Exploring the Feasibility of an Online Diabetes Wellness Programme among Periodontitis Patients with Type II Diabetes Mellitus during the COVID-19 Pandemic
Abstract
1. Introduction
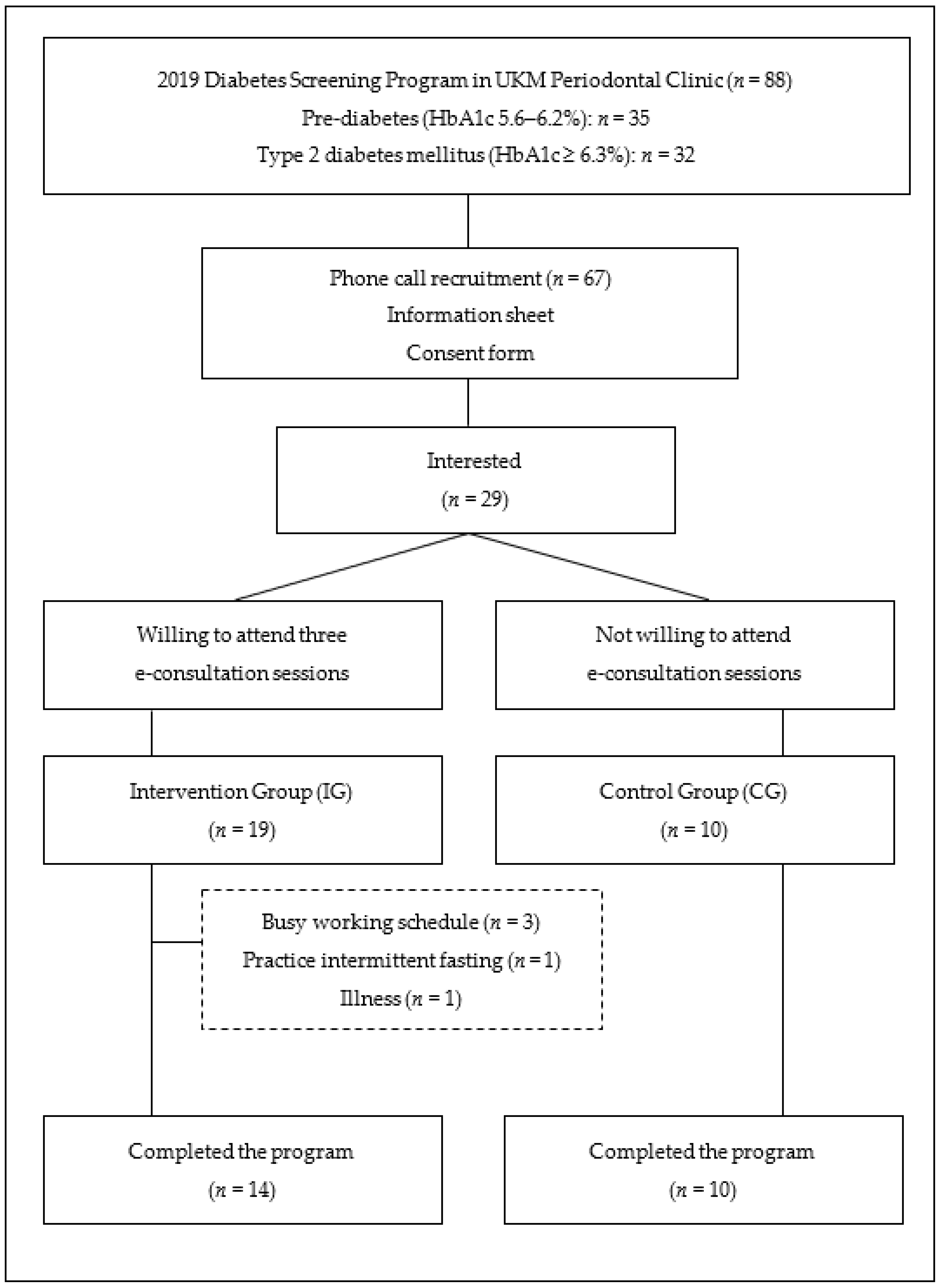
2. Materials and Methods
2.1. Study Design
2.2. Online Diabetes Wellness Programme
2.3. Data Collection
2.4. Statistical Analysis
3. Results
3.1. Changes in Diabetes-Related Knowledge and Lifestyle Practices
3.2. Qualitative Feedback on the Online Education Programme
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bui, F.Q.; Almeida-da-Silva, C.L.C.; Huynh, B.; Trinh, A.; Liu, J.; Woodward, J.; Asadi, H.; Ojcius, D.M. Association between periodontal pathogens and systemic disease. Biomed. J. 2019, 42, 27–35. [Google Scholar] [CrossRef] [PubMed]
- Tonetti, M.S.; Greenwell, H.; Kornman, K.S. Staging and grading of periodontitis: Framework and proposal of a new classification and case definition. J. Periodontol. 2018, 89, S159–S172. [Google Scholar] [CrossRef] [PubMed]
- Polak, D.; Shapira, L. An update on the evidence for pathogenic mechanisms that may link periodontitis and diabetes. J. Clin. Periodontol. 2018, 45, 150–166. [Google Scholar] [CrossRef] [PubMed]
- Preshaw, P.M.; Alba, A.L.; Herrera, D.; Jepsen, S.; Konstantinidis, A.; Makrilakis, K.; Taylor, R. Periodontitis and diabetes: A two-way relationship. Diabetologia 2012, 55, 21–31. [Google Scholar] [CrossRef]
- Teeuw, W.J.; Kosho, M.X.F.; Poland, D.C.W.; Gerdes, V.E.A.; Loos, B.G. Periodontitis as a possible early sign of diabetes mellitus. BMJ Open Diabetes Res. Care 2017, 5, e000326. [Google Scholar] [CrossRef]
- Institute for Public Health (IPH); National Institutes of Health; Ministry of Health Malaysia. National Health and Morbidity Survey (NHMS) 2019: Vol. 1: NCDs-Non-Communicable Diseases: Risk Factors and Other Health Problems. 2020. Available online: https://iku.moh.gov.my/images/IKU/Document/REPORT/NHMS2019/Report_NHMS2019-NCD_v2.pdf (accessed on 22 October 2022).
- Oral Health Division, Ministry of Health Malaysia. National Oral Health Survey of Adults 2010 (NOHSA 2010); Ministry of Health Malaysia: Putrajaya, Malaysia, 2013. [Google Scholar]
- Oral Health Division, Ministry of Health Malaysia. Management of Chronic Periodontitis. 2012. Available online: http://www.moh.gov.my/moh/attachments/8817.pdf (accessed on 22 October 2022).
- Kelly, J.T.; Reidlinger, D.P.; Hoffmann, T.C.; Campbell, K.L. Telehealth methods to deliver dietary interventions in adults with chronic disease: A systematic review and meta-analysis. Am. J. Clin. Nutr. 2016, 104, 1693–1702. [Google Scholar] [CrossRef] [PubMed]
- Hussain, A.; Bhowmik, B.; do Vale Moreira, N.C. COVID-19 y diabetes: Conocimiento en progreso. Diabetes Res. Clin. Pract. 2020, 162, 108142. [Google Scholar] [CrossRef] [PubMed]
- Iwasaki, M.; Usui, M.; Ariyoshi, W.; Nakashima, K.; Nagai-Yoshioka, Y.; Inoue, M.; Kobayashi, K.; Nishihara, T. Interruption of regular dental visits during the COVID-19 pandemic due to concerns regarding dental visits was associated with periodontitis in Japanese office workers. J. Periodontal. Res. 2021, 56, 1091–1098. [Google Scholar] [CrossRef] [PubMed]
- Wander, P.L.; Lowy, E.; Beste, L.A.; Tulloch-Palomino, L.; Korpak, A.; Peterson, A.C. The incidence of diabetes among 2,777,768 veterans with and without recent SARS-CoV-2 infection. Diabetes Care 2022, 45, 782–788. [Google Scholar] [CrossRef] [PubMed]
- Mehta, P.; Stahl, M.G.; Germone, M.M.; Nagle, S.; Guigli, R.; Thomas, J.; Shull, M.; Liu, E. Telehealth and nutrition support during the COVID-19 pandemic. Komp. Nutr. Diet. 2021, 1, 110–112. [Google Scholar] [CrossRef]
- Jamil, N.A.; Mohd-Said, S.; Hwa, C.S.; Sameeha, M.J.; Kruger, E. Needs Assessment Towards Development of an Integrated Diabetes-Oral Health Nutrition Education Module: A Qualitative Study. Int. J. Integr. Care 2021, 21, 10. [Google Scholar] [CrossRef] [PubMed]
- Jamil, N.A.; Chau, S.H.; Abdul Razak, N.I.; Shamsul Kamar, I.I.; Mohd-Said, S.; Rani, H.; Sameeha, M.J. Development and evaluation of an integrated diabetes-periodontitis nutrition and health education module. BMC Med. Educ. 2021, 21, 278. [Google Scholar] [CrossRef] [PubMed]
- Aris, M.A.; Pasi, H.; Shalihin, M.S.; Othman, U.; Abdul, N.H. Translation and Validation of Malay Version of the Simplified Diabetes Knowledge Test (DKT). Int. Med. J. Malays. 2018, 17, 76–84. [Google Scholar] [CrossRef]
- Shamsuddin, N.; Koon, P.B.; Zakaria, S.Z.; Noor, M.I.; Jamal, R. Reliability and validity of Malay language version of International Physical Activity Questionnaire (IPAQ-M) among the Malaysian cohort participants. Int. J. Public Health Res. 2015, 5, 643–653. [Google Scholar]
- Fei Yee, L.; Victor, G.; Chui Ling, G.; Wai Keung, L. Cross cultural adaptation and validation of the Malay Oral Impacts on Daily Performances. In Proceedings of the Faculty of Dentistry UKM Research & Innovation Symposium 1.0, Kuala Lumpur, Malaysia, 12–14 March 2019; pp. 102–104. [Google Scholar]
- Shanita, N.S.; Norimah, A.K.; Abu Hanifah, S. Development and validation of a Food Frequency Questionnaire (FFQ) for assessing sugar consumption among adults in Klang Valley, Malaysia. Malays. J. Nutr. 2012, 18, 283–293. [Google Scholar] [PubMed]
- Tee, E.S.; Noor, M.I.; Azudin, M.N.; Idris, K. Nutrient Composition of Malaysian Foods, 4th ed.; Institute of Medical Research: Kuala Lumpur, Malaysia, 1997. [Google Scholar]
- Shahar, S.; Chong, C.P.; Haron, H.; Noh, M.F. Sugar content of selected Malaysian desserts, snacks and cooked foods commonly consumed by Malaysian older adults. J. Sains Kesihat. Malays. 2018, 16, 235–236. [Google Scholar] [CrossRef][Green Version]
- Sharifah Azizah, T.N.; Nik Shanita, S.; Hasnah, H. Amount and types of sugars in selected commercial and traditional kuih in Klang Valley, Malaysia. Int. Food Res. J. 2015, 22, 2642–2649. [Google Scholar]
- Zainuddin, N.S.; Shahar, S.; Safii, N.S.; Haron, H.; Omar, M.A. Sugar intake and metabolic syndrome among older adults in Peninsular Malaysia. Malays. J. Nutr. 2018, 24, 163–174. [Google Scholar]
- Booth, A.O.; Lowis, C.; Hunter, S.J.; Dean, M.; Cardwell, C.R.; McKinley, M.C. Development and evaluation of a computer-based, self-management tool for people recently diagnosed with type 2 diabetes. J. Diabetes Res. 2016, 2016, 3192673. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ramadas, A.; Chan, C.K.; Oldenburg, B.; Hussein, Z.; Quek, K.F. Randomised-controlled trial of a web-based dietary intervention for patients with type 2 diabetes: Changes in health cognitions and glycemic control. BMC Public Health 2018, 18, 716. [Google Scholar] [CrossRef] [PubMed]
- Miller, C.K.; Kristeller, J.L.; Headings, A.; Nagaraja, H.; Miser, W.F. Comparative effectiveness of a mindful eating intervention to a diabetes self-management intervention among adults with type 2 diabetes: A pilot study. J. Acad. Nutr. Diet. 2012, 112, 1835–1842. [Google Scholar] [CrossRef] [PubMed]
- Ashton, L.M.; Sharkey, T.; Whatnall, M.C.; Williams, R.L.; Bezzina, A.; Aguiar, E.J.; Collins, C.E.; Hutchesson, M.J. Effectiveness of interventions and behaviour change techniques for improving dietary intake in young adults: A systematic review and meta-analysis of RCTs. Nutrients 2019, 11, 825. [Google Scholar] [CrossRef] [PubMed]
- Asaad, G.; Soria-Contreras, D.C.; Bell, R.C.; Chan, C.B. Effectiveness of a lifestyle intervention in patients with type 2 diabetes: The Physical Activity and Nutrition for Diabetes in Alberta (PANDA) trial. InHealthcare 2016, 4, 73. [Google Scholar] [CrossRef] [PubMed]
- Morton, K.; Beauchamp, M.; Prothero, A.; Joyce, L.; Saunders, L.; Spencer-Bowdage, S.; Dancy, B.; Pedlar, C. The effectiveness of motivational interviewing for health behaviour change in primary care settings: A systematic review. Health Psychol. Rev. 2015, 9, 205–223. [Google Scholar] [CrossRef] [PubMed]
- Tripathi, P.; Paranjape, M.; Tripathi, R.; Khandagale, S.; Bhagwat, G.; Kakrani, A. Effectiveness of Specifically Modified Plant Based Dietary Intervention and Anti-Gravity Exercise in Type 2 Diabetics a Follow-up Study. Int. J. Diabetes Endocrinol. 2018, 3, 50–57. [Google Scholar] [CrossRef]
- Leon, B.G.; Jensen, M.D.; Hartman, J.J.; Jensen, T.B. Self-Measured vs Professionally measured waist circumference. Ann. Fam. Med. 2016, 14, 262–266. [Google Scholar] [CrossRef] [PubMed]
- Gehlawat, M.; Lakshminarayanan, S.; Kar, S.S. Structured diabetes education program for improving self-care behavior in primary care settings of Puducherry: Evidence from a randomized controlled trial. Indian J. Community Med. 2019, 44, 107–112. [Google Scholar] [CrossRef]
- Wunsch, K.; Kienberger, K.; Niessner, C. Changes in physical activity patterns due to the COVID-19 pandemic: A systematic review and meta-analysis. Int. J. Environ. Res. Public Health 2022, 19, 2250. [Google Scholar] [CrossRef]
- Farid, D. COVID-19 and telenutrition: Remote consultation in clinical nutrition practice. Curr. Dev. Nutr. 2020, 4, nzaa124. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, A.; Gupta, R.; Misra, A. Telemedicine for diabetes care in India during COVID19 pandemic and national lockdown period: Guidelines for physicians. Diabetes Metab. Syndr. 2020, 14, 273–276. [Google Scholar] [CrossRef]
- Nor, N.M.; Shukri, N.A.; Yassin, N.Q.; Sidek, S.; Azahari, N. Barriers and enablers to make lifestyle changes among type 2 diabetes patients: A review. Sains Malays. 2019, 48, 1491–1502. [Google Scholar] [CrossRef]
- Ngwenya, B.T.; van Zyl, D.G.; Webb, E.M. Factors influencing non-attendance of clinic appointments in diabetic patients at a Gauteng hospital in 2007/2008. J. Endocrinol. Metab. Diabetes S. Afr. 2009, 14, 106–110. [Google Scholar] [CrossRef]

| Characteristic | IG (n = 14) | CG (n = 10) | p-Value | Total (n = 24) |
|---|---|---|---|---|
| Age (years) a | 54.1 (13.0) | 41.1 (11.5) | 0.019 | 48.7 (13.8) |
| Sex b | 0.403 | |||
| Male | 10 (71.4) | 5 (50.0) | 15 (62.5) | |
| Female | 4 (28.6) | 5 (50.0) | 9 (37.5) | |
| Ethnic Group b | 0.580 | |||
| Malay | 9 (64.3) | 8 (80.0) | 17 (70.8) | |
| Chinese | 4 (28.6) | 2 (20.0) | 5 (25.0) | |
| Indian | 1 (7.1) | 0 | 1 (4.2) | |
| Marital Status b | 0.393 | |||
| Single | 3 (21.4) | 4 (40.0) | 7 (29.2) | |
| Married | 11(78.6) | 6 (60.0) | 17 (70.8) | |
| Education Level b | ||||
| Secondary | 10 (71.4) | 0 | <0.001 | 10 (41.7) |
| Tertiary | 4 (28.6) | 10 (100.0) | 14 (58.3) | |
| Smoking Status b | 0.615 | |||
| Yes, currently smoke | 2 (14.3) | 3 (30.0) | 5 (20.8) | |
| Periodontitis Status b | 0.091 | |||
| Duration of diagnosis (year) c | 3.5 (4.3) | 2.0 (1.0) | 2.5 (2.0) |
| Parameter | IG (n = 14) | CG (n = 10) | p-Value between Group a (IG-CG at W0) | p-Value within Group IG b (W0–W12) | p-Value within Group CG b (W0–W12) | ||
|---|---|---|---|---|---|---|---|
| W0 | W12 | W0 | W12 | ||||
| Diabetes knowledge (%) | 44.3 (12.7) | 56.2 (11.6) | 45.3 (14.7) | 55.3 (10.9) | 0.854 | 0.008 | 0.062 |
| Body weight (kg) | 70.2 (15.1) | 68.8 (14.7) | 69.5 (20.4) | 69.7 (20.8) | 0.916 | 0.039 | 0.825 |
| Height (m) | 1.65 (0.09) | - | 1.62 (0.08) | - | 0.407 | - | - |
| Body mass index (kg/m2) | 25.8 (5.1) | 25.3 (4.9) | 26.4 (7.6) | 26.5 (7.7) | 0.820 | 0.029 | 0.895 |
| Waist circumference (cm) | 90.9 (17.5) | 90.6 (20.6) | 88.4 (17.9) | 88.7 (19.2) | 0.736 | 0.929 | 0.747 |
| Physical activity (MET-min/week) | 1797.2 (1196.2) | 1318.3 (591.0) | 1629.7 (2394.5) | 664.9 (422.8) | 0.723 | 0.306 | 0.314 |
| Oral health impact on daily performance (OIDP) * | 6.5 (18.8) | 0.0 (16.0) | 2.0 (70.5) | 0.0 (6.0) | 0.928 c | 0.066 d | 0.075 d |
| Energy (kcal/day) | 2095 (411) | 1490 (379) | 2127 (560) | 2032 (485) | 0.875 | <0.001 | 0.289 |
| Carbohydrate (g/day) | 276.7 (57.4) | 181.7 (35.7) | 292.6 (101.8) | 227.9 (69.0) | 0.629 | <0.001 | 0.015 |
| Protein (g/day) | 70.0 (17.3) | 62.0 (21.4) | 70.8 (19.2) | 77.0 (14.2) | 0.909 | 0.202 | 0.190 |
| Fat (g/day) | 82.1 (26.7) | 57.2 (26.2) | 79.3 (25.2) | 92.2 (27.1) | 0.801 | 0.021 | 0.172 |
| Added sugar intake (g/day) * | 32.4 (24.9) | 11.0 (21.6) | 51.2 (57.7) | 26.0 (89.6) | 0.259 | 0.016 c | 0.646 |
| Theme | Sub-Theme | Quotes |
|---|---|---|
| Convenience | Save time and cost | “It saves time and is cost-efficient. It didn’t bother me to drive and park my car” (S3, 45 years old). “I don’t need to leave home and go to the clinic at a specific time” (S9, 67 years old). |
| Feel more relaxed, comfortable, and safer | “I feel so comfortable doing it while at home. Feel more relaxed during counselling and safer due to COVID-19” (S5, 63 years old). | |
| Flexible | “It has flexible schedule arrangement plus I don’t need to worry about traffic” (S9, 67 years old). “It is easy to attend and free to do at any time and place” (S7, 64 years old). | |
| Practical | Easy to follow | “It is not too strict and easy to follow” (S7, 64 years old). “It is easy to remember the recommended changes because it also includes educational videos on the website” (S6, 61 years old). |
| Two-way learning | “It is still face-to-face and allows me to learn more from consultants rather than self-learning through education videos” (S2, 52 years old). “A very good programme. I get a chance to ask specifically about dietary practice and oral health even in a pandemic” (S9, 67 years old). | |
| Informative | “The content was very informative. I have become more health-conscious than before” (S5, 63 years old). | |
| Preferred approach during pandemic | “Good and new experience to use Google Meet for online counselling. It is very suitable to use now due to the pandemic outbreak” (S10, 62 years old). “I feel that it should continue as we are currently facing a pandemic and need to stay at home. It can be applied to any disease condition if they have good internet coverage” (S12, 51 years old). | |
| Increase awareness | “It increases my awareness to regularly take my medicine and insulin, which I previously skipped as I did not know of the consequences. It guides me to slowly reduce and control my alcohol intake, which previously I was unaware that it could affect my blood sugar control and health” (S12, 51 years old). “I became more aware of the relationship between these two diseases (diabetes and periodontitis) that I realised it is important to manage both conditions simultaneously” (S2, 52 years old). | |
| Increase in knowledge | “It helps me to increase my knowledge about my health, and I can feel my body healthier” (S6, 61 years old). | |
| Positive changes | Eating habits and exercise | “The modules taught me how to eat correctly and also suggested suitable exercise specific duration. Now, it has already become my usual routine to exercise, and I learn to eat more moderately” (S12, 51 years old). |
| Weight | “I’m very delighted as I have reduced my weight after joining this programme. The counselling helps to increase my determination to continue practicing a healthy lifestyle” (S6, 61 years old). |
| Theme | Sub-Theme | Quotes |
|---|---|---|
| Internal | Lack of self- discipline | “I find it hard to follow all recommended dietary intake due to my old eating habit. Even if I’m given more time, it depends on my self-discipline to practice it consistently every day” (S1, 59 years old). “I personally feel that the suggestions are not too strict and quite okay to follow, but it becomes too hard to accommodate with my usual lifestyle such as taking a less sweet drink or limit it to once daily” (S3, 45 years old). |
| Short duration | “Hard to initiate changes and I need more time to practice it gradually. The 3-month duration was inadequate to practice all suggested changes” (S10, 62 years old). “I need more time (more than 3 months) to make all the suggested dietary changes as suggested during the counselling” (S4, 22 years old). “It is very easy to follow the suggestions, but I need more time to discipline myself” (S9, 67 years old). | |
| External | Lack of support | “I find it hard to follow the suggestion because the people around me are unsupportive” (S3, 45 years old). |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rusly, N.F.S.; Jamil, N.A.; Mohd-Dom, T.N.; Rani, H.; Mohd-Said, S.; Mohd-Norwir, N.A.; Hamat, A. Exploring the Feasibility of an Online Diabetes Wellness Programme among Periodontitis Patients with Type II Diabetes Mellitus during the COVID-19 Pandemic. Healthcare 2022, 10, 2129. https://doi.org/10.3390/healthcare10112129
Rusly NFS, Jamil NA, Mohd-Dom TN, Rani H, Mohd-Said S, Mohd-Norwir NA, Hamat A. Exploring the Feasibility of an Online Diabetes Wellness Programme among Periodontitis Patients with Type II Diabetes Mellitus during the COVID-19 Pandemic. Healthcare. 2022; 10(11):2129. https://doi.org/10.3390/healthcare10112129
Chicago/Turabian StyleRusly, Nur Fadzlin Syahira, Nor Aini Jamil, Tuti Ningseh Mohd-Dom, Haslina Rani, Shahida Mohd-Said, Nur Adila Mohd-Norwir, and Afendi Hamat. 2022. "Exploring the Feasibility of an Online Diabetes Wellness Programme among Periodontitis Patients with Type II Diabetes Mellitus during the COVID-19 Pandemic" Healthcare 10, no. 11: 2129. https://doi.org/10.3390/healthcare10112129
APA StyleRusly, N. F. S., Jamil, N. A., Mohd-Dom, T. N., Rani, H., Mohd-Said, S., Mohd-Norwir, N. A., & Hamat, A. (2022). Exploring the Feasibility of an Online Diabetes Wellness Programme among Periodontitis Patients with Type II Diabetes Mellitus during the COVID-19 Pandemic. Healthcare, 10(11), 2129. https://doi.org/10.3390/healthcare10112129









