International Overview of Somatic Dysfunction Assessment and Treatment in Osteopathic Research: A Scoping Review
Abstract
:1. Introduction
2. Materials and Methods
Registration and Reporting
3. Results
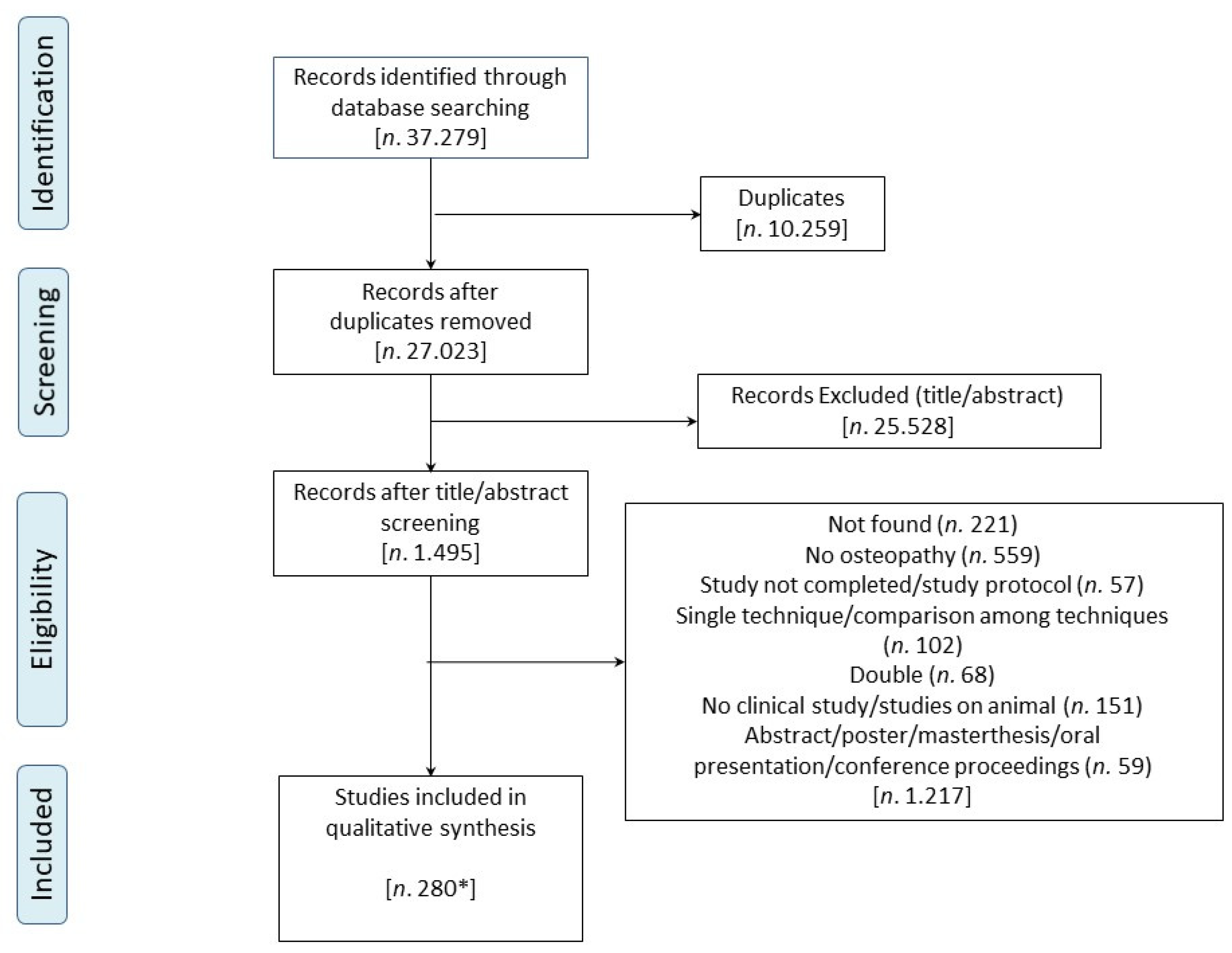
3.1. Study Selection
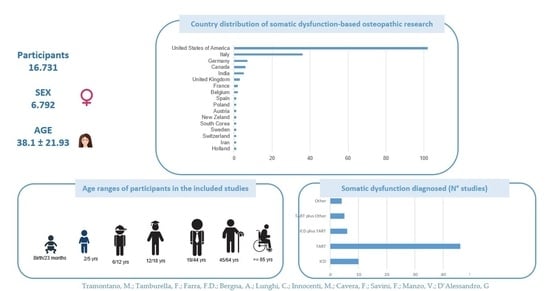
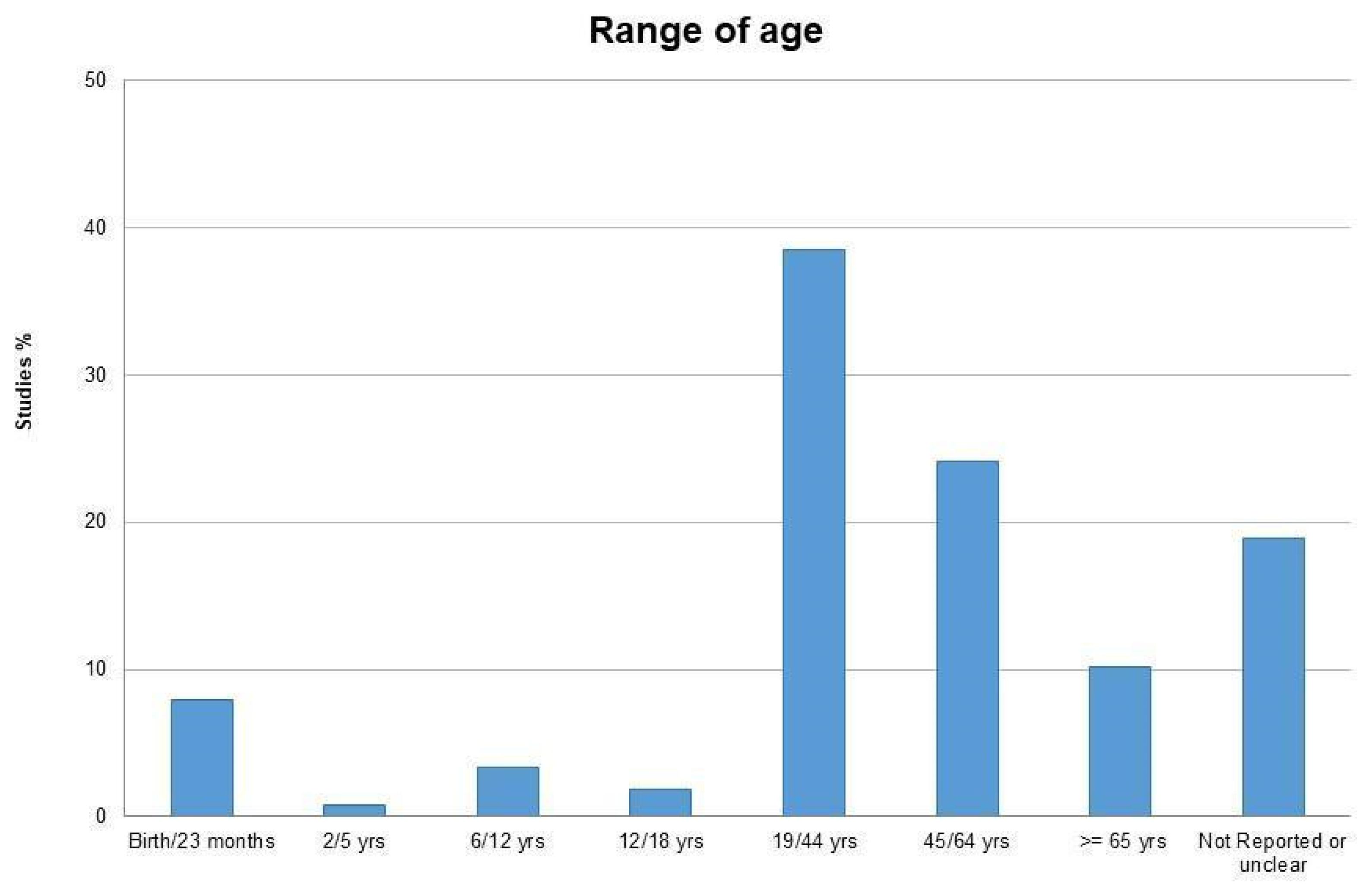
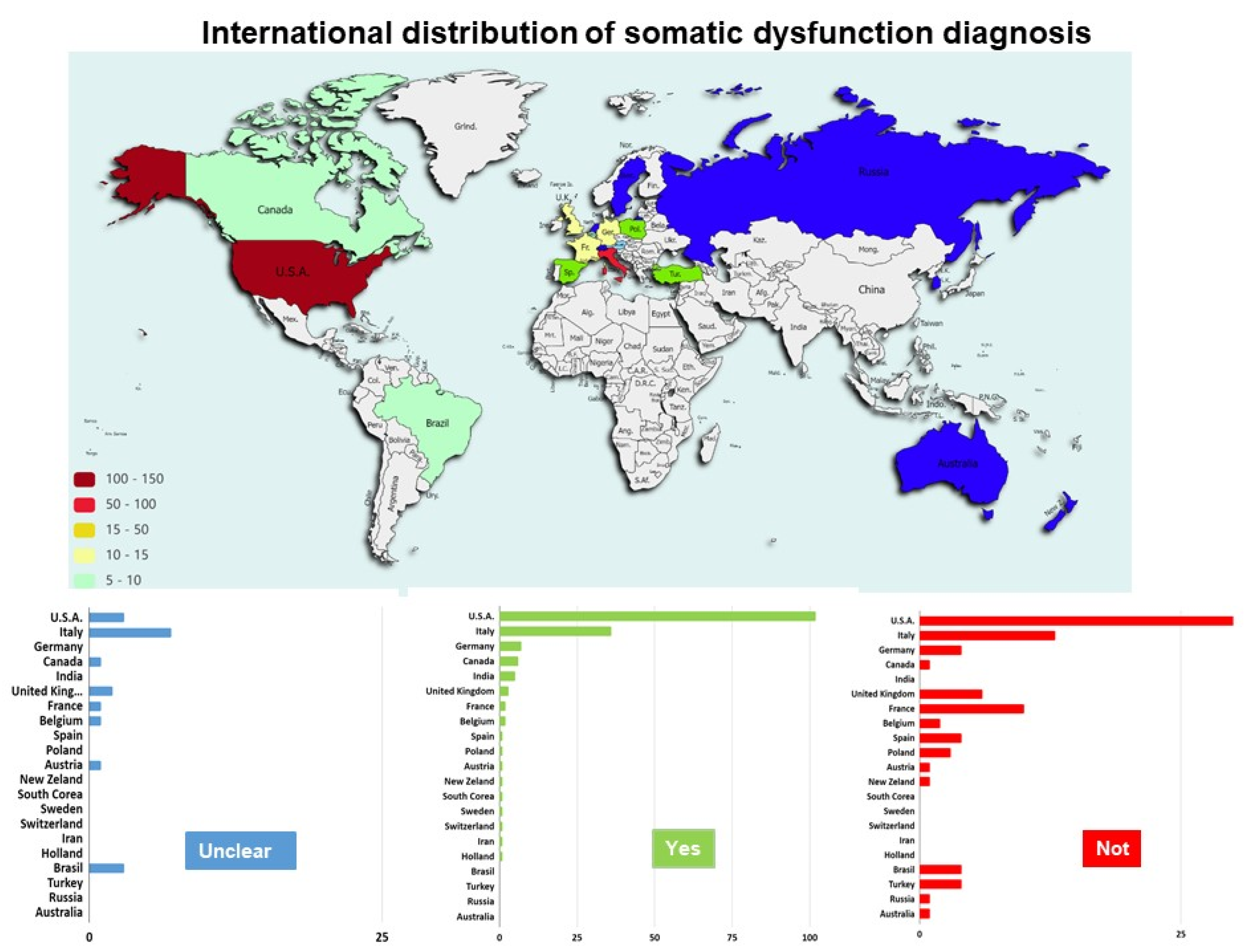
3.2. Characteristics of the Included Studies
3.3. Data Synthesis
3.3.1. Somatic Dysfunction in the Assessment
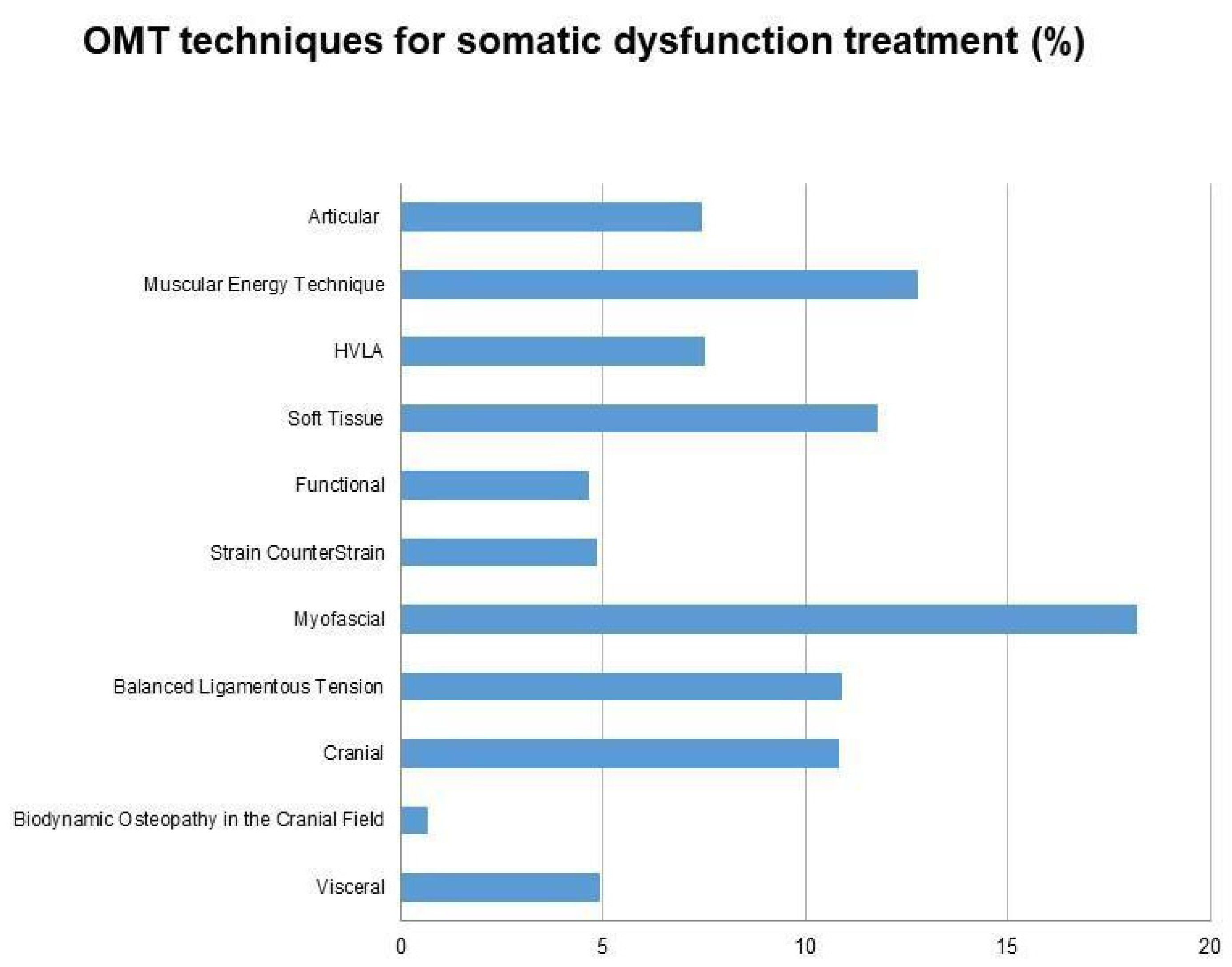
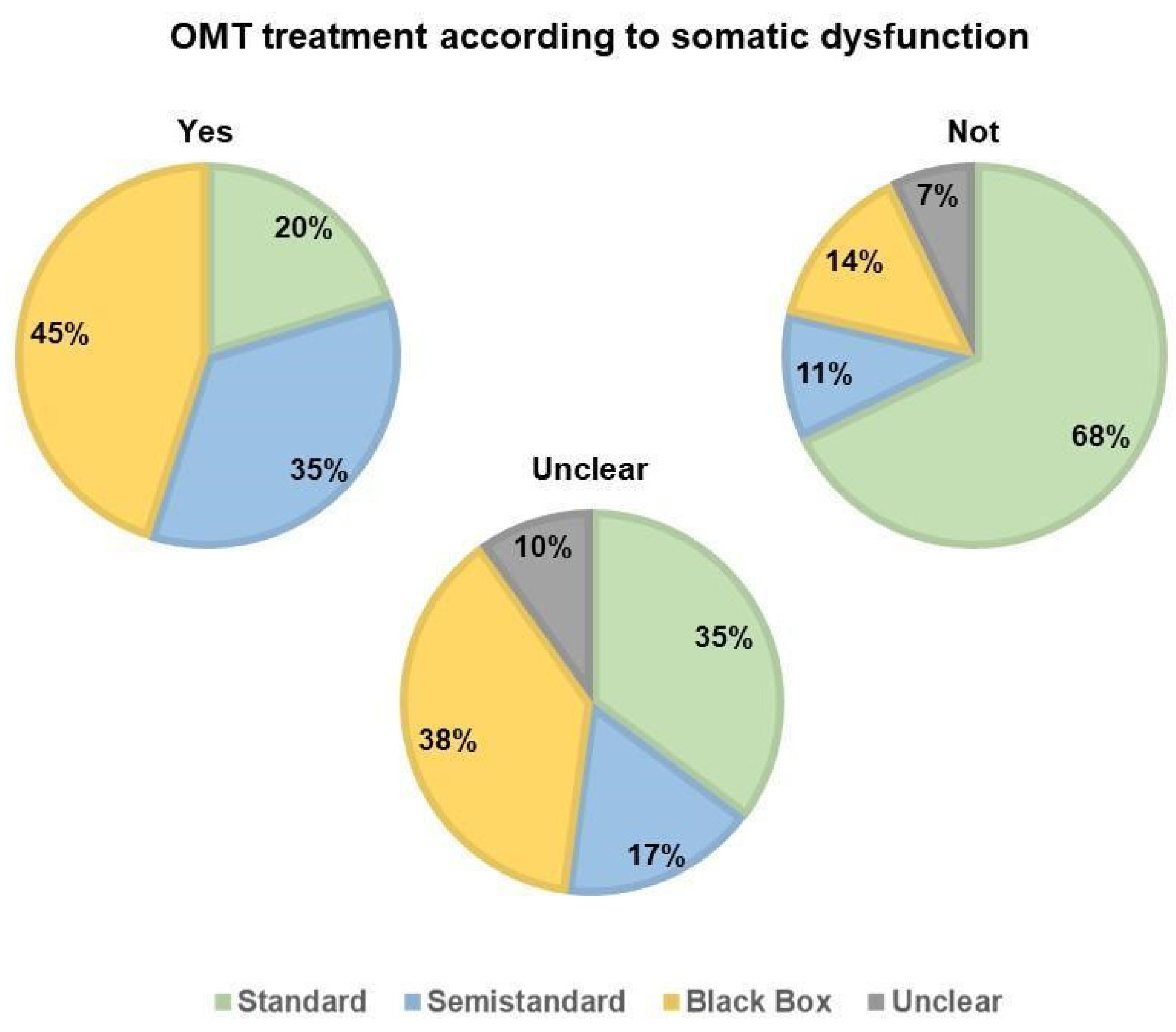
3.3.2. Somatic Dysfunction in the Treatment
3.3.3. Somatic Dysfunction in the Time Frame of Treatment
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Baroni, F.; Tramontano, M.; Barsotti, N.; Chiera, M.; Lanaro, D.; Lunghi, C. Osteopathic structure/function models renovation for a person-centered approach: A narrative review and integrative hypothesis. J. Complement. Integr. Med. 2021. [Google Scholar] [CrossRef]
- Hruby, R.T.P.; Lunghi, C.; Fusco, G. The five osteopathic models: Rational, Application, Integration. In From Tradition to Innovation for a Centered Person Osteopathy; Handspring Publishing: Pencaitland, UK, 2017. [Google Scholar]
- Osteopathic International Alliance. Osteopathic Healthcare. Available online: https://oialliance.org/wp-content/uploads/2021/02/OIA_Report_2020_FINAL.pdf (accessed on 6 December 2021).
- Mahlberg, S.J.; Liou, Y.L.; Lloyd, J. Establishing osteopathic assessments to fulfill osteopathic recognition standards: A model for dermatology and other subspecialties. J. Osteopath. Med. 2021, 121, 739–745. [Google Scholar] [CrossRef] [PubMed]
- Sciomachen, P.; Arienti, C.; Bergna, A.; Castagna, C.; Consorti, G.; Lotti, A.; Lunghi, C.; Tramontano, M.; Longobardi, M. Core competencies in osteopathy: Italian register of osteopaths proposal. Int. J. Osteopath. Med. 2018, 27, 1–5. [Google Scholar] [CrossRef] [Green Version]
- Morin, C.; Gaboury, I. Osteopathic empirical research: A bibliometric analysis from 1966 to 2018. BMC Complement. Med. Ther. 2021, 21, 196. [Google Scholar] [CrossRef] [PubMed]
- Licciardone, J.; Gatchel, R.J.; Aryal, S. Recovery from Chronic Low Back Pain after Osteopathic Manipulative Treatment: A Randomized Controlled Trial. J. Am. Osteopath. Assoc. 2016, 116, 144–155. [Google Scholar] [CrossRef] [Green Version]
- Task Force on the Low Back Pain Clinical Practice Guidelines. American Osteopathic Association Guidelines for Osteopathic Manipulative Treatment (OMT) for Patients with Low Back Pain. J. Am. Osteopath. Assoc. 2016, 116, 536–549. [Google Scholar] [CrossRef] [Green Version]
- Ruffini, N.; D’Alessandro, G.; Cardinali, L.; Frondaroli, F.; Cerritelli, F. Osteopathic manipulative treatment in gynaecology and obstetrics: A systematic review. Complement. Ther. Med. 2016, 26, 72–78. [Google Scholar] [CrossRef]
- D’Ippolito, M.; Tramontano, M.; Buzzi, M.G. Effects of Osteopathic Manipulative Therapy on Pain and Mood Disorders in Patients With High-Frequency Migraine. J. Am. Osteopath. Assoc. 2017, 117, 365–369. [Google Scholar] [CrossRef] [Green Version]
- Lanaro, D.; Ruffini, N.; Manzotti, A.; Lista, G. Osteopathic manipulative treatment showed reduction of length of stay and costs in preterm infants: A systematic review and meta-analysis. Medicine 2017, 96, e6408. [Google Scholar] [CrossRef]
- Cerritelli, F.; Cicchitti, L.; Martelli, M.; Barlafante, G.; Renzetti, C.; Pizzolorusso, G.; Lupacchini, M.; D’Orazio, M.; Marinelli, B.; Cozzolino, V.; et al. Osteopathic manipulative treatment and pain in preterms: Study protocol for a randomised controlled trial. Trials 2015, 16, 84. [Google Scholar] [CrossRef] [Green Version]
- Fornari, M.; Carnevali, L.; Sgoifo, A. Single Osteopathic Manipulative Therapy Session Dampens Acute Autonomic and Neuroendocrine Responses to Mental Stress in Healthy Male Participants. J. Am. Osteopath. Assoc. 2017, 117, 559–567. [Google Scholar] [CrossRef] [Green Version]
- Tamburella, F.; Piras, F.; Piras, F.; Spanò, B.; Tramontano, M.; Gili, T. Cerebral Perfusion Changes after Osteopathic Manipulative Treatment: A Randomized Manual Placebo-Controlled Trial. Front. Physiol. 2019, 10, 403. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ponzo, V.; Cinnera, A.M.; Mommo, F.; Caltagirone, C.; Koch, G.; Tramontano, M. Osteopathic Manipulative Therapy Potentiates Motor Cortical Plasticity. J. Am. Osteopath. Assoc. 2018, 118, 396–402. [Google Scholar] [CrossRef] [PubMed]
- Tramontano, M.; Cerritelli, F.; Piras, F.; Spanò, B.; Tamburella, F.; Piras, F.; Caltagirone, C.; Gili, T. Brain Connectivity Changes after Osteopathic Manipulative Treatment: A Randomized Manual Placebo-Controlled Trial. Brain Sci. 2020, 10, 969. [Google Scholar] [CrossRef] [PubMed]
- Cerritelli, F.; Chiacchiaretta, P.; Gambi, F.; Perrucci, M.G.; Barassi, G.; Visciano, C.; Bellomo, R.G.; Saggini, R.; Ferretti, A. Effect of manual approaches with osteopathic modality on brain correlates of interoception: An fMRI study. Sci. Rep. 2020, 10, 3214. [Google Scholar] [CrossRef] [Green Version]
- Henley, C.E.; Ivins, D.; Mills, M.; Wen, F.K.; Benjamin, B.A. Osteopathic manipulative treatment and its relationship to autonomic nervous system activity as demonstrated by heart rate variability: A repeated measures study. Osteopath. Med. Prim. Care 2008, 2, 7. [Google Scholar] [CrossRef] [Green Version]
- Budgell, B.; Hirano, F. Innocuous mechanical stimulation of the neck and alterations in heart-rate variability in healthy young adults. Auton. Neurosci. 2001, 91, 96–99. [Google Scholar] [CrossRef]
- Budgell, B.; Polus, B. The effects of thoracic manipulation on heart rate variability: A controlled crossover trial. J. Manip. Physiol. Ther. 2006, 29, 603–610. [Google Scholar] [CrossRef]
- World Health Organization. International Statistical Classification of Diseases and Related Health Problems 10th Revision. Available online: https://www.who.int/classifications/icd/ICD10Volume2_en_2010.pdf (accessed on 15 November 2021).
- Lunghi, C.; Tozzi, P.; Fusco, G. The biomechanical model in manual therapy: Is there an ongoing crisis or just the need to revise the underlying concept and application? J. Bodyw. Mov. Ther. 2016, 20, 784–799. [Google Scholar] [CrossRef]
- Licciardone, J.C.; Nelson, K.E.; Glonek, T.; Sleszynski, S.L.; Cruser, D.A. Osteopathic manipulative treatment of somatic dysfunction among patients in the family practice clinic setting: A retrospective analysis. J. Am. Osteopath. Assoc. 2005, 105, 537–544. [Google Scholar]
- Baroni, F.; Ruffini, N.; D’Alessandro, G.; Consorti, G.; Lunghi, C. The role of touch in osteopathic practice: A narrative review and integrative hypothesis. Complement. Ther. Clin. Pract. 2021, 42, 101277. [Google Scholar] [CrossRef] [PubMed]
- Tramontano, M.; Pagnotta, S.; Lunghi, C.; Manzo, C.; Manzo, F.; Consolo, S.; Manzo, V. Assessment and Management of Somatic Dysfunctions in Patients With Patellofemoral Pain Syndrome. J. Am. Osteopath. Assoc. 2020, 120, 165–173. [Google Scholar] [CrossRef]
- Esteves, J.E.; Zegarra-Parodi, R.; van Dun, P.; Cerritelli, F.; Vaucher, P. Models and theoretical frameworks for osteopathic care—A critical view and call for updates and research. Int. J. Osteopath. Med. 2020, 35, 1–4. [Google Scholar] [CrossRef] [Green Version]
- Lunghi, C.; Liem, T. Models and theoretical frameworks for osteopathic care—A critical view and call for updates and research. Int. J. Osteopath. Med. 2020, 37, 48–51. [Google Scholar] [CrossRef]
- Alvarez, G.; Van Biesen, T.; Roura, S. Professional identity in the evolution of osteopathic models: Response to Esteves et al. Int. J. Osteopath. Med. 2020, 36, 58–59. [Google Scholar] [CrossRef]
- Steel, A.; Foley, H.; Redmond, R. Person-centred care and traditional philosophies in the evolution of osteopathic models and theoretical frameworks: Response to Esteves et al. Int. J. Osteopath. Med. 2020, 35, 60–61. [Google Scholar] [CrossRef]
- Sampath, K.K.; Fairs, E. A piece of the puzzle: Response to Esteves et al. Int. J. Osteopath. Med. 2020, 38, 39–40. [Google Scholar] [CrossRef]
- Noy, M.; Macedo, L.; Carlesso, L. Biomedical origins of the term ’osteopathic lesion’ and its impact on people in pain. Int. J. Osteopath. Med. 2020, 37, 40–43. [Google Scholar] [CrossRef]
- Bergna, A.; Vismara, L.; Parravicini, G.; Dal Farra, F. A new perspective for Somatic Dysfunction in Osteopathy: The Variability Model. J. Bodyw. Mov. Ther. 2020, 24, 181–189. [Google Scholar] [CrossRef]
- Moran, R. Somatic dysfunction–Conceptually fascinating, but does it help us address health needs? Int. J. Osteopath. Med. 2016, 16, 1–2. [Google Scholar] [CrossRef] [Green Version]
- Peters, M.D.J.; Godfrey, C.; McInerney, P.; Munn, Z.; Tricco, A.C.; Khalil, H. Chapter 11: Scoping Reviews (2020 version). In JBI Manual for Evidence Synthesis; Aromataris, E., Munn, Z., Eds.; JBI: Adelaide, Australia, 2020; Available online: https://synthesismanual.jbi.global (accessed on 15 November 2021).
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Available online: http://www.zotero.org (accessed on 15 November 2021).
- Osteopathic International Alliance. Osteopathy and Osteopathic Medicine. Available online: https://oialliance.org/wp-content/uploads/2014/01/OIA-Stage-2-Report.pdf (accessed on 15 November 2021).
- American Association of Colleges of Osteopathic Medicine. Osteopathic Core Competencies for Medical Students. Available online: https://www.aacom.org/docs/default-source/core-competencies/corecompetencyreport2012.pdf?sfvrsn=4 (accessed on 15 November 2021).
- Gazzetta Ufficiale Della Repubblica Italiana (G.U.) Anno 159°—Numero 25. 3 Gennaio 2018; p. 10. Available online: https://www.gazzettaufficiale.it/eli/gu/2018/01/31/25/sg/%20pdf (accessed on 15 November 2021).
- General Osteopathic Council. Osteopathic Practice Standard. Available online: https://standards.osteopathy.org.uk/ (accessed on 15 November 2021).
- Sleszynski, S.L.; Glonek, T. Outpatient Osteopathic SOAP Note Form: Preliminary results in osteopathic outcomes-based research. J. Am. Osteopath. Assoc. 2005, 105, 181–205. [Google Scholar] [PubMed]
- Giusti, R. Glossary of Osteopathic Terminology. Third Edition. Available online: https://www.aacom.org/docs/default-source/default-document-library/glossary2017.pdf?sfvrsn=a41c3b97_6 (accessed on 15 November 2021).
- Nesi, J. Models and theoretical frameworks for osteopathic care—A critical view from a non regulated country. Int. J. Osteopath. Med. 2020, 36, 62–63. [Google Scholar] [CrossRef]
- Ménard, M.; Draper-Rodi, J.; Merdy, O.; Wagner, A.; Tavernier, P.; Jacquot, E.; Mhadhbi, H. Finding a way between osteopathic principles and evidence-based practices: Response to Esteves et al. Int. J. Osteopath. Med. 2020, 37, 45–47. [Google Scholar] [CrossRef]
- Bettelli, L.; Pisa, V.; Formica, A. “I do it my way”-Italian osteopaths’ beliefs and attitudes about five osteopathic models: A qualitative study. Int. J. Osteopath. Med. 2020, 38, 57–64. [Google Scholar] [CrossRef]
- Santiago, R.; Campos, B.; Moita, J.; Nunes, A. Response to: Models and theoretical frameworks for osteopathic care-A critical view and call for updates and research. Int. J. Osteopath. Med. 2020, 37, 52–53. [Google Scholar] [CrossRef]
- Vogel, S. Continuing debates about models of practice. Int. J. Osteopath. Med. 2020, 37, 1–2. [Google Scholar] [CrossRef]
- Thomson, O.P.; Petty, N.J.; Moore, A.P. Reconsidering the patient-centeredness of osteopathy. Int. J. Osteopath. Med. 2013, 16, 25–32. [Google Scholar] [CrossRef] [Green Version]
- Lunghi, C.; Baroni, F. Cynefin Framework for Evidence-Informed Clinical Reasoning and Decision-Making. J. Am. Osteopath. Assoc. 2019, 119, 312–321. [Google Scholar] [CrossRef]
- Liem, T.; Lunghi, C. Reconceptualizing Principles and Models in Osteopathic Care: A Clinical Application of the Integral Theory. Altern. Ther. Health Med. 2021, AT6750, epub ahead of print. [Google Scholar]
- Castagna, C.; Consorti, G.; Turinetto, M.; Lunghi, C. Osteopathic Models Integration Radar Plot: A Proposed Framework for Osteopathic Diagnostic Clinical Reasoning. J. Chiropr. Humanit. 2021, 28, 49–59. [Google Scholar] [CrossRef]
- Gasperini, M.; Vanacore, N.; Massimi, L.; Consolo, S.; Haass, C.; Scapillati, M.E.; Petracca, M. Effects of osteopathic approach in infants with deformational plagiocephaly: An outcome research study. Minerva Pediatr. (Torino) 2021. [Google Scholar] [CrossRef] [PubMed]
- Tramontano, M.; Consorti, G.; Morone, G.; Lunghi, C. Vertigo and Balance Disorders—The Role of Osteopathic Manipulative Treatment: A Systematic Review. Schwindel und Gleichgewichtsstörungen. Complement. Med. Res. 2021, 28, 368–377. [Google Scholar] [CrossRef]
- Tramontano, M.; Martino Cinnera, A.; Petracca, M.; Gaeta, A.; Tamburella, F.; Audouard, M.; Caltagirone, C. Outpatient Satisfaction With Osteopathic Manipulative Treatment in a Hospital Center: A Survey. Altern. Ther. Health Med. 2018, 24, 18–24. [Google Scholar] [PubMed]
- Lunghi, C.; Iacopini, A.; Baroni, F.; Consorti, G.; Cerritelli, F. Thematic Analysis of Attitudes Held by a Group of Italian Osteopaths Toward Osteopathic Evaluation, Treatment, and Management in the Neonatal and Pediatric Field: A Qualitative Study. J. Manip. Physiol. Ther. 2021, 44, 164–175. [Google Scholar] [CrossRef]
- Dal Farra, F.; Risio, R.G.; Vismara, L.; Bergna, A. Effectiveness of osteopathic interventions in chronic non-specific low back pain: A systematic review and meta-analysis. Complement. Ther. Med. 2021, 56, 102616. [Google Scholar] [CrossRef]
- Lunghi, C.; Consorti, G.; Tramontano, M.; Esteves, J.E.; Cerritelli, F. Perspectives on tissue adaptation related to allostatic load: Scoping review and integrative hypothesis with a focus on osteopathic palpation. J. Bodyw. Mov. Ther. 2020, 24, 212–220. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, T.C.; Glasziou, P.P.; Boutron, I.; Milne, R.; Perera, R.; Moher, D.; Altman, D.G.; Barbour, V.; Macdonald, H.; Johnston, M.; et al. Better reporting of interventions: Template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014, 348, 1687. [Google Scholar] [CrossRef] [Green Version]
- Alvarez, G.; Cerritelli, F.; Urrutia, G. Using the template for intervention description and replication (TIDieR) as a tool for improving the design and reporting of manual therapy interventions. Man. Ther. 2016, 24, 85–89. [Google Scholar] [CrossRef]
- Mintken, P.E.; DeRosa, C.; Little, T.; Smith, B. A Model for Standardizing Manipulation Terminology in Physical Therapy Practice. J. Man. Manip. Ther. 2008, 16, 50–56. [Google Scholar] [CrossRef]
- Chaitow, L. Can we describe what we do? J. Bodyw. Mov. Ther. 2014, 18, 315–316. [Google Scholar] [CrossRef] [PubMed] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tramontano, M.; Tamburella, F.; Dal Farra, F.; Bergna, A.; Lunghi, C.; Innocenti, M.; Cavera, F.; Savini, F.; Manzo, V.; D’Alessandro, G. International Overview of Somatic Dysfunction Assessment and Treatment in Osteopathic Research: A Scoping Review. Healthcare 2022, 10, 28. https://doi.org/10.3390/healthcare10010028
Tramontano M, Tamburella F, Dal Farra F, Bergna A, Lunghi C, Innocenti M, Cavera F, Savini F, Manzo V, D’Alessandro G. International Overview of Somatic Dysfunction Assessment and Treatment in Osteopathic Research: A Scoping Review. Healthcare. 2022; 10(1):28. https://doi.org/10.3390/healthcare10010028
Chicago/Turabian StyleTramontano, Marco, Federica Tamburella, Fulvio Dal Farra, Andrea Bergna, Christian Lunghi, Mattia Innocenti, Fabio Cavera, Federica Savini, Vincenzo Manzo, and Giandomenico D’Alessandro. 2022. "International Overview of Somatic Dysfunction Assessment and Treatment in Osteopathic Research: A Scoping Review" Healthcare 10, no. 1: 28. https://doi.org/10.3390/healthcare10010028
APA StyleTramontano, M., Tamburella, F., Dal Farra, F., Bergna, A., Lunghi, C., Innocenti, M., Cavera, F., Savini, F., Manzo, V., & D’Alessandro, G. (2022). International Overview of Somatic Dysfunction Assessment and Treatment in Osteopathic Research: A Scoping Review. Healthcare, 10(1), 28. https://doi.org/10.3390/healthcare10010028