Transl. Behav. Med. 2017, 7, 478–485. [Google Scholar] [CrossRef]
- Urueña, A.; Hidalgo, A.; Arenas, E. Identifying capabilities in innovation projects: Evidences from eHealth. J. Bus. Res. 2016, 69, 4843–4848. [Google Scholar] [CrossRef]
- Zayyad, M.A.; Toycan, M. Factors affecting sustainable adoption of e-health technology in developing countries: An exploratory survey of Nigerian hospitals from the perspective of healthcare professionals. PeerJ 2018, 6, e4436. [Google Scholar] [CrossRef]
- Mills, D.K. Future Medicine: The Impact of 3D Printing. J. Nanomater. Mol. Nanotechnol. 2015, 4, 2. [Google Scholar] [CrossRef]
- Wildenbos, G.; Peute, L.; Jaspers, M. Aging barriers influencing mobile health usability for older adults: A literature based framework (MOLD-US). Int. J. Med. Inform. 2018, 114, 66–75. [Google Scholar] [CrossRef]
- Ramaswamy, V.; Ozcan, K. Strategy and co-creation thinking. Strat. Leadersh. 2013, 41, 5–10. [Google Scholar] [CrossRef]
- Cleland, D.L.; Ireland, L.R. Project Management: Strategic Design and Implementation; McGraw Hill Professional: New York, NY, USA, 2006; 549p. [Google Scholar]
- Gaddi, A.; Capello, F.; Manca, M. (Eds.) eHealth, Care and Quality of Life; Springer International Publishing A&G: New York, NY, USA, 2014; p. 236. [Google Scholar]
- Potvin, L.; Cargo, M.; McComber, A.M.; Delormier, T.; Macaulay, A.C. Implementing participatory intervention and research in communities: Lessons from the Kahnawake Schools Diabetes Prevention Project in Canada. Soc. Sci. Med. 2003, 56, 1295–1305. [Google Scholar] [CrossRef]
- Freeman, R.E. Stakeholder Theory: The State of the Art; Cambridge University Press: Cambridge, UK; New York, NY, USA, 2010; 362p. [Google Scholar]
- Kazadi, K.; Lievens, A.; Mahr, D. Stakeholder co-creation during the innovation process: Identifying capabilities for knowledge creation among multiple stakeholders. J. Bus. Res. 2016, 69, 525–540. [Google Scholar] [CrossRef]
- WHO. Key Components of a Well Functioning Health System. WHO. 2010. Available online: https://www.who.int/healthsystems/EN_HSSkeycomponents.pdf?ua=1 (accessed on 20 September 2022).
- Bessant, J.; Künne, C.; Möslein, K. Opening Up Healthcare Innovation: Innovation Solutions for a 21st Century Healthcare System; Advanced Institute for Management Research (AIM): London, UK, 2012. [Google Scholar]
- Kurzweil, R. The Singularity is Near: When Humans Transcend Biology; Viking: New York, NY, USA, 2005. [Google Scholar]
- Ewert, B.; Evers, A. An Ambiguous Concept: On the Meanings of Co-production for Health Care Users and User Organizations? VOLUNTAS Int. J. Volunt. Nonprofit Organ. 2014, 25, 425–442. [Google Scholar] [CrossRef]
- Lo Presti, L.; Testa, M.; Maggiore, G.; Marino, V. Key drivers involved in the telemonitoring of COVID-19 for self-health management: An exploratory factor analysis. BMC Health Serv. Res. 2022, 22, 520. [Google Scholar] [CrossRef]
- Tozzi, A.E.; Gesualdo, F.; Urbani, E.; Sbenaglia, A.; Ascione, R.; Procopio, N.; Croci, I.; Rizzo, C. Digital Surveillance Through an Online Decision Support Tool for COVID-19 Over One Year of the Pandemic in Italy: Observational Study. J. Med. Internet Res. 2021, 23, e29556. [Google Scholar] [CrossRef] [PubMed]
- Yin, R.K. Case Study Research: Design and Methods; SAGE Publishing: Thousand Oaks, CA, USA, 2009; 241p. [Google Scholar]
- Breidbach, C.; Brodie, R. Engagement platforms in the sharing economy: Conceptual foundations and research directions. J. Serv. Theory Pract. 2017, 27, 761–777. [Google Scholar] [CrossRef]
- Lang, A. Government capacities and stakeholders: What facilitates ehealth legislation? Glob. Health 2014, 10, 4. [Google Scholar] [CrossRef]
- Oertzen, A.S.; Odekerken-Schröder, G.; Brax, S.A.; Mager, B. Co-creating services—Conceptual clarification, forms and outcomes. J. Serv. Manag. 2018, 29, 641–679. [Google Scholar] [CrossRef]
- Elg, M.; Engström, J.; Witell, L.; Poksinska, B.B. Co-creation and learning in health-care service development. J. Serv. Manag. 2012, 23, 328–343. [Google Scholar] [CrossRef]
- Holden, R.J.; Karsh, B.-T. The Technology Acceptance Model: Its past and its future in health care. J. Biomed. Inform. 2010, 43, 159–172. [Google Scholar] [CrossRef]
| Name | Paginemediche |
|---|---|
| Type | Health engagement (internet communication) platform |
| Website | paginemediche.it |
| Country | Italy |
| Year of establishment | 2015 |
| Key areas |
|
| Data sources | paginemediche.it; Lo Presti et al. (2019) [45]; Lo Presti et al. (2022) [76]; Tozzi et al. (2021) [77] |
| Actors | Providers | Payers | Suppliers | Consumers | |
|---|---|---|---|---|---|
| Phase | |||||
| Planning |
|
| Information support, real participation, and involvement in the planning process |
| |
| Design |
| - |
| - | |
| Delivery |
| - |
|
| |
| Maintenance |
| - |
|
| |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Laurisz, N.; Ćwiklicki, M.; Żabiński, M.; Canestrino, R.; Magliocca, P. Co-Creation in Health 4.0 as a New Solution for a New Era. Healthcare 2023, 11, 363. https://doi.org/10.3390/healthcare11030363
Laurisz N, Ćwiklicki M, Żabiński M, Canestrino R, Magliocca P. Co-Creation in Health 4.0 as a New Solution for a New Era. Healthcare. 2023; 11(3):363. https://doi.org/10.3390/healthcare11030363
Chicago/Turabian StyleLaurisz, Norbert, Marek Ćwiklicki, Michał Żabiński, Rossella Canestrino, and Pierpaolo Magliocca. 2023. "Co-Creation in Health 4.0 as a New Solution for a New Era" Healthcare 11, no. 3: 363. https://doi.org/10.3390/healthcare11030363
APA StyleLaurisz, N., Ćwiklicki, M., Żabiński, M., Canestrino, R., & Magliocca, P. (2023). Co-Creation in Health 4.0 as a New Solution for a New Era. Healthcare, 11(3), 363. https://doi.org/10.3390/healthcare11030363






