Abstract
The quality and experience of healthcare systems affect the economy and prosperity of cities all over the world. Governments of several countries are struggling to improve the efficiency of their healthcare systems and decrease healthcare spending costs. In this paper, we discuss one of the most critical and busy processes among healthcare topics: ambulatory care center (ACC) appointment scheduling systems. We investigate the appointment-scheduling issue using a robust optimization framework to minimize operational costs while ensuring the improvement of healthcare service quality. Our findings and insights provide healthcare practitioners with tools to improve operational efficiency and service quality.
Keywords:
scheduling; healthcare management; hospital management; optimization; mathematical programming MSC:
90B35; 90C11; 90C27
1. Introduction
Most countries are experiencing the problems of aging and expanding populations. With more than seven million citizens, Hong Kong is considered one of the Asian Tigers and has seen an increasing and aging population. According to the statistics of the Hong Kong Government, the median age of Hong Kong’s people has risen from 37.2 to 51.8. However, the ongoing COVID-19 pandemic has affected a large proportion of elderly people. Therefore, it impresses a need for elderly care services and personnel requirements, such as doctors and nurses, which results in the deterioration of hospitals’ service quality and government expenditure. The Health Department of the Hong Kong Special Administrative Region (HKSAR) indicated in 2014 that over HKD 93 billion in healthcare spending was slashed in 2013, which comprised 5.1% of the total GDP (gross domestic product). Nearly 13 thousand Hong Kong dollars per capita was contributed to health treatment, which exceeded the median salary of the Hong Kong workforce. The government predicts that the number of people aged 55 and up will double in the next 15 years, while the workforce will shrink. As a result, the elderly dependency ratio, which measures the pressure on the production population, will rapidly increase. However, due to the unpredictable explosion of COVID-19, there has been an exponentially increased number of confirmed cases of the virus in Hong Kong that affected the aging population. To address the problem of the aging population and inadequate provision of healthcare services, the government can either allot more money to boost the capacities of healthcare facilities or enhance the efficiency of the existing healthcare system. The former requires a longer timeframe and a substantial amount of capital from the planning stage to the implementation stage. Another issue is the inadequacy of the workforce in the healthcare sector. Many doctors refuse to join public hospitals due to the long working hours and relatively low remunerations compared to private clinics or hospitals. The government has resorted to increasing the salaries of doctors and nurses and transferring the cost to the patients. Therefore, governments are now pursuing the latter method, which is more practical and favorable to long-term development. To accommodate more patients with the existing facilities, higher efficiency in resource allocation is required.
To deal with the abovementioned problems, we conducted a series of studies on Hong Kong healthcare services. In this paper, we study one of the busiest hospital departments, the ambulatory care center (ACC). The ACC is a medical care facility that offers outpatient healthcare evaluation and treatment. In Hong Kong, the ACC plays a very significant role due to limited resources, such as workforce, land supply, and the growing demand for outpatient care. As outpatients are not hospitalized in the unit, patients can come late, cancel bookings, or even miss bookings without notification. These behaviors cannot be eliminated by rules due to humanitarian issues. On the other hand, the consultation time for each patient is not a deterministic factor. Therefore, we develop a model that can deal with the abovementioned factors to maximize the benefits for the patients and minimize waste and abuse of resources. In this paper, we have set the objectives below:
- To identify the key business concerns and impact of robustness in the appointment scheduling system;
- To develop a robust optimization model for the appointment scheduling problem in healthcare;
- To understand the structural properties of the developed robust optimization model;
- To assess the effectiveness of the proposed robust optimization models based upon the real data collected from the Hospital Authority;
- To analyze and reveal useful insights for managing the appointment scheduling system in healthcare.
2. Background
In many service operations, the appointment-scheduling problem emerges as a challenging problem in which patients are serviced sequentially, the service time is unpredictable, and the practitioner must allocate time slots for serving patients in advance. Modern healthcare utilizes many types of expensive equipment and facilities, such as MRI installations, operation theaters, and CT scanners, in addition to highly skilled and well-paid workers. For instance, we consider the appointment-scheduling problem for scheduling surgeries for outpatients. The information on which surgery is to be done on a particular day is known in advance; however, the time to carry out the scheduled surgery can vary. Typically, on the preceding day, the hospital manager makes decisions on the number of operation theaters to be opened, the allocation of surgeries to operation theaters, and the sequencing of surgeries. The objective is to minimize the following single or multiple items:
- (1)
- The set-up fee for creating separate consultancy spaces;
- (2)
- The aggregated overtime expenses for all consultancy rooms;
- (3)
- The idle time between individual consultancy services;
- (4)
- The waiting time for patients.
To create a reliable appointment-to-consultancy-room allocation strategy, we consider the uncertainties related to the duration of each consulting service. We design a robust optimization framework for the appointment-scheduling problem in healthcare and study managerial insights for improving the efficiency of hospital operations. We employ random variables to represent the duration of a typical consulting service. It is not necessary to have a precise understanding of the underlying probability distributions because it is presumed that the unknown parameters are part of a polyhedral uncertainty set. We further analyze the structural properties for the appointment scheduling problem in healthcare and produce a near-optimal scheduling plan. The proposed approach’s implementation in real-world hospital management and managerial insights are discussed. The academic contribution of this paper is summarized as follows:
- (1)
- The theoretical results on the tractability of the proposed robust optimization model are of significant scientific value;
- (2)
- The proposed technique for solving the large-scale optimization problem with uncertainties can be applied to solve other problems;
- (3)
- The managerial insights for robust appointment scheduling in healthcare are of great interest in practice.
3. Literature Review
We conducted initial searches in the literature concerning the concept of appointment scheduling in healthcare. Cayirli and Veral [1] provided a comprehensive review of research on appointment scheduling in outpatient services, formulated the general problem, and modeled considerations and a taxonomy of methodologies. Gupta and Denton [2] demonstrated the design of an appointment scheduling system and identified the potential for the novel application of IE/OR models. Cayirli et al. [3] examined the connections between appointment system components and patient panel characteristics to evaluate the performance of ambulatory care. Kim and Giachetti [4] developed a stochastic mathematical overbooking model to predict the optimal number of appointments that patients accept to maximize the expected total earnings. A universal “Dome” appointment rule was introduced by Cayirli et al. [5] and can be parameterized for different clinics by a planning constant based on environmental factors, such as walk-ins, no-shows, the number of appointments made per session, the variability of service times, and the cost of doctors’ idle time and patients’ waiting time. Meskens et al. [6] optimized the usage of the operating room by reducing makespan and overtime and maximizing affinities between surgical team members by taking advantage of the “expressive power” of the constraint programming paradigm. For scheduling arrivals at a medical facility with no-show behavior, Zacharias and Pinedo [7] suggested an overbooking model intending to minimize the predicted weighted sum of patient waiting time, doctor idle time, and overtime. Kemper et al. [8] proposed a method for establishing appointment times in the D/G/1 queuing system by systematically minimizing the predicted loss per customer.
Since the main concern of this paper is to investigate the appointment-scheduling problem with uncertain service time, we also reviewed the robust optimization technique for addressing the uncertainty problem. Robust optimization is an approach that ensures the solutions remain feasible and near-optimal when data is changed. Soyster [9] investigated the work on robust optimization by attaining all uncertain parameters to reach their worst-case value, which was deemed over-conservative in a practical setting. Mulvey et al. [10] integrated the concept of scenario-based analysis, and goal programming and presented stochastic programming formulations to derive robust solutions. By using an ellipsoidal uncertainty set to modify the level of conservatism, Ben-Tal and Nemirovski [11] achieved some progress and provided comprehensible mathematical reformulations. By creating a polyhedron for each parameter, Bertsimas Bertsimas and Thile [12] addressed uncertainty to develop the idea of a “budget of uncertainty” to rein in conservatism. When employing numerous ranges to characterize unknown parameters, Düzgün and Thile [13] noted that a single range for each parameter still produced excessively conservative findings.
A substantial number of papers in the literature relevant to robust appointment scheduling dealing with uncertain service time was found. Denton et al. [14] proposed a stochastic optimization model and derived some practical heuristics to compute operation theatres schedules that hedged against the uncertainty in surgery duration. Utilizing statistical data on surgery duration, Hans et al. [15] considered the robust surgery-loading problem for the operation theatres department in a hospital and proposed various constructive heuristics and local search techniques to maximize capacity utilization and minimize the risk of overtime; Denton et al. [16] mentioned two types of models for assigning surgery blocks to operating rooms under uncertainty. When each work has a random processing length determined by a joint discrete probability distribution, Begen and Queyanne [17] examined the best appointment-scheduling strategy by minimizing the projected total underage and overage costs. Mittal et al. [18] used a strong optimization framework to investigate the appointment-scheduling problem, prove the existence of a closed-form optimal solution, and create the first constant-factor approximation algorithm. In a multistage operating room department with stochastic service time and numerous patient types, Saremi et al. [19] addressed the appointment scheduling of outpatient surgeries. To reduce the patients’ waiting time, surgical completion time, and cancellation rate, three simulation-based optimization strategies were proposed. Rachuba and Werners [20] integrated data on stochastic parameters into a scenario-based mixed integer optimization model with a focus on different stakeholders’ objectives that are simultaneously taken into account within a multi-criteria optimization model to avoid rescheduling when taking into account uncertainties of treatment duration and emergency arrivals. Mak et al. [21] created distribution-free models that precisely describe tractable conic programs to solve the appointment-scheduling problem by assuming only moment-by-moment information about job durations. To determine the best arrival order for patients with different features, Kong et al. [22] investigated a stochastic appointment-sequencing problem. They investigated the best sequencing rules using the idea of stochastic ordering, and they discovered why the smallest variance first rule was not as effective as they had hoped. Zhang et al. [23] investigated a distributional resilient formulation based on an ambiguity set that exploited the first two moments and derived an approximated semi-definite programming model for appointment scheduling under random service duration with uncertain distributions. They assigned their scheduled arrival times to reduce the anticipated total waiting time and used a chance constraint to limit the likelihood of the server over time given a sequence of appointments arriving at a particular server. A systematic literature review for no-shows in appointment scheduling and the application of robust optimization in heath appointment other domains can be seen in [24,25,26,27,28,29,30,31,32,33]. Wang et al. [34] presented a multi-station network model that carefully established a compromise between assumptions that permitted tractability and assumptions that prevented real-world adoption. The authors examined sequential appointment scheduling in a network of stations with exponential service delays, no-show potential, and overbooking to allow for real-world applicability and claimed that a heuristic myopic scheduling method was nearly ideal. Cox III and Boyed [35] offered a universal strawman method for creating a reliable system for robust scheduling of provider appointments in most situations. To verify the existence of both entities and causalities, an examination of the theory of limited thinking processes was conducted by utilizing a primary care practice. Recently, based on information about patient appointments, Issabakhsh et al. [36] created a mathematical model for mixed integer programming infusion appointment scheduling. Through the planning horizon, this model reduced the weighted sum of patient wait times overall and the number of beds utilized. To determine the best patient appointment times, a mathematical model using mixed integer programming and resilient slack allocation was used, taking into account the possibility that patient infusion times may be longer than anticipated [37,38,39].
This model proposed in this paper generates a workforce schedule that minimizes overtime and balances a doctor’s workload over a year, satisfying weekly patient demand. The objective function minimizes the addition between the workload of each pair of patients and the number of yearly overtime hours of the workforce as well [40,41,42,43,44]. By assuming that the input is only patients with a single session and that consultation and installation time are zero, the considered problem without resource constraints is reduced to the two stages as given in the flow shop problem, which is NP-hard [45]. Furthermore, resource variation is usually seen as an element that makes the planning/scheduling problem harder to solve [46]. Our problem should thus be at least NP-hard. Any continuous nonlinear function can be arbitrarily well approximated using a piecewise affine function [47]. In turn, MILP can be used to encode a piecewise affine function [48,49]. The treatment of non-convexity is the advantage of the MILP approach over a nonlinear optimization method. While most nonlinear approaches do not offer this guarantee and may be “caught” by local minima, some MILP solution methods do guarantee globally optimal solutions [50,51].
Our review of the literature indicated that a vast majority of studies have concentrated on finding robust appointment scheduling policies while considering the uncertainties of service time, with relatively less emphasis on sensitivity analysis concerning the uncertainty parameters and appropriate algorithms. The presented project aims at bridging these gaps.
4. Proposed Model
Every day, hospitals have to manage a large amount of uncertain data and make influential decisions. Hospital managers need to manage uncertain data efficiently. Therefore, a large-scale optimization method to deal with uncertain parameters is highly desired. A method like this ensures high-quality information choices and produces feasible and optimal policies. The characteristics of high tractability in this approach make hospital managers capable of doing adjustments and what-if analyses. To tackle the inefficient and unbalanced assignment between doctors and patients, hospital managers apply a robust optimization method for capacity planning and appointment scheduling at ACC. The choice of the robust optimization model can be justified for the following reasons:
- Data distributions are no longer required or are less strict; rough assumptions on the bounded support parameters exist [37].
- Preliminary data analysis can be performed much more easily.
- Robust components are tractable and independent of the number of parameters.
- The computation of the data is faster.
- The worst-case scenario can be considered, and risk analysis can be conducted.
- Robust optimization can be integrated into different models.
Our study emphasizes the robust appointment-scheduling problem that aims to assign appointments to consultancy rooms and minimize the total fixed cost associated with opening a consultancy room and the total overtime cost across all consultancy rooms
4.1. Basic Model
The deterministic capacity planning model for room and appointment scheduling can be unrealistic in practice. Hospital managers usually do not have sufficient information on the capacity occupancy status, even at the beginning of the planned period. Hence, in reality, the deterministic capacity planning model resembles a mixed integer linear program. When hospital administrators plan the resources to accommodate, the actual service time is always uncertain. Replacing the uncertain parameter with best point estimators is believed to be a useful method to solve the problem. Expected value can be an option to replace uncertain service time. Nevertheless, the downside of this approach is the feasibility of the solutions.
The solution might not be able to be implemented. Hospital managers might need to adopt some sensitivity analysis to rectify their solutions, which is described as a reactive approach. Lai and Ng [38] pointed out that in reality decision makers opt for proactive tools to generate their solutions. Robust optimization is one of the proactive approaches and is more appropriate for hospital managers, especially when they are risk-averse [39]. Recently, robust optimization has become a more popular approach when decision-makers face uncertain optimization problems. Under the framework of robust optimization, we use a polyhedral uncertainty set in capacity planning to model the uncertain service duration. The only mild assumption is that decision makers are capable of estimating the maximum and minimum value of service durations, which is able to be derived from historical data. Without the information of exact distribution, the actual durations are bounded within the abovementioned polyhedral uncertainty sets. The goal is to minimize the possible cost in the worst situation for any realized durations within the uncertainty set.
The appointment-scheduling problem includes two important decisions: (1) how many consultancy rooms are to be opened on a particular day and (2) which appointments are to be assigned to each consultancy room? The objective is to minimize the weighted sum of the total cost of opening consultancy rooms and the total overtime associated with overbooking a consultancy room. We present the following variables to develop the model.
- Indices:index of appointment blocks,
- index of consultancy rooms,
- Parameters:exact duration of block in room , and are lower and upper limits on the service duration of , respectively,
- scheduled session length for each consultancy room .
- predetermined price to launch ,
- variable price per unit of time to maintain , open.
- Decision variables:
- a binary variable equal to 1 if consultancy room is open and 0 otherwise.
- a binary variable equal to 1 if appointment is allocated to consultancy room and 0 otherwise.
- overtime for .
We develop a deterministic model to determine the number of open consultancy rooms and the number of appointment allocations to consultancy rooms. Consider the following linear programming model:
Subject to
4.2. Robust Optimization Model
Note that the proposed deterministic appointment-scheduling model (D-AS) does not always hold in practice. Parameters in D-AS are always uncertain at the beginning of a planning period. In recent years, robust optimization has evolved as a preeminent technique in immunizing uncertain mathematical optimization. The large-scale optimization problem with uncertain parameters can easily be solved under the robust optimization techniques. We employ the robust optimization method to model uncertain duration as a polyhedral uncertainty set. We mildly assume that decision makers are able to provide reasonable estimations of lower and upper bounds on the uncertain duration according to the estimation derived from historical data. The actual duration, without exact knowledge of distribution, must lie within the aforementioned polyhedral uncertainty set. Our work seeks to minimize the worst permutation cost for all realizations of duration within the uncertainty set. Recall that indicates actual duration required to fulfill appointment in the consultancy room , and that are lower and upper bounds on the duration to fulfill appointment , respectively; . Let
Equation (4) shows the idea of Bertsimas and Sim (2004) [30] and Denton et al. (2010) [16]. As a controlled variable, determines how conservative the worst-case scenario is. More specifically, denotes an upper limit on number of duration outcomes for the worst-case situation. Thus, in particular, if , we consider only the best scenario. All actual durations receive their lowest values; if , the worst-case scenario is taken into consideration. Within the framework of the appointment-scheduling problem in this paper, we take as an integer value. This variable indicates the maximum duration taken by doctors to provide the best treatment to a patient. Therefore, the robust version of appointment scheduling problem (R-AS) is formulated as a two-stage recourse model below:
Subject to
where
Subject to
The objective function is used to minimize the additional cost associated with overtime, wherein and are fixed and is a decision variable. Note that equals either 0 or the difference between the actual duration and the planned session length in . Hence, the expression of in (5) can be reformulated as follows:
Subject to
where
Since the variable indicates a binary choice, the above reformulation is a nonlinear program. However, the special structure of this reformulation motivates us to transform it into a linear program. Note that constraints (7) promise that if for some , then for all . This ensures that we formulate as a mixed integer linear program (MILP) again in the following:
Subject to
For the sake of obtaining the dual of , we define , . Note that constraints (7) imply that if reaches its lower bound , will be 0; if is at its upper bound , will be 1. On the basis of this definition, the above reformulated mixed integer linear program (MILP) (10) can be expressed as follows:
Subject to
This reformulation is a mixed integer linear program (MILP) and the decision variables are and . Therefore, the dual of the above reformulation of is:
Subject to
Note that is the dual variable associated with constraint (12), the dual variables associated with constraints (13), and are the dual variables associated with bounds (14). Recall the two-stage recourse problem (5) formulated by the R-AS, we reformulate (5) as follows:
Subject to
The above reformulation is a mixed integer nonlinear program (MINP) due to the multiplication of and in constraints (21). Consequently, a modified robust version of appointment scheduling problem (MR-AS) is presented as follows:
Subject to
Note that is the service overtime more than the lower bound to fulfill appointment i in each consultation room j. Therefore, we are able to obtain robust solutions to the appointment-scheduling problem by solving the mixed integer linear program (MILP) (22), which seeks to avoid the worst case by imposing a limit on the level of conservativeness of the derived solution. A sensitive analysis with respect to each parameter in (22) can be conducted to reflect the corresponding relationships. We derive the proposed model for solving the problem.
5. Result and Discussion
In this session, we apply the simulated data based on the hospital information to evaluate the effectiveness of the robust optimization model. In order to diminish the complexity of the demonstration, we make several assumptions on the parameters. First, we assume that the costs of opening different consultation rooms are the same and that the equipment inside the rooms is similar. Second, we assume that in the short-term, the demand of the hospital and its distribution are static, as the usage of the Hong Kong hospital capacity is forecast to be consistently increasing in the long run. Third, we assume that once we decide to open a new consultation room, then a new doctor can be assigned to the room immediately without affecting the current operations of the center. In the short-run, we can obtain the minimum operational cost of the hospital or clinic by choosing the number of opened consultation rooms and assigning the number of appointments in blocks with the given parameters. The program code was written in MATLAB (2021b) and we have taken the help of linear programming from [52] to deliver the solution of mixed integer linear programming problem. In Figure 1, we can see the change in cost against the number of opened consultation rooms.
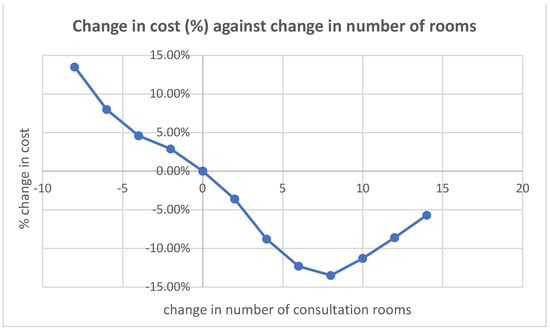
Figure 1.
Change in total price against change in the number of rooms.
In this figure, before we increase the number of consultation rooms by eight, we can see the inverse relationship between the change in cost (in percentage) and the change in the number of open consultation rooms. Intuitively, if we open a new room, the fixed cost will increase; therefore, the change in cost is positive. However, when we consider the overtime cost, then the reduction in overtime service will cause a reduction in overtime cost, which in turn compensates for the increase in the fixed cost due to more opened consultation rooms. That is also the reason that when we reduce the number of current opened consultation room, the total cost increases even though the fixed cost has been reduced. (i.e., the overtime cost increases). The trend changes when it reaches the number of opened consultation rooms to eight. Beyond that point, the reduction in overtime costs, such as at point 8, cannot compensate for the fixed cost of extra consultation rooms. However, it is still better than the original setting without any extra open rooms. Therefore, we can see the reduction in total cost is less when we further provide more rooms. The result shows that we can achieve the minimum cost if we open eight more extra rooms in the existing settings. Several factors can affect the shape of the curve. Intuitively, we know that if the demand for the ambulatory care center decreases, the required rooms will decrease because the overrun cost will be lower if fewer customers are present. If the current setting is the optimal point, the minimum point will touch the zero point.
We demonstrate the utility of the proposed robust capacity-planning model for ambulatory care clinics with information uncertainty. The data provided by the hospital authority were normalized to implement the experiment. We assume the number of appointments at the beginning of the period is zero. The hospital managers decide which consultation rooms to be opened in order to accommodate four blocks or appointments. The fixed cost of opening a consultation room is given as well as the service overrun cost and the normal capacity (working hours) of a consultation room, which are shown in Table 1.

Table 1.
Fixed cost of consultation rooms, variable cost per unit service overrun and regular capacity for each consultation room.
The relationship between and approximates the cost of opening a new consultation room. In Table 2, the lower and upper values of the uncertainty set of service duration to fulfill the appointment .

Table 2.
Lower and upper bounds on the uncertainty set.
As mentioned, decides the conservativeness of the optimal solution generated from the modified robust capacity problem. In this case, implies the minimum conservative configuration, in which the actual service duration to fulfill the appointments reaches the lower bound. Note that = 12 implies the most conservative situation, meaning that the actual service duration attained its maximum level for each consultation room. In the meantime, the sensitivity analysis for the optimal solution is calculated from the modified robust capacity planning problem with the service overtime cost per unit for each consultation room.
Table 1, Table 2 and Table 3 are used to calculate the required value for comparing different values of and . However, we change the value of the variables present in the constraints of the model (22) for proper justification. We present the comparison test in Table 4 as below:

Table 3.
Different scenarios with different variable costs of service overtime in each consultation room.

Table 4.
Five Experiments for comparison purpose.
In Figure 2, the trend of the total fixed cost of opening a consultation room, and the variable of service overtime is shown when both and alter.
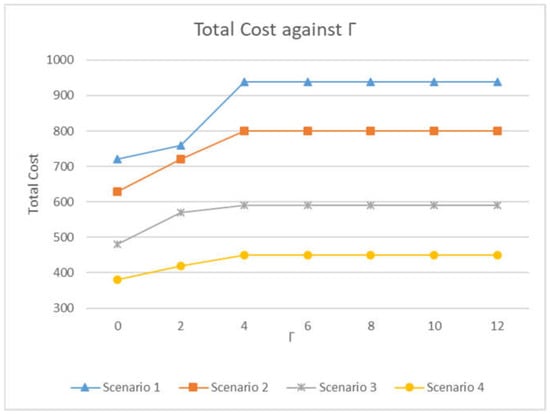
Figure 2.
The trend of the total cost of opening consultation room and service overtime with respect to and .
Without surprise, the increase in degree of conservativeness increases the total cost in optimal objective function monotonically. Therefore, the deterioration of total cost is even worse for the larger cost of service overtime ( is larger) when increases. For all scenarios, the worst case occurs ahead of the theoretical situation, i.e., for all scenarios in the numerical examples. To indicate the usefulness and effectiveness of the robust optimization model, different values of the optimal solution from the deterministic models of capacity planning problem are generated. Therefore, the results from the modified robust version of capacity planning problem can be compared to the deterministic ones. As the middle value of the interval in Table 2 to fulfill appointments, the nominal values of service duration corresponding to the appointment can be considered to be 750. The measure of effectiveness of the suggested model is defined as the ratios of the expected cost from the deterministic model to that from the modified robust version of capacity planning problem. The trend of the ratio corresponding to the nominal values for Scenario 1 in Table 2 is shown in Figure 2.
In Figure 3, when increases, the modified robust version of capacity planning model can generate better solutions. The superiority of the solution according to the model first decreases and then remains unchanged. This means that the optimal value will remain constant after some threshold of . In Figure 3, the threshold is . The observation is that the solution from the suggested model will contribute a reduction in total cost. Additionally, the best situation is when .
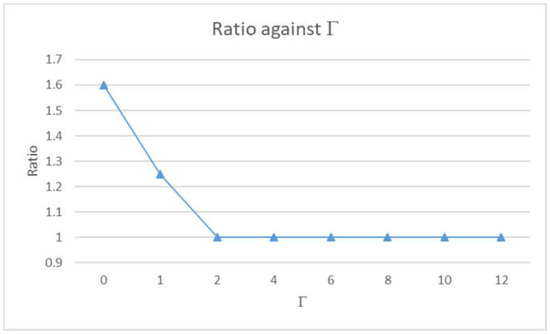
Figure 3.
The ratios of the total cost from deterministic model to the total cost from modified robust model with respect to .
6. Management Insights
Before deciding which rooms or sites to open, hospital managers have to investigate the cost structure of each room. A higher fixed cost of the consultancy room is usually associated with a higher variable cost. If a room with a higher capacity has a lower cost, the managers will definitely choose that. The cost of paying doctors and nurses for a specific day, the cost of utilities, and the price of building the rooms and the equipment are all included in the fixed cost. The variable cost includes the overtime cost of service and other utility costs. After determining the fixed and variable costs, the conservatism of the decisionmakers can be assigned based on their own confidence levels. The lower the total cost, the more conservative the decisionmakers are with the decision variable. The hospital managers have no difference in the costs when their conservatism level is greater than the fixed level, regardless of any scenarios. The cost increases when the conservative value of the parameter decreases until it reaches the required level. On the other hand, if the suggested model is used, the hospital managers can expect the total cost to be improved when the conservatism level reaches the maximum value.
7. Conclusions
We have created a reliable appointment-scheduling model that can reduce overall costs while ignoring the distribution of overflow time in order to address the recently increasing demand for hospital capacity. The number of open consultation rooms and the number of appointments in each block are the two primary decisions made in order to achieve the reduced cost. The variable costs of overflow service must be balanced against the fixed expense of keeping consultation rooms open. The validity of our model has been demonstrated by simulated data and the optimal course of action in the given situation during the peak time. We can only apply these limits appropriately if the resources are limited. The maximum number of patients in a block, the number of doctors on duty, and the number of rooms that can be opened are possible restrictions. The capacity of the hospital may be determined using this model, which also offers managerial aspects for evaluating the impact of changes to the existing settings. It is important to analyze seasonal trends since the majority of variables might be volatile over time.
Author Contributions
Y.G., formal analysis, conceptualization; Q.Z., investigation, supervision; C.K.L., writing—original draft preparation; B.R., validation, formal analysis. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability Statement
The program code and data that support the plots discussed within this paper is available from the corresponding author upon request.
Acknowledgments
We would also like to thank the anonymous reviewers who helped us to clarify many points and improve the paper. All authors acknowledge the support from their respective institutes/universities.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Cayirli, T.; Veral, E. Outpatient scheduling in health care: A review of literature. Prod. Oper. Manag. 2003, 12, 519–549. [Google Scholar] [CrossRef]
- Gupta, D.; Denton, B. Appointment scheduling in health care: Challenges and opportunities. IIE Trans. 2008, 40, 800–819. [Google Scholar] [CrossRef]
- Cayirli, T.; Veral, E.; Rosen, H. Designing appointment scheduling systems for ambulatory care services. Health Care Manag. Sci. 2006, 9, 47–58. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Giachetti, R.E. A stochastic mathematical appointment overbooking model for healthcare providers to improve profits. IEEE Trans. Syst. Man Cybern.-Part A Syst. Hum. 2006, 36, 1211–1219. [Google Scholar] [CrossRef]
- Cayirli, T.; Yang, K.K.; Quek, S.A. A universal appointment rule in the presence of no-shows and walk-ins. Prod. Oper. Manag. 2012, 21, 682–697. [Google Scholar] [CrossRef]
- Meskens, N.; Duvivier, D.; Hanset, A. Multi-objective operating room scheduling considering desiderata of the surgical team. Decis. Support Syst. 2013, 55, 650–659. [Google Scholar] [CrossRef]
- Zacharias, C.; Pinedo, M. Appointment scheduling with no-shows and overbooking. Prod. Oper. Manag. 2014, 23, 788–801. [Google Scholar] [CrossRef]
- Kemper, B.; Klaassen, C.A.; Mandjes, M. Optimized appointment scheduling. Eur. J. Oper. Res. 2014, 239, 243–255. [Google Scholar] [CrossRef]
- Soyster, A.L. Convex programming with set-inclusive constraints and applications to inexact linear programming. Oper. Res. 1973, 21, 1154–1157. [Google Scholar] [CrossRef]
- Mulvey, J.M.; Vanderbei, R.J.; Zenios, S.A. Robust optimization of large-scale systems. Oper. Res. 1995, 43, 264–281. [Google Scholar] [CrossRef]
- Ben-Tal, A.; Nemirovski, A. Selected topics in robust convex optimization. Math. Program. 2008, 112, 125–158. [Google Scholar] [CrossRef]
- Bertsimas, D.; Thiele, A. Robust and data-driven optimization: Modern decision making under uncertainty. In Models, Methods, and Applications for Innovative Decision Making; INFORMS: Catonsville, MD, USA, 2006; pp. 95–122. [Google Scholar]
- Düzgün, R.; Thiele, A. Robust Optimization with Multiple Ranges: Theory and Application to R&D Project Selection; Technical Report; Lehigh University: Bethlehem, PA, USA, 2010; pp. 103–118. [Google Scholar]
- Denton, B.; Viapiano, J.; Vogl, A. Optimization of surgery sequencing and scheduling decisions under uncertainty. Health Care Manag. Sci. 2007, 10, 13–24. [Google Scholar] [CrossRef]
- Hans, E.; Wullink, G.; Van Houdenhoven, M.; Kazemier, G. Robust surgery loading. Eur. J. Oper. Res. 2008, 185, 1038–1050. [Google Scholar] [CrossRef]
- Denton, B.T.; Miller, A.J.; Balasubramanian, H.J.; Huschka, T.R. Optimal allocation of surgery blocks to operating rooms under uncertainty. Oper. Res. 2010, 58, 802–816. [Google Scholar] [CrossRef]
- Begen, M.A.; Queyranne, M. Appointment scheduling with discrete random durations. Math. Oper. Res. 2011, 36, 240–257. [Google Scholar] [CrossRef]
- Mittal, S.; Schulz, A.S.; Stiller, S. Robust appointment scheduling. In Approximation, Randomization, and Combinatorial Optimization. Algorithms and Techniques (APPROX/RANDOM 2014); Schloss Dagstuhl-Leibniz-Zentrum fuer Informatik: Wadern, Germany, 2014. [Google Scholar]
- Saremi, A.; Jula, P.; ElMekkawy, T.; Wang, G.G. Appointment scheduling of outpatient surgical services in a multistage operating room department. Int. J. Prod. Econ. 2013, 141, 646–658. [Google Scholar] [CrossRef]
- Rachuba, S.; Werners, B. A robust approach for scheduling in hospitals using multiple objectives. J. Oper. Res. Soc. 2014, 65, 546–556. [Google Scholar] [CrossRef]
- Mak, H.Y.; Rong, Y.; Zhang, J. Appointment scheduling with limited distributional information. Manag. Sci. 2015, 61, 316–334. [Google Scholar] [CrossRef]
- Kong, Q.; Lee, C.Y.; Teo, C.P.; Zheng, Z. Appointment sequencing: Why the smallest-variance-first rule may not be optimal. Eur. J. Oper. Res. 2016, 255, 809–821. [Google Scholar] [CrossRef]
- Zhang, Y.; Shen, S.; Erdogan, S.A. Distributionally robust appointment scheduling with moment-based ambiguity set. Oper. Res. Lett. 2017, 45, 139–144. [Google Scholar] [CrossRef]
- Dantas, L.F.; Fleck, J.L.; Oliveira, F.L.C.; Hamacher, S. No-shows in appointment scheduling–a systematic literature review. Health Policy 2018, 122, 412–421. [Google Scholar] [CrossRef]
- Kong, Q.; Li, S.; Liu, N.; Teo, C.P.; Yan, Z. Appointment scheduling under time-dependent patient no-show behavior. Manag. Sci. 2020, 66, 3480–3500. [Google Scholar] [CrossRef]
- Li, J.; Fu, H.; Lai, K.K.; Ram, B. Optimization of Multi-Objective Mobile Emergency Material Allocation for Sudden Disasters. Public Health Front. 2022, 10, 927241. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Cheng, W.; Lai, K.K.; Ram, B. Multi-AGV Flexible Manufacturing Cell Scheduling Considering Charging. Mathematics 2022, 10, 3417. [Google Scholar] [CrossRef]
- Xu, Y.; Wang, M.; Lai, K.K.; Ram, B. A Stochastic Model for Shipping Container Terminal Storage Management. J. Mar. Sci. Eng. 2022, 10, 1429. [Google Scholar] [CrossRef]
- Li, J.; Liu, H.; Lai, K.K.; Ram, B. Vehicle and UAV Collaborative Delivery Path Optimization Model. Mathematics 2022, 10, 3744. [Google Scholar] [CrossRef]
- Bertsimas, D.; Sim, M. Robust discrete optimization and network flows. Math. Program. 2003, 98, 49–71. [Google Scholar] [CrossRef]
- Ben-Tal, A.; Nemirovski, A. Robust convex optimization. Math. Oper. Res. 1998, 23, 769–805. [Google Scholar] [CrossRef]
- Ben-Tal, A.; Nemirovski, A. Robust solutions of uncertain linear programs. Oper. Res. Lett. 1999, 25, 1–13. [Google Scholar] [CrossRef]
- Ben-Tal, A.; Nemirovski, A. Robust solutions of linear programming problems contaminated with uncertain data. Math. Program. 2000, 88, 411–424. [Google Scholar] [CrossRef]
- Wang, D.; Muthuraman, K.; Morrice, D. Coordinated patient appointment scheduling for a multistation healthcare network. Oper. Res. 2019, 67, 599–618. [Google Scholar] [CrossRef]
- Cox, J.F., III; Boyd, L.H. Using the theory of constraints’ processes of ongoing improvement to address the provider appointment scheduling system design problem. Health Syst. 2020, 9, 124–158. [Google Scholar] [CrossRef]
- Issabakhsh, M.; Lee, S.; Kang, H. Scheduling patient appointment in an infusion center: A mixed integer robust optimization approach. Health Care Manag. Sci. 2021, 24, 117–139. [Google Scholar] [CrossRef] [PubMed]
- Alem, D.J.; Morabito, R. Production planning in furniture settings via robust optimization. Comput. Oper. Res. 2012, 39, 139–150. [Google Scholar] [CrossRef]
- Lai, K.K.; Ng, W.L. A stochastic approach to hotel revenue optimization. Comput. Oper. Res. 2005, 32, 1059–1072. [Google Scholar] [CrossRef]
- Wu, Y. Linear robust models for international logistics and inventory problems under uncertainty. Int. J. Comput. Integr. Manuf. 2011, 24, 352–364. [Google Scholar] [CrossRef][Green Version]
- Azmat, C.S.; Hürlimann, T.; Widmer, M. Mixed integer programming to schedule a single-shift workforce under annualized hours. Ann. Oper. Res. 2004, 128, 199–215. [Google Scholar] [CrossRef]
- Ouazene, Y.; Yalaoui, F.; Chehade, H.; Yalaoui, A. Workload balancing in identical parallel machine scheduling using a mathematical programming method. Int. J. Comput. Intell. 2014, 7, 58–67. [Google Scholar] [CrossRef]
- Schwerdfeger, S.; Walter, R. Improved algorithms to minimize workload balancing criteria on identical parallel machines. Comput. Oper. Res. 2018, 93, 123–134. [Google Scholar] [CrossRef]
- Ouazene, Y.; Nguyen, N.Q.; Yalaoui, F. Workload Balancing on Identical Parallel Machines: Theoretical and Computational Analysis. Appl. Sci. 2012, 11, 3677. [Google Scholar] [CrossRef]
- Tran, Q.N.H.; Nguyen, N.Q.; Chehade, H.; Amodeo, L.; Yalaoui, F. Outpatient Appointment Optimization: A Case Study of a Chemotherapy Service. Appl. Sci. 2022, 12, 659. [Google Scholar] [CrossRef]
- Lenstra, J.K. Sequencing by Enumerative Methods. Ph.D. Thesis, Universiteit van Amsterdam, Amsterdam, The Netherlands, 1976. [Google Scholar]
- Nguyen, N.Q.; Yalaoui, F.; Amodeo, L.; Chehade, H.; Toggenburger, P. Electrical Vehicle Charging Coordination Algorithms Framework. In Studies in Systems, Decision and Control; Springer International Publishing: Berlin/Heidelberg, Germany, 2018; pp. 357–373. [Google Scholar]
- Floudas, C.A. Nonlinear and Mixed-Integer Optimization: Fundamentals and Applications; Oxford University Press: Oxford, UK, 1995. [Google Scholar]
- Sontag, E.D. Interconnected automata and linear systems: A theoretical framework in discrete-time. In International Hybrid Systems Workshop; Springer: Berlin/Heidelberg, Germany, 1995; pp. 436–448. [Google Scholar]
- Bemporad, A.; Ferrari-Trecate, G.; Morari, M. Observability and controllability of piecewise affine and hybrid systems. IEEE Trans. Autom. Control 2000, 45, 1864–1876. [Google Scholar] [CrossRef]
- Richards, A.; How, J. Mixed-integer programming for control. In Proceedings of the 2005 American Control Conference, Portland, OR, USA, 8–10 June 2005; pp. 2676–2683. [Google Scholar]
- Wolsey, L.A. Heuristic analysis, linear programming and branch and bound. In Combinatorial Optimization II; Springer: Berlin/Heidelberg, Germany, 1980; pp. 121–134. [Google Scholar]
- Mishra, S.K.; Ram, B. Introduction to Linear Programming with MATLAB®; Chapman and Hall/CRC: London, UK, 2017. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).