Effectiveness of Pulmonary Rehabilitation among COVID-19 Patients: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Protocol and Registration
2.2. Research Question
- “PICOS”
- P (Population) = COVID-19 patients
- I (Intervention) = respiratory rehabilitation
- C (Comparison) = standard treatment
- O (Outcome) = physical function and quality of life
- S (Study design) = randomized controlled trial, and controlled clinical studies.
2.3. Types of Outcome Measures
2.3.1. Primary Outcomes
- Physical function.
- Quality of life.
2.3.2. Secondary Outcomes
- 3.
- Dyspnoea.
- 4.
- Respiratory function.
- 5.
- Physical activity intensity level.
- 6.
- Anxiety.
- 7.
- Depression.
- 8.
- Peripheral muscle performance of lower limbs.
2.4. Data Sources
2.5. Eligibility Criteria
2.5.1. Inclusion Criteria
- 9.
- Unvaccinated COVID-19 patients with no age limit.
- 10.
- Publications with no language limitation and with full text available.
- 11.
- Pulmonary rehabilitation.
- 12.
- Randomized controlled trials, and controlled clinical studies.
2.5.2. Exclusion Criteria
2.6. Study Selection
2.7. Data Extraction
2.8. Assessment of Risk of Bias
2.9. Analysis
2.9.1. Measurement of Treatment Effect
2.9.2. Sensitivity Analysis
2.9.3. Summary of Findings Table
- Key findings that were summarized (participants, comparative and baseline data, and results) [22].
- Statistical results that have been condensed.
- A summary of the evidence’s quality, the degree of the effect, and the source of information utilized in the assumed risk.
3. Results
3.1. Included Studies
3.2. Participants
3.3. Intervention
3.4. Comparison
3.5. Excluded Studies
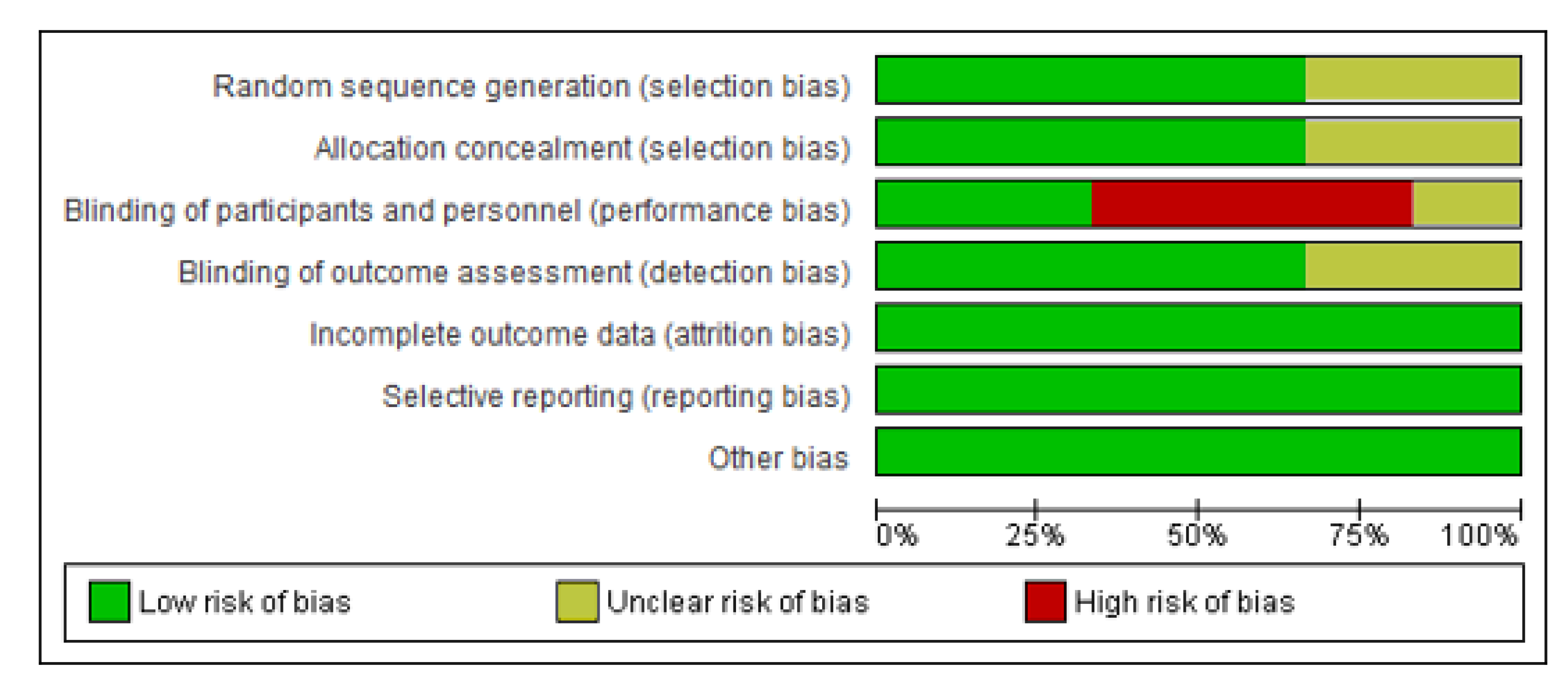
3.6. Risk of Bias in Included Studies
3.6.1. Random Sequence and Allocation Concealment
3.6.2. Blinding of Participants, Personnel, and Outcome Assessment
3.6.3. Incomplete Outcome Data
3.6.4. Selective Reporting
3.6.5. Other Potential Sources of Bias
3.7. Outcomes
3.7.1. Primary Outcomes
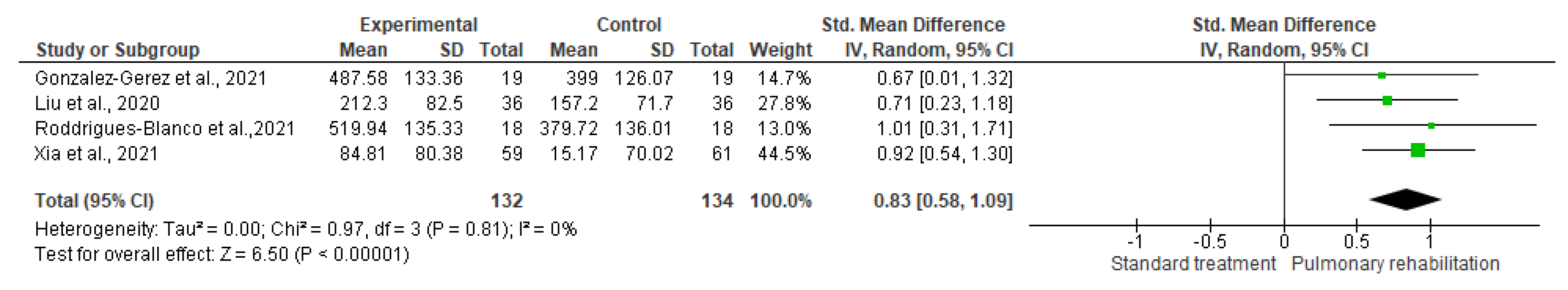
Physical Function
Quality of Life
3.7.2. Secondary Outcomes
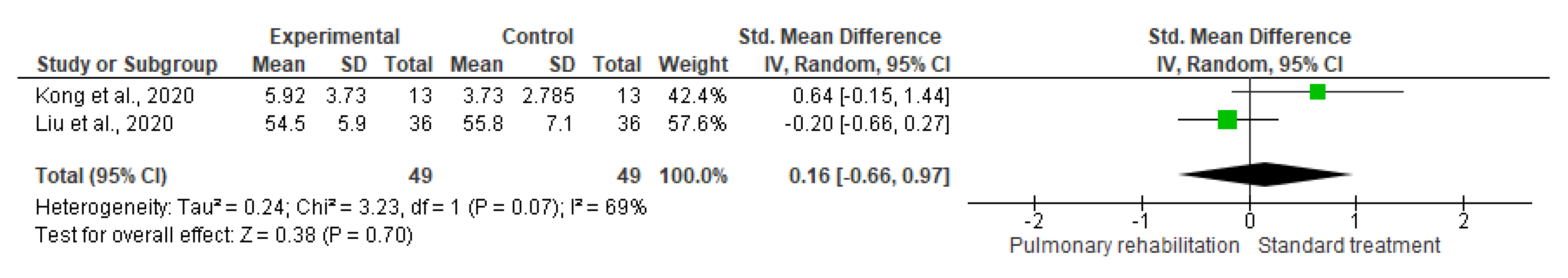
Depression
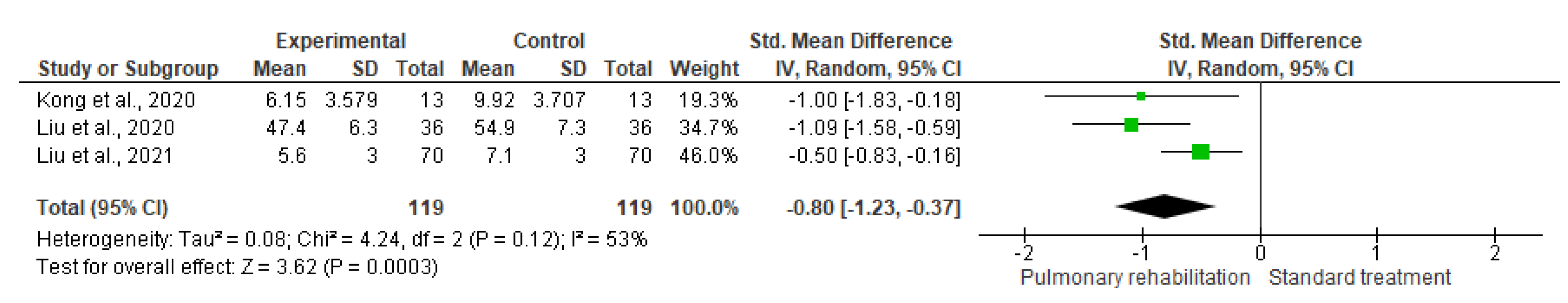
Anxiety
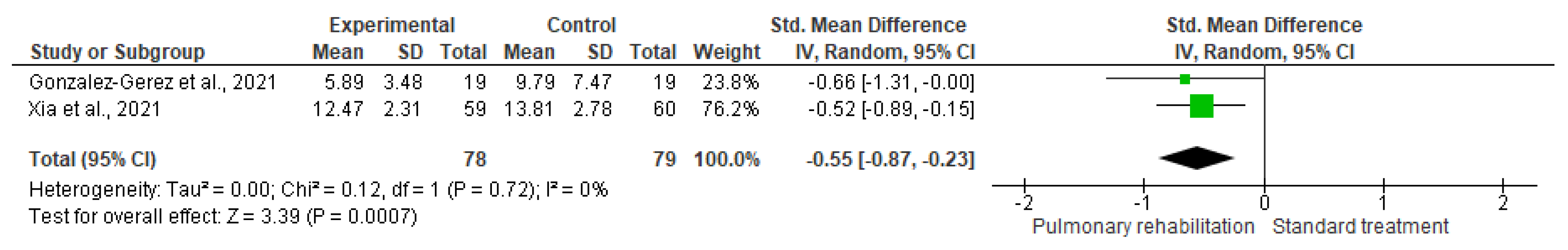
Dyspnoea
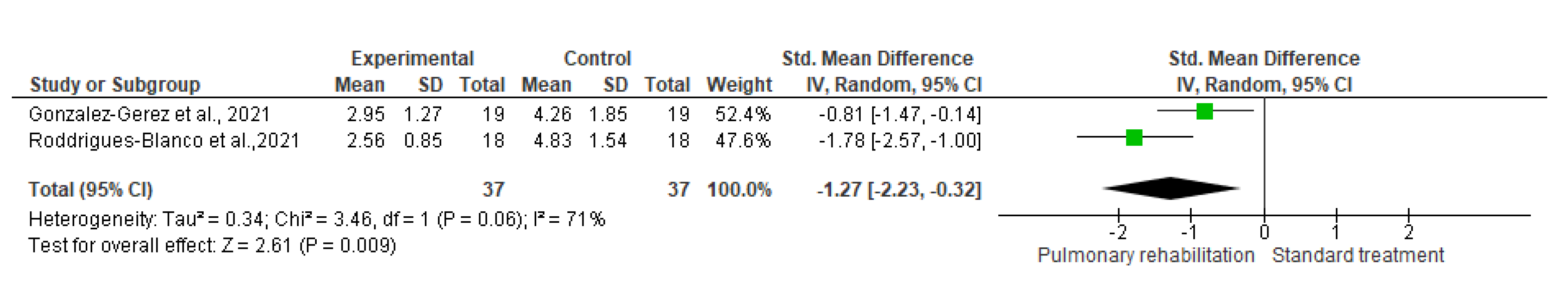
Physical Activity Intensity Level
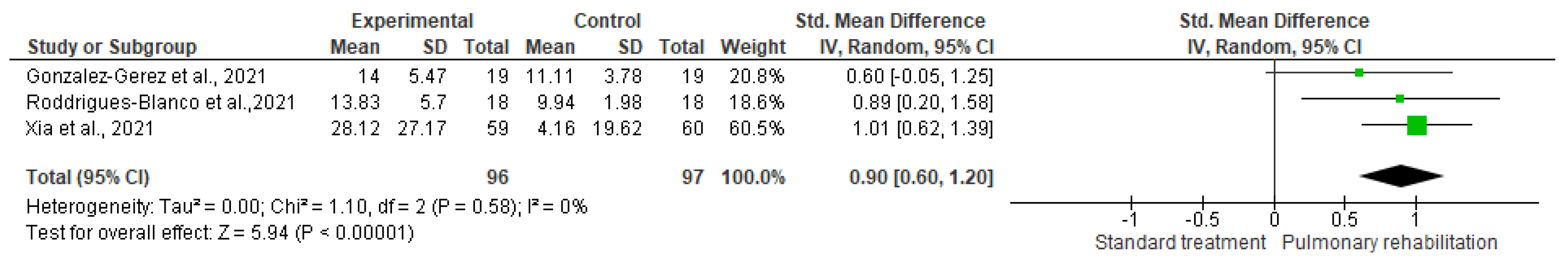
Peripheral Muscle Performance of Lower Limbs
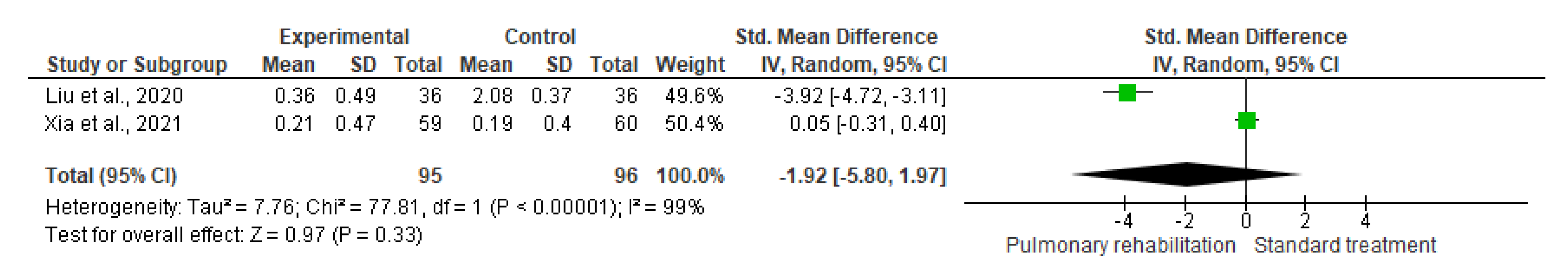
Pulmonary Function
Sleep Quality
Social Support
4. Discussion
4.1. Summary of Main Results
4.2. Overall Completeness and Applicability of Evidence
4.3. Quality of the Evidence
4.4. Potential Biases in the Review Process
4.5. Limitation of the Study
4.6. Agreements and Disagreements with Other Studies or Reviews
5. Conclusions
5.1. Implications for Practice
5.2. Implications for Research
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bourin, M. Posttraumatic stress disorder concerning the end of the covid-19 lockdown: A mini review. Arch. Depress. Anxiety 2020, 6, 6–9. [Google Scholar]
- Fathi, M.; Vakili, K.; Sayehmiri, F.; Mohamadkhani, A.; Hajiesmaeili, M.; Rezaei-Tavirani, M.; Eilami, O. The prognostic value of comorbidity for the severity of COVID-19: A systematic review and meta-analysis study. PLoS ONE 2021, 16, e0246190. [Google Scholar] [CrossRef] [PubMed]
- Cascella, M.; Rajnik, M.; Aleem, A.; Dulebohn, S.C.; Di Napoli, R. Features, Evaluation, and Treatment of Coronavirus (COVID-19). In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. Available online: https://www.ncbi.nlm.nih.gov/books/NBK554776/ (accessed on 13 October 2022).
- Peel, M.M. Epidemic poliomyelitis, post-poliomyelitis sequelae and the eradication program. Microbiol. Aust. 2020, 41, 196–200. [Google Scholar] [CrossRef]
- Wu, Z.; McGoogan, J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72,314 cases from the Chinese Center for Disease Control and Prevention. JAMA 2020, 323, 1239–1242. [Google Scholar] [CrossRef] [PubMed]
- AL-Mhanna, S.B.; Ghazali, W.S.W.; Mohamed, M.; Sheikh, A.M.; Tabnjh, A.K.; Afolabi, H.; Mutalub, Y.B.; Adeoye, A.O.; Nur, M.M.; Aldhahi, M.I. Evaluation of physical activity among undergraduate students in Mogadishu Universities in the aftermath of COVID-19 restrictions. PeerJ 2022, 10, e14131. [Google Scholar] [CrossRef]
- Huang, C.; Huang, L.; Wang, Y.; Li, X.; Ren, L.; Gu, X.; Kang, L.; Guo, L.; Liu, M.; Zhou, X. 6-month consequences of COVID-19 in patients discharged from hospital: A cohort study. Lancet 2021, 397, 220–232. [Google Scholar] [CrossRef]
- Zhu, S.; Gao, Q.; Yang, L.; Yang, Y.; Xia, W.; Cai, X.; Hui, Y.; Zhu, D.; Zhang, Y.; Zhang, G. Prevalence and risk factors of disability and anxiety in a retrospective cohort of 432 survivors of Coronavirus Disease-2019 (COVID-19) from China. PLoS ONE 2020, 15, e0243883. [Google Scholar] [CrossRef]
- Hao, F.; Tan, W.; Jiang, L.; Zhang, L.; Zhao, X.; Zou, Y.; Hu, Y.; Luo, X.; Jiang, X.; McIntyre, R.S. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain Behav. Immun. 2020, 87, 100–106. [Google Scholar] [CrossRef]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; McIntyre, R.S.; Choo, F.N.; Tran, B.; Ho, R.; Sharma, V.K. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav. Immun. 2020, 87, 40–48. [Google Scholar] [CrossRef]
- Altena, E.; Baglioni, C.; Espie, C.A.; Ellis, J.; Gavriloff, D.; Holzinger, B.; Schlarb, A.; Frase, L.; Jernelöv, S.; Riemann, D. Dealing with sleep problems during home confinement due to the COVID-19 outbreak: Practical recommendations from a task force of the European CBT-I Academy. J. Sleep Res. 2020, 29, e13052. [Google Scholar] [CrossRef]
- de Sire, A.; Moggio, L.; Marotta, N.; Agostini, F.; Tasselli, A.; Drago Ferrante, V.; Curci, C.; Calafiore, D.; Ferraro, F.; Bernetti, A. Impact of Rehabilitation on Fatigue in Post-COVID-19 Patients: A Systematic Review and Meta-Analysis. Appl. Sci. 2022, 12, 8593. [Google Scholar] [CrossRef]
- McCarthy, H.; Potts, H.W.; Fisher, A. Physical activity behavior before, during, and after COVID-19 restrictions: Longitudinal smartphone-tracking study of adults in the United Kingdom. J. Med. Internet Res. 2021, 23, e23701. [Google Scholar] [CrossRef]
- Mammi, P.; Ranza, E.; Rampello, A.; Ravanetti, D.; Cavaldonati, A.; Moretti, S.; Gobbi, E.; Rodà, F.; Brianti, R. Post COVID-19 ongoing symptoms and health related quality of life: Does rehabilitation matter? Preliminary evidence. Am. J. Phys. Med. Rehabil. 2022. [Google Scholar] [CrossRef]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef]
- Visco, V.; Vitale, C.; Rispoli, A.; Izzo, C.; Virtuoso, N.; Ferruzzi, G.J.; Santopietro, M.; Melfi, A.; Rusciano, M.R.; Maglio, A. Post-COVID-19 Syndrome: Involvement and Interactions between respiratory, cardiovascular and nervous systems. J. Clin. Med. 2022, 11, 524. [Google Scholar] [CrossRef]
- Liu, K.; Zhang, W.; Yang, Y.; Zhang, J.; Li, Y.; Chen, Y. Respiratory rehabilitation in elderly patients with COVID-19: A randomized controlled study. Complement. Ther. Clin. Pract. 2020, 39, 101166. [Google Scholar] [CrossRef]
- Hermann, M.; Pekacka-Egli, A.-M.; Witassek, F.; Baumgaertner, R.; Schoendorf, S.; Spielmanns, M. Feasibility and efficacy of cardiopulmonary rehabilitation following COVID-19. Am. J. Phys. Med. Rehabil. 2020, 99, 865–869. [Google Scholar] [CrossRef]
- Andrenelli, E.; Negrini, F.; De Sire, A.; Patrini, M.; Lazzarini, S.G.; Ceravolo, M.G. Rehabilitation and COVID-19: A rapid living systematic review 2020 by Cochrane Rehabilitation Field. Update as of September 30th, 2020. Eur. J. Phys. Rehabil. Med. 2020, 56, 846–852. [Google Scholar] [CrossRef]
- Higgins, J. Cochrane Handbook for Systematic Reviews of Interventions; The Cochrane Collaboration; Wiley Blackwell: Hoboken, NJ, USA, 2019; Available online: www.cochrane-handbook.org (accessed on 10 September 2022).
- GRADEpro. Computer Program; McMaster University: Hamilton, ON, Canada, 2015; Available online: https://www.gradepro.org/ (accessed on 10 September 2022).
- Schünemann, H.J.; Oxman, A.D.; Higgins, J.P.; Vist, G.E.; Glasziou, P.; Guyatt, G.H. Presenting Results and ‘Summary of Findings’ Tables. In Cochrane Handbook for Systematic Reviews of Interventions; Cochrane Book Series; Wiley Online Library: Hoboken, NJ, USA, 2008; pp. 335–357. [Google Scholar]
- Gonzalez-Gerez, J.J.; Saavedra-Hernandez, M.; Anarte-Lazo, E.; Bernal-Utrera, C.; Perez-Ale, M.; Rodriguez-Blanco, C. Short-term effects of a respiratory telerehabilitation program in confined COVID-19 patients in the acute phase: A pilot study. Int. J. Environ. Res. Public Health 2021, 18, 7511. [Google Scholar] [CrossRef]
- Rodriguez-Blanco, C.; Gonzalez-Gerez, J.J.; Bernal-Utrera, C.; Anarte-Lazo, E.; Perez-Ale, M.; Saavedra-Hernandez, M.J.M. Short-term effects of a conditioning telerehabilitation program in confined patients affected by COVID-19 in the acute phase. A pilot randomized controlled trial. Medicina 2021, 57, 684. [Google Scholar] [CrossRef]
- Xia, W.; Zhan, C.; Liu, S.; Yin, Z.; Wang, J.; Chong, Y.; Zheng, C.; Fang, X.; Cheng, W.; Reinhardt, J.D. A telerehabilitation programme in post-discharge COVID-19 patients (TERECO): A randomised controlled trial. Thorax 2021, 77, 697–706. [Google Scholar]
- Kong, X.; Kong, F.; Zheng, K.; Tang, M.; Chen, Y.; Zhou, J.; Li, Y.; Diao, L.; Wu, S.; Jiao, P. Effect of psychological–behavioral intervention on the depression and anxiety of COVID-19 patients. Front. Psychiatry 2020, 11, 586355. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Yang, Y.-Q.; Liu, Y.; Pei, S.-L.; Yang, H.-H.; Wu, J.-J.; Luo, C.-K. Effects of group psychological intervention combined with pulmonary rehabilitation exercises on anxiety and sleep disorders in patients with mild coronavirus disease 2019 (COVID-19) infections in a Fangcang hospital. Psychol. Health Med. 2022, 27, 333–342. [Google Scholar] [CrossRef] [PubMed]
- Mohamed, A.A.; Alawna, M. The effect of aerobic exercise on immune biomarkers and symptoms severity and progression in patients with COVID-19: A randomized control trial. J. Bodyw. Mov. Ther. 2021, 28, 425–432. [Google Scholar] [CrossRef]
- Fila, E.; Rocco, I.; Rocco, G.; Zuccon, U.; Ruberti, E. Recommendations for the respiratory rehabilitation of hospitalized and discharged COVID-19 patients: A sistematic review. G. Ital. Med. Lav. Erg. 2021, 43, 56–65. [Google Scholar]
- Goodwin, V.A.; Allan, L.; Bethel, A.; Cowley, A.; Cross, J.L.; Day, J.; Drummond, A.; Hall, A.J.; Howard, M.; Morley, N. Rehabilitation to enable recovery from COVID-19: A rapid systematic review. Physiotherapy 2021, 111, 4–22. [Google Scholar] [CrossRef]
- Bernal-Utrera, C.; Anarte-Lazo, E.; Gonzalez-Gerez, J.J.; De-La-Barrera-Aranda, E.; Saavedra-Hernandez, M.; Rodriguez-Blanco, C. Could physical therapy interventions be adopted in the management of critically ill patients with COVID-19? A scoping review. Int. J. Environ. Res. Public Health 2021, 18, 1627. [Google Scholar] [CrossRef]





| Reference | Journal | Population | Year of Publication | Sample Size (F) | Participants/Age | Period of Recruitment | Gender | Method (Exercise Name, Duration, Intensity, Sets, Reps). | Status of the Patient at Intervention | Duration of Intervention | Outcome Measures | PRO Measure Instrument |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. [17] | Complementary Therapies in Clinical Practice | China | 2020 | 72 EX = 36 CO = 36 | Elderly patients with COVID-19. 69.4 ± 8.0 | 1 January 2020 to 6 February 2020 | Male | Participant subjected to pulmonary rehabilitation of two S/W for ten M. The intervention includes respiratory muscle EX, cough EX, diaphragmatic EX: stretching EX at 60% of the individual’s maximal expiratory mouth pressure. While the CO received only standard treatment | Definite diagnosis of COVID-19 | Six W | 1. PFT 2. functional tests 3. QOL 4. Activities of daily living 5. Mental status tests. | 1. Spirometer 2. 6MWT 3. SF-36 4. FIM scores 5. SAS anxiety and SDS depression scores |
| 2. [26] | Frontiers in Psychiatry | China | 2020 | 16 EX = 13 CO = 13 | COVID-19 patients 49.98 ± 13.73 | 23 February 2020 to 13 March 2020 | Male and female | Patients undergo breathing exercises for 20 M every D, to stimulate nasal and diaphragmatic breathing, increase expiratory duration, reduce respiratory flow, and regulate breathing rhythm + psychological support The CO received only Standard treatment | Definite diagnosis of COVID-19 | 10 D | 1. Depression and anxiety, 2. Social support | 1. HADS-A and HADS-D 2. PSSS |
| 3. [23] | International Journal of Environmental Research and Public Health | Spain | 2021 | 38 Ex = 19 Co = 19 | Mild to moderate symptomatology in the acute stage COVID-19 patients 40.79 ± 9.84 | 19 October 2020 | Male and female | Respiratory telerehabilitation programme, the breathing EX was once /D for seven D at home; based on the assessment of the RPE, patients underwent four RPE on a scale of seven-ten for ten M). The CO received only Standard treatment | Confined COVID-19 Patients in the Acute Phase | One W | 1. Physical function 2. Peripheral muscle performance of lower limbs 3. Multidimensional nature of dyspnoea 4. Physical activity intensity level | 1. 6MWT 2. Thirty-Second STST 3. Multidimensional Dyspnoea-12 4. RPE |
| 4. [27] | Psychology, Health & Medicine | China | 2021 | 140 Ex = 70 Co = 70 | patients with mild COVID-19 infections All age group | In March 2020 | Male and female | Pulmonary rehabilitation included Five-tone breathing EX, five-step breathing EX and two-section motion E, for seven D. The CO received only Standard treatment | Definite diagnosis of COVID-19 | One W | 1. Anxiety state 2. Sleep quality | 1. SAI 2. PQSI |
| 5. [24] | Medicine | Spain | 2021 | 36 EX = 18, CO = 18 | COVID-19 patients with mild to moderate symptomatology 39.39 ± 1174 | 23 October 2020 | Telerehabilitation programme included ten EX based on non-specific toning EX of resistance and strength one/D for seven D using the RPE scale to determine EX intensity. The CO received only Standard treatment | Confined COVID-19 Patients in the Acute Phase | One W | 1. Physical function 2. Peripheral muscle performance of lower limbs. 3. Physical activity intensity level | 1. 6MWT 2. 30STST 3. RPE | |
| 6. [25] | Rehabilitation | China | 2021 | 120 EX = 59 CO = 61 | Hospitalized COVID-19 survivors with remaining dyspnoea 49.17 ± 10.75 | 28 May 2020 | Male and female | Participants were subjected to six W of unsupervised home EX programme for three-four S/W. Ex includes: -breathing control and thoracic expansion. The CO received only Standard treatment | In post-discharge COCID-19 patients | six W | 1. Physical function, 2. Peripheral muscle performance of lower limp 3. Pulmonary function, 4. QOL 5. Dyspnoea | 1. 6MWT 2. squat time in seconds 3. Spirometer 4. HRQOL12 5. mMRC dyspnoea |
| Outcome | Certainty Assessment | № of Patients | Effect | Certainty | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| № of Studies | Study Design | Risk of Bias | Inconsistency | Indirectness | Imprecision | Other Considerations | Respiratory Rehabilitation | Standard Treatment | Absolute (95% CI) | ||
| Physical function | 4 | RCT | serious b | serious c | not serious | serious a | none | 132 | 134 | SMD 0.83. higher (0.58 higher to 1.09 higher) | ⨁◯◯◯ Very low |
| Physical-health-related quality of life. | 2 | RCT | serious b | serious d | not serious | serious a | none | 95 | 96 | SMD 0.02 higher (0.57 lower to 0.62 higher) | ⨁◯◯◯ Very low |
| Mental-health-related quality of life | 2 | RCT | serious b | serious c | not serious | serious a | none | 95 | 96 | SMD 0.06 lower (0.51 lower to 0.40 higher) | ⨁◯◯◯ Very low |
| Depression | 2 | RCT | serious f | serious d | not serious | serious a | none | 49 | 49 | SMD 0.16 SD higher (0.66 lower to 0.97 higher) | ⨁◯◯◯ Very low |
| Anxiety | 3 | RCT | serious b | not serious | not serious | serious a | none | 119 | 119 | SMD 0.8 lower (1.23 lower to 0.37 lower) | ⨁⨁◯◯ Low |
| Dyspnoea | 2 | RCT | not serious | not serious | not serious | serious a | none | 78 | 79 | SMD 0.55 lower (0.87 lower to 0.23 lower) | ⨁⨁⨁◯ Moderate |
| Physical activity intensity level | 2 | RCT | not serious | serious d | not serious | serious a | none | 37 | 37 | SMD 1.27 lower (2.23 lower to 0.32 lower) | ⨁⨁◯◯ Low |
| Peripheral muscle performance of lower limp | 3 | RCT | not serious | not serious | not serious | serious a | none | 96 | 97 | SMD 0.9 higher (0.6 higher to 1.2 higher) | ⨁⨁⨁◯ Moderate |
| Pulmonary function | 2 | RCT | serious b | very serious e | not serious | serious a | none | 95 | 96 | SMD 1.92 lower (5.8 lower to 1.97 higher) | ⨁◯◯◯ Very low |
| Sleep quality | 1 | RCT | serious g | not serious | not serious | serious a | none | 70 | 70 | MD 0.5 lower (0.83 lower to 0.16 lower) | ⨁⨁◯◯ Low |
| Social support | 2 | RCT | serious b | serious e | not serious | serious a | none | 49 | 49 | SMD 0.79 higher (0.94 lower to 2.53 higher) | ⨁◯◯◯ Very low |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
AL-Mhanna, S.B.; Mohamed, M.; Noor, N.M.; Afolabi, H.A.; Irekeola, A.A.; Bello, K.E.; Aldhahi, M.I.; Wan Ghazali, W.S. Effectiveness of Pulmonary Rehabilitation among COVID-19 Patients: A Systematic Review and Meta-Analysis. Healthcare 2022, 10, 2130. https://doi.org/10.3390/healthcare10112130
AL-Mhanna SB, Mohamed M, Noor NM, Afolabi HA, Irekeola AA, Bello KE, Aldhahi MI, Wan Ghazali WS. Effectiveness of Pulmonary Rehabilitation among COVID-19 Patients: A Systematic Review and Meta-Analysis. Healthcare. 2022; 10(11):2130. https://doi.org/10.3390/healthcare10112130
Chicago/Turabian StyleAL-Mhanna, Sameer Badri, Mahaneem Mohamed, Norhayati Mohd Noor, Hafeez Abiola Afolabi, Ahmad Adebayo Irekeola, Kizito Eneye Bello, Monira I. Aldhahi, and Wan Syaheedah Wan Ghazali. 2022. "Effectiveness of Pulmonary Rehabilitation among COVID-19 Patients: A Systematic Review and Meta-Analysis" Healthcare 10, no. 11: 2130. https://doi.org/10.3390/healthcare10112130
APA StyleAL-Mhanna, S. B., Mohamed, M., Noor, N. M., Afolabi, H. A., Irekeola, A. A., Bello, K. E., Aldhahi, M. I., & Wan Ghazali, W. S. (2022). Effectiveness of Pulmonary Rehabilitation among COVID-19 Patients: A Systematic Review and Meta-Analysis. Healthcare, 10(11), 2130. https://doi.org/10.3390/healthcare10112130