Utilization of Artificial Intelligence in Disease Prevention: Diagnosis, Treatment, and Implications for the Healthcare Workforce
Abstract
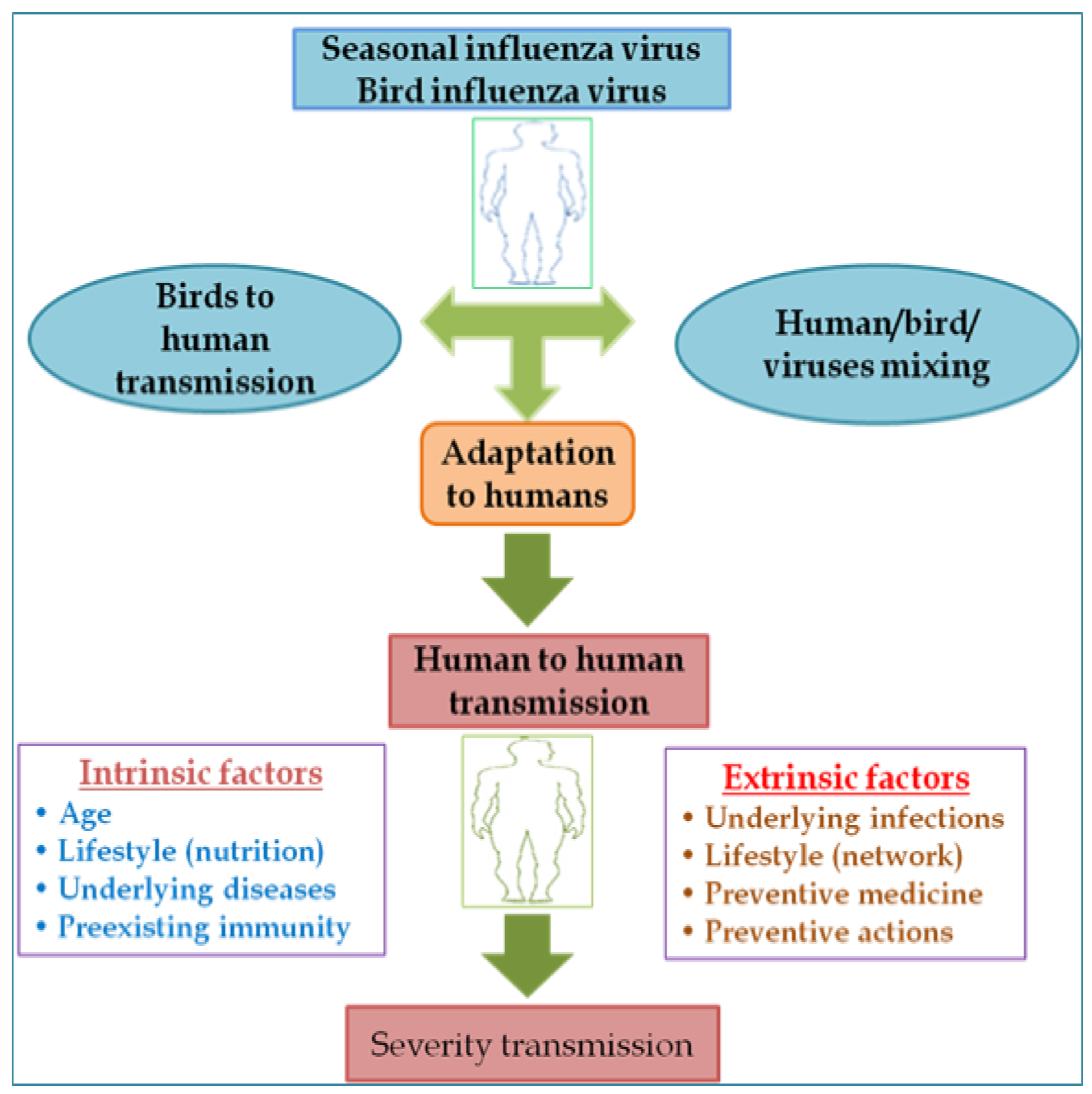
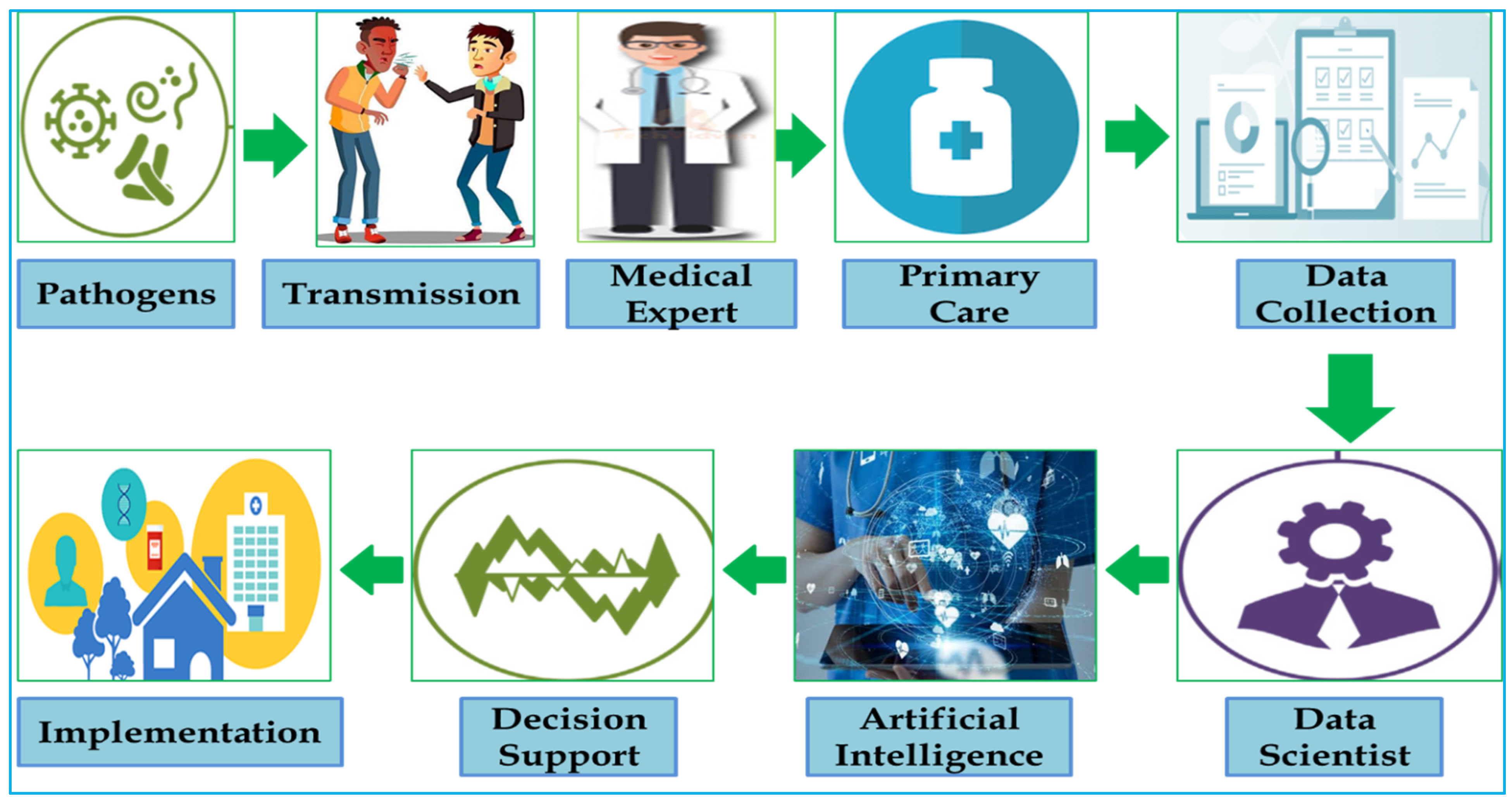
:1. Introduction
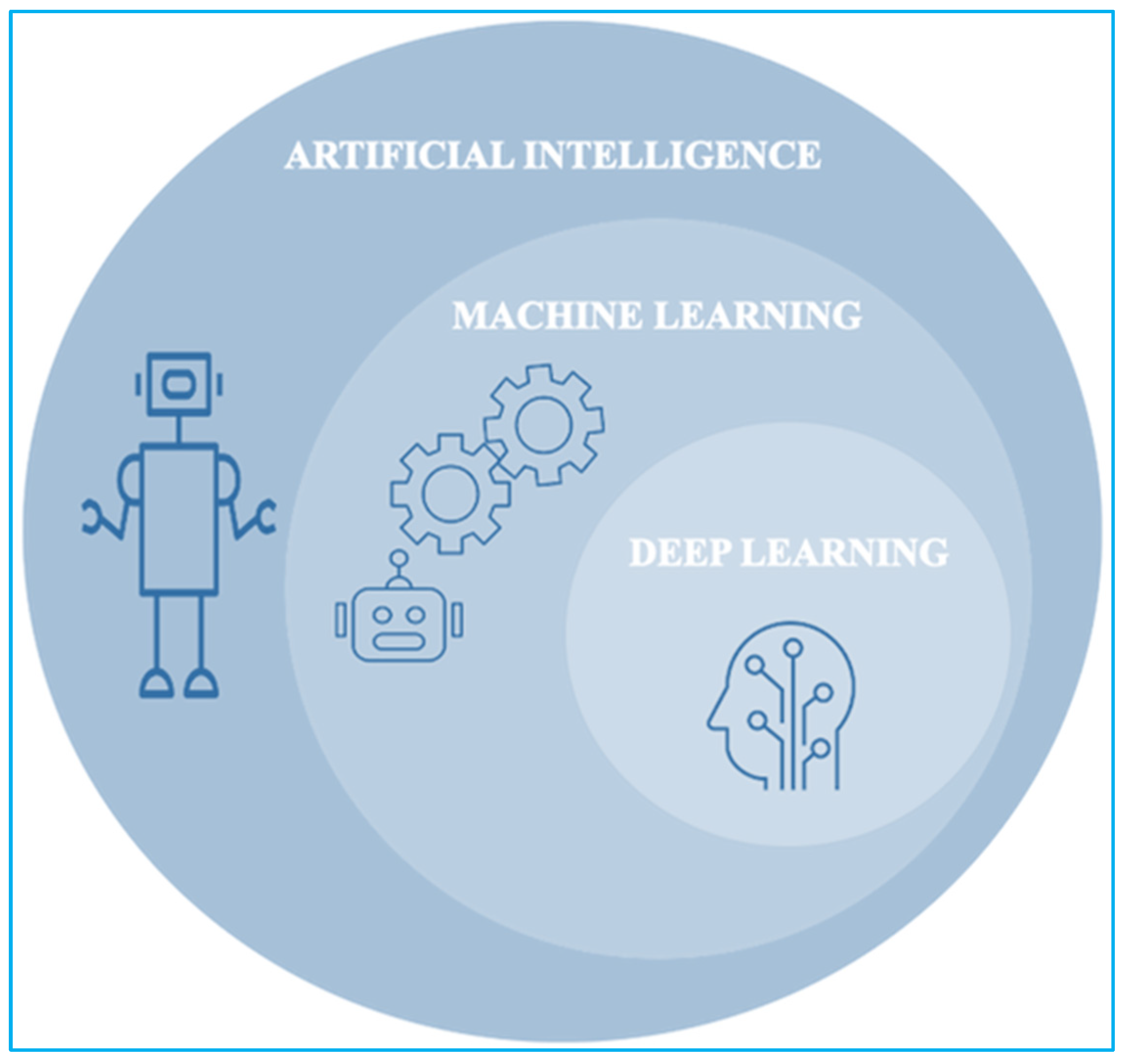
2. Types of AI Those Are Useful in Healthcare
2.1. Machine Learning and Deep Learning
2.2. Natural Language Processing
2.3. Robotic Process Automation
2.4. Explainable and Interpretable AI
2.5. Administrative Applications
3. Diagnosis and Treatment Applications
4. Applications for Patient Involvement and Adherence
5. Implications for the Healthcare Workforce
5.1. Bias
5.1.1. Understanding Bias
Mitigating Bias
Accounting for Bias
5.2. Various Implications for the Healthcare Workforce
5.3. AI to the Rescue
5.4. Productivity
5.5. Workload
5.6. Performance
5.7. Teamwork
5.8. Newer Challenges
5.9. Professional Liability
5.10. Labour Market Implications
5.11. Provider Competencies
6. Ethical Implications
6.1. Six Principles to Ensure that AI Serves the Public Interest in All Countries
6.1.1. Protecting Human Autonomy
6.1.2. Promoting Human Well-Being and Safety, as well as the Public Interest
6.1.3. Importance of Transparency, Explainability, and Intelligibility
6.1.4. Fostering Responsibility and Accountability
6.1.5. Ensuring Inclusiveness and Equity
6.1.6. Promoting AI that Is both Responsive and Sustainable
7. AI in Disaster Management
8. Conclusions
9. The Future of AI in Healthcare
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Infection Prevention and Control. 2021. Available online: https://www.who.int/health-topics/infection-prevention-and-control#tab=tab_1 (accessed on 4 May 2021).
- Taubenberger, J.K.; Morens, D.M. 1918 influenza: The mother of all pandemics. Emerg. Infect. Dis. 2006, 12, 15–22. [Google Scholar] [CrossRef] [PubMed]
- Silver, D.; Schrittwieser, J.; Simonyan, K.; Antonoglu, I.; Huang, A.; Guez, A.; Hubert, T.; Baker, L.; Lai, M.; Bolton, A.; et al. Mastering the game of Go without human knowledge. Nature 2017, 550, 354–359. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.H.; Asch, S.M. Machine learning and prediction in medicine—Beyond the peak of inflated expectations. N. Engl. J. Med. 2017, 376, 2507–2509. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boon, I.S.; Yong, T.P.T.A.; Boon, C.S. Assessing the role of artificial intelligence (AI) in clinical oncology: Utility of machine learning in radiotherapy target volume delineation. Medicines 2018, 5, 131. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Im, H.; Pathania, D.; McFarland, P.J.; Sohani, A.R.; Degani, I.; Allen, M.; Coble, B.; Kilcoyne, A.; Hong, S.; Rohrer, L.; et al. Design and clinical validation of a point-of-care device for the diagnosis of lymphoma via contrast-enhanced microholography and machine learning. Nat. Biomed. Eng. 2018, 2, 666–674. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Wickramarathne, T.L.; Chawla, N.V. Representing higher-order dependencies in networks. Sci. Adv. 2016, 2, E1600028. [Google Scholar] [CrossRef] [Green Version]
- Belle, A.; Kon, M.A.; Najarian, K. Biomedical informatics for computer-aided decision support systems: A survey. Sci. World J. 2013, 2013, E769639. [Google Scholar] [CrossRef] [Green Version]
- Deloitte Insights State of AI in the Enterprise Deloitte. 2018. Available online: https://www2.deloitte.com/content/dam/insights/us/articles/4780_State-of-AI-in-the-enterprise/DI_State-of-AI-in-the-enterprise-2nd-ed.pdf (accessed on 5 December 2021).
- Lee, S.I.; Celik, S.; Logsdon, B.A.; Lundberg, S.M.; Martins, T.J.; Oehler, V.G.; Estey, E.H.; Miller, C.P.; Chien, S.; Dai, J.; et al. A machine learning approach to integrate big data for precision medicine in acute myeloid leukemia. Nat. Commun. 2018, 9, 42. [Google Scholar] [CrossRef]
- Sordo, M. Introduction to Neural Networks in Healthcare. Open Clin. 2002. Available online: www.openclinical.org/docs/int/neuralnetworks011.pdf (accessed on 20 November 2021).
- Fakoor, R.; Ladhak, F.; Nazi, A.; Huber, M. Using deep learning to enhance cancer diagnosis and classification. A conference presentation. In Proceedings of the 30th International Conference on Machine Learning, Atlanta, GA, USA, 21 June 2013. [Google Scholar]
- Vial, A.; Stirling, D.; Field, M.; Ros, M.; Ritz, C.; Carolan, M.; Holloway, L.; Miller, A.A. The role of deep learning and radiomic feature extraction in cancer-specific predictive modelling: A review. Transl. Cancer Res. 2018, 7, 803–816. [Google Scholar] [CrossRef]
- Pourhomayoun, M.; Shakibi, M. Predicting mortality risk in patients with COVID-19 using artificial intelligence to help medical decision-making. Smart Health 2021, 20, E100171. [Google Scholar] [CrossRef] [PubMed]
- Ho, T.S.; Weng, T.-C.; Wang, J.-D.; Han, H.-C.; Cheng, H.-C.; Yang, C.-C.; Yu, C.-H.; Liu, Y.-J.; Hu, C.H.; Huang, C.-Y.; et al. Comparing machine learning with case-control models to identify confirmed dengue cases. PLoS Negl. Trop. Dis. 2020, 14, E0008843. [Google Scholar] [CrossRef] [PubMed]
- Weng, S.F.; Reps, J.; Kai, J.; Garibaldi, J.M.; Qureshi, N. Can machine-learning improve cardiovascular risk prediction using routine clinical data? PLoS ONE 2017, 12, E0174944. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chiu, H.-Y.R.; Hwang, C.-K.; Chen, S.-Y.; Shih, F.-Y.; Han, H.-C.; King, C.-C.; Gilbert, J.R.; Fang, C.-C.; Oyang, Y.-J. Machine learning for emerging infectious disease field responses. Sci. Rep. 2022, 12, E328. [Google Scholar] [CrossRef]
- Alfred, R.; Obit, J.H. The role of machine learning methods in limiting the speed of deadly diseases: A systematic review. Heliyon 2021, 7, E07371. [Google Scholar] [CrossRef]
- Zhang, Y.-H.; Hu, X.-F.; Ma, J.-C.; Wang, X.-Q.; Luo, H.-R.; Wu, Z.-F.; Zhang, S.; Shi, D.-J.; Yu, Y.-Z.; Qiu, X.-M.; et al. Clinical applicable AI system based on deep learning algorithm for differentiation of pulmonary infectious disease. Front. Med. 2021, 8, E753055. [Google Scholar] [CrossRef]
- James, G.; Witten, D.; Hastie, T.; Tibshirani, R. An Introduction to Statistical Learning; Springer: Berlin/Heidelberg, Germany, 2013; Volume 112. [Google Scholar]
- Cortes, C.; Vapnik, V. Support-vector networks. Mach. Learn. 1995, 20, 273–297. [Google Scholar] [CrossRef]
- Cho, S.; Hong, H.; Ha, B.-C. A hybrid approach based on the combination of variable selection using decision trees and casebased reasoning using the Mahalanobis distance: For bankruptcy prediction. Expert Syst. Appl. 2010, 37, 3482–3488. [Google Scholar] [CrossRef]
- Therneau, T.M.; Atkinson, B.; Ripley, M.B. The Rpart Package; R Foundation for Statistical Computing: Oxford, UK, 2010. [Google Scholar]
- Maimon, O.Z.; Rokach, L. Data Mining with Decision Trees: Theory and Applications; World Scientific: Singapore, 2014; Volume 81. [Google Scholar]
- Sa-Ngamuang, C.; Haddawy, P.; Luvira, V.; Piyaphanee, W.; Iamsirithaworn, S.; Lawpoolsri, S. Accuracy of dengue clinical diagnosis with and without NS1 antigen rapid test: Comparison between human and Bayesian network model decision. PLoS Negl. Trop. Dis. 2018, 12, E0006573. [Google Scholar] [CrossRef]
- Kim, H.-J.; Han, D.; Kim, J.-H.; Kim, D.; Ha, B.; Seong, W.; Lee, Y.-K.; Lim, D.; Hong, S.O.; Park, M.-J.; et al. An easy-to-use machine learning model to predict the prognosis of patients with COVID-19: Retrospective cohort study. J. Med. Internet Res. 2020, 22, E24225. [Google Scholar] [CrossRef]
- Liang, W.; Yao, J.; Chen, A.; Lv, Q.; Zanin, M.; Liu, J.; Wong, S.; Li, Y.; Lu, J.; Liang, H.; et al. Early triage of critically ill COVID-19 patients using deep learning. Nat. Commun. 2021, 11, E826. [Google Scholar] [CrossRef] [PubMed]
- Wu, G.; Yang, P.; Xie, Y.; Woodruff, H.C.; Rao, X.; Guiot, J.; Frix, A.-N.; Louis, R.; Moutschen, M.; Li, J.; et al. Development of a clinical decision support system for severity risk prediction and triage of COVID-19 patients at hospital admission: An international multicentre study. Eur. Respir. J. 2020, 56, E2001104. [Google Scholar] [CrossRef]
- Esteva, A.; Robicquet, A.; Ramsundar, B.; Kuleshov, V.; DePristo, M.; Chou, K.; Cui, C.; Corrado, G.; Thrun, S.; Dean, J. A guide to deep learning in healthcare. Nat. Med. 2019, 25, 24–29. [Google Scholar] [CrossRef] [PubMed]
- Bresnick, J. “What is the Role of Natural Language Processing in Healthcare?” Health IT Analytics. 2020. Available online: https://healthitanalytics.com/features/what-is-the-role-of-natural-language-processing-in-healthcare (accessed on 25 November 2021).
- Juhn, Y.; Liu, H. Artificial intelligence approaches using natural language processing to advance EHR-based clinical research. J. Allerg. Clin. Immunol. 2020, 145, 463–469. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rangasamy, S.; Nadenichek, R.; Rayasam, M.; Sozdatelev, A. Natural Language Processing in Healthcare. McKinsey & Company. 2018. Available online: https://www.mckinsey.com/industries/healthcare-systems-and-services/our-insights (accessed on 31 December 2021).
- Hussain, A.; Malik, A.; Halim, M.U.; Ali, A.M. The use of robotics in surgery: A review. Int. J. Clin. Pract. 2014, 68, 1376–1382. [Google Scholar] [CrossRef]
- Lotsch, J.; Kringel, D.; Ultsch, A. Explainable artificial intelligence (XAI) in biomedicine: Making AI decisions trustworthy for physicians and patients. Biomedinformatics 2022, 2, 1–17. [Google Scholar] [CrossRef]
- Linardatos, P.; Papastefanopoulos, V.; Kotasiantis, S. Explainable AI: A review of machine learning interpretability methods. Entropy 2021, 23, 18. [Google Scholar] [CrossRef]
- Lipton, Z.C. The mythos of model interpretability. Queue 2018, 16, 31–57. [Google Scholar] [CrossRef]
- Doshi-Velez, F.; Kim, B. Towards a rigorous science of interpretable machine learning. arXiv 2017, arXiv:1702.08608. [Google Scholar]
- Gilpin, L.H.; Bau, D.; Yuan, B.Z.; Bajwa, A.; Specter, M.; Kagal, L. Explaining explanations: An overview of interpretability of machine learning. In Proceedings of the 2018 IEEE 5th International Conference on Data Science and Advanced Analytics (DSAA), Turin, Italy, 1–3 October 2018; pp. 80–89. [Google Scholar]
- Adadi, A.; Berrada, M. Peeking inside the black-box: A survey on explainable artificial intelligence (XAI). IEEE Access 2018, 6, 52138–52160. [Google Scholar] [CrossRef]
- Datta, A.; Matlock, M.K.; Dang, N.L.; Moulin, T.; Woeltje, K.F.; Yanik, E.L.; Swamidass, S.J. Black box’ to ‘conversational’ machine learning: Ondansetron reduces risk of hospital-acquired venous thromboembolism. IEEE J. Biomed. Health Informat. 2021, 25, 2204–2214. [Google Scholar] [CrossRef] [PubMed]
- Datta, A.; Flynn, N.R.; Barnette, D.A.; Woeltje, K.F.; Miller, J.P.; Swamidass, S.J. Machine learning liver-injuring drug interactions with non-steroidal anti-inflammatory drugs (NSAIDs) from a retrospective electronic health record (EHR) cohort. PLoS Comput. Biol. 2021, 17, E1009053. [Google Scholar] [CrossRef] [PubMed]
- Shamshirband, S.; Fathi, M.; Dehzangi, A.; Chronopoulos, A.T.; Alinejad-Rokny, H. A review on deep learning approaches in healthcare systems: Taxonomies, challenges, and open issues. J. Biomed. Infomat. 2021, 113, E103627. [Google Scholar] [CrossRef] [PubMed]
- Naser, M.Z. An engineer’s guide to eXplainable artificial intelligence and interpretable machine learning: Navigating causality, forced goodness, and the false perception of inference. Autom. Const. 2021, 129, E103821. [Google Scholar] [CrossRef]
- Dikshit, A.; Pradhan, B. Interpretable and explainable AI (XAI) model for spatial drought prediction. Sci. Total Environ. 2021, 801, E149797. [Google Scholar] [CrossRef]
- Berg, S. Nudge Theory Explored to Boost Medication Adherence; American Medical Association: Chicago, IL, USA, 2018; Available online: www.ama-assn.org/delivering-care/patient-support-advocacy/nudge-theory-exploredboost-medication-adherence (accessed on 20 October 2021).
- Commins, J. Nurses Say Distractions Cut Bedside Time by 25%. Health Leaders. 2010. Available online: www.healthleadersmedia.com/nursing/nurses-say-distractions-cut-bedside-time-25 (accessed on 10 October 2021).
- Utermohlen, K. Four robotic Process Automation (RPA) Applications in the Healthcare Industry. Medium. 2018. Available online: https://medium.com/@karl.utermohlen/4-robotic-process-automation-rpa-applications-inthe-healthcare-industry-4d449b24b613 (accessed on 10 September 2021).
- Buchanan, B.G.; Shortliffe, E.H. Rule-Based Expert Systems: The MYCIN Experiments of the Stanford Heuristic Programming Project; Reading, Addison-Wesley: Boston, MA, USA, 1984. [Google Scholar]
- Davenport, T.H. The AI Advantage Cambridge; MIT Press: Cambridge, MA, USA, 2018. [Google Scholar]
- Ross, C.; Swetlitz, I. IBM Pitched Its Watson Supercomputer as a Revolution in Cancer Care. It’s Nowhere Close Stat. 2017. Available online: www.statnews.com/2017/09/05/watson-ibm-cancer (accessed on 4 May 2021).
- Right Care Shared Decision Making Programme, Capita. Measuring Shared Decision Making: A Review of Research Evidence. NHS. 2012. Available online: www.england.nhs.uk/wp-content/uploads/2013/08/7sdm-report.pdf (accessed on 4 May 2021).
- Loria, K. Putting the AI in Radiology. Radiol. Today 2018, 19, 10. Available online: www.radiologytoday.net/archive/rt0118p10.shtml (accessed on 4 May 2021).
- Schmidt-Erfurth, U.; Bogunovic, H.; Sadeghipour, A.; Schlegl, T.; Langs, G.; Gerendas, B.S.; Osborne, A.; Waldstein, S.M. Machine learning to analyze the prognostic value of current imaging biomarkers in neovascular age-related macular degeneration. Opthamol. Retina 2018, 2, 24–30. [Google Scholar] [CrossRef]
- Aronson, S.; Rehm, H. Building the foundation for genomic-based precision medicine. Nature 2015, 526, 336–342. [Google Scholar] [CrossRef]
- Rysavy, M. Evidence-based medicine: A science of uncertainty and an art of probability. Virtual Mentor 2013, 15, 4–8. [Google Scholar]
- Davenport, T.H.; Hongsermeier, T.; Mc Cord, K.A. Using AI to Improve Electronic Health Records Harvard Business Review. 2018. Available online: https://hbr.org/2018/12/using-ai-to-improve-electronic-health-records (accessed on 4 May 2021).
- Volpp, K.G.; Mohta, N.S. Patient Engagement Survey: Improved Engagement Leads to Better Outcomes, but Better Tools Are Needed. Insights Report. NEJM Catalyst. 2016. Available online: https://catalyst.nejm.org/doi/full/10.1056/CAT.16.0842#:~:text=in%20the%20world.-,Patient%20Engagement%20Survey%3A%20Improved%20Engagement%20Leads%20to%20Better%20Outcomes%2C%20but,appear%20to%20be%20the%20norm. (accessed on 4 May 2021).
- User Testing. Healthcare Chatbot Apps Are on the Rise but the Overall Customer Experience (cx) Falls Short According to a UserTesting Report; User Testing: San Francisco, CA, USA, 2019. [Google Scholar]
- Deloitte from Brawn to Brains: The Impact of Technology on Jobs in the UK. Deloitte. 2015. Available online: www2.deloitte.com/content/dam/Deloitte/uk/Documents/Growth/deloitte-uk-insights-from-brawns-to-brain.pdf (accessed on 1 May 2021).
- McKinsey Global Institute. A Future that Works: Automation, Employment, and Productivity McKinsey Global Institute. 2017. Available online: www.mckinsey.com/∼/media/mckinsey/featured%20insights/Digital%20Disruption/Harnessing%20automation%20for%20a%20future%20that%20works/MGI-A-future-that-works-Executive-summary.ashx (accessed on 28 April 2021).
- Obermeyer, Z.; Powers, B.; Vogeli, C.; Mullainathan, S. Dissecting racial bias in an algorithm used to manage the health of populations. Science 2019, 366, 447–453. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, M.P.; Ghorbani, A.; Zou, J. Multiaccuracy: Black-box-post-processing for fairness in classification. AIES 2019, 247–254. [Google Scholar]
- Atzmueller, M. Declarative aspects in explicative data mining for computational sense making. In Declarative Programming and Knowledge Management; Springer: Heidelberg, Germany, 2018; pp. 97–114. [Google Scholar]
- Guidotti, R.; Monreale, A.; Ruggieri, S.; Turini, F.; Giannotti, F.; Pedreschi, D. A survey of methods for explaining black box models. ACM Comput. Surv. 2019, 51, E93. [Google Scholar] [CrossRef] [Green Version]
- Kletzer, L.G. The question with AI isn’t whether we’ll lose our jobs—It’s how much we’ll get paid. Available online: https://hbr.org/2018/01/the-question-with-ai-isnt-whether-well-lose-our-jobs-its-how-much-well-get-paid (accessed on 11 November 2019).
- Robert, N. How artificial intelligence is changing nursing. Nurs. Manag. 2019, 50, 30–39. [Google Scholar] [CrossRef] [PubMed]
- Davenport, T.H.; Glover, W.J. Artificial intelligence and the augmentation of health care decision-making. N. Engl. J. Med. Catalyst. 2018, 4. Available online: https://catalyst.nejm.org/ai-technologies-augmentation-healthcare-decisions/ (accessed on 11 November 2019).
- Marine, A.; Ruotsalainen, J.H.; Serra, C.; Verbeek, J.H. Preventing occupational stress in healthcare workers. Cochrane Database Syst. Rev. 2006, 4, CD002892. [Google Scholar]
- Nieuwenhuijsen, K.; Bruinvels, D.; Frings-Dresen, M. Psychosocial work environment and stress related disorders, a systematic review. Occup. Med. 2010, 60, 277–286. [Google Scholar] [CrossRef] [Green Version]
- Erickson, S.M.; Rockwern, B.; Koltov, M.; McLean, R.M.; Medical Practice and Quality Committee of the American College of Physicians. Putting patients first by reducing administrative tasks in health care: A position paper of the American college of physicians. Ann. Intern. Med. 2017, 16, 659–661. [Google Scholar] [CrossRef] [Green Version]
- Sinsky, C.; Colligan, L.; Li, L.; Prgomet, M.; Reynolds, S.; Goeders, L.; Westbrook, J.; Tutty, M.; Bilke, G. Allocation of physician time in ambulatory practice: A time and motion study in 4 specialties. Ann. Intern. Med. 2016, 165, 753–760. [Google Scholar] [CrossRef]
- Accenture. Artificial Intelligence is the Future of Growth. Available online: https://www.accenture.com/us-en/insight-artificial-intelligence-future-growth (accessed on 11 November 2021).
- Bresnick, J. Amazon Takes on Unstructured EHR Data with Machine Learning. NLP. Available online: https://healthitanalytics.com/news/amazon-takes-on-unstructured-ehr-data-with-machine-learning-nlp (accessed on 11 November 2021).
- Hosny, A.; Parmar, C.; Quackenbush, J.; Schwartz, L.H.; Aerts, H.J.W.L. Artificial intelligence in radiology. Nat. Rev. Cancer 2018, 18, 500–510. [Google Scholar] [CrossRef]
- Nsoesie, E.O. Evaluating artificial intelligence applications in clinical settings. JAMA Netw. Open 2018, 1, E182658. [Google Scholar] [CrossRef] [Green Version]
- Nundy, S.; Hodgkins, M.L. The application of AI to Augment Physicians and Reduce Burnout. Health Affairs Blog. 18 September 2018. Available online: https://www.healthaffairs.org/do/10.1377/forefront.20180914.711688/ (accessed on 15 November 2021).
- AiCure. NIH Expects AiCure Technologies’s New Adherence Monitoring Platform to Have “a Significant Impact… [and] Widespread Application in Research and in Care”. Press Release. Available online: https://aicure.com/news/nih-expects-aicure-technologiess-new-adherence-monitoring-platform-to-have-a-significant-impact-and-widespread-application-in-research-and-in-care/ (accessed on 15 November 2021).
- Wartman, S.; Combs, C. Medical education must move from the information age to the age of artificial intelligence. Acad. Med. 2018, 93, 1107–1119. [Google Scholar] [CrossRef] [PubMed]
- Nuffield Council on Bioethics. Bioethics Briefing Note. Artificial Intelligence (AI) in Healthcare and Research. Available online: http://nuffieldbioethics.org/project/briefing-notes/artificial-intelligence-ai-healthcare-research (accessed on 15 November 2021).
- Davenport, T.H.; Dreyer, K. AI Will Change Radiology, but It Won’t Replace Radiologists. Harv. Bus. Rev. 2018. Available online: https://hbr.org/2018/03/ai-will-change-radiology-but-it-wont-replace-radiologists (accessed on 15 November 2021).
- Available online: https://becominghuman.ai/the-ethics-of-artificial-intelligence-in-healthcare-5fe148427764 (accessed on 15 November 2021).
- World Health Organisation. WHO Issues First Global Report on Artificial Intelligence (AI) in Health and Six Guiding Principles for Its Design and Use. 2021. Available online: https://www.who.int/news/item/28-06-2021-who-issues-first-global-report-on-ai-in-health-and-six-guiding-principles-for-its-design-and-use (accessed on 15 December 2021).
- Murdoch, B. Privacy and artificial intelligence: Challenges for protecting health information in a new era. BMC Med. Ethics 2021, 22, E122. [Google Scholar] [CrossRef] [PubMed]
- Iacobucci, G. Patient data were shared with Google on an “inappropriate legal basis”, says NHS data guardian. BMJ 2017, 357, j2439. [Google Scholar] [CrossRef] [PubMed]
- More, Y.M. Disaster management using artificial intelligence. J. Xian Uni. Agric. Technol. 2019, 11, 1633–1637. [Google Scholar]
- Saravi, S.; Kalawsky, R.; Joannou, D.; Casado, M.R.; Fu, G.; Meng, F. Use of artificial intelligence to improve resilience and preparedness against adverse food events. Water 2019, 11, 973. [Google Scholar] [CrossRef] [Green Version]
- Sakurai, M.; Murayama, Y. Information technologies and disaster management-benefits and issues. Prog. Disas. Sci. 2019, 2, E100012. [Google Scholar] [CrossRef]

| S.N. | Type of AI | Application | Reference |
|---|---|---|---|
| 1 | AI | Clinical oncology | [5] |
| 2 | Machine learning | Lymphoma | [6] |
| 3 | Machine learning | Myeloid leukemia | [10] |
| 4 | Deep learning | Cancer | [13] |
| 5 | AI | COVID-19 | [14] |
| 6 | Machine learning | Dengue | [15] |
| 7 | Machine learning | Cardiovascular diseases | [16] |
| 8 | Deep learning | Pulmonary infection | [19] |
| 9 | Deep learning | COVID-19 | [27] |
| 10 | Machine learning | Venous thromboembolism | [40] |
| 11 | Machine learning | Neovascular macular degeneration | [53] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wani, S.U.D.; Khan, N.A.; Thakur, G.; Gautam, S.P.; Ali, M.; Alam, P.; Alshehri, S.; Ghoneim, M.M.; Shakeel, F. Utilization of Artificial Intelligence in Disease Prevention: Diagnosis, Treatment, and Implications for the Healthcare Workforce. Healthcare 2022, 10, 608. https://doi.org/10.3390/healthcare10040608
Wani SUD, Khan NA, Thakur G, Gautam SP, Ali M, Alam P, Alshehri S, Ghoneim MM, Shakeel F. Utilization of Artificial Intelligence in Disease Prevention: Diagnosis, Treatment, and Implications for the Healthcare Workforce. Healthcare. 2022; 10(4):608. https://doi.org/10.3390/healthcare10040608
Chicago/Turabian StyleWani, Shahid Ud Din, Nisar Ahmad Khan, Gaurav Thakur, Surya Prakash Gautam, Mohammad Ali, Prawez Alam, Sultan Alshehri, Mohammed M. Ghoneim, and Faiyaz Shakeel. 2022. "Utilization of Artificial Intelligence in Disease Prevention: Diagnosis, Treatment, and Implications for the Healthcare Workforce" Healthcare 10, no. 4: 608. https://doi.org/10.3390/healthcare10040608
APA StyleWani, S. U. D., Khan, N. A., Thakur, G., Gautam, S. P., Ali, M., Alam, P., Alshehri, S., Ghoneim, M. M., & Shakeel, F. (2022). Utilization of Artificial Intelligence in Disease Prevention: Diagnosis, Treatment, and Implications for the Healthcare Workforce. Healthcare, 10(4), 608. https://doi.org/10.3390/healthcare10040608








