Modeling of Fundus Laser Exposure for Estimating Safe Laser Coagulation Parameters in the Treatment of Diabetic Retinopathy
Abstract
:1. Introduction
2. Materials and Methods
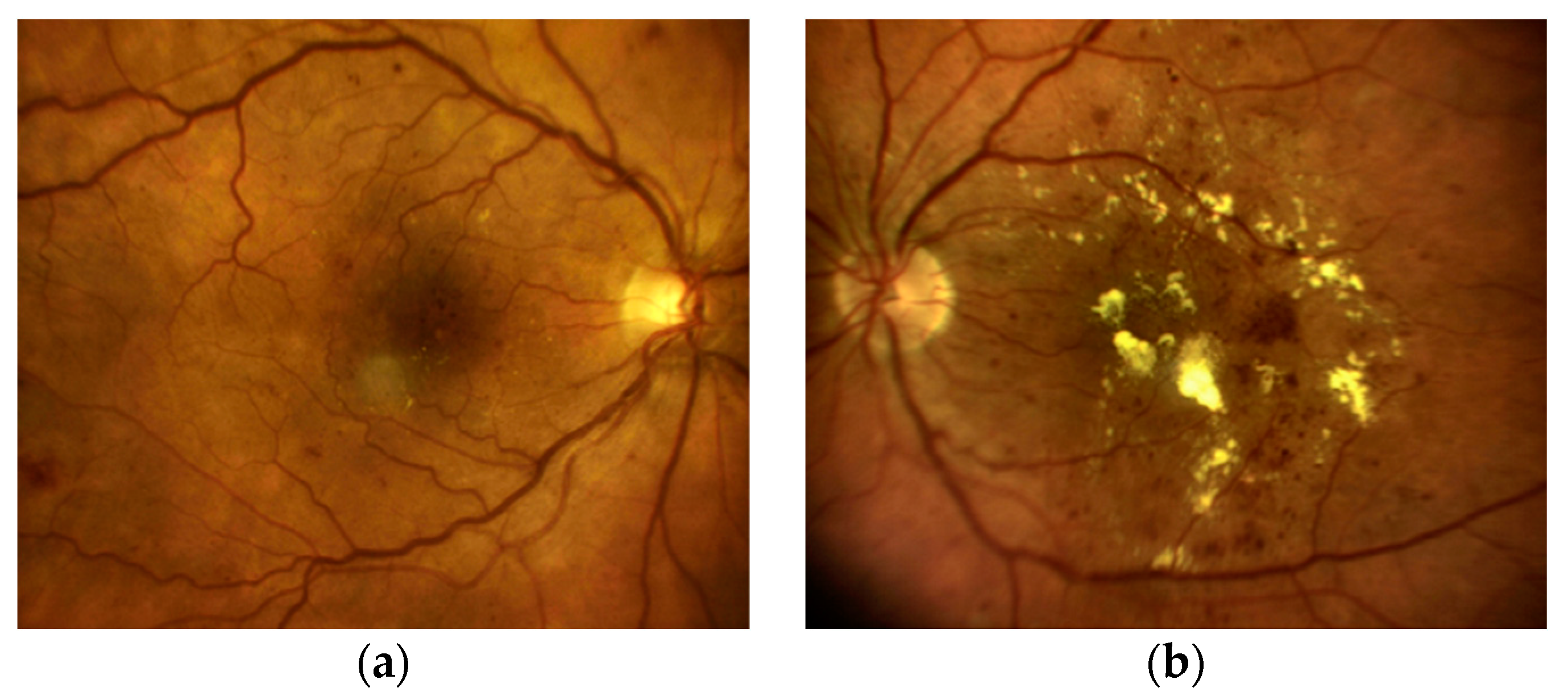
2.1. Research Material
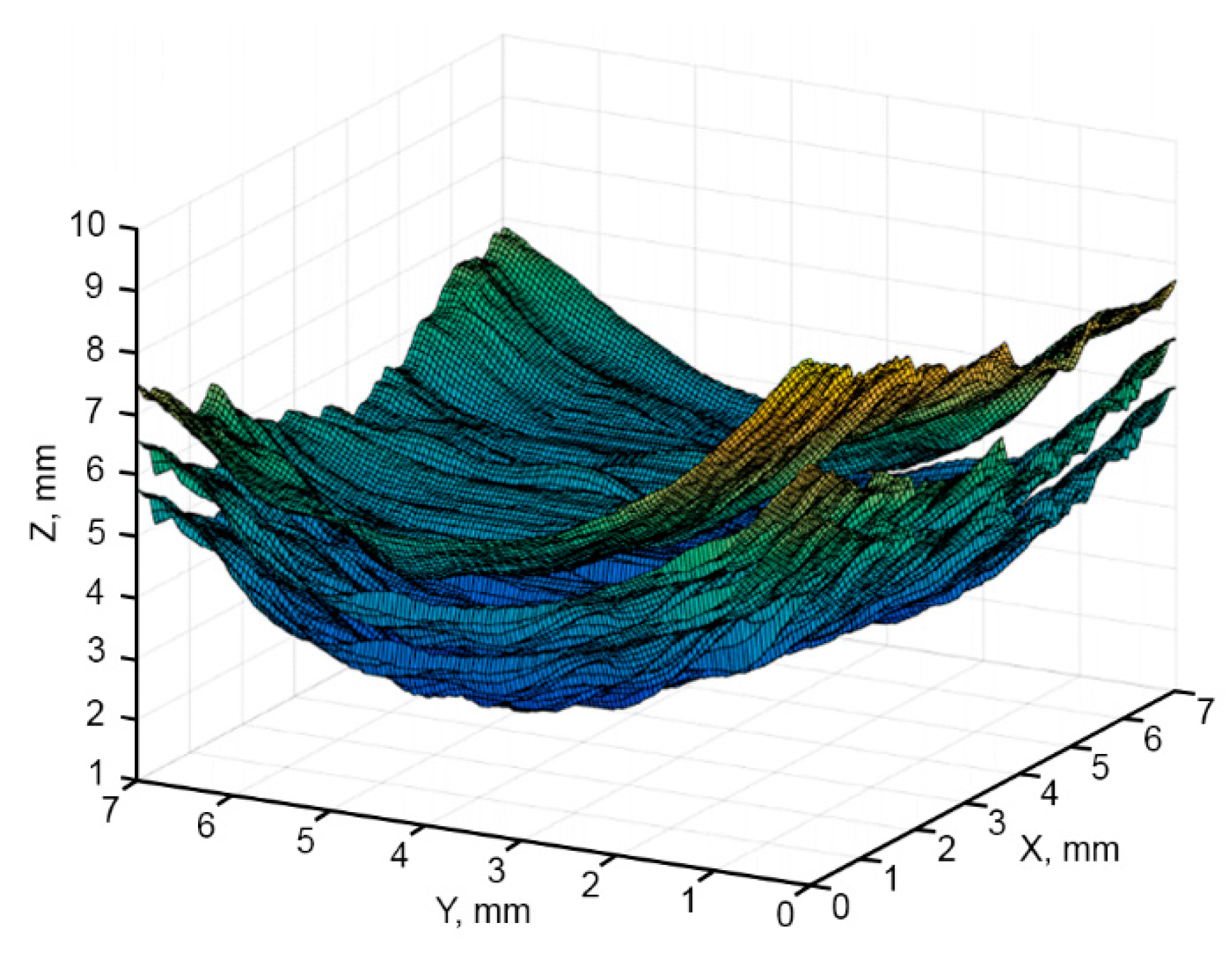
2.2. OCT Image Analysis and Reconstruction of 3D Fundus Structure Model
- Step 1. Constructing a halftone image.
- Step 2. Detection of the contour lines of the retina.
- Step 3. Selection of a group of points located on contour lines.
- Step 4. Approximation of contour lines through selected points.
- Step 5. Construction of the image with selected layers based on smoothed contour lines.
2.3. Heat Propagation Modeling
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lipatov, D.V.; Smirnova, N.B.; Aleksandrova, V.K. Modern algorithm for laser coagulation of the retina in diabetic retinopathy. Diabetes Mellit. 2007, 3, 45–46. [Google Scholar] [CrossRef] [Green Version]
- Gafurov, S.D.; Katakhonov, S.M.; Holmonov, M.M. Features of the use of lasers in medicine. Eur. Sci. 2019, 3, 92–95. [Google Scholar]
- Zamytsky, E.A.; Zolotarev, A.V.; Karlova, E.V.; Zamytsky, P.A. Analysis of the intensity of coagulates in laser treatment of diabetic macular edema using a robotic laser Navilas. Saratov. J. Med. Sci. Res. 2017, 13, 375–378. [Google Scholar]
- Kotsur, T.V.; Izmailov, A.S. The effectiveness of laser coagulation in the macula and high-density microphotocoagulation in the treatment of diabetic maculopathy. Ophthalmol. Stat. 2016, 9, 43–45. [Google Scholar] [CrossRef] [Green Version]
- Kozak, I.; Luttrull, J.K. Modern retinal laser therapy. Saudi J. Ophthalmol. 2015, 29, 137–146. [Google Scholar] [CrossRef]
- Chhablani, J.; Kozak, I.; Barteselli, G.; El-Emam, S. A novel navigated laser system brings new efficacy to the treatment of retinovascular disorders. Oman J. Ophthalmol. 2013, 6, 18–22. [Google Scholar] [CrossRef]
- Shirokanev, A.S.; Kirsh, D.V.; Ilyasova, N.Y.; Kupriyanov, A.V. Investigation of algorithms for placing coagulates on the fundus image. Comput. Opt. 2018, 42, 712–721. [Google Scholar] [CrossRef]
- Ilyasova, N.Y.; Shirokanev, A.S.; Kupriynov, A.V.; Paringer, R.A. Technology of intellectual feature selection for a system of automatic formation of a coagulate plan on retina. Comput. Opt. 2019, 43, 304–315. [Google Scholar] [CrossRef]
- Mukhin, A.; Kilbas, I.; Paringer, R.; Ilyasova, N. Application of the gradient descent for data balancing in diagnostic image analysis problems. In Proceedings of the IEEE Xplore, 2020 International Conference on Information Technology and Nanotechnology (ITNT), Samara, Russia, 26–29 May 2020; pp. 1–4. [Google Scholar] [CrossRef]
- Ilyasova, N.Yu.; Demin, N.S.; Shirokanev, A.S.; Kupriyanov, A.V.; Zamytskiy, E.A. Method for selection macular edema region using optical coherence tomography data. Comput. Opt. 2020, 44, 250–258. [Google Scholar] [CrossRef]
- Andriyanov, N.A.; Dementiev, V.E. Developing and studying the algorithm for segmentation of simple images using detectors based on doubly stochastic random fields. Pattern Recognit. Image Anal. 2019, 29, 1–9. [Google Scholar] [CrossRef]
- Shirokanev, A.S.; Kibitkina, A.S.; Ilyasova, N.Y.; Degtyarev, A.A. Methods of mathematical modeling of fundus laser exposure for therapeutic effect evaluation. Comput. Opt. 2020, 44, 809–820. [Google Scholar] [CrossRef]
- Fiandono, I.; Firdausy, K. Median filtering for optic disc segmentation in retinal image. Kinetik 2018, 3, 75–82. [Google Scholar] [CrossRef]
- Joon, H.L.; Joonseok, L.; Sooah, C.; Ji, E.S.; Minyoung, L.; Sung, H.K.; Jin, Y.L.; Dae, H.S.; Joon, M.K.; Jung, H.B.; et al. Development of decision support software for deep learning-based automated retinal disease screening using relatively limited fundus photograph data. Electronics 2021, 10, 163. [Google Scholar] [CrossRef]
- Arfan, G.; Chan, H.S.; Vaisakh, S.; Jahanzeb, A.; Raed, A.A. Accelerating retinal fundus image classification using artificial neural networks (ANNs) and reconfigurable hardware (FPGA). Electronics 2019, 8, 1522. [Google Scholar] [CrossRef] [Green Version]
- Ling, L.; Dingyu, X.; Xinglong, F. Automatic diabetic retinopathy grading via self-knowledge distillation. Electronics 2020, 9, 1337. [Google Scholar] [CrossRef]
- Jyostna, D.B.; Veeranjaneyulu, N.; Shaik, N.Sh.; Saqib, H.; Muhammad, B.; Praveen, K.; Reddy, M.; Ohyun, J. Blended multi-modal deep ConvNet features for diabetic retinopathy severity prediction. Electronics 2020, 9, 914. [Google Scholar] [CrossRef]
- Artemov, S.; Belyaev, A.; Bushukina, O.; Khrushchalina, S.; Kostin, S.; Lyapin, A.; Ryabochkina, P.; Taratynova, A. Endovenous laser coagulation using two-micron laser radiation: Mathematical modeling and in vivo experiments. In Proceedings of the International Conference on Advanced Laser Technologies (ALT), Prague, Czech Republic, 15–20 September 2019; Volume 19, pp. 14–21. [Google Scholar]
- Moutray, T.; Evans, J.R.; Lois, N.; Armstrong, D.J.; Peto, T.; Azuara-Blanco, A. Different lasers and techniques for proliferative diabetic retinopathy. Cochrane Database Syst. Rev. 2018, 3, 1–87. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Belucio-Neto, J.; De Oliveira, X.C.; De Oliveira, D.R.; Passos, R.M.; Maia, M.; Maia, A. Functional and anatomical outcomes in patients submitted to panretinal photocoagulation using 577nm multispot vs 532nm single-spot laser: A clinical trial. Investig. Ophthalmol. Vis. Sci. 2016, 57, 1–18. [Google Scholar]
- Ghassemi, F.; Ebrahimiadib, N.; Roohipoor, R.; Moghimi, S.; Alipour, F. Nerve fiber layer thickness in eyes treated with red versus green laser in proliferative diabetic retinopathy: Short-term results. Ophthalmologica 2013, 230, 195–200. [Google Scholar] [CrossRef]
- Inan, U.U.; Polat, O.; Inan, S.; Yigit, S.; Baysal, Z. Comparison of pain scores between patients undergoing panretinal photocoagulation using navigated or pattern scan laser systems. Arq. Bras. O1almol. 2016, 79, 8–15. [Google Scholar] [CrossRef] [Green Version]
- Zhang, S.; Cao, G.F.; Xu, X.Z.; Wang, C.H. Pattern scan laser versus single spot laser in panretinal photocoagulation treatment for proliferative diabetic retinopathy. Int. Eye Sci. 2017, 17, 205–208. [Google Scholar]
- Almutairi, M.; Zureigat, H.; Izani Ismail, A.; Fareed Jameel, A. Fuzzy numerical solution via finite difference scheme of wave equation in double parametrical fuzzy number form. Mathematics 2021, 9, 667. [Google Scholar] [CrossRef]
- Anuar, N.S.; Bachok, N.; Pop, I. Numerical computation of dusty hybrid nanofluid flow and heat transfer over a deformable sheet with slip fffect. Mathematics 2021, 9, 643. [Google Scholar] [CrossRef]
- Ahmad, F.; Almatroud, A.O.; Hussain, S.; Farooq, S.E.; Ullah, R. Numerical solution of nonlinear diff. equations for heat transfer in micropolar fluids over a stretching domain. Mathematics 2020, 8, 854. [Google Scholar] [CrossRef]
- Pak, J.M. Switching extended Kalman filter bank for indoor localization using wireless sensor networks. Electronics 2021, 10, 718. [Google Scholar] [CrossRef]
- Shirikanev, A.; Ilyasova, A.; Demin, N.S.; Zamyckij, E. Extracting a DME area based on graph-based image segmentation and collation of OCT retinal images. J. Phys. 2021, 1–9. [Google Scholar] [CrossRef]
- Kistenev, Y.; Buligin, A.; Sandykova, E.; Sim, E.; Vrazhnov, D. Modeling of IR laser radiation propagation in bio-tissues. In Proceedings of SPIE 2019; SPIE Press: Bellingham, WA, USA, 2019; Volume 11208, pp. 1–4. [Google Scholar]
- Samarsky, A.A. Schemes of the increased order of accuracy for the multidimensional heat conduction equation. J. Comput. Math. Math. Phys. 1963, 3, 812–840. [Google Scholar]
- Anufriev, I.E.; Osipov, P.A. Mathematical Methods for Modeling Physical Processes. Finite Difference Method. With Solutions of Typical Problems; St. Petersburg State Polytechnic University, Institute of Applied Mathematics and Mechanics: Saint Petersburg, Russia, 2014; pp. 1–282. [Google Scholar]
- Azima, Y.I. Use of the integro-interpolation method for construction of difference equations for determination of thermal properties and unsteady-state heat fluxes. Eng. Phys. Thermophys. 1998, 71, 795–802. [Google Scholar] [CrossRef]







| I | J | K | S | RMS |
|---|---|---|---|---|
| 60 | 200 | 500 | 1000 | 0.015130427 |
| 120 | 200 | 500 | 1000 | 0.002634052 |
| 240 | 200 | 500 | 1000 | 0.00050212 |
| 480 | 200 | 500 | 1000 | 0.000172598 |
| I | J | K | S | RMS |
|---|---|---|---|---|
| 200 | 60 | 500 | 1000 | 0.015772823 |
| 200 | 120 | 500 | 1000 | 0.003441242 |
| 200 | 240 | 500 | 1000 | 0.001191759 |
| 200 | 480 | 500 | 1000 | 0.000531296 |
| I | J | K | S | RMS |
|---|---|---|---|---|
| 200 | 200 | 60 | 1000 | 0.025006277 |
| 200 | 200 | 120 | 1000 | 0.004207547 |
| 200 | 200 | 240 | 1000 | 0.002474279 |
| 200 | 200 | 480 | 1000 | 0.001344305 |
| 200 | 200 | 960 | 1000 | 0.000694162 |
| I | J | K | S | RMS |
|---|---|---|---|---|
| 200 | 200 | 500 | 200 | 0.000323827 |
| 200 | 200 | 500 | 400 | 0.000186017 |
| 200 | 200 | 500 | 800 | 0.000103741 |
| 200 | 200 | 500 | 1600 | 0.00005.58805 |
| 200 | 200 | 500 | 3200 | 0.00002.92848 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shirokanev, A.; Ilyasova, N.; Andriyanov, N.; Zamytskiy, E.; Zolotarev, A.; Kirsh, D. Modeling of Fundus Laser Exposure for Estimating Safe Laser Coagulation Parameters in the Treatment of Diabetic Retinopathy. Mathematics 2021, 9, 967. https://doi.org/10.3390/math9090967
Shirokanev A, Ilyasova N, Andriyanov N, Zamytskiy E, Zolotarev A, Kirsh D. Modeling of Fundus Laser Exposure for Estimating Safe Laser Coagulation Parameters in the Treatment of Diabetic Retinopathy. Mathematics. 2021; 9(9):967. https://doi.org/10.3390/math9090967
Chicago/Turabian StyleShirokanev, Aleksandr, Nataly Ilyasova, Nikita Andriyanov, Evgeniy Zamytskiy, Andrey Zolotarev, and Dmitriy Kirsh. 2021. "Modeling of Fundus Laser Exposure for Estimating Safe Laser Coagulation Parameters in the Treatment of Diabetic Retinopathy" Mathematics 9, no. 9: 967. https://doi.org/10.3390/math9090967
APA StyleShirokanev, A., Ilyasova, N., Andriyanov, N., Zamytskiy, E., Zolotarev, A., & Kirsh, D. (2021). Modeling of Fundus Laser Exposure for Estimating Safe Laser Coagulation Parameters in the Treatment of Diabetic Retinopathy. Mathematics, 9(9), 967. https://doi.org/10.3390/math9090967








