Abstract
Background: Percutaneous coronary intervention (PCI) is associated with a short hospital stay and fast recovery. However, it might be related to insufficient implementation of lifestyle changes after the procedure. Conversely, coronary artery bypass grafting (CABG) is a highly invasive technique that requires a prolonged hospital stay and long rehabilitation with more opportunities for education. This study aimed to evaluate the impact of CABG on adherence to lifestyle modifications and knowledge about coronary artery disease (CAD) in comparison with PCI. We also evaluated the level of education and tried to define groups of patients that might require targeted education. Methods: Data was collected using a self-designed 56-item questionnaire. Questions assessed the knowledge of CAD risk factors and the level of their control. Results: The study group consisted of 155 consecutive patients admitted to the Cardiology Department. Patients with a history of PCI (68%) (at least 8 weeks before) were included in the prior-PCI group, and patients with previous surgical revascularization (also at least 8 weeks before) were assigned to the prior-CABG group (32%). The knowledge score was higher in the prior-CABG group. The median (IQR) results in the prior-PCI vs. prior-CABG group were, respectively: 20 (12–24) vs. 22 (19–25) [points, per 31 max.]; p = 0.01. Similar results were obtained in the level of risk control (prior-PCI vs. prior-CABG, respectively: 6 (4–7) vs. 7 (6–8) [points, per 15 max.]; p = 0.002). Conclusions: The method of treatment of CAD might impact the implementation of lifestyle modifications after the procedure. More effort is required to improve secondary prevention, especially in PCI patients.
1. Introduction
The importance of cardiovascular disorders (CVD), being the leading cause of death in developed countries, is unquestionable [1]. Furthermore, CVD are strongly related to several well-known modifiable risk factors. According to World Health Organization data, up to 80% of premature CVD-related deaths could be avoided with proper prevention introduced in time [2]. Previously reported studies have indicated no differences in the level of knowledge about CVD and risk factor control between patients with a history of one or several percutaneous coronary interventions (PCI) [3,4]. A short hospitalization period or low awareness about the severity of the disease among patients undergoing fast and convenient procedures might explain this finding. On the contrary, coronary artery bypass grafting (CABG) is a more stressful procedure associated with a longer hospital stay. There is a paucity of data comparing adherence to secondary prevention recommendations in patients with a history of several PCI procedures and patients after CABG. Further investigation might provide additional data to understand the factors that shape patients’ attitudes towards lifestyle changes and help create personalized educational programs. Thus, we sought to assess the knowledge, awareness, and prevalence of self-reported risk factors for CAD in the groups of patients after CABG or PCI procedures.
2. Materials and Methods
2.1. Methodology
A complete description of the methodology was reported previously [3]. Briefly, a self-designed questionnaire comprising 18 questions concerning sociodemographic and clinical profile, 11 assessing knowledge about CAD, and 6 referring to the CAD risk factor control was used. Some questions included a few subsections, so the maximal knowledge score was 31 points. For the assessment of risk control, we analysed information from our survey and clinical data obtained during hospitalization and the maximal score was 15 points. The questionnaire is presented in Supplementary Materials. The questionnaire S1 is presented in Supplementary Materials. The study group included 155 consecutive patients admitted to the 2nd Department of Cardiology and Cardiovascular Interventions at the University Hospital in Kraków (Poland) from July 2016 to July 2019. The inclusion criteria comprised the history of PCI or CABG and the patient’s consent. All patients were enrolled by a trained researcher and signed informed consent and consent for the processing of personal data. All patients provided written informed consent to participate in the study. According to the clinical profile, the patients were divided into two subgroups: the prior-PCI group comprised patients that had undergone PCI at least eight weeks prior to the current hospitalization; the prior-CABG group included patients with a history of CABG at least eight weeks prior to the enrolment. The number of patients in the groups is presented in Figure 1. The study protocol was approved by the local ethics committee. The study was conducted under the ethical principles of clinical research based on the Declaration of Helsinki with its later amendments.
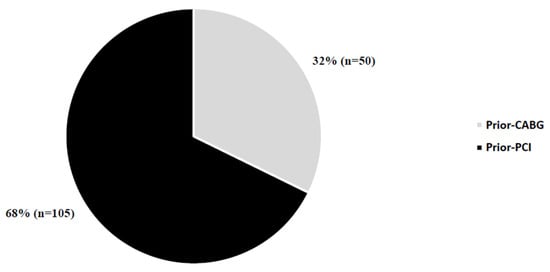
Figure 1.
Number of patients in study groups. Abbreviations: CABG, coronary artery bypass grafting; PCI, percutaneous coronary intervention.
2.2. Statistical Analysis
Standard statistical tests performed with Statistica v13 software (StatSoft, Inc., Kraków, Poland) were used for data processing. The Shapiro–Wilk test was used to determine the normality of distribution. The chi-square test was applied for the comparison of qualitative variables, presented as numbers and percentages. Student’s t-test and the Mann–Whitney U test were used for comparison of quantitative variables that were presented as mean and standard deviation (SD) or median and interquartile range (IQR). The correlations between independent variables were assessed with Spearman’s rank correlation, and multiple regression analysis was applied for more complex interaction models. Statistical significance was set at a p value < 0.05.
3. Results
The results of the comparison of the sociodemographic and clinical profiles are presented in Table 1 and Table 2. The knowledge score was higher in the prior-CABG group (prior-PCI vs. prior-CABG, respectively: 20 (12–24) vs. 22 (19–25) [points, per 31 max.]; p = 0.01). Similar results were obtained from the comparison of the level of risk control (prior-PCI vs. prior-CABG, respectively: 6 (4–7) vs. 7 (6–8) [points, per 15 max]; p = 0.002). The median age of patients (IQR) was higher in the prior-CABG group: (prior-PCI vs. prior-CABG, respectively: 66 (60–75) vs. 70 (66–79); p = 0.03). The median duration of CAD (IQR) was also longer in the prior-CABG group: (prior-PCI vs. prior-CABG, respectively: 8 (3–15) vs. 19 (10–24.5); p = 0.001) as well as the proportion patients with a history of two or more previous cardiac hospitalizations was greater in the prior-CABG group (prior-PCI vs. prior-CABG, respectively: 63 (60%) vs. 40 (80%); p = 0.02).

Table 1.
Comparison of sociodemographic profile.

Table 2.
Comparison of clinical profile.
The results of the prevalence of particular CAD risk factors are presented in Table 3. Patients after CABG were found to have better control of glucose despite an even higher prevalence of diabetes mellitus (Table 2 and Table 3). In addition, they participated in cardiac rehabilitation more often as compared with the prior-PCI group (Table 3). Stationary rehabilitation was the most popular option. It was attended by 33% of respondents, most often in the prior-CABG group (prior-CABG vs. prior-PCI: 73% vs. 33%; p = 0.001). No differences were observed in other forms of rehabilitation. In multiple regression analysis, the impact of cardiac rehabilitation on the level of knowledge score was found only in the prior-CABG group for not attending any form of rehabilitation (R2 = 0.2, ꞵ = −9.9; p = 0.02). No relationship was found between the level of knowledge and any form of rehabilitation. Avoiding cardiac rehabilitation was associated with worse results in the risk control score in the overall population (R2 = 0.20, ꞵ = −2.9; p = 0.001) and the prior-PCI group (R2 = 0.15, ꞵ = −2.5; p = 0.004). Furthermore, participation in ambulatory rehabilitation also appeared to be related to a worse level of risk control in the overall population (R2 = 0.19, ꞵ = −1.4; p = 0.01) and in the prior-CABG group (R2 = 0.3, ꞵ = −3.0; p = 0.004). No association was found for any other form of rehabilitation. Prescribed medications were omitted at least once per month by 13% of patients (prior-PCI vs. prior-CABG, respectively: 13% vs. 11%; p = 0.7). The comparison of home blood pressure control also revealed no significant differences, 4% of patients never measured blood pressure at home (3% including only hypertensive patients) and 75% made the measurement more than once a week (78% of hypertensive patients). All of the patients in the CABG group controlled blood pressure, even without an original diagnosis of arterial hypertension. The analysis of the frequency of general practitioner (GP) visits revealed no differences between groups. However, patients in the prior-CABG group were found to visit cardiologists more often (visits every six months, prior-CABG vs. prior-PCI: 88% vs. 68%; p = 0.01). The risk control score was affected only by the frequency of cardiologist visits and no impact was found for the GP visits; patients visiting cardiologists at least once per 6 months achieved better results: 6 (5–8) vs. 5 (4–6) [points]; p = 0.006.

Table 3.
Comparison of particular CAD risk factors in study groups.
Analysis of the impact of other factors on the level of knowledge and the risk control is presented in Table 4 and Table 5. Significant correlations were found in the overall population for the duration of CAD and the level of risk control (R = 0.17; p = 0.002) and the number of hospitalizations and the level of CAD risk control (R = 0.2; p = 0.001). Analysis of the relationship between the actual level of patients’ knowledge and self-assessed level of knowledge revealed a correlation in the overall population (R = 0.24; p = 0.01) and in the prior-PCI group (R = 0.34; p = 0.001), however, a similar correlation was not observed between the self-assessed level of care about one’s health and the level of risk control (R = 0.14; p = 0.08).

Table 4.
Impact of factors other than a history of PCI or CABG on the level of knowledge and the level of coronary artery disease risk control—independent analysis.

Table 5.
Impact of factors other than a history of PCI or CABG on the level of knowledge and the level of coronary artery disease risk control—multiple regression model.
4. Discussion
This study demonstrates that patients after CABG have a higher knowledge score and level of risk control score in comparison with the prior-PCI group. They also more often attended any form of cardiac rehabilitation. However, the age of patients was higher, the duration of the CAD was longer and the number of patients with a history of two or more previous cardiac hospitalizations was also higher in the prior-CABG group. Significant correlations were found in the overall population for the duration of CAD and the level of risk control, and the number of hospitalizations and the level of CAD risk control. These variables and correlations are worth emphasizing and might, from presuppositions, impact higher knowledge and level of risk control scores in the prior-CABG group. Nonetheless, the results of this study suggest that further improvement in education and control of risk factors must be taken into consideration. Treatment of CAD has significantly developed in recent decades, which may result in the reduction of major risk factors [5,6]. The role of the pharmacological treatment of CAD is unquestionable but highly insufficient to obtain maximal control of risk factors [7,8,9,10]. Furthermore, secondary prevention programs have a beneficial impact on risk factor control and both cardiac mortality and the quality of life [11,12].
The large cross-sectional study EUROASPIRE IV has shown that most patients with CAD do not fulfil the guideline standards for secondary prevention. A high prevalence of risk factors such as persistent smoking, unhealthy diet, physical inactivity, obesity, and diabetes was observed [7]. Polish multicentre national health survey WOBASZ II has shown that about one-third of the adult population had comorbid hypertension and hypercholesterolemia, and that control of these factors was strongly associated with CAD [13]. Furthermore, less than half of the patients took part in any kind of cardiac prevention and rehabilitation program [7,8,9]. Percutaneous coronary intervention is associated with faster recovery, immediate relief of symptoms, shorter hospital stays, and improved short- medium-term prognosis as compared with CABG [14,15]. The risk of periprocedural death, stroke, and bleeding complications after the PCI procedure is also determined by the access type and the experience of the operator [16]. Stent type might also influence long-term mortality, especially in patients presenting with STEMI [17]. On the contrary, the surgeon’s experience was not associated with long-term mortality following CABG [18]. Another important factor reducing patients’ predicted morbidity and mortality is cardiac rehabilitation [14]. A previous meta-analysis reported reduced cardiovascular mortality and improved quality of life in patients participating in cardiac rehabilitation [19]. Furthermore, it might also be connected with a reduction in the number of uncontrolled risk factors [20]. Different studies have confirmed the importance of cardiac rehabilitation as a part of secondary prevention strategies and demonstrated a reduction in CVD mortality and better quality of life [7,21,22]. The general uptake of cardiac rehabilitation in our study was 56% and it was similar to that reported in other studies [7,9,23,24]. In the prior-CABG group, this percentage was significantly higher (78%) than in the prior-PCI group (46%). Patients after CABG more frequently attend stationary rehabilitation. Cardiac rehabilitation reduces mortality in PCI and CABG patients. However, a greater impact on reducing the number of cardiovascular events was reported in the CABG group [25]. Furthermore, the postprocedural hospital stay is longer after CABG than after PCI [5]. This might be connected to better education provided during post-operative hospitalization and early in-hospital rehabilitation. Further cardiac rehabilitation emphasizes this effect and improves patient awareness in combination with comprehensive education programs [26,27,28].
In our institution, patient education includes recommendations written on a discharge card and explanations provided by a medical doctor. Patients are also advised on other reliable sources of information, including online materials. However, lack of time and stress associated with hospitalization might result in poor compliance and a lower level of patient knowledge.
Higher social status (higher education, income, living in an urban area) was associated with better knowledge results but not with a better risk control score. The SPIRR CAD study examined the standard and psychosocial risk factor profiles concerning socio-economic status (SES) [29]. Only smoking was more common in patients with low SES. The results demonstrated no direct influence of SES on better risk factor control [30]. It might be assumed that education alone does not have the desired impact on the patients’ lifestyle modification. Other programs improving patients’ awareness and motivation should be implemented. In this study, patients after CABG were found to have better control of glucose despite an even higher prevalence of diabetes mellitus. The modifiable risk profiles and risk factor knowledge were improved alternatively in the CHOICE trial [27]. This program comprised clinic visits, telephone support, and obligatory cholesterol reduction and preferential risk factor modification. The CHOICE group had higher risk factor levels such as total cholesterol, systolic blood pressure, smoking status, and physical activity than the control group after one year. Three or more risk factors above the recommended values were reported in 21% of participants. Various educational programs during recent years have proven their efficacy in the improvement of lifestyle changes [26,28,31,32]. The correlation between the level of knowledge and the level of risk factor control has not been found in the overall population. Patients achieving better results in knowledge tests had no improvement in CAD risk factor control. These findings are in line with data suggesting no impact of education alone on the mortality rate [11]. Thus, personalized educational programs for CAD patients might be crucial for further improvement in the long-term outcomes.
5. Conclusions
Patients after CABG have a higher knowledge score and level of risk factor control score in comparison to the patients after PCI. Longer procedure-related hospitalization, a greater number of hospitalizations, a longer duration of CAD, and the scope of the CABG procedure might be associated with these findings. Education and cardiac rehabilitation programs should be widely implemented in patients with CAD.
Study Limitations
Several limitations should be acknowledged. We presented data based on a single-centre experience with a relatively low number of patients. We have only included patients admitted to the 2nd Department of Cardiology and Cardiovascular Interventions at the University Hospital in Kraków (Poland) from July 2016 to July 2019. Therefore, multicentre studies are essential to creating recommendations and educational programs that might be introduced into common clinical practice. Furthermore, there are several significant differences in the clinical profiles between the main groups of the study. Although, we were focused not only on the impact of the CABG procedure itself but also on the profile of patients in the study groups to identify factors with the potential to impact knowledge and risk control. All included patients were stable and admitted with chronic coronary artery syndrome, but also with various cardiological comorbidities. Thus, patients with an initially more severe condition at admission might have had poorer adherence to health recommendations. Furthermore, the health and mental condition might influence the data provided in the questionnaire. Another limitation is the absence of validation. We decided to use a self-constructed questionnaire. However, there is a lack of validated tools that might be suitable for this study. Our study included a relatively low number of patients. Thus, we could not use propensity score matching in statistical analysis. Therefore, an imbalance in baseline characteristics might be observed between the groups.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/healthcare10061142/s1, The questionnaire S1: Assessment of the knowledge and control of risk factors for the development of atherosclerosis among patients after first-time and subsequent revascularization of coronary vessels.
Author Contributions
K.W., T.T. and M.M. conceived the idea for the study and prepared the manuscript. K.W. and T.T. conducted the statistical analysis. K.W., T.T., M.M., A.D., T.R., S.B. and D.D. have substantial contributions to the analysis and interpretation of data. All authors revised the manuscript critically for important intellectual content. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the local ethics committee.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- OECD; European Union. Main causes of mortality. In Health at a Glance: Europe 2018: State of Health in the EU Cycle; OECD Publishing: Paris, France; European Union: Brussels, Belgium, 2018. [Google Scholar] [CrossRef]
- Cardiovascular Diseases—Data and Statistics—WHO/Europe. Available online: http://www.euro.who.int/en/health-topics/noncommunicable-diseases/cardiovascular-diseases/data-and-statistics (accessed on 14 April 2020).
- Wójcicki, K.; Krycińska, R.; Tokarek, T.; Siudak, Z.; Dziewierz, A.; Rajtar-Salwa, R.; Januszek, R.; Reczek-Siwiec, A.; Dudek, D. Knowledge and prevalence of risk factors for coronary artery disease in patients after the first and repeated percutaneous coronary intervention. Kardiol Pol. 2020, 78, 147–153. [Google Scholar] [CrossRef] [PubMed]
- Nolan, M.T.; McKee, G. Is Knowledge Level of Coronary Heart Disease and Risk Factors Among Post-Percutaneous Coronary Intervention Patients Adequate? J. Cardiovasc. Nurs. 2016, 31, E1–E9. [Google Scholar] [CrossRef] [PubMed]
- Jaworski, R.; Jankowska, E.A.; Ponikowski, P.; Banasiak, W. Costs of management of patients with coronary artery disease in Poland: The multicenter RECENT study. Pol. Arch. Med. Wewn. 2012, 122, 599–607. [Google Scholar] [CrossRef] [PubMed]
- Ford, E.S.; Ajani, U.A.; Croft, J.B.; Critchley, J.A.; Labarthe, D.R.; Kottke, T.E.; Giles, W.H.; Capewell, S. Explaining the decrease in U.S. deaths from coronary disease, 1980–2000. N. Engl. J. Med. 2007, 356, 2388–2398. [Google Scholar] [CrossRef]
- Kotseva, K.; Wood, D.; De Bacquer, D.; De Backer, G.; Rydén, L.; Jennings, C.; Gyberg, V.; Amouyel, P.; Bruthans, J.; Castro Conde, A.; et al. EUROASPIRE IV: A European Society of Cardiology survey on the lifestyle, risk factor and therapeutic management of coronary patients from 24 European countries. Eur. J. Prev. Cardiol. 2016, 23, 636–648. [Google Scholar] [CrossRef] [PubMed]
- De Backer, G.; De Bacquer, D.; Rydén, L.; Kotseva, K.; Gaita, D.; Georgiev, B.; Gotcheva, N.; Mancas, S.; Miličić, D.; the EUROASPIRE investigators; et al. Lifestyle and risk factor management in people at high cardiovascular risk from Bulgaria, Croatia, Poland, Romania and the United Kingdom who participated in both the EUROASPIRE III and IV primary care surveys. Eur. J. Prev. Cardiol. 2016, 23, 1618–1627. [Google Scholar] [CrossRef]
- Kotseva, K. EUROASPIRE—Time Trends in Lifestyle, Cardiovascular Risk Factors, and Therapeutic Management in Patients with Coronary Disease in Europe: A Comparison of EUROASPIRE IV and V Surveys over 5 Years in 21 Countries; ESC Congress: Munich, Germany, 2018. [Google Scholar]
- Jankowski, P.; Czarnecka, D.; Wolfshaut-Wolak, R.; Łysek, R.; Łukaszewska, A.; Bogacki, P.; Grodecki, J.; Mirek-Bryniarska, E.; Nessler, J.; Podolec, P.; et al. Secondary prevention of coronary artery disease in contemporary clinical practice. Cardiol. J. 2015, 22, 219–226. [Google Scholar] [CrossRef]
- Brown, J.P.; Clark, A.; Dalal, H.; Welch, K.; Taylor, R.S. Effect of patient education in the management of coronary heart disease: A systematic review and meta-analysis of randomized controlled trials. Eur. J. Prev. Cardiol. 2013, 20, 701–714. [Google Scholar] [CrossRef]
- Clark, A.M.; Hartling, L.; Vandermeer, B.; McAlister, F.A. Meta-analysis: Secondary prevention programs for patients with coronary artery disease. Ann. Intern. Med. 2005, 143, 659–672. [Google Scholar] [CrossRef]
- Niklas, A.; Marcinkowska, J.; Kozela, M.; Andrzej, P.; Tomasz, Z.; Wojciech, D.; Aleksandra, P.; Magdalena, K.; Krystyna, K.; Andrzej, T. Blood pressure and cholesterol control in patients with hypertension and hypercholesterolemia: The results from the Polish multicenter national health survey WOBASZ II. Pol. Arch. Intern. Med. 2019, 129, 864–873. [Google Scholar]
- Neumann, F.-J.; Sousa-Uva, M.; Ahlsson, A.; Alfonso, F.; Banning, A.P.; Benedetto, U.; Byrne, R.A.; Collet, J.-P.; Falk, V.; Head, S.J.; et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur. Heart J. 2019, 40, 87–165. [Google Scholar] [CrossRef] [PubMed]
- Serruys, P.W.; Morice, M.C.; Kappetein, A.P.; Colombo, A.; Holmes, D.R.; Mack, M.J.; Ståhle, E.; Feldman, T.E.; van den Brand, M.; Bass, E.J.; et al. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N. Engl. J. Med. 2009, 360, 961–972. [Google Scholar] [CrossRef] [PubMed]
- Tokarek, T.; Dziewierz, A.; Plens, K.; Rakowski, T.; Zabojszcz, M.; Dudek, D.; Siudak, Z. Radial Approach Expertise and Clinical Outcomes of Percutanous Coronary Interventions Performed Using Femoral Approach. J. Clin. Med. 2019, 8, 1484. [Google Scholar] [CrossRef] [PubMed]
- Siudak, Z.; Dziewierz, A.; Rakowski, T.; Żmudka, K.; Legutko, J.; Bartus, S.; Dragan, J.; Zasada, W.; Tokarek, T.; Kułaga, T.; et al. Borderline trend towards long-term mortality benefit from drug eluting stents implantation in ST-elevation myocardial infarction patients in Poland-data from NRDES registry. Catheter. Cardiovasc. Interv. 2014, 83, 436–442. [Google Scholar] [CrossRef] [PubMed]
- Burt, B.M.; ElBardissi, A.W.; Huckman, R.S.; Cohn, L.C.; Cevasco, M.W.; Rawn, J.D.; Aranki, S.F.; Byrne, J.G. Influence of experience and the surgical learning curve on long-term patient outcomes in cardiac surgery. J. Thorac. Cardiovasc. Surg. 2015, 150, 1061–1068.e3. [Google Scholar] [CrossRef] [PubMed]
- Burt, B.M.; ElBardissi, A.W.; Huckman, R.S.; Cohn, L.H.; Cevasco, M.W.; Rawn, J.D.; Aranki, S.F.; Byrne, J.G. Exercise-Based Cardiac Rehabilitation for Coronary Heart Disease: Cochrane Systematic Review and Meta-Analysis. J. Am. Coll. Cardiol. 2016, 67, 1061–1068. [Google Scholar]
- Prescott, E.; Eser, P.; Mikkelsen, N.; Holdgaard, A.; Marcin, T.; Wilhelm, M.; Gil, C.P.; González-Juanatey, J.R.; Moatemri, F.; Iliou, M.C.; et al. Cardiac rehabilitation of elderly patients in eight rehabilitation units in western Europe: Outcome data from the EU-CaRE multi-centre observational study. Eur. J. Prev. Cardiol. 2020, 27, 2047487320903869. [Google Scholar] [CrossRef]
- Driscoll, A.; Hinde, S.; Harrison, A.; Bojke, L.; Doherty, P. Estimating the health loss due to poor engagement with cardiac rehabilitation in Australia. Int. J. Cardiol. 2020, 317, 7–12. [Google Scholar] [CrossRef]
- Al Quait, A.; Doherty, P.; Gutacker, N.; Mills, J. In the modern era of percutaneous coronary intervention: Is cardiac rehabilitation engagement purely a patient or a service level decision? Eur. J. Prev. Cardiol. 2017, 24, 1351–1357. [Google Scholar] [CrossRef][Green Version]
- Jankowski, P.; Czarnecka, D.; Łysek, R.; Skrzek, A.; Smaś-Suska, M.; Mazurek, A.; Brzozowska-Kiszka, M.; Wolfshaut-Wolak, R.; Surowiec, S.; Bogacki, P.; et al. Secondary prevention in patients after hospitalization due to coronary artery disease: What has changed since 2006? Kardiol. Pol. 2014, 72, 355–362. [Google Scholar] [CrossRef]
- Perk, J.; Hambraeus, K.; Burell, G.; Carlsson, R.; Johansson, P.; Lisspers, J. Study of Patient Information after percutaneous Coronary Intervention (SPICI): Should prevention programmes become more effective? EuroIntervention 2015, 10, e1–e7. [Google Scholar] [CrossRef] [PubMed]
- Hansen, D.; Dendale, P.; Leenders, M.; Berger, J.; Raskin, A.; Vaes, J.; Meeusen, R. Reduction of cardiovascular event rate: Different effects of cardiac rehabilitation in CABG and PCI patients. Acta Cardiol. 2009, 64, 639–644. [Google Scholar] [CrossRef] [PubMed]
- Griffo, R.; Ambrosetti, M.; Tramarin, R.; Fattirolli, F.; Temporelli, P.L.; Vestri, A.R.; De Feo, S.; Tavazzi, L.; for the ICAROS investigators. Effective secondary prevention through cardiac rehabilitation after coronary revascularization and predictors of poor adherence to lifestyle modification and medication. Results of the ICAROS Survey. Int. J. Cardiol. 2013, 167, 1390–1395. [Google Scholar] [CrossRef] [PubMed]
- Redfern, J.; Briffa, T.; Ellis, E.; Freedman, S.B. Choice of secondary prevention improves risk factors after acute coronary syndrome: 1-year follow-up of the CHOICE (Choice of Health Options In prevention of Cardiovascular Events) randomised controlled trial. Heart 2009, 95, 468–475. [Google Scholar] [CrossRef] [PubMed]
- Kochiadakis, G. Cardiac rehabilitation: The discrepancy between level of recommendation and utilization. Hellenic. J. Cardiol. 2019, 60, 66–67. [Google Scholar] [CrossRef]
- Orth-Gomér, K.; Deter, H.-C.; Grün, A.-S.; Herrmann-Lingen, C.; Albus, C.; Bosbach, A.; Ladwig, K.-H.; Ronel, J.; Söllner, W.; de Zwaan, M.; et al. Socioeconomic factors in coronary artery disease—Results from the SPIRR-CAD study. J. Psychosom. Res. 2018, 105, 125–131. [Google Scholar] [CrossRef]
- Roth, C.; Berger, R.; Kuhn, M. The role of the socio-economic environment on medical outcomes after ST-segment elevation myocardial infarction. BMC Public Health 2019, 19, 630. [Google Scholar] [CrossRef]
- Gentz, C.A. Perceived learning needs of the patient undergoing coronary angioplasty: An integrative review of the literature. Heart Lung 2000, 29, 161–172. [Google Scholar] [CrossRef]
- Álvarez-Álvarez, I.; Martínez-González, M.Á.; Sánchez-Tainta, A.; Corella, D.; Díaz-López, A.; Fitó, M.; Vioque, J.; Romaguera, D.; Martínez, J.A.; Wärnberg, J.; et al. Adherence to an Energy-restricted Mediterranean Diet Score and Prevalence of Cardiovascular Risk Factors in the PREDIMED-Plus: A Cross-sectional Study. Rev. Esp. Cardiol. 2019, 72, 925–934. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).