The Burden of Alcohol-Related Emergency Department Visits in a Hospital of a Large European City
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Legal Issues
2.3. Study Setting
2.4. Participants
- 1.
- age 18 years and above;
- 2.
- confirmed alcohol consumption or positive alcohol test result, with presence of suspected alcohol consumption based on clinical symptoms (slurred speech, impaired balance, aggression, increase in talkativeness, altered perception of the environment); and
- 3.
- positive alcohol test in patients who were unconscious or had altered mental status.
- 4.
- In cases of doubt about a record’s inclusion, a decision was made after two authors were independently consulted.
2.5. Data Sources and Measurement
2.6. Variables
2.6.1. Primary Outcomes
2.6.2. Secondary Outcomes
2.7. Statistical Methods
3. Results
3.1. Primary Outcomes
3.1.1. Distribution of ED Visits
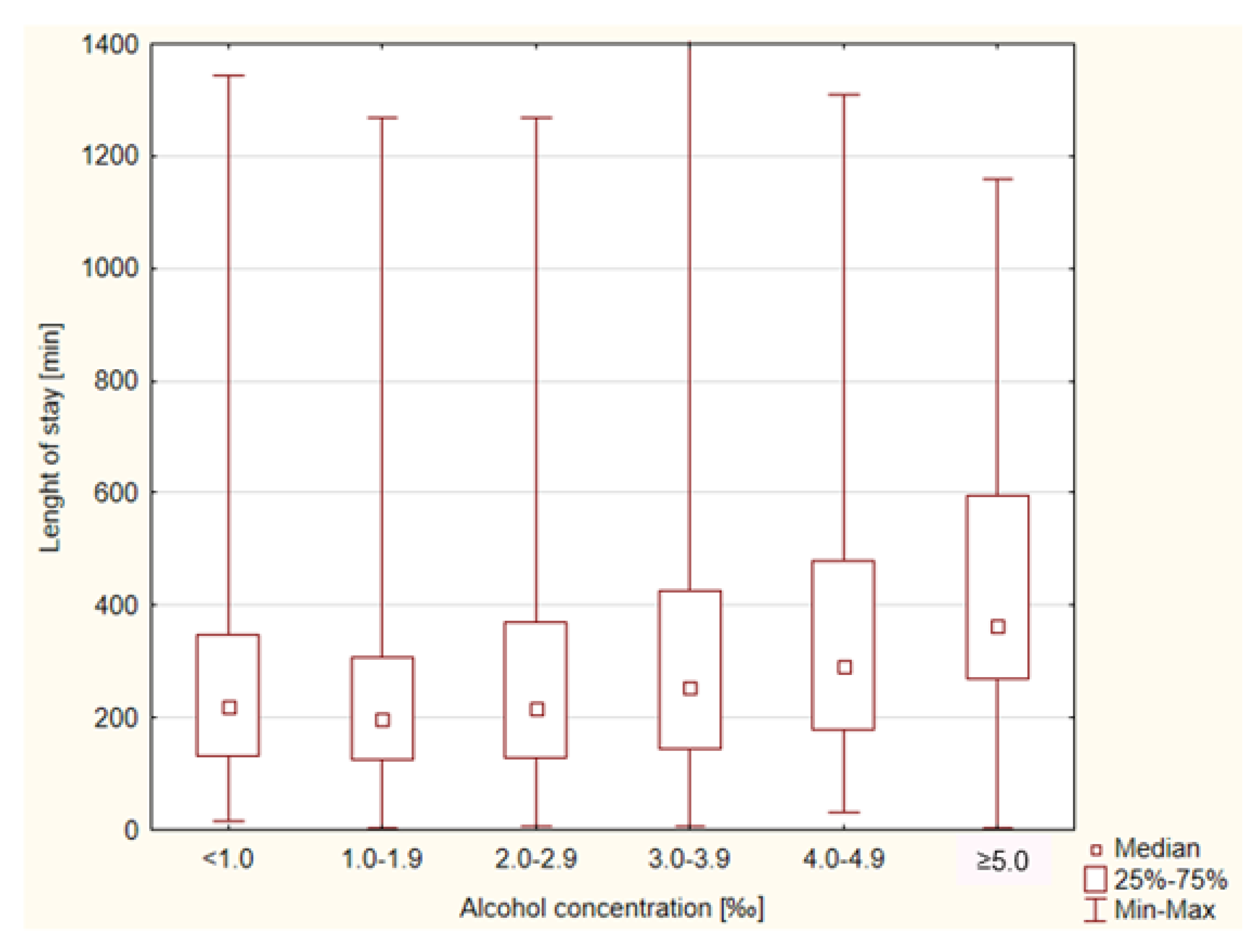
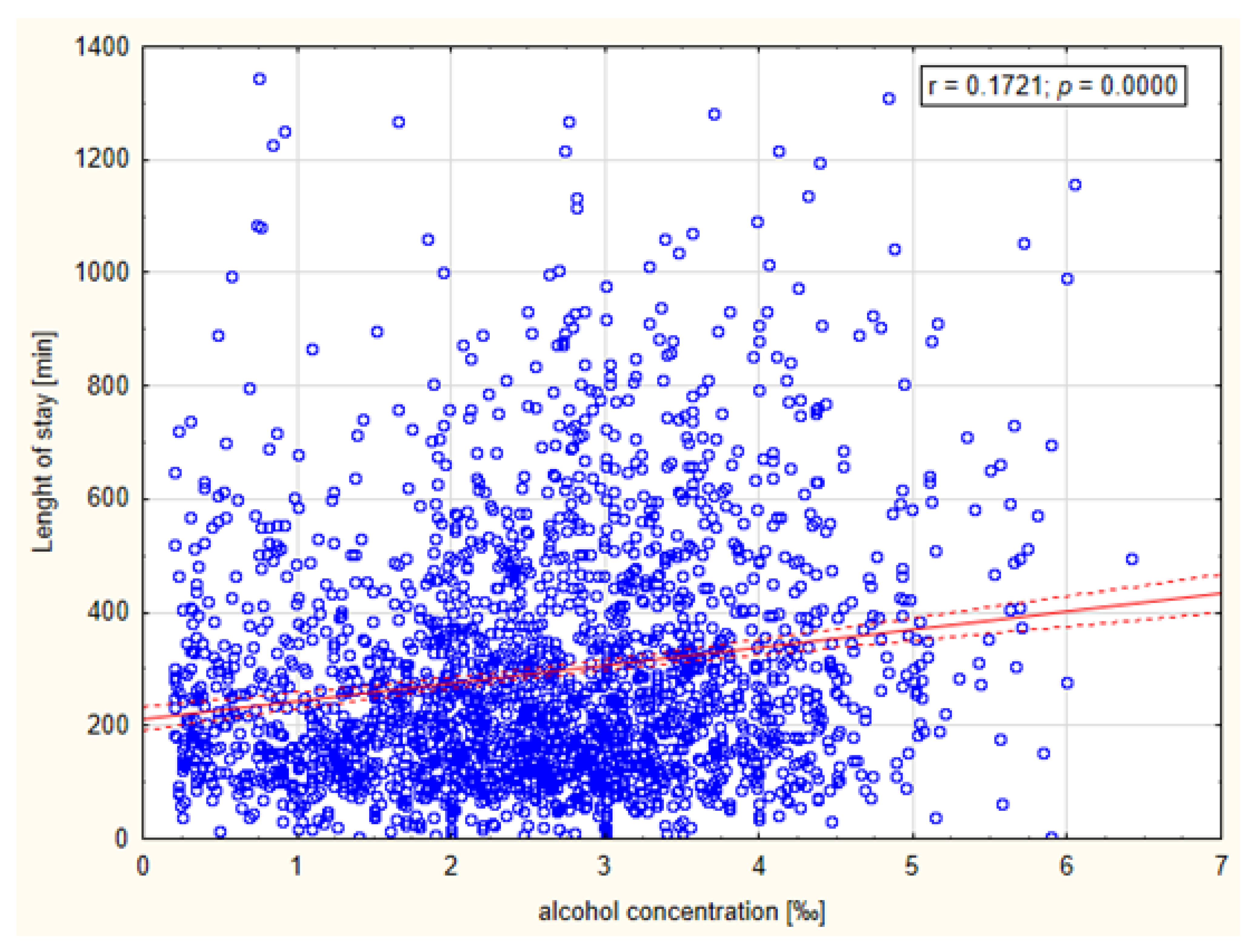
3.1.2. Resources
3.2. Secondary Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Alcohol Consumption, Harm and Policy Responses—Poland. Available online: https://www.euro.who.int/__data/assets/pdf_file/0005/402197/ACHP_FS_Poland.pdf (accessed on 9 September 2022).
- Alcohol, Recorded per Capita (15+) Consumption (in Litres of Pure Alcohol). Available online: https://www.who.int/data/gho/data/indicators/indicator-details/GHO/alcohol-recorded-per-capita-(15-)-consumption-(in-litres-of-pure-alcohol) (accessed on 9 September 2022).
- Średnie Roczne Spożycie Napojów Alkoholowych na 1 Mieszkańca w Litrach w Przeliczeniu na 100% Alkohol (w latach 1993-2021). Available online: https://www.parpa.pl/index.php/badania-i-informacje-statystyczne/statystyki (accessed on 9 September 2022).
- Frequency of Heavy Episodic Drinking by Sex, Age and Educational Attainment Level. Available online: https://ec.europa.eu/eurostat/databrowser/view/hlth_ehis_al3e/default/table?lang=en (accessed on 9 September 2022).
- Murdoch, D.; Pihl, R.O.; Ross, D. Alcohol and crimes of violence: Present issues. Int. J. Addict. 1990, 25, 1065–1081. [Google Scholar] [CrossRef]
- Connor, J.; Norton, R.; Ameratunga, S.; Jackon, R. The Contribution of Alcohol to Serious Car Crash Injuries. Epidemiology 2004, 15, 337–344. [Google Scholar] [CrossRef]
- Rehm, J.; Taylor, B.; Mohapatra, S.; Irving, H.; Baliunas, D.; Patra, J.; Roerecke, M. Alcohol as a risk factor for liver cirrhosis: A systematic review and meta-analysis. Drug Alcohol Rev. 2010, 29, 437–445. [Google Scholar] [CrossRef] [PubMed]
- Gardner, J.D.; Mouton, A.J. Alcohol effects on cardiac function. Compr. Physiol. 2015, 5, 791–802. [Google Scholar] [PubMed]
- Alcohol-Attributable Fractions (15+), Cancer Deaths. Available online: https://www.who.int/data/gho/data/indicators/indicator-details/GHO/alcohol-attributable-fractions-(15-)-cancer-deaths (accessed on 9 September 2022).
- Alcohol-Attributable Fractions (15+), Road Traffic Crash Deaths (%). Available online: https://www.who.int/data/gho/data/indicators/indicator-details/GHO/alcohol-attributable-fractions-(15-)-road-traffic-crash-deaths-(-) (accessed on 9 September 2022).
- Caputo, F.; Agabio, R.; Vignoli, T.; Patussi, V.; Fanucchi, T.; Cimarosti, P.; Meneguzzi, C.; Greco, G.; Rossin, R.; Parisi, M.; et al. Diagnosis and treatment of acute alcohol intoxication and alcohol withdrawal syndrome: Position paper of the Italian Society on Alcohol. Intern Emerg. Med. 2019, 14, 143–160. [Google Scholar] [CrossRef] [PubMed]
- Rehm, J.; Mathers, C.; Popova, S.; Thavorncharoensap, M.; Teerawattananon, Y.; Patra, J. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet Lond. Engl. 2009, 373, 2223–2233. [Google Scholar] [CrossRef]
- Mackie, D. Role of the emergency department. Emerg. Med. Australas EMA 2019, 31, 1109–1110. [Google Scholar] [CrossRef]
- Graber, T.W. Structure and function of the emergency department: Matching emergency department choices to the emergency department mission. Emerg. Med. Clin. North Am. 2004, 22, 47–72. [Google Scholar] [CrossRef]
- Verelst, S.; Moonen, P.-J.; Desruelles, D.; Gillet, J.-B. Emergency Department Visits Due to Alcohol Intoxication: Characteristics of Patients and Impact on the Emergency Room. Alcohol Alcohol 2012, 47, 433–438. [Google Scholar] [CrossRef]
- Kowalenko, T.; Burgess, B.; Szpunar, S.M.; Irvin-Babcock, C.B. Alcohol and trauma—In every age group. Am. J. Emerg. Med. 2013, 31, 705–709. [Google Scholar] [CrossRef]
- Cherpitel, C.J. Alcohol and injuries: A review of international emergency room studies. Addict. Abingdon Engl. 1993, 88, 923–937. [Google Scholar] [CrossRef] [PubMed]
- Joseph, D.; Vogel, J.A.; Smith, C.S.; Barrett, W.; Bryskiewicz, G.; Eberhardt, A.; Edwards, D.; Rappaport, L.; Colwell, C.B.; McVaney, K.E. Alcohol as a Factor in 911 Calls in Denver. Prehosp. Emerg. Care 2018, 22, 427–435. [Google Scholar] [CrossRef] [PubMed]
- McNicholl, B.; Goggin, D.; O’Donovan, D. Alcohol-related presentations to emergency departments in Ireland: A descriptive prevalence study. BMJ Open 2018, 8, e021932. [Google Scholar] [CrossRef] [PubMed]
- Calle, P.; Hautekiet, A.; Francois, H.; Sundahl, N.; Cornelis, C.; Calle, S.; Damen, J.; Vanbrabant, P.; De Turck, B.; De Graeve, K.; et al. Alcohol-related emergency department admissions among adolescents in the Ghent and Sint-Niklaas areas. Acta Clin. Belg. 2015, 70, 345–349. [Google Scholar] [CrossRef] [PubMed]
- Vanschoenbeek, G.M.; Hautekiet, T.; Calle, S.; Cornelis, C.; François, H.; Hautekiet, A.; Sundahl, N.; De Paepe, P.; Devriese, D.; De Graeve, K.; et al. Alcohol-related emergency department admissions in an elderly population. Acta Clin. Belg. 2019, 74, 194–199. [Google Scholar] [CrossRef]
- Pirmohamed, M.; Brown, C.; Owens, L.; Luke, C.; Gilmore, I.; Breckenridge, A.; Park, B. The burden of alcohol misuse on an inner-city general hospital. QJM Mon. J. Assoc. Physicians 2000, 93, 291–295. [Google Scholar] [CrossRef]
- Alcohol, Harmful Use (15+), 12 Month Prevalence (%) with 95%CI. Available online: https://www.who.int/data/gho/data/indicators/indicator-details/GHO/alcohol-harmful-use-(15-)-12-month-prevalence-(-)-with-95-ci (accessed on 9 September 2022).
- Alcohol, Heavy Episodic Drinking (15+), Drinkers Only, Past 30 Days (%). Available online: https://www.who.int/data/gho/data/indicators/indicator-details/GHO/alcohol-heavy-episodic-drinking-(population)-past-30-days-(-) (accessed on 9 September 2022).
- Knudsen, A.K.; Skogen, J.C. Monthly variations in self-report of time-specified and typical alcohol use: The Nord-Trøndelag Health Study (HUNT3). BMC Public Health 2015, 15, 172. [Google Scholar] [CrossRef]
- Maniaci, M.J.; Lachner, C.; Vadeboncoeur, T.F.; Hodge, D.O.; Dawson, N.L.; Rummans, T.A.; Roy, A.; Burton, M.C. Involuntary patient length-of-stay at a suburban emergency department. Am. J. Emerg. Med. 2020, 38, 534–538. [Google Scholar] [CrossRef]
- Klein, L.R.; Driver, B.E.; Miner, J.R.; Martel, M.L.; Cole, J.B. Emergency department length of stay for ethanol intoxication encounters. Am. J. Emerg. Med. 2018, 36, 1209–1214. [Google Scholar] [CrossRef]
- Jung, Y.-C.; Namkoong, K. Alcohol: Intoxication and poisoning—Diagnosis and treatment. Handb. Clin. Neurol. 2014, 125, 115–121. [Google Scholar]
- Shield, K.D.; Parry, C.; Rehm, J. Chronic diseases and conditions related to alcohol use. Alcohol Res. Curr. Rev. 2013, 35, 155–173. [Google Scholar]
- Iranpour, A.; Nakhaee, N. A Review of Alcohol-Related Harms: A Recent Update. Addict. Health 2019, 11, 129–137. [Google Scholar] [PubMed]
- Rehm, J.; Gmel, G.; Sempos, C.T. Alcohol-related morbidity and mortality. Alcohol Res. Health J. Natl. Inst. Alcohol Abuse Alcohol 2003, 27, 39–51. [Google Scholar]
- National Clinical Guideline Centre (UK). Alcohol Use Disorders: Diagnosis and Clinical Management of Alcohol-Related Physical Complications; Royal College of Physicians: London, UK, 2010. [Google Scholar]
- McLay, S.V.; MacDonald, E.; Fatovich, D.M. Alcohol-related presentations to the Royal Perth Hospital Emergency Department: A prospective study: Alcohol and Ed. Emerg. Med. Australas 2017, 29, 531–538. [Google Scholar] [CrossRef]
- Gentil, L.; Huỳnh, C.; Grenier, G.; Fleury, M.-J. Predictors of emergency department visits for suicidal ideation and suicide attempt. Psychiatry Res. 2020, 285, 112805. [Google Scholar] [CrossRef]
- Betz, M.E.; Boudreaux, E.D. Managing Suicidal Patients in the Emergency Department. Ann. Emerg. Med. 2016, 67, 276–282. [Google Scholar] [CrossRef]
- Eitel, D.R. The Emergency Severity Index Triage Algorithm Version 2 Is Reliable and Valid. Acad. Emerg. Med. 2003, 10, 1070–1080. [Google Scholar] [CrossRef]
- Müller, M.; Schechter, C.B.; Hautz, W.E.; Sauter, T.C.; Exadaktylos, A.K.; Stock, S.; Birrenbach, T. The development and validation of a resource consumption score of an emergency department consultation. PloS ONE 2021, 16, e0247244. [Google Scholar] [CrossRef]
| BAC 1 (‰) | Admission Rate (%) |
|---|---|
| <1.0 | 38.40 |
| 1.0–1.9 | 38.34 |
| 2.0–2.9 | 28.41 |
| 3.0–3.9 | 17.70 |
| 4.0–4.9 | 15.76 |
| ≥5.0 | 5.77 |
| Source | SS | DF | MS | F | p | Eta-Squared |
|---|---|---|---|---|---|---|
| BAC 1 | 3,999,189 | 4 | 999,797 | 21.746 | <0.001 * | 0.0367 |
| sex | 16,734 | 1 | 16,734 | 0.364 | 0.5463 | |
| interaction | 802,220 | 4 | 200,555 | 4.362 | 0.0016 * | 0.0076 |
| Error | 104,732,907 | 2278 | 45,976 | |||
| BAC 1 | 832,428 | 4 | 208,107 | 4.5086 | 0.0012 * | 0.0078 |
| radiology | 34,323 | 1 | 34,323 | 0.7436 | 0.3885 | |
| interaction | 388,466 | 4 | 97,117 | 2.1040 | 0.0778 | |
| Error | 105,146,483 | 2278 | 46,157 | |||
| BAC 1 | 1,244,006 | 4 | 311,002 | 6.730 | <0.001 * | 0.0116 |
| laboratory | 93,230 | 1 | 93,231 | 2.017 | 0.1556 | |
| interaction | 142,849 | 4 | 35,712 | 0.773 | 0.5427 | |
| Error | 105,269,567 | 2278 | 46,211 | |||
| BAC 1 | 2,937,682 | 4 | 734,421 | 16.406 | <0.001 * | 0.0280 |
| medications | 2,621,366 | 1 | 2,621,366 | 58.558 | <0.001 * | 0.0250 |
| interaction | 436,985 | 4 | 109,246 | 2.440 | 0.0449 * | 0.0042 |
| Error | 101,974,601 | 2278 | 44,765 | |||
| BAC 1 | 3,117,824 | 4 | 779,456 | 17.356 | <0.001 * | 0.0295 |
| sedation | 2,977,058 | 1 | 2,977,058 | 66.288 | <0.001 * | 0.0282 |
| interaction | 298,316 | 4 | 74,579 | 1.661 | 0.1564 | |
| Error | 102,306,551 | 2278 | 44,911 | |||
| BAC 1 | 850,714 | 4 | 212,679 | 4.6083 | 0.0010 * | 0.008 |
| suturing | 18,885 | 1 | 18,885 | 0.4092 | 0.5224 | |
| interaction | 378,143 | 4 | 94,536 | 2.0484 | 0.0851 | |
| Error | 105,131,932 | 2278 | 46,151 | |||
| BAC 1 | 167,389 | 4 | 41,847 | 0.9097 | 0.4572 | |
| decontamination | 411,859 | 1 | 411,860 | 8.9537 | 0.0027 * | 0.0039 |
| interaction | 316,435 | 4 | 79,109 | 1.7198 | 0.1428 | |
| Error | 104,784,962 | 2278 | 45,999 | |||
| BAC 1 | 3,186,348 | 4 | 796,587 | 17.267 | <0.001 * | 0.0297 |
| day of the week | 375,109 | 6 | 62,518 | 1.355 | 0.2292 | |
| interaction | 1,224,723 | 24 | 51,030 | 1.106 | 0.3273 | |
| Error | 103,941,645 | 2253 | 46,135 | |||
| BAC 1 | 3,255,132 | 4 | 813,783 | 17.659 | <0.001 * | 0.0307 |
| month | 723,288 | 11 | 65,753 | 1.427 | 0.1537 | |
| interaction | 1,957,041 | 44 | 44,478 | 0.965 | 0.5375 | |
| Error | 102,671,258 | 2228 | 46,082 | |||
| BAC 1 | 2,706,758 | 4 | 676,689 | 14.651 | <0.001 * | 0.0251 |
| Time interval | 146,408 | 2 | 73,204 | 1.585 | 0.2051 | |
| interaction | 469,089 | 8 | 58,636 | 1.270 | 0.2548 | |
| Error | 104,983,332 | 2273 | 46,187 |
| Resource | n | % |
|---|---|---|
| Radiology | 2186 | 95.46 |
| Laboratory tests | 1895 | 82.75 |
| Monitoring | 1396 | 60.96 |
| Medications | 1390 | 60.69 |
| Sedation | 502 | 21.92 |
| Suturing | 159 | 6.94 |
| Decontamination | 25 | 1.09 |
| Diagnosis (ICD-10 Code) | n | % |
|---|---|---|
| Alcohol-related disorders (F10) | 592 | 25.82 |
| Toxic effect of alcohol (T51) | 359 | 15.66 |
| Superficial injury of head (S00) | 122 | 5.32 |
| Open wound of head (S01) | 118 | 5.15 |
| Abdominal and pelvic pain (R10) | 63 | 2.75 |
| Pain in throat and chest (R07) | 58 | 2.53 |
| Evidence of alcohol involvement determined by level of intoxication (Y91) | 53 | 2.31 |
| Other general symptoms and signs (R68) | 41 | 1.79 |
| Syncope and collapse (R55) | 37 | 1.61 |
| Epilepsy and recurrent seizures (G40) | 32 | 1.40 |
| Intracranial injury (S06) | 27 | 1.17 |
| Other and unspecified injuries of head (S09) | 24 | 1.04 |
| Localization/Characteristics of Injury | n | % |
|---|---|---|
| Trauma in anamnesis | 610 | 26.64 |
| Injuries in examination | 451 | 19.69 |
| Injuries to the head | 344 | 76.27 |
| Injuries to the neck | 4 | 0.89 |
| Injuries to the thorax | 13 | 2.88 |
| Injuries to the abdomen, lower back, lumbar spine, and pelvis | 14 | 3.10 |
| Injuries to the lower extremity | 22 | 4.88 |
| Injuries to the upper extremity | 25 | 5.54 |
| Injuries involving multiple or unspecified body regions and foreign bodies | 24 | 5.32 |
| Burns, corrosions and frostbites | 4 | 0.89 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cholerzyńska, H.; Zasada, W.; Kłosiewicz, T.; Konieczka, P.; Mazur, M. The Burden of Alcohol-Related Emergency Department Visits in a Hospital of a Large European City. Healthcare 2023, 11, 786. https://doi.org/10.3390/healthcare11060786
Cholerzyńska H, Zasada W, Kłosiewicz T, Konieczka P, Mazur M. The Burden of Alcohol-Related Emergency Department Visits in a Hospital of a Large European City. Healthcare. 2023; 11(6):786. https://doi.org/10.3390/healthcare11060786
Chicago/Turabian StyleCholerzyńska, Hanna, Wiktoria Zasada, Tomasz Kłosiewicz, Patryk Konieczka, and Mateusz Mazur. 2023. "The Burden of Alcohol-Related Emergency Department Visits in a Hospital of a Large European City" Healthcare 11, no. 6: 786. https://doi.org/10.3390/healthcare11060786
APA StyleCholerzyńska, H., Zasada, W., Kłosiewicz, T., Konieczka, P., & Mazur, M. (2023). The Burden of Alcohol-Related Emergency Department Visits in a Hospital of a Large European City. Healthcare, 11(6), 786. https://doi.org/10.3390/healthcare11060786





