Association between Chronic Disease Self-Management, Health Status, and Quality of Life in Older Taiwanese Adults with Chronic Illnesses
Abstract
1. Introduction
2. Methods
2.1. Design
2.2. Setting and Sample
2.3. Data Collection
2.4. Measures
2.4.1. Demographics
2.4.2. Health Status
2.4.3. Chronic Disease Self-Management
2.4.4. Quality of Life (QoL)
2.5. Ethical Approval
2.6. Data Analysis
3. Results
3.1. Participants’ Characteristics
3.2. Health Status
3.3. Chronic Disease Self-Management and Quality of Life
3.4. Relationships among Chronic Disease Self-Management, Health Status, and Quality of Life
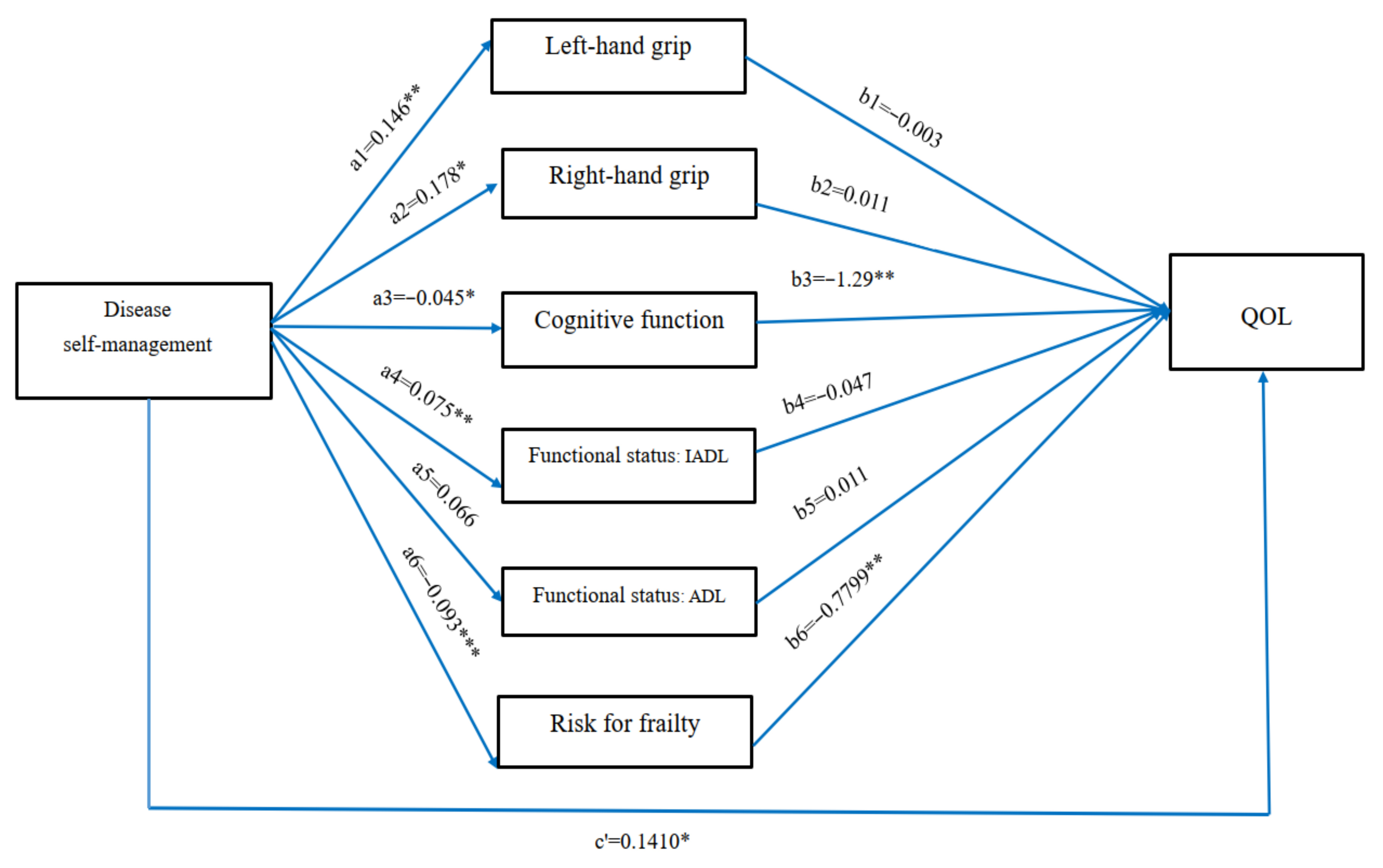
3.5. Mediating Effects of the Health Status on the Relationship between Chronic Disease Self-Management and Quality of Life
4. Discussion
4.1. Mediating Effect of Health Status on the Relationship between Chronic Illness Self-Management and Quality of Life
4.2. Relationships between Health Status, Chronic Disease Self-Management, and Quality of Life
5. Suggestions and Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Li, P.-S.; Hsieh, C.-J.; Miao, N.-F. A Study of Physical Activity, Frailty, and Health-Related Quality of Life Among Community-Dwelling Older Adults in Taiwan. J. Nurs. Res. 2020, 28, e124. [Google Scholar] [CrossRef] [PubMed]
- Maresova, P.; Javanmardi, E.; Barakovic, S.; Barakovic Husic, J.; Tomsone, S.; Krejcar, O.; Kuca, K. Consequences of chronic diseases and other limitations associated with old age—A scoping review. BMC Pub. Health 2019, 19, 1431. [Google Scholar] [CrossRef] [PubMed]
- Park, J.; Oh, H.; Park, W.; Kwon, S.; Ham, O.; Suh, Y.; Jeong, H.; Seo, W. Causal Relationships Between Modifiable Risk Factors of Cognitive Impairment, Cognitive Function, Self-Management, and Quality of Life in Patients with Rheumatic Diseases. Orthop. Nurs. 2018, 37, 305–315. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Park, E.; An, M. The Cognitive Impact of Chronic Diseases on Functional Capacity in Community-Dwelling Adults. J. Nurs. Res. 2019, 27, 1–8. [Google Scholar] [CrossRef]
- Chen, Y.; Funk, M.; Wen, J.; Tang, X.; He, G.; Liu, H. Effectiveness of a multidisciplinary disease management program on outcomes in patients with heart failure in China: A randomized controlled single center study. Heart Lung 2018, 47, 24–31. [Google Scholar] [CrossRef]
- Davis, J.C.; Bryan, S.; Li, L.C.; Best, J.R.; Hsu, C.L.; Gomez, C.; Vertes, K.A.; Liu-Ambrose, T. Mobility and cognition are associated with wellbeing and health related quality of life among older adults: A cross-sectional analysis of the Vancouver Falls Prevention Cohort. BMC Geriatr. 2015, 15, 75. [Google Scholar] [CrossRef]
- Gallucci, M.; Ongaro, F.; Meggiolaro, S.; Antuono, P.; Gustafson, D.R.; Forloni, G.L.; Albani, D.; Gajo, G.B.; Durante, E.; Caberlotto, L.; et al. Factors related to disability: Evidence from the “Treviso Longeva (TRELONG) Study”. Arch. Gerontol. Geriatr. 2011, 52, 309–316. [Google Scholar] [CrossRef]
- Lee, H.J.; Yun, J. Health-related quality of life in South Korean community-dwelling older adults with multimorbidity: A convergent parallel mixed-methods approach. Qual. Life Res. 2020, 29, 721–732. [Google Scholar] [CrossRef]
- Cramm, J.M.; Nieboer, A.P. Disease Management: The Need for a Focus on Broader Self-Management Abilities and Quality of Life. Popul. Health Manag. 2015, 18, 246–255. [Google Scholar] [CrossRef]
- Taylor, J.L.; Roberts, L.; Hladek, M.D.; Liu, M.; Nkimbeng, M.; Boyd, C.M.; Szanton, S.L. Achieving self-management goals among low income older adults with functional limitations. Geriatr. Nurs. 2019, 40, 424–430. [Google Scholar] [CrossRef]
- Cramm, J.M.; Hartgerink, J.M.; de Vreede, P.L.; Bakker, T.J.; Steyerberg, E.W.; Mackenbach, J.P.; Nieboer, A.P. The relationship between older adults’ self-management abilities, well-being and depression. Eur. J. Ageing 2012, 9, 353–360. [Google Scholar] [CrossRef]
- Stoller, M.A.; Stoller, E.P. Perceived income adequacy among elderly retirees. J. Appl. Gerontol. 2003, 22, 230–251. [Google Scholar] [CrossRef]
- Steverink, N.; Lindenberg, S. Do good self-managers have less physical and social resource deficit and more well-being in later life? Eur. J. Ageing 2008, 5, 181–189. [Google Scholar] [CrossRef]
- Grady, P.A.; Gough, L.L. Self-management: A comprehensive approach to management of chronic conditions. Am. J. Public Health 2014, 104, e25–e31. [Google Scholar] [CrossRef]
- Bourbeau, J. Disease-specific self-management programs in patients with advanced chronic obstructive pulmonary disease: A comprehensive and critical evaluation. Dis. Manag. Health Outcomes 2003, 11, 311–319. [Google Scholar] [CrossRef]
- Pungchompoo, W.; Parinyajittha, S.; Pungchompoo, S.; Kumtan, P. Effectiveness of a self-management retraining program improving the quality of life of people receiving continuous ambulatory peritoneal dialysis. Nurs. Health Sci. 2020, 22, 406–415. [Google Scholar] [CrossRef]
- Cramm, J.M.; Twisk, J.; Nieboer, A.P. Self-management abilities and frailty are important for healthy aging among community-dwelling older people—A cross-sectional study. BMC Geriatr. 2014, 14, 28. [Google Scholar] [CrossRef]
- Cramm, J.M.; Hartgerink, J.M.; Steyerberg, E.W.; Bakker, T.J.; Mackenbach, J.P.; Nieboer, A.P. Understanding older patients’ self-management abilities: Functional loss, self-management, and well-being. Qual. Life Res. 2013, 22, 85–92. [Google Scholar] [CrossRef]
- Cramm, J.M.; Nieboer, A.P. Self-management abilities, physical health and depressive symptoms among patients with cardiovascular diseases, chronic obstructive pulmonary disease, and diabetes. Patient Educ. Couns. 2012, 87, 411–415. [Google Scholar] [CrossRef]
- Cramm, J.M.; Nieboer, A.P. The importance of health behaviours and especially broader self-management abilities for older Turkish immigrants. Eur. J. Public Health 2018, 28, 1087–1092. [Google Scholar] [CrossRef]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Mahoney, F.; Barthel, D. Functional evaluation: The Barthel Index. Md. State Med. J. 1965, 14, 61–65. [Google Scholar]
- Chung, Y.F.; Sung, H.C.; Lin, L.P. Health Status and health resource utilization among older people in rural mining area. Tzu Chi Nurs. J. 2005, 4, 34–41. [Google Scholar] [CrossRef]
- Lawton, M.P.; Brody, E.M. Assessment of older people: Self-maintaining and instrumental activities of daily living. Gerontologist 1969, 9, 179–186. [Google Scholar] [CrossRef]
- Rikli, R.E.; Jones, C.J. Development and validation of a functional fitness test for community-residing older adults. J. Aging Phys. Act. 1999, 7, 129–161. [Google Scholar] [CrossRef]
- Chen, H.T.; Lin, C.H.; Yu, L.H. Normative physical fitness scores for community-dwelling older adults. J. Nurs. Res. 2009, 17, 30–41. [Google Scholar] [CrossRef]
- Satake, S.; Senda, K.; Hong, Y.J.; Miura, H.; Endo, H.; Sakurai, T.; Kondon, I.; Toba, K. Validity of the Kihon checklist for assessing frailty status. Geriatr. Gerontol. Int. 2016, 16, 709–715. [Google Scholar] [CrossRef]
- Sampaio, P.Y.S.; Sampaio, R.A.C.; Yamada, M.; Ogita, M.; Arai, H. Validation and translation of the Kihon checklist (frailty index) in to Brazilian Portuguese. Geriatr. Gerontol. Int. 2014, 14, 561–569. [Google Scholar] [CrossRef] [PubMed]
- Sampaio, P.Y.S.; Sampaio, R.A.C.; Yamada, M.; Arai, H. Systematic review of the Kihon checklist: Is it a reliable assessment of frailty? Geriatr. Gerontol. Int. 2016, 16, 893–902. [Google Scholar] [CrossRef] [PubMed]
- Galvin, J.E.; Roe, C.M.; Xiong, C.; Morris, J.C. Validity and reliability of the AD8 informant interview in dementia. Neurology 2006, 67, 1942–1948. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.C.; Anderson, R.M.; Chang, C.S.; Hagertly, B.M.; Loveland-Cherry, C.J. Development and testing of the diabetes self-management instrument: A confirmatory analysis. Res. Nurs. Health 2008, 31, 370–380. [Google Scholar] [CrossRef]
- Lorig, K.; Stewart, A.; Ritter, P.; Gonz’alez, V.; Laurent, D.; Lynch, J. Outcome Measures for Health Education and the Health Care Interventions; SAGE: Thousand Oaks, CA, USA, 1996; pp. 1–112. ISBN 978-0761900672. [Google Scholar]
- Yao, K.P. Developmemt and application of the WHOQOL-Taiwan version. J. Formos. Med. Assoc. 2002, 6, 193–200. [Google Scholar]
- Preacher, K.; Hayes, A. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav. Res. Methods 2008, 40, 879–891. [Google Scholar] [CrossRef]
- Park, M.O.; Oh, H.S.; Seo, W.S. Effects of a cognitive rehabilitation programme on cognitive function, self-management and quality of life in patients with chronic obstructive pulmonary disease. Int. J. Nurs. Pract. 2021, 27, e12932. [Google Scholar] [CrossRef]
- Shevil, E.; Finlayson, M. Pilot study of a cognitive intervention program for persons with multiple sclerosis. Health Educ. Res. 2010, 25, 41–53. [Google Scholar] [CrossRef]
- Cuevas, H.E.; Stuifbergen, A.K.; Ward, C. Participant Perspectives of Cognitive Rehabilitation for Type 2 Diabetes: Expectations and Impact. J. Aging Res. 2018, 2018, 6563457. [Google Scholar] [CrossRef]
- Newman, R.; Lyons, K.D.; Coster, W.J.; Wong, J.; Festa, K.; Ko, N.Y. Feasibility, acceptability and potential effectiveness of an occupation-focused cognitive self-management program for breast cancer survivors. Br. J. Occup. Ther. 2019, 82, 604–611. [Google Scholar] [CrossRef]
- Leveille, S.G.; Wagner, E.H.; Davis, C.; Grothaus, L.; Wallace, J.; LoGerfo, M.; Kent, D. Preventing disability and managing chronic illness in frail older adults: A randomized trial of a community-based partnership with primary care. J. Am. Geriatr. Soc. 1998, 46, 1191–1198. [Google Scholar] [CrossRef]
- Wu, L.M.; Austin, J.; Hamilton, J.G.; Valdimarsdottir, H.; Isola, L.; Rowley, S.; Warbet, R.; Winkel, G.; Redd, W.H.; Rini, C. Self-efficacy beliefs mediate the relationship between subjective cognitive functioning and physical and mental well-being after hematopoietic stem cell transplant. Psychooncology 2012, 21, 1175–1184. [Google Scholar] [CrossRef]
- Musekamp, G.; Schuler, M.; Seekatz, B.; Bengel, J.; Faller, H.; Meng, K. Does improvement in self-management skills predict improvement in quality of life and depressive symptoms? A prospective study in patients with heart failure up to one year after self-management education. BMC Cardiovasc. Disord. 2017, 17, 51. [Google Scholar] [CrossRef][Green Version]
- Ahmadzadeh, S.; Matlabi, H.; Allahverdipour, H.; Khodaei Ashan, S. The effectiveness of self-management program on quality of life among haemodialysis patients. Prog. Palliat. Care 2017, 25, 177–184. [Google Scholar] [CrossRef]
- Lorig, K.R.; Sobel, D.S.; Stewart, A.L.; Brown, B.W.J.; Bandura, A.; Ritter, P.; Gonzalez, V.M.; Laurent, D.D.; Holman, H.R. Evidence Suggesting That a Chronic Disease Self-Management Program Can Improve Health Status While Reducing Hospitalization: A Randomized Trial. Med. Care 1999, 37, 5–14. [Google Scholar] [CrossRef]
- Fortin, M.; Lapointe, L.; Hudon, C.; Vanasse, A.; Ntetu, A.L.; Maltais, D. Multomorbidity and quality of life in primary care: A systematic review. Health Qual. Life Outcomes 2004, 2, 51. [Google Scholar] [CrossRef]
- Hill, K.; Kellard, K.; Middleton, S.; Cox, L.; Pound, E. Understanding Resources in Later Life; Loughborough University Press: Loughborough, UK; Joseph Rowntree Foundation: London, UK, 2007; pp. 1–96. ISBN 978 1 85935 561 9. [Google Scholar]
- Feng, L.A.; Hean, S.; Worswick, L.; Wilkinson, C.; Fearnley, S.; Ersser, S. The impact of the economic recession on well-being and quality of life of older people. Health Soc. Care Community 2012, 20, 617–624. [Google Scholar] [CrossRef]
- Olivares, P.R.; Gusi, N.; Pireto, J.; Hernadez-Mocholi, M.A. Fitness and health-related quality of life dimension in community-dwelling middle aged and older adults. Health Qual. Life Outcomes 2011, 9, 117. [Google Scholar] [CrossRef]
- Wanderley, F.A.C.; Silva, G.; Marques, E.; Oliveria, J.; Mota, J.; Carvalho, J. Association between objectively assessed physical activity levels and fitness and self-reported health-related quality of life in community-dwelling older adults. Qual. Life Res. 2011, 20, 1371–1378. [Google Scholar] [CrossRef]
- Suominen, H. Physical activity and health: Musculoskeletal issue. Eur. J. Physiother. 2007, 9, 65–75. [Google Scholar] [CrossRef]
- Enkvist, A.; Ekstron, H.; Elmstahl, S. What factors affect life satisfication (LS) among the oldest-old? Arch. Gerontol. Geriatr. 2012, 54, 140–155. [Google Scholar] [CrossRef]
- Andersson, L.B.; Marcusson, J.; Wressle, E. Health-related quality of life and activities of daily living in 85-year-olds in Sweden. Health Soc. Care Community 2014, 22, 368–374. [Google Scholar] [CrossRef] [PubMed]
- Martín-Arribas, M.C.; Copa, P.D.A.; Paz, M.P.D.L. Quality of life, disability and handicap in patients with toxic oil syndrome. J. Adv. Nurs. 2005, 50, 595–604. [Google Scholar] [CrossRef] [PubMed]
- Giebel, C.M.; Sutcliffe, C.; Challis, D. Activities of daily living and quality of life across different stages of dementia: A UK study. Aging Ment. Health 2015, 19, 63–71. [Google Scholar] [CrossRef]
- Franzén, K.; Blomqvist, K.; Saveman, B.I. Impact of chronic heart failure on elderly persons’ daily life: A validation study. Eur. J. Cardiovasc. Nurs. 2006, 5, 137–145. [Google Scholar] [CrossRef]
- Black, S.A.; Rush, R.D. Cognitive and functional decline in adults aged 75 and older. J. Am. Geriatr. Soc. 2002, 50, 1978–1986. [Google Scholar] [CrossRef]
- Du, S.; Yuan, C. Evaluation of patient self-management outcomes in health care: A systematic review. Int. Nurs. Rev. 2010, 57, 159–167. [Google Scholar] [CrossRef]
- Redman, B.K. Patient Self-Management of Chronic Disease: The Health Care Provider’s Challenge; Jones and Bartlett: Mississauga, ON, Canada, 2004; pp. 1–209. ISBN 978-1404800182. [Google Scholar]
| Variable | Number of Subjects | (%) |
|---|---|---|
| Gender | ||
| Male | 42 | 37.5 |
| Female | 70 | 62.3 |
| Age Mean: 72.58 ± 7.49 Median: 72 Range: 60 to 99 | ||
| 60–65 years old | 18 | 16.1 |
| 66–70 years old | 32 | 28.6 |
| 71–75 years old | 21 | 18.8 |
| 76–80 years old | 25 | 22.3 |
| Eighty-one years old and over | 16 | 14.3 |
| Marital status | ||
| Single/separated/divorced/widowed/other | 23 | 20.5 |
| Married | 89 | 78.9 |
| Living status (whether living with others) | ||
| No | 18 | 16.1 |
| Yes | 94 | 83.9 |
| People living together (number of people) Mean: 2.63 ± 1.93 Median: 2 Range: 0 to 10 | ||
| Living alone | 18 | 16.1 |
| Two people | 56 | 50.0 |
| Three people or more | 38 | 33.9 |
| Religious belief | ||
| None | 20 | 17.9 |
| Buddhism | 53 | 47.3 |
| Taoism/folk beliefs | 23 | 20.5 |
| Christianity/Catholicism | 16 | 14.3 |
| Level of education | ||
| Literate/illiterate | 9 | 8.0 |
| Primary school | 25 | 22.3 |
| Middle school/junior high school | 20 | 17.9 |
| Senior high school/vocational school | 22 | 19.6 |
| Junior college | 10 | 8.9 |
| College (inclusive) and above | 26 | 23.2 |
| Employed | ||
| No | 104 | 92.9 |
| Yes | 8 | 7.1 |
| Main source of income | ||
| Children/spouse/parents/others | 46 | 41.1 |
| Pension | 56 | 50.0 |
| Government grants | 10 | 8.9 |
| Adequacy of living allowance | ||
| Abundant and in surplus | 30 | 26.8 |
| Generally enough | 71 | 63.4 |
| Not enough | 11 | 9.8 |
| Number of diseases Mean: 1.60 ± 0.94 Median: 1 Range: 1 to 6 | ||
| One | 66 | 58.9 |
| Two | 31 | 27.7 |
| Three and more | 15 | 13.4 |
| CCI (after age adjustment) Mean: 2.39 ± 2.37 Median: 3 Range: 0 to 9 | ||
| 0 | 50 | 44.6 |
| 2 | 2 | 1.8 |
| 3 | 14 | 12.5 |
| 4 | 24 | 21.4 |
| 5 | 14 | 12.5 |
| Six and more | 8 | 7.2 |
| Scale/Subscale (Number of Items) | Risk as Showing Score | Number (%) | Mean (SD) |
|---|---|---|---|
| AD8 (8) | 1.59 ± 2.11 | ||
| 0 | 48 (42.9) | ||
| 1 | 24 (21.4) | ||
| ≥2 | (Early symptoms of dementia) | 40 (35.7) | |
| Kihon Checklist (25) | |||
| Physical strength (5) | ≥3 (low physical strength) | 24 (21.4) | 1.38 (±1.39) |
| Nutrition (2) | 2 (low nutritional status) | 1 (0.9) | 0.26 (±0.46) |
| Oral function (3) | ≥2 (low oral function) | 26 (23.2) | 1.0 (±0.92) |
| Socialization (1) | Negative answer on No. 16 (house-bound) | 16 (14.3) | 0.14 (±0.35) |
| Memory (3) | ≥1 (low cognitive function) | 58 (51.8) | 0.75 (±0.84) |
| Mood (5) | ≥2 (depression risk) | 30 (26.8) | 1.03 (±1.38) |
| Lifestyle (20) | ≥10 (frailty) | 10 (8.9) | 4.42 (±3.48) |
| Total KCL score (25) | ≥7 (general frailty or elevated risk of needing LTCI service) | 39 (34.8) | 5.46 (±4.32) |
| Scale (Possible Range of Scores) | Mean | SD | Minimum | Maximum | Score Index |
|---|---|---|---|---|---|
| Disease self-management a (0 to 117) | 65.99 | 16.78 | 23 | 95 | 56.49 |
| Partnership (0 to 24) | 18.31 | 5.75 | 5 | 24 | 75.56 |
| Performance of self-care activities (0 to 66) | 31.40 | 8.57 | 6 | 54 | 47.58 |
| Problem solving (0 to 12) | 8.2 | 3.29 | 1 | 12 | 68.38 |
| Emotion handling (0 to 15) | 8.9 | 3.34 | 2 | 15 | 74.53 |
| Overall QoL b | 57.82 | 8.32 | 23.56 | 78.43 | 72.27 |
| Physical domain (4 to 20) | 14.59 | 2.47 | 7.43 | 20 | 72.72 |
| Psychological domain (4 to 20) | 14.19 | 2.49 | 6 | 20 | 70.95 |
| Social relationships domain (4 to 20) | 14.28 | 2.29 | 9 | 20 | 71.44 |
| Environment domain (4 to 20) | 14.92 | 2.17 | 7.56 | 20 | 74.62 |
| Variable | (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | (9) | (10) | (11) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| (1) Living expenses | - | ||||||||||
| (2) Comorbidity | 0.05 | - | |||||||||
| (3) ADL | −0.15 | −0.10 | - | ||||||||
| (4) IADL | −0.08 | 0.07 | 0.71 ** | - | |||||||
| (5) Risk for frailty | 0.28 ** | 0.26 ** | −0.57 ** | −0.65 ** | - | ||||||
| (6) Very early dementia | 0.20 ** | 0.23 ** | −0.34 ** | −0.38 ** | 0.49 ** | - | |||||
| (7) Left handgrip | −0.19 * | 0.03 | 0.16 | 0.25 ** | −0.40 ** | −0.25 ** | - | ||||
| (8) Right handgrip | −0.11 | 0.06 | 0.17 | 0.32 ** | −0.40 ** | −0.24 * | 0.87 ** | - | |||
| (9) Lower extremities muscle strength | −0.02 | −0.19 | 0.15 | 0.29 ** | −0.21 | −0.24 * | 0.25 * | 0.26 * | - | ||
| (10) Chronic self-management | −0.00 | −0.08 | 0.21 * | 0.33 ** | −0.35 ** | −0.33 ** | 0.26 ** | 0.27 ** | 0.10 | - | |
| (11) Quality of life | −0.32 ** | −0.20 * | 0.34 ** | 0.37 ** | −0.56 ** | −0.50 ** | 0.26 ** | 0.26 ** | 0.44 ** | 0.18 | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Han, T.-C.; Lin, H.-S.; Chen, C.-M. Association between Chronic Disease Self-Management, Health Status, and Quality of Life in Older Taiwanese Adults with Chronic Illnesses. Healthcare 2022, 10, 609. https://doi.org/10.3390/healthcare10040609
Han T-C, Lin H-S, Chen C-M. Association between Chronic Disease Self-Management, Health Status, and Quality of Life in Older Taiwanese Adults with Chronic Illnesses. Healthcare. 2022; 10(4):609. https://doi.org/10.3390/healthcare10040609
Chicago/Turabian StyleHan, Tung-Chen, Huey-Shyan Lin, and Ching-Min Chen. 2022. "Association between Chronic Disease Self-Management, Health Status, and Quality of Life in Older Taiwanese Adults with Chronic Illnesses" Healthcare 10, no. 4: 609. https://doi.org/10.3390/healthcare10040609
APA StyleHan, T.-C., Lin, H.-S., & Chen, C.-M. (2022). Association between Chronic Disease Self-Management, Health Status, and Quality of Life in Older Taiwanese Adults with Chronic Illnesses. Healthcare, 10(4), 609. https://doi.org/10.3390/healthcare10040609






