Ectopic Eye Tooth Management: Photobiomodulation/Low-Level Laser Emission Role in Root Resorption after Fixed Orthodontic Treatment
Abstract
1. Introduction
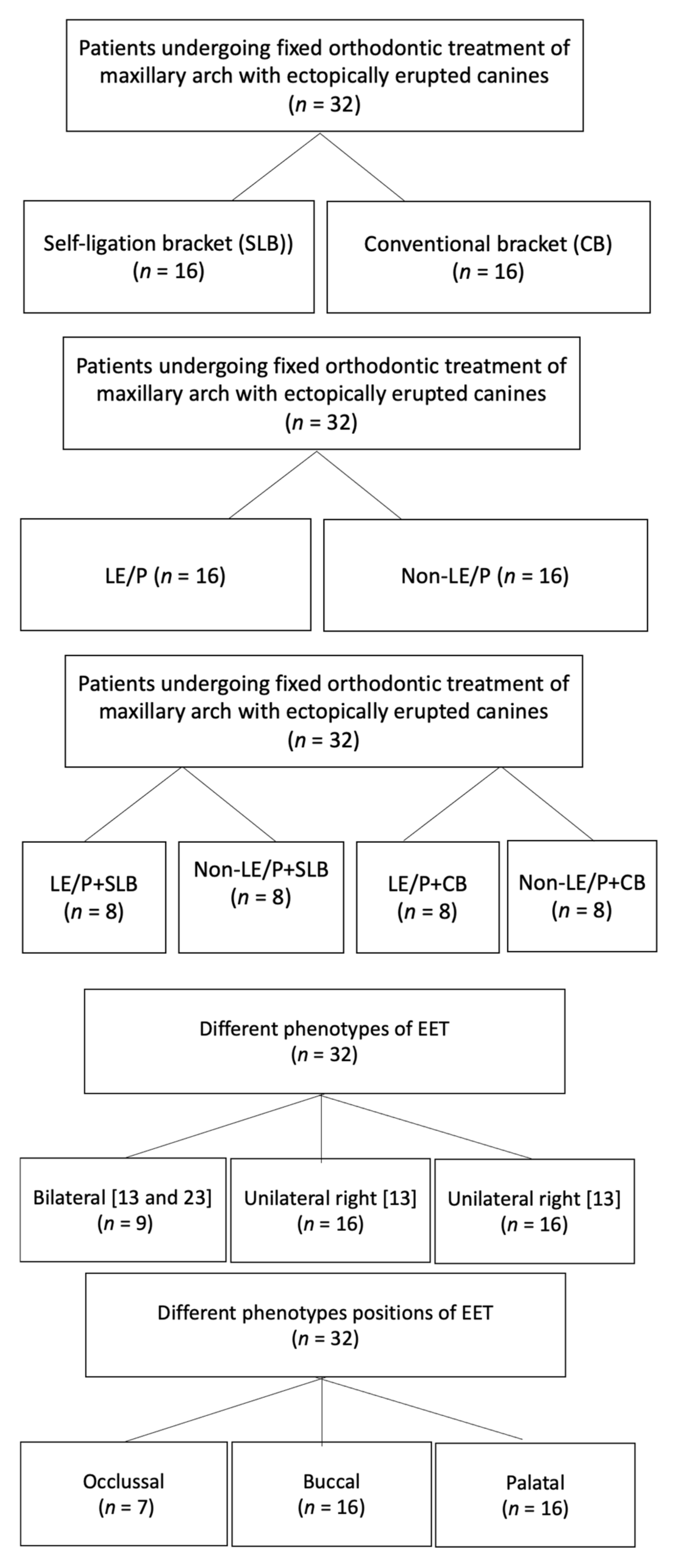
- in two-treatment modalities namely self-ligating bracket (SLB) vs. conventional bracket (CB).
- in two-treatment intervention (TI) (LE/P vs. non-LE/P).
- in four different TI (LE/P + SLB, LE/P + CB, non-LE/P + SLB, and non-LE/P + CB).
- in three different phenotypes of EET (Unilateral 13, Unilateral 23 and Bilateral)
- in three different phenotype positions of EET (Buccal, Occlusal and Palatal)
2. Materials and Methods
Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bishara, S. Textbook of Orthodontics; Saunders Company: Philadelphia, PA, USA, 2001; pp. 83–85. [Google Scholar]
- Ackerman, M.B. Enhancement Orthodontics: Theory and Practice; Wiley-Blackwell: Hoboken, NJ, USA, 2007. [Google Scholar]
- Talic, N.F. Adverse effects of orthodontic treatment: A clinical perspective. Saudi Dent. J. 2011, 23, 55–59. [Google Scholar] [CrossRef] [PubMed]
- Storey, E. The nature of tooth movement. Am. J. Orthod. 1973, 63, 292–314. [Google Scholar] [CrossRef]
- Mohammed, A.H.; Tatakis, D.N.; Dziak, R. Leukotrienes in orthodontic tooth movement. Am. J. Orthod. Dentofac. Orthop. 1989, 95, 231–237. [Google Scholar] [CrossRef]
- Proffit, W.R.; Fields, H.; Sarver, D. Contemporary Orthodontics, 4th ed.; Mosby: St. Louis, MI, USA, 2007. [Google Scholar]
- Sarver, D.M.; Proffit, W.; Ackerman, J. Diagnosis and treatment planning in orthodontics. In Orthodontics, Current Principles and Techniques, 3rd ed.; Mosby: St. Louis, MI, USA, 2000; Volume 27, p. 128. [Google Scholar]
- Parkin, N.; Benson, P.E.; Thind, B.; Shah, A.; Khalil, I.; Ghafoor, S. Open versus closed surgical exposure of canine teeth that are displaced in the roof of the mouth. Cochrane Database Syst. Rev. 2017, 2017, CD006966. [Google Scholar] [CrossRef]
- Levander, E.; Bajka, R.; Malmgren, O. Early radiographic diagnosis of apical root resorption during orthodontic treatment: A study of maxillary incisors. Eur. J. Orthod. 1998, 20, 57–63. [Google Scholar] [CrossRef]
- Brezniak, N.; Wasserstein, A. Orthodontically induced inflammatory root resorption. Part I: The basic science aspects. Angle Orthod. 2002, 72, 175–179. [Google Scholar]
- Hartsfield, J., Jr.; Everett, E.T.; Al-Qawasmi, R. Genetic factors in external apical root resorption and orthodontic treatment. Crit. Rev. Oral Biol. Med. 2004, 15, 115–122. [Google Scholar] [CrossRef]
- Qamruddin, I.; Alam, M.K.; Mahroof, V.; Fida, M.; Khamis, M.F.; Husein, A. Effects of low-level laser irradiation on the rate of orthodontic tooth movement and associated pain with self-ligating brackets. Am. J. Orthod. Dentofac. Orthop. 2017, 152, 622–630. [Google Scholar] [CrossRef]
- Qamruddin, I.; Alam, M.K.; Mahroof, V.; Fida, M.; Khamis, M.F.; Husein, A. Photobiostimulatory effect of a single dose of low-level laser on orthodontic tooth movement and pain. Pain Res. Manag. 2021, 2021, 6690542. [Google Scholar] [CrossRef]
- Alam, M.K. Laser-assisted orthodontic tooth movement in Saudi population: A prospective clinical intervention of low-level laser therapy in the 1st week of pain perception in four treatment modalities. Pain Res. Manag. 2019, 2019, 6271835. [Google Scholar] [CrossRef]
- Jawad, M.M.; Husein, A.; Alam, M.K.; Hassan, R.; Shaari, R. Overview of non-invasive factors (low level laser and low intensity pulsed ultrasound) accelerating tooth movement during orthodontic treatment. Lasers Med. Sci. 2014, 29, 367–372. [Google Scholar] [CrossRef]
- Alazzawi, M.M.J.; Husein, A.; Alam, M.K.; Hassan, R.; Shaari, R.; Azlina, A.; Salzihan, M. Effect of low level laser and low intensity pulsed ultrasound therapy on bone remodeling during orthodontic tooth movement in rats. Prog. Orthod. 2018, 19, 10. [Google Scholar] [CrossRef]
- Li, Y.; Deng, S.; Mei, L.; Li, Z.; Zhang, X.; Yang, C.; Li, Y. Prevalence and severity of apical root resorption during orthodontic treatment with clear aligners and fixed appliances: A cone beam computed tomography study. Prog. Orthod. 2020, 21, 1. [Google Scholar] [CrossRef]
- Patel, S.; Ford, T.P. Is the resorption external or internal? Dent. Update 2007, 34, 218–229. [Google Scholar] [CrossRef]
- Bille, M.; Kvetny, M.; Kjaer, I. A possible association between early apical resorption of primary teeth and ectodermal characteristics of the permanent dentition. Eur. J. Orthod. 2008, 30, 346–351. [Google Scholar] [CrossRef][Green Version]
- Brin, I.; Tulloch, J.C.; Koroluk, L.; Philips, C. External apical root resorption in Class II malocclusion: A retrospective review of 1-versus 2-phase treatment. Am. J. Orthod. Dentofac. Orthop. 2003, 124, 151–156. [Google Scholar] [CrossRef]
- Brezniak, N.; Goren, S.; Zoizner, R.; Dinbar, A.; Arad, A.; Wasserstein, A.; Heller, M. A comparison of three methods to accurately measure root length. Angle Orthod. 2004, 74, 786–791. [Google Scholar]
- Brusveen, E.M.G.; Brudvik, P.; Bøe, O.E.; Mavragani, M. Apical root resorption of incisors after orthodontic treatment of impacted maxillary canines: A radiographic study. Am. J. Orthod. Dentofac. Orthop. 2012, 141, 427–435. [Google Scholar] [CrossRef]
- Alqerban, A.; Jacobs, R.; Souza, P.C.; Willems, G. In-vitro comparison of 2 cone-beam computed tomography systems and panoramic imaging for detecting simulated canine impaction-induced external root resorption in maxillary lateral incisors. Am. J. Orthod. Dentofac. Orthop. 2009, 136, 764.e1–764.e11. [Google Scholar] [CrossRef]
- Sherrard, J.F.; Rossouw, P.E.; Benson, B.W.; Carrillo, R.; Buschang, P.H. Accuracy and reliability of tooth and root lengths measured on cone-beam computed tomographs. Am. J. Orthod. Dentofac. Orthop. 2010, 137, S100–S108. [Google Scholar] [CrossRef]
- Malmgren, O.; Goldson, L.; Hill, C.; Orwin, A.; Petrini, L.; Lundberg, M. Root resorption after orthodontic treatment of traumatized teeth. Am. J. Orthod. 1982, 82, 487–491. [Google Scholar] [CrossRef]
- Leite, V.; Conti, A.C.; Navarro, R.; Almeida, M.; Oltramari-Navarro, P.; Almeida, R. Comparison of root resorption between self-ligating and conventional preadjusted brackets using cone beam computed tomography. Angle Orthod. 2012, 82, 1078–1082. [Google Scholar] [CrossRef]
- Pandis, N.; Nasika, M.; Polychronopoulou, A.; Eliades, T. External apical root resorption in patients treated with conventional and self-ligating brackets. Am. J. Orthod. Dentofac. Orthop. 2008, 134, 646–651. [Google Scholar] [CrossRef]
- Chen, S.S.-H.; Greenlee, G.M.; Kim, J.-E.; Smith, C.L.; Huang, G.J. Systematic review of self-ligating brackets. Am. J. Orthod. Dentofac. Orthop. 2010, 137, 726.e1–726.e18. [Google Scholar] [CrossRef]
- Aras, I.; Unal, I.; Huniler, G.; Aras, A. Root resorption due to orthodontic treatment using self-ligating and conventional brackets. J. Orofac. Orthop. Fortschr. Der Kieferorthopädie 2018, 79, 181–190. [Google Scholar] [CrossRef]
- Ng, D.; Chan, A.K.; Papadopoulou, A.K.; Dalci, O.; Petocz, P.; Darendeliler, M.A. The effect of low-level laser therapy on orthodontically induced root resorption: A pilot double blind randomized controlled trial. Eur. J. Orthod. 2018, 40, 317–325. [Google Scholar] [CrossRef]
- Khaw, C.M.A.; Dalci, O.; Foley, M.; Petocz, P.; Darendeliler, M.A.; Papadopoulou, A.K. Physical properties of root cementum: Part 27. Effect of low-level laser therapy on the repair of orthodontically induced inflammatory root resorption: A double-blind, split-mouth, randomized controlled clinical trial. Am. J. Orthod. Dentofac. Orthop. 2018, 154, 326–336. [Google Scholar] [CrossRef]
- Lempesi, E.; Pandis, N.; Fleming, P.S.; Mavragani, M. A comparison of apical root resorption after orthodontic treatment with surgical exposure and traction of maxillary impacted canines versus that without impactions. Eur. J. Orthod. 2014, 36, 690–697. [Google Scholar] [CrossRef][Green Version]
- Janson, G.R.; de Luca Canto, G.; Martins, D.R.; Henriques, J.F.C.; de Freitas, M.R. A radiographic comparison of apical root resorption after orthodontic treatment with 3 different fixed appliance techniques. Am. J. Orthod. Dentofac. Orthop. 2000, 118, 262–273. [Google Scholar] [CrossRef]
- Jiang, R.-P.; McDonald, J.; Fu, M.-k. Root resorption before and after orthodontic treatment: A clinical study of contributory factors. Eur. J. Orthod. 2010, 32, 693–697. [Google Scholar] [CrossRef]




| Root Length Comparison before (R1) and after (R2) Orthodontic Treatment | Group | N | Mean Root Resorption R = (R2 − R1) mm | Std. Deviation | 95% Confidence Interval of the Difference | t-Value | |
|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||
| 11R1−11R2 | SLB | 16 | 0.29 | 0.18 | 0.19988 | 0.39262 | 2.02 |
| CB | 16 | 0.20 | 0.04 | 0.18389 | 0.22236 | ||
| 21R1−21R2 | SLB | 16 | 0.23 | 0.08 | 0.18226 | 0.27274 | −0.21 |
| CB | 16 | 0.23 | 0.06 | 0.19955 | 0.26670 | ||
| 12R1−12R2 | SLB | 16 | 0.18 | 0.23 | 0.05793 | 0.30332 | 0.08 |
| CB | 16 | 0.18 | 0.07 | 0.13628 | 0.21497 | ||
| 22R1−22R2 | SLB | 16 | 0.29 | 0.04 | 0.26827 | 0.31548 | 0.71 |
| CB | 16 | 0.28 | 0.07 | 0.23916 | 0.31459 | ||
| 13R1−13R2 | SLB | 16 | 0.57 | 0.13 | 0.50228 | 0.64147 | −3.91 |
| CB | 16 | 0.88 | 0.28 | 0.72614 | 1.02886 | ||
| 23R1−23R2 | SLB | 16 | 0.94 | 0.17 | 0.84683 | 1.03067 | −4.51 |
| CB | 16 | 1.19 | 0.14 | 1.11499 | 1.26376 | ||
| Root Length Comparison before (R1) and after (R2) Orthodontic Treatment | Group | N | Mean Root Resorption R = (R2 − R1) mm | Std. Deviation | 95% Confidence Interval of the Difference | t-Value | |
|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||
| 11R1−11R2 | LE/P | 16 | 0.30 | 0.08 | 0.01830 | 0.10920 | 0.28 |
| Non-LE/P | 16 | 0.22 | 0.05 | 0.01797 | 0.10953 | ||
| 21R1−21R2 | LE/P | 16 | 0.23 | 0.07 | −0.03820 | 0.05195 | 0.31 |
| Non-LE/P | 16 | 0.23 | 0.05 | −0.03833 | 0.05208 | ||
| 12R1−12R2 | LE/P | 16 | 0.23 | 0.18 | −0.06414 | 0.12539 | 0.66 |
| Non-LE/P | 16 | 0.19 | 0.06 | −0.06681 | 0.12806 | ||
| 22R1−22R2 | LE/P | 16 | 0.27 | 0.05 | −0.03439 | 0.03814 | 0.10 |
| Non-LE/P | 16 | 0.27 | 0.05 | −0.03439 | 0.03814 | ||
| 13R1−13R2 | LE/P | 16 | 0.56 | 0.12 | −0.46058 | −0.15692 | −4.15 |
| Non-LE/P | 16 | 0.87 | 0.27 | −0.46331 | −0.15419 | ||
| 23R1−23R2 | LE/P | 16 | 0.93 | 0.17 | −0.33628 | −0.11497 | −4.16 |
| Non-LE/P | 16 | 1.16 | 0.13 | −0.33653 | −0.11472 | ||
| Tooth | Groups | N (32) | Mean Resorption (R) | Std. Deviation | F Value | p Value |
|---|---|---|---|---|---|---|
| 11 | LE/P + SLB | 8 | 0.3750 | 0.22960 | 3.830 | 0.020 * |
| Non-LE/P + SLB | 8 | 0.2175 | 0.05651 | |||
| LE/P + CB | 8 | 0.2038 | 0.04955 | |||
| Non-LE/P + CB | 8 | 0.2025 | 0.01832 | |||
| 21 | LE/P + SLB | 8 | 0.2137 | 0.06523 | 0.204 | 0.893 |
| Non-LE/P + SLB | 8 | 0.2413 | 0.10371 | |||
| LE/P + CB | 8 | 0.2375 | 0.05548 | |||
| Non-LE/P + CB | 8 | 0.2287 | 0.07338 | |||
| 12 | LE/P + SLB | 8 | 0.2075 | 0.25645 | 0.323 | 0.809 |
| Non-LE/P + SLB | 8 | 0.1537 | 0.21494 | |||
| LE/P + CB | 8 | 0.1425 | 0.07086 | |||
| Non-LE/P + CB | 8 | 0.2088 | 0.06446 | |||
| 22 | LE/P + SLB | 8 | 0.2612 | 0.03563 | 1.770 | 0.176 |
| Non-LE/P + SLB | 8 | 0.3225 | 0.02816 | |||
| LE/P + CB | 8 | 0.2738 | 0.09164 | |||
| Non-LE/P + CB | 8 | 0.2800 | 0.04811 | |||
| 13 | LE/P + SLB | 8 | 0.5900 | 0.09118 | 5.076 | 0.006 * |
| Non-LE/P + SLB | 8 | 0.5537 | 0.16578 | |||
| LE/P + CB | 8 | 0.8362 | 0.27412 | |||
| Non-LE/P + CB | 8 | 0.9187 | 0.30638 | |||
| 23 | LE/P + SLB | 8 | 0.8125 | 0.11449 | 15.521 | 0.000 * |
| Non-LE/P + SLB | 8 | 1.0650 | 0.11928 | |||
| LE/P + CB | 8 | 1.2225 | 0.10859 | |||
| Non-LE/P + CB | 8 | 1.1563 | 0.16570 |
| Tooth | Ectopic Canine | N(32) | Mean | Std. Deviation | F Value | p Value |
|---|---|---|---|---|---|---|
| 11 | Bilateral | 9 | 0.1989 | 0.04343 | 1.703 | 0.200 |
| Unilateral 13 | 12 | 0.3033 | 0.20299 | |||
| Unilateral 23 | 11 | 0.2327 | 0.07086 | |||
| 21 | Bilateral | 9 | 0.2278 | 0.07259 | 0.007 | 0.993 |
| Unilateral 13 | 12 | 0.2308 | 0.04522 | |||
| Unilateral 23 | 11 | 0.2318 | 0.10157 | |||
| 12 | Bilateral | 9 | 0.2322 | 0.21730 | 0.636 | 0.536 |
| Unilateral 13 | 12 | 0.1600 | 0.12649 | |||
| Unilateral 23 | 11 | 0.1536 | 0.16931 | |||
| 22 | Bilateral | 9 | 0.2878 | 0.03701 | 1.002 | 0.380 |
| Unilateral 13 | 12 | 0.2667 | 0.05228 | |||
| Unilateral 23 | 11 | 0.3009 | 0.07648 | |||
| 13 | Bilateral | 9 | 0.6200 | 0.30749 | 0.975 | 0.389 |
| Unilateral 13 | 12 | 0.7750 | 0.29950 | |||
| Unilateral 23 | 11 | 0.7555 | 0.18190 | |||
| 23 | Bilateral | 9 | 1.0511 | 0.18937 | 0.236 | 0.791 |
| Unilateral 13 | 12 | 1.0425 | 0.18582 | |||
| Unilateral 23 | 11 | 1.0982 | 0.23549 |
| Tooth | Canine Position | N (32) | Mean | Std. Deviation | F Value | p Value |
|---|---|---|---|---|---|---|
| 11 | Occlusal | 7 | 0.2600 | 0.07000 | 0.964 | 0.393 |
| Buccal | 13 | 0.2108 | 0.03883 | |||
| Palatal | 12 | 0.2858 | 0.21232 | |||
| 21 | Occlusal | 7 | 0.2500 | 0.07047 | 0.346 | 0.710 |
| Buccal | 13 | 0.2208 | 0.06551 | |||
| Palatal | 12 | 0.2292 | 0.08670 | |||
| 12 | Occlusal | 7 | 0.1986 | 0.19239 | 0.158 | 0.855 |
| Buccal | 13 | 0.1869 | 0.14338 | |||
| Palatal | 12 | 0.1567 | 0.19047 | |||
| 22 | Occlusal | 7 | 0.2657 | 0.04467 | 1.095 | 0.348 |
| Buccal | 13 | 0.2769 | 0.06316 | |||
| Palatal | 12 | 0.3033 | 0.05959 | |||
| 13 | Occlusal | 7 | 0.6243 | 0.19139 | 0.772 | 0.472 |
| Buccal | 13 | 0.7246 | 0.24939 | |||
| Palatal | 12 | 0.7833 | 0.32129 | |||
| 23 | Occlusal | 7 | 1.1286 | 0.21575 | 0.621 | 0.545 |
| Buccal | 13 | 1.0685 | 0.18920 | |||
| Palatal | 12 | 1.0217 | 0.20919 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alam, M.K.; Ganji, K.K.; Alfawzan, A.A.; Manay, S.M.; Srivastava, K.C.; Chaudhari, P.K.; Hosni, H.A.; Alswairki, H.J.; Alansari, R.A. Ectopic Eye Tooth Management: Photobiomodulation/Low-Level Laser Emission Role in Root Resorption after Fixed Orthodontic Treatment. Healthcare 2022, 10, 610. https://doi.org/10.3390/healthcare10040610
Alam MK, Ganji KK, Alfawzan AA, Manay SM, Srivastava KC, Chaudhari PK, Hosni HA, Alswairki HJ, Alansari RA. Ectopic Eye Tooth Management: Photobiomodulation/Low-Level Laser Emission Role in Root Resorption after Fixed Orthodontic Treatment. Healthcare. 2022; 10(4):610. https://doi.org/10.3390/healthcare10040610
Chicago/Turabian StyleAlam, Mohammad Khursheed, Kiran Kumar Ganji, Ahmed Ali Alfawzan, Srinivas Munisekhar Manay, Kumar Chandan Srivastava, Prabhat Kumar Chaudhari, Hala A. Hosni, Haytham Jamil Alswairki, and Reem Ahmed Alansari. 2022. "Ectopic Eye Tooth Management: Photobiomodulation/Low-Level Laser Emission Role in Root Resorption after Fixed Orthodontic Treatment" Healthcare 10, no. 4: 610. https://doi.org/10.3390/healthcare10040610
APA StyleAlam, M. K., Ganji, K. K., Alfawzan, A. A., Manay, S. M., Srivastava, K. C., Chaudhari, P. K., Hosni, H. A., Alswairki, H. J., & Alansari, R. A. (2022). Ectopic Eye Tooth Management: Photobiomodulation/Low-Level Laser Emission Role in Root Resorption after Fixed Orthodontic Treatment. Healthcare, 10(4), 610. https://doi.org/10.3390/healthcare10040610










