Prehospital Stroke Care, Paramedic Training Needs, and Hospital-Directed Feedback in Lithuania
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Setting
2.3. Ethics
2.4. Statistical Analysis
3. Results
3.1. Demographic Characteristics
3.2. Stroke Care Knowledge and Training Needs
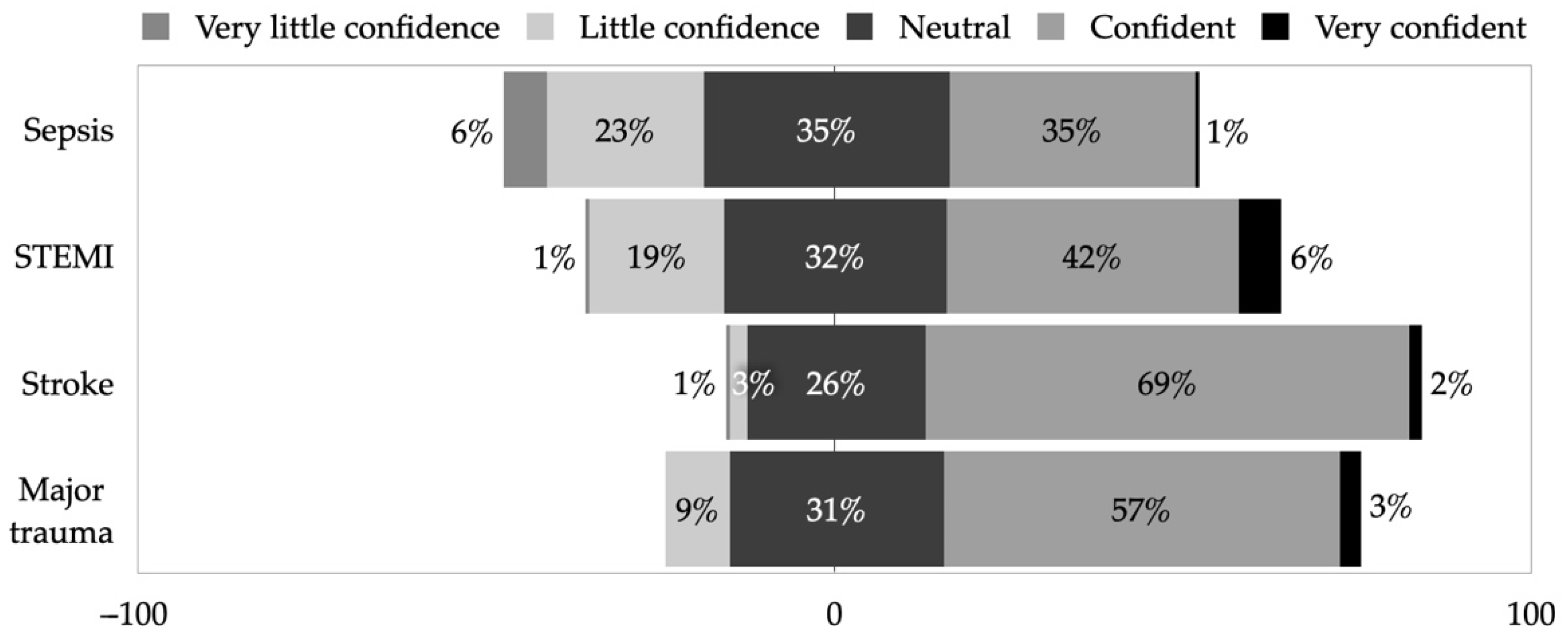
3.3. Confidence, Influence, and Trends Dealing with Time-Critical Conditions
3.4. Conditions Mimicking Stroke
3.5. Feedback
3.6. Attitude toward the Lithuanian Stroke Network
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Collaborators, G.S.; Feigin, V.L.; Stark, B.A.; Johnson, C.O.; Roth, G.A.; Bisignano, C.; Abady, G.G.; Abbasifard, M.; Abbasi-Kangevari, M.; Abd-Allah, F.; et al. Global, Regional, and National Burden of Stroke and Its Risk Factors, 1990–2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 2021, 20, 795–820. [Google Scholar] [CrossRef]
- Wafa, H.A.; Wolfe, C.D.A.; Emmett, E.; Roth, G.A.; Johnson, C.O.; Wang, Y. Burden of Stroke in Europe: Thirty-Year Projections of Incidence, Prevalence, Deaths, and Disability-Adjusted Life Years. Stroke 2020, 51, 2418–2427. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, A.; Czlonkowska, A.; Ford, G.A.; Fonseca, A.C.; Luijckx, G.J.; Korv, J.; Ossa, N.P.; Price, C.; Russell, D.; Tsiskaridze, A.; et al. European Academy of Neurology and European Stroke Organization Consensus Statement and Practical Guidance for Pre-hospital Management of Stroke. Eur. J. Neurol. 2018, 25, 425–433. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Emberson, J.; Lees, K.R.; Lyden, P.; Blackwell, L.; Albers, G.; Bluhmki, E.; Brott, T.; Cohen, G.; Davis, S.; Donnan, G.; et al. Effect of Treatment Delay, Age, and Stroke Severity on the Effects of Intravenous Thrombolysis with Alteplase for Acute Ischaemic Stroke: A Meta-Analysis of Individual Patient Data from Randomised Trials. Lancet 2014, 384, 1929–1935. [Google Scholar] [CrossRef] [Green Version]
- Melaika, K.; Sveikata, L.; Wiśniewski, A.; Jaxybayeva, A.; Ekkert, A.; Jatužis, D.; Masiliūnas, R. Changes in Prehospital Stroke Care and Stroke Mimic Patterns during the COVID-19 Lockdown. Int. J. Environ. Res. Public Health 2021, 18, 2150. [Google Scholar] [CrossRef]
- Mueller-Kronast, N.; Froehler, M.T.; Jahan, R.; Zaidat, O.; Liebeskind, D.; Saver, J.L.; Investigators, S. Impact of EMS Bypass to Endovascular Capable Hospitals: Geospatial Modeling Analysis of the US STRATIS Registry. J. Neurointerv. Surg. 2020, 12, 1058–1063. [Google Scholar] [CrossRef]
- Zhang, S.; Zhang, J.; Zhang, M.; Zhong, G.; Chen, Z.; Lin, L.; Lou, M. Prehospital Notification Procedure Improves Stroke Outcome by Shortening Onset to Needle Time in Chinese Urban Area. Aging Dis. 2018, 9, 426. [Google Scholar] [CrossRef] [Green Version]
- Li, T.; Munder, S.P.; Chaudhry, A.; Madan, R.; Gribko, M.; Arora, R. Emergency Medical Services Providers’ Knowledge, Practices, and Barriers to Stroke Management. Open Access Emerg. Med. 2019, 11, 297–303. [Google Scholar] [CrossRef] [Green Version]
- Abboud, M.E.; Band, R.; Jia, J.; Pajerowski, W.; David, G.; Guo, M.; Mechem, C.C.; Messé, S.R.; Carr, B.G.; Mullen, M.T. Recognition of Stroke by EMS Is Associated with Improvement in Emergency Department Quality Measures. Prehospital Emerg. Care 2016, 20, 729–736. [Google Scholar] [CrossRef]
- Oostema, J.A.; Chassee, T.; Baer, W.; Edberg, A.; Reeves, M.J. Brief Educational Intervention Improves Emergency Medical Services Stroke Recognition. Stroke 2019, 50, 1193–1200. [Google Scholar] [CrossRef]
- Sveikata, L.; Melaika, K.; Wiśniewski, A.; Vilionskis, A.; Petrikonis, K.; Stankevičius, E.; Jurjans, K.; Ekkert, A.; Jatužis, D.; Masiliūnas, R. Interactive Training of the Emergency Medical Services Improved Prehospital Stroke Recognition and Transport Time. Front. Neurol. 2022, 13, 765165. [Google Scholar] [CrossRef] [PubMed]
- Choi, B.; Tsai, D.; McGillivray, C.G.; Amedee, C.; Sarafin, J.-A.; Silver, B. Hospital-Directed Feedback to Emergency Medical Services Improves Prehospital Performance. Stroke 2018, 45, 2137–2140. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eaton-Williams, P.; Mold, F.; Magnusson, C. Effective Clinical Feedback Provision to Ambulance Clinicians: A Literature Review. J. Paramed. Pract. 2020, 12, 109–117. [Google Scholar] [CrossRef]
- McClelland, G.; Flynn, D.; Rodgers, H.; Price, C. A Survey of UK Paramedics’ Views about Their Stroke Training, Current Practice and the Identification of Stroke Mimics. Br. Paramed. J. 2017, 2, 4–15. [Google Scholar] [CrossRef]
- Masiliūnas, R.; Vilionskis, A.; Bornstein, N.M.; Rastenytė, D.; Jatužis, D. The Impact of a Comprehensive National Policy on Improving Acute Stroke Patient Care in Lithuania. Eur. Stroke J. 2022, 7, 134–142. [Google Scholar] [CrossRef] [PubMed]
- Jatužis, D.; Rastenytė, D.; Vilionskis, A.; Matijošaitis, V.; Ryliškienė, K. Galvos Smegenų Insulto Diagnostikos, Gydymo Ir Profilaktikos Metodika; Vilniaus Universiteto Leidykla: Vilnius, Lithuania, 2021; ISBN 978-609-07-0584-1. [Google Scholar]
- Ministry of Health of the Republic of Lithuania. Available online: https://e-seimas.lrs.lt/portal/legalAct/lt/TAD/TAIS.437212/asr (accessed on 10 May 2022).
- Eaton, G. Paramedic. Noun. Br. Paramed. J. 2019, 4, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Brunton, L.; Boaden, R.; Knowles, S.; Ashton, C.; Parry-Jones, A.R. Pre-Hospital Stroke Recognition in a UK Centralised Stroke System: A Qualitative Evaluation of Current Practice. Br. Paramed. J. 2019, 4, 31–39. [Google Scholar] [CrossRef]
- Williams, I.; Valderrama, A.L.; Bolton, P.; Greek, A.; Greer, S.; Patterson, D.G.; Zhang, Z. Factors Associated with Emergency Medical Services Scope of Practice for Acute Cardiovascular Events. Prehospital Emerg. Care 2011, 16, 189–197. [Google Scholar] [CrossRef]
- Powers, W.J.; Rabinstein, A.A.; Ackerson, T.; Adeoye, O.M.; Bambakidis, N.C.; Becker, K.; Biller, J.; Brown, M.; Demaerschalk, B.M.; Hoh, B.; et al. Guidelines for the Early Management of Patients with Acute Ischemic Stroke: 2019 Update to the 2018 Guidelines for the Early Management of Acute Ischemic Stroke: A Guideline for Healthcare Professionals from the American Heart Association/American Stroke Association. Stroke 2019, 50, e344–e418. [Google Scholar] [CrossRef]
- Suppan, M.; Stuby, L.; Carrera, E.; Cottet, P.; Koka, A.; Assal, F.; Savoldelli, G.L.; Suppan, L. Asynchronous Distance Learning of the National Institutes of Health Stroke Scale During the COVID-19 Pandemic (E-Learning vs. Video): Randomized Controlled Trial. J. Med. Internet Res. 2021, 23, e23594. [Google Scholar] [CrossRef]
- Grotta, J.C.; Yamal, J.-M.; Parker, S.A.; Rajan, S.S.; Gonzales, N.R.; Jones, W.J.; Alexandrov, A.W.; Navi, B.B.; Nour, M.; Spokoyny, I.; et al. Prospective, Multicenter, Controlled Trial of Mobile Stroke Units. N. Engl. J. Med. 2021, 385, 971–981. [Google Scholar] [CrossRef] [PubMed]
- Ebinger, M.; Siegerink, B.; Kunz, A.; Wendt, M.; Weber, J.E.; Schwabauer, E.; Geisler, F.; Freitag, E.; Lange, J.; Behrens, J.; et al. Association Between Dispatch of Mobile Stroke Units and Functional Outcomes Among Patients with Acute Ischemic Stroke in Berlin. JAMA 2021, 325, 454–466. [Google Scholar] [CrossRef] [PubMed]
- Ramanathan, R.S.; Wisco, D.; Vela-Duarte, D.; Zafar, A.; Taqui, A.; Winners, S.; Buletko, A.B.; Hustey, F.; Reimer, A.; Russman, A.; et al. Pre-Hospital Diagnosis in Mobile Stroke Unit. J. Stroke Cerebrovasc. Dis. 2021, 30, 105801. [Google Scholar] [CrossRef] [PubMed]
- Phillips, D.; Grunwald, I.Q.; Walter, S.; Faßbender, K. Mobile Stroke Unit in the UK Healthcare System: Avoidance of Unnecessary Accident and Emergency Admissions. Br. Paramed. J. 2021, 5, 64. [Google Scholar] [CrossRef]
- Koivulahti, O.; Tommila, M.; Haavisto, E. The Accuracy of Preliminary Diagnoses Made by Paramedics—A Cross-Sectional Comparative Study. Scand. J. Trauma Resusc. Emerg. Med. 2020, 28, 70. [Google Scholar] [CrossRef]
- Pollard, J.; Black, S. Do paramedics find it beneficial to learn the diagnosis given to their patients in the emergency department? Emerg. Med. J. 2015, 32, 421. [Google Scholar] [CrossRef]
- Cash, R.E.; Crowe, R.P.; Rodriguez, S.A.; Panchal, A.R. Disparities in Feedback Provision to Emergency Medical Services Professionals. Prehospital Emerg. Care 2017, 21, 773–778. [Google Scholar] [CrossRef]
- McGuire, S.S.; Luke, A.; Klassen, A.B.; Myers, L.A.; Mullan, A.F.; Sztajnkrycer, M.D. It’s Time to Talk to Prehospital Providers: Feedback Disparities among Ground-Based Emergency Medical Services Providers and Its Impact on Job Satisfaction. Prehospital Disaster Med. 2021, 36, 486–494. [Google Scholar] [CrossRef]
- Gunderson, M.R.; Florin, A.; Price, M.; Reed, J. NEMSMA Position Statement and White Paper: Process and Outcomes Data Sharing between EMS and Receiving Hospitals. Prehospital Emerg. Care 2020, 25, 307–313. [Google Scholar] [CrossRef]
- Gibson, L.; Whiteley, W. The Differential Diagnosis of Suspected Stroke: A Systematic Review. J. R. Coll. Physicians Edinb. 2013, 43, 114–118. [Google Scholar] [CrossRef]
- Khanevski, A.N.; Kvistad, C.E.; Novotny, V.; Næss, H.; Thomassen, L.; Logallo, N.; Bjerkreim, A.T. Incidence and Etiologies of Stroke Mimics after Incident Stroke or Transient Ischemic Attack. Stroke 2019, 50, 2937–2940. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Visseren, F.L.J.; Mach, F.; Smulders, Y.M.; Carballo, D.; Koskinas, K.C.; Bäck, M.; Benetos, A.; Biffi, A.; Boavida, J.-M.; Capodanno, D.; et al. 2021 ESC Guidelines on Cardiovascular Disease Prevention in Clinical Practice. Eur. J. Prev. Cardiol. 2022, 29, 5–115. [Google Scholar] [CrossRef] [PubMed]
- Karliński, M.; Gluszkiewicz, M.; Członkowska, A. The Accuracy of Prehospital Diagnosis of Acute Cerebrovascular Accidents: An Observational Study. Arch. Med. Sci. Ams. 2015, 11, 530–535. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kozera-Strzelińska, D.; Karliński, M.; Rak, G.; Wojdacz, M.; Sienkiewicz-Jarosz, H.; Kurkowska-Jastrzębska, I. Stroke and TIA Mimics in Patients Referred to a Neurological Emergency Department by Non-Ambulance Physicians, Ambulance Physicians and Paramedics. Neurol. Neurochir. Pol. 2019, 53, 83–89. [Google Scholar] [CrossRef]




| n (%) | ||
|---|---|---|
| Female gender | 120 | (74.5) |
| Age range (years) | ||
| 20–29 | 10 | (6.4) |
| 30–39 | 11 | (7.0) |
| 40–49 | 53 | (33.8) |
| 50–59 | 58 | (36.9) |
| 60–69 | 24 | (15.3) |
| 70+ | 1 | (0.6) |
| Experience in prehospital care (years) | ||
| <2 | 6 | (3.7) |
| 3–5 | 14 | (8.7) |
| 6–10 | 8 | (5.0) |
| 11–20 | 17 | (10.6) |
| 21–30 | 58 | (36.0) |
| 31–40 | 44 | (27.3) |
| 41+ | 14 | (8.7) |
| Ambulance employer | ||
| Vilnius city | 97 | (60.2) |
| Vilnius district | 59 | (36.6) |
| Both | 5 | (3.2) |
| Education | ||
| Community nurse | 134 | (83.8) |
| Paramedic | 22 | (13.8) |
| Medical doctor | 4 | (2.5) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Melaika, K.; Sveikata, L.; Vilionskis, A.; Wiśniewski, A.; Jurjans, K.; Klimašauskas, A.; Jatužis, D.; Masiliūnas, R. Prehospital Stroke Care, Paramedic Training Needs, and Hospital-Directed Feedback in Lithuania. Healthcare 2022, 10, 1958. https://doi.org/10.3390/healthcare10101958
Melaika K, Sveikata L, Vilionskis A, Wiśniewski A, Jurjans K, Klimašauskas A, Jatužis D, Masiliūnas R. Prehospital Stroke Care, Paramedic Training Needs, and Hospital-Directed Feedback in Lithuania. Healthcare. 2022; 10(10):1958. https://doi.org/10.3390/healthcare10101958
Chicago/Turabian StyleMelaika, Kazimieras, Lukas Sveikata, Aleksandras Vilionskis, Adam Wiśniewski, Kristaps Jurjans, Andrius Klimašauskas, Dalius Jatužis, and Rytis Masiliūnas. 2022. "Prehospital Stroke Care, Paramedic Training Needs, and Hospital-Directed Feedback in Lithuania" Healthcare 10, no. 10: 1958. https://doi.org/10.3390/healthcare10101958
APA StyleMelaika, K., Sveikata, L., Vilionskis, A., Wiśniewski, A., Jurjans, K., Klimašauskas, A., Jatužis, D., & Masiliūnas, R. (2022). Prehospital Stroke Care, Paramedic Training Needs, and Hospital-Directed Feedback in Lithuania. Healthcare, 10(10), 1958. https://doi.org/10.3390/healthcare10101958









