Virtual Reality in Critical Care Nursing Education: A Scoping Review
Abstract
1. Introduction
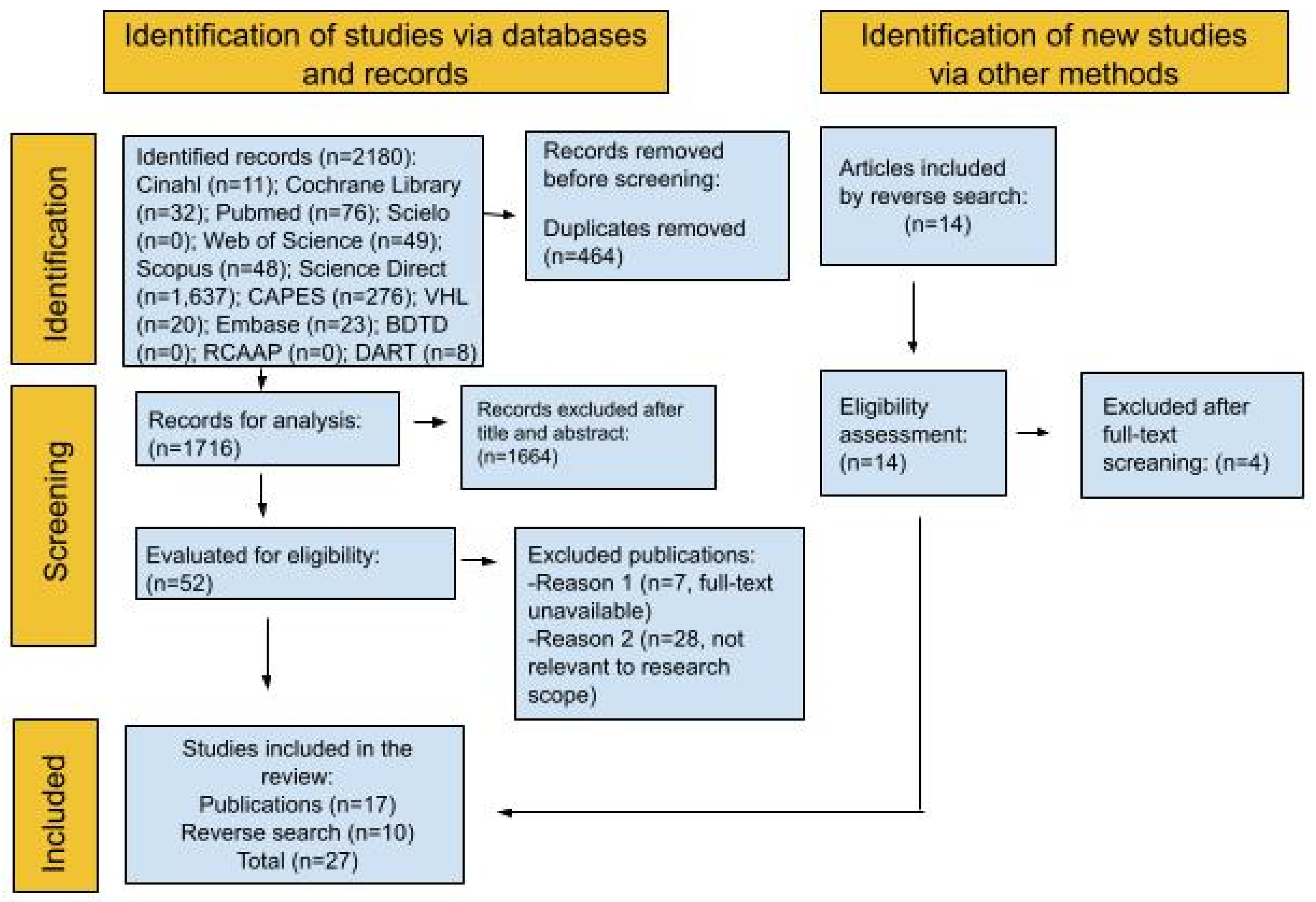
2. Materials and Methods
3. Results
4. Discussion
4.1. Nursing Skills
4.1.1. Cardiopulmonary Resuscitation
4.1.2. Tracheostomy
4.1.3. Nasogastric
4.1.4. Mechanical Ventilation
4.1.5. Other Nursing Skills
4.2. Impact on Teaching and Learning
4.3. Challenges in VR
4.4. Limitations of the Review
4.5. Future Research Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| VR | Virtual Reality |
| JBI | Joanna Briggs Institute |
| PRISMA-ScR | Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews |
| PAGER | Patterns, Advances, Gaps, Evidence for Practice, and Research Recommendations |
| ICU | Intensive Care Unit |
| HMDs | Head-Mounted Displays |
| CPR | Cardiopulmonary Resuscitation |
| IV | Intravenous |
| N/A | Not Applicable |
References
- Aguiar, B., Gomes, M., Lins, A., & Muniz, M. T. (2021). Utilização da realidade virtual para o ensino em saúde. Revista Educação Inclusiva, 5(1), 106–118. Available online: https://revista.uepb.edu.br/REIN/article/view/325 (accessed on 15 January 2025).
- Al-Mugheed, K., Bayraktar, N., Al-Bsheish, M., Al-Syouf, A., Aldhmadi, B. K., Jarrar, M., & Alkhazali, M. (2022). Effectiveness of game-based virtual reality phone application and online education on knowledge, attitude and compliance of standard precautions among nursing students. PLoS ONE, 17(11), e0275130. [Google Scholar] [CrossRef] [PubMed]
- Alotaibi, F. Z., Alkhatabi, R., Allowaihiq, L., Alhazzani, H., Alshehri, G., Hajr, E. A., & Alkholaiwi, F. (2022). Assessment of the ability, perception, and readiness of nurses to manage tracheostomy-related complications in Riyadh City: A cross-sectional study. BMC Nursing, 21, 320. [Google Scholar] [CrossRef] [PubMed]
- Araújo, F. J. d., Santos, L. A., Mungo, W. S., Bezerra, O. P. C., de Castilhos, C. S., Demuner, J. A., de Oliveira, N. P., Oliveira, P. R., & Carretero, J. d. S. (2024). Tecnologia e educação: O ensino por meio da realidade virtual. Revista Contemporânea, 4(1), 2039–2052. [Google Scholar] [CrossRef]
- Babaita, A. O., Kako, M., Teramoto, C., Okamoto, M., Hayashi, Y., Ohshimo, S., Sadamori, T., Hattori, M., & Moriyama, M. (2024). Face-to-face versus 360° VR video: A comparative study of two teaching methods in nursing education. BMC Nursing, 23, 199. [Google Scholar] [CrossRef]
- Banville, F., Milhomme, D., Perron, A., Houle, J., Therrien, D., Peguero-Rodriguez, G., Charette, S., Menelas, B., Trépanier, M., & Bouchard, S. (2023). Using virtual reality to improve nurses’ students’ clinical surveillance in a critical care context: A psychological perspective on learning. Annual Review of Cybertherapy and Telemedicine, 21, 245–250. Available online: https://www.arctt.info/volume-21-summer-2023 (accessed on 1 November 2024).
- Bayram, S. B., & Caliskan, N. (2019). Effect of a game-based virtual reality phone application on tracheostomy care education for nursing students: A randomized controlled trial. Nurse Education Today, 79, 25–31. [Google Scholar] [CrossRef]
- Botha, B. S., Wet, L., & Botma, Y. (2021). Undergraduate nursing student experiences in using immersive virtual reality to manage a patient with a foreign object in the right lung. Clinical Simulation in Nursing, 56, 76–83. [Google Scholar] [CrossRef]
- Bradbury-Jones, C., Aveyard, H., Herber, O. R., Isham, L., Taylor, J., & O’Malley, S. (2021). Scoping reviews: The PAGER framework for improving the quality of reporting. International Journal of Social Research Methodology, 25(4), 457–470. [Google Scholar] [CrossRef]
- Branco, M. J. C., Lucas, A. P. M., Marques, R. M. D., & Sousa, P. P. (2020). The role of the nurse in caring for the critical patient with sepsis. Revista Brasileira de Enfermagem, 73(4), e20190031. [Google Scholar] [CrossRef]
- Brown, R., Rasmussen, R., Baldwin, I., & Wyeth, P. (2012). Design and implementation of a virtual world training simulation of ICU first hour handover processes. Australian Critical Care, 25(3), 178–187. [Google Scholar] [CrossRef][Green Version]
- Butt, A. L., Kardong-Edgren, S., & Ellertson, A. (2018). Using game-based virtual reality with haptics for skill acquisition. Clinical Simulation in Nursing, 16, 25–32. [Google Scholar] [CrossRef]
- Chang, Y. M., & Lai, C. L. (2021). Exploring the experiences of nursing students in using immersive virtual reality to learn nursing skills. Nurse Education Today, 97, 104670. [Google Scholar] [CrossRef]
- Chang, Y. Y., Chao, L. F., Chang, W., Lin, C. M., Lee, Y. H., Latimer, A., & Chung, M. L. (2024). Impact of an immersive virtual reality simulator education program on nursing students’ intravenous injection administration: A mixed methods study. Nurse Education Today, 132, 106002. [Google Scholar] [CrossRef]
- Chao, Y. C., Hu, S. H., Chiu, H. Y., Huang, P. H., Tsai, H. T., & Chuang, Y. H. (2021). The effects of an immersive 3D interactive video program on improving student nurses’ nursing skill competence: A randomized controlled trial study. Nurse Education Today, 103, 104979. [Google Scholar] [CrossRef]
- Cheng, A., Fijacko, N., Lockey, A., Greif, R., Abelairas-Gomez, C., Gosak, L., & Lin, Y. (2024). Use of augmented and virtual reality in resuscitation training: A systematic review. Resuscitation Plus, 18, 100643. [Google Scholar] [CrossRef]
- Faria, J. M. S., Pontífice-Souza, P., & Gomes, M. J. P. (2018). La comodidad del paciente en cuidados intensivos: Una revisión integradora. Enfermería Global, 17(2), 477–489. [Google Scholar] [CrossRef]
- Filho, A. S. C., Lemos, W. B., Souza, R. C., & Lima, L. L. B. (2020). Realidade virtual como ferramenta educacional e assistencial na saúde: Uma revisão integrativa. Journal of Health Informatics, 12(2), 58–63. Available online: https://jhi.sbis.org.br/index.php/jhi-sbis/article/view/708 (accessed on 15 January 2025).
- Fleming, G. A., Petrie, J. R., Bergenstal, R. M., Holl, R. W., Peters, A. L., & Heinemann, L. (2020). Diabetes digital app technology: Benefits, challenges, and recommendations. Diabetologia, 63, 229–241. [Google Scholar] [CrossRef] [PubMed]
- García-Pazo, P., Pol-Castañeda, S., Moreno-Mulet, C., Pomar-Forteza, A., & Carrero-Planells, A. (2023). Virtual reality and critical care education in nursing: A cross-sectional study. Nurse Education Today, 131, 105971. [Google Scholar] [CrossRef]
- Hall, K., Bhowmik, J., Simonda, I., & Edward, K. L. (2024). The use of simulated participant and virtual reality simulation to enhance nursing students’ communication skills in “end of life care”: A single-arm repeated measures study. Clinical Simulation in Nursing, 91, 101543. [Google Scholar] [CrossRef]
- Harmon, J., Pitt, V., Summons, P., & Inder, K. J. (2021). Use of artificial intelligence and virtual reality within clinical simulation for nursing pain education: A scoping review. Nurse Education Today, 97, 104700. [Google Scholar] [CrossRef] [PubMed]
- Hong, C., & Wang, L. (2023). Virtual reality technology in nursing professional skills training: Bibliometric analysis. JMIR Serious Games, 11, e44766. [Google Scholar] [CrossRef]
- Hubail, D., Mondal, A., Jabir, A. A., & Patel, B. (2022). Comparison of a virtual reality compression-only Cardiopulmonary Resuscitation (CPR) course to the traditional course with content validation of the VR course—A randomized control pilot study. Annals of Medicine and Surgery, 73, 103241. [Google Scholar] [CrossRef] [PubMed]
- Junior, J. C. F. S., Cabral, P. M. F., & Bruno, L. V. P. (2020). O desenvolvimento de competências de liderança em mundos digitais virtuais tridimensionais. Revista Valore, 5, 293–311. [Google Scholar] [CrossRef]
- Kiegaldie, D., & Shaw, L. (2023). Virtual reality simulation for nursing education: Effectiveness and feasibility. BMC Nursing, 22, 488. [Google Scholar] [CrossRef]
- Kim, J., & Seo, M. (2024). Development and effects of extended reality training for nursing students on intravenous therapy using an infusion pump: A mixed methods study. Clinical Simulation in Nursing, 94, 101563. [Google Scholar] [CrossRef]
- Kuyt, K., Park, S. H., Chang, T. P., Jung, T., & MacKinnon, R. (2021). The use of virtual reality and augmented reality to enhance cardiopulmonary resuscitation: A scoping review. Advances in Simulation, 6, 11. [Google Scholar] [CrossRef]
- Lau, S. T., Siah, C. J. R., Loh, W. L., & Rusli, K. D. B. (2023). Enhancing professional competency in clinical procedures using head-mounted display virtual reality: A mixed method study. Medical Education Online, 28(1), 2232134. [Google Scholar] [CrossRef]
- Lee, H., & Han, J. W. (2022). Development and evaluation of a virtual reality mechanical ventilation education program for nursing students. BMC Medical Education, 22, 775. [Google Scholar] [CrossRef]
- Ma, J., Wangb, Y., Joshi, S., Wang, H., Young, C., Pervez, A., Qu, Y., & Washburn, S. (2024). Using immersive virtual reality technology to enhance nursing education: A comparative pilot study to understand efficacy and effectiveness. Applied Ergonomics, 115, 104159. [Google Scholar] [CrossRef]
- Marques, F. M., Pinheiro, M. J., & Alves, P. V. (2022). O julgamento clínico e a tomada de decisão nos estudantes do curso de licenciatura em enfermagem. Ciência & Saúde Coletiva, 27(5), 1731–1740. [Google Scholar] [CrossRef]
- Merola, R., Vargas, M., Sanfilippo, F., Vergano, M., Mistraletti, G., Vetrugno, L., Pascale, G., Bignami, E. G., Servillo, G., & Battaglini, D. (2025). Tracheostomy practice in the Italian intensive care units: A point-prevalence survey. Medicina, 61(1), 87. [Google Scholar] [CrossRef]
- Mir, T., Shafi, O., Balla, S., Munir, M. B., Qurehi, W. T., Kakouros, N., Bhat, Z., Koul, P., & Rab, T. (2024). Intensive care admissions and outcome of cardiac arrests: A national cohort study from the United States. Journal of Intensive Care Medicine, 39(2), 118–124. [Google Scholar] [CrossRef]
- Ouzzani, M., Hammady, H., Fedorowicz, Z., & Elmagarmid, A. (2016). Rayyan: A web and mobile app for systematic reviews. Systematic Reviews, 5, 210. [Google Scholar] [CrossRef]
- Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J. M., Akl, E. A., Brennan, S. E., Chou, R., Glanville, J., Grimshaw, J. M., Hróbjartsson, A., Lalu, M. M., Li, T., Loder, E. W., Mayo-Wilson, E., McDonald, S., … Moher, D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ, 372(71), n71. [Google Scholar] [CrossRef] [PubMed]
- Perez, A., Gaehle, K., Sobczak, B., & Stein, K. (2022). Virtual simulation as a learning tool for teaching graduate nursing students to manage difficult conversations. Clinical Simulation in Nursing, 62, 66–72. [Google Scholar] [CrossRef]
- Peters, M. D. J., Godfrey, C., McInerney, P., Khalil, H., Larsen, P., Marnie, C., Pollock, D., Tricco, A. C., & Munn, Z. (2022). Best practice guidance and reporting items for the development of scoping review protocols. JBI Evidence Synthesis, 20((4)), 953–968. [Google Scholar] [CrossRef] [PubMed]
- Peters, M. D. J., Godfrey, C., McInerney, P., Munn, Z., Tricco, A. C., & Khalil, H. (2024). Scoping reviews (2020). In E. Aromataris, C. Lockwood, K. Porritt, B. Pilla, & Z. Jordan (Eds.), JBI manual for evidence synthesis. JBI. [Google Scholar] [CrossRef]
- Plotzky, C., Lindwedel, U., Sorber, M., Loessl, B., Konig, P., Kunze, C., Kugler, C., & Meng, M. (2021). Virtual reality simulations in nurse education: A systematic mapping review. Nurse Education Today, 101, 104868. [Google Scholar] [CrossRef] [PubMed]
- Rim, D., & Shin, H. (2021). Effective instructional design template for virtual simulations in nursing education. Nurse Education Today, 96, 104624. [Google Scholar] [CrossRef]
- Samosorn, A. B., Gilbert, G. E., Bauman, E. B., Khine, J., & McGonigle, D. (2020). Teaching airway insertion skills to nursing faculty and students using virtual reality: A pilot study. Clinical Simulation in Nursing, 39, 18–26. [Google Scholar] [CrossRef]
- Serpa, L. F., & Netto, A. V. (2024). Percepção de enfermeiras educadoras sobre treinamento simulado utilizando realidade virtual aplicado aos alunos do curso de enfermagem. Revista Saúde em Redes, 10(1), 4267. [Google Scholar] [CrossRef]
- Shorey, S., & Ng, E. D. (2021). The use of virtual reality simulation among nursing students and registered nurses: A systematic review. Nurse Education Today, 98, 104662. [Google Scholar] [CrossRef] [PubMed]
- Tamilselvan, C., Chua, S. M., Chew, H. S. J., & Devi, M. K. (2023). Experiences of simulation-based learning among undergraduate nursing students: A systematic review and meta-synthesis. Nurse Education Today, 121, 105711. [Google Scholar] [CrossRef]
- Trevi, R., Chiappinotto, S., Palese, A., & Galazzi, A. (2024). Virtual reality for cardiopulmonary resuscitation healthcare professionals training: A systematic review. Journal of Medical Systems, 48(50), 50. [Google Scholar] [CrossRef]
- Tricco, A. C., Lillie, E., Zarin, W., O’Brien, K. K., Colquhoun, H., Levac, D., Moher, D., Peters, M. D., Horsley, T., Weeks, L., & Straus, S. E. (2018). PRISMA extension for scoping reviews: Checklist and explanation. Annals of Internal Medicine, 169(7), 467–473. [Google Scholar] [CrossRef] [PubMed]
- Ulrich, D., Farra, S., Smith, S., & Hodgson, E. (2014). The student experience using virtual reality simulation to teach decontamination. Clinical Simulation in Nursing, 10(11), 546–553. [Google Scholar] [CrossRef]
- Wood, J., Ebert, L., & Duff, J. (2022). Implementation methods of virtual reality simulation and the impact on confidence and stress when learning patient resuscitation: An integrative review. Clinical Simulation in Nursing, 66, 5–17. [Google Scholar] [CrossRef]
- Yang, J., Zhou, W. J., Zhou, S. C., Luo, D., Liu, Q., Wang, A. I., Yu, S. H., Shu, X. P., He, X. Y., Hu, F., Yang, B. X., & Chen, J. (2024). Integrated virtual simulation and face-to-face simulation for clinical judgment training among undergraduate nursing students: A mixed-methods study. BMC Medical Education, 24, 32. [Google Scholar] [CrossRef]
- Yee, A. (2023). Clinical decision-making in the intensive care unit: A concept analysis. Intensive and Critical Care Nursing, 77, 103430. [Google Scholar] [CrossRef]
| Data Sources | Search Query |
|---|---|
| Cumulative Index to Nursing and Allied Health Literature (CINAHL) | Nursing care AND Virtual Reality AND Intensive Care Units |
| Cochrane Library | “nursing care” in Title Abstract Keyword AND “virtual reality” in Title Abstract Keyword AND “intensive care unit” in Title Abstract Keyword |
| PubMed | ((“nursing care”[All Fields] OR “nursing care”[MeSH Terms]) AND (“virtual reality”[MeSH Terms] OR (“virtual reality”[All Fields]) AND (“intensive care units”[MeSH Terms] OR (“intensive care units”[All Fields])) |
| SciELO | ((TS = (Nursing care)) AND TS = (Virtual Reality)) AND TS = (Intensive Care Units) |
| Web of Science | ((ALL = (Nursing care)) AND ALL = (Virtual Reality)) AND ALL = (Intensive Care Units) |
| SCOPUS | (TITLE-ABS-KEY (Nursing care) AND TITLE-ABS-KEY (Virtual Reality) AND TITLE-ABS-KEY (Intensive Care Units)) |
| Science Direct | Nursing care AND Virtual Reality AND Intensive Care Units |
| CAPES Thesis and Dissertation Catalog | Nursing care AND Virtual Reality AND Intensive Care Units |
| Virtual Health Library (VHL) | (Nursing care) AND (Virtual Reality) AND (Intensive Care Units) |
| Embase | (“nursing”/exp OR nursing) AND virtual AND (“reality”/exp OR reality) AND intensive AND (“care”/exp OR care) AND units |
| Brazilian Digital Library of Theses and Dissertations (BDTD) | (All fields: Nursing care AND All fields: Virtual Reality AND All fields: Intensive Care Units) |
| Scientific Open Access Repository of Portugal (RCAAP) | Nursing care AND Virtual Reality AND Intensive Care Units |
| DART-Europe E-theses Portal | Nursing care AND Virtual Reality AND Intensive Care Units |
| (Author, Year)/Country | Study Design | Sample Size/Population | Interface Used | Content Addressed | Main Evidence |
|---|---|---|---|---|---|
| (Trevi et al., 2024)/Italy | Systematic Review | 1042 records identified, 15 included in the final sample/Not applicable (N/A) | 3D virtual scenario with a viewer | Cardiopulmonary resuscitation (CPR) training | High usability and participant satisfaction, improved skill performance, and knowledge retention. Reduced response time to the procedure and lower teaching costs. |
| (Wood et al., 2022)/Australia | Integrative Review | 859 articles identified, 5 included in the review (N/A) | Multi-user virtual world (MUVW) and vSim (avatars), virtual patients, head-mounted displays (HMDs) | Resuscitation | Development of leadership skills, team-based learning, and a positive impact on self-confidence were evident in resuscitation training. |
| (Bayram & Caliskan, 2019)/Turkey | Randomized Controlled Trial | Initial population of 238 students, with 86 remaining in the study/First-year nursing students | Game-based mobile VR application | Tracheostomy care | The experimental group showed higher performance in internal cannula cleaning and peristomal skin care skills, as well as a shorter time in the first execution. |
| (Brown et al., 2012)/Australia | Methodological Study—Prototype Application | (N/A)/ICU nurses | Virtual world with avatars + viewer (Open Simulator) | Patient handover during the first hour of an ICU shift | Pedagogical benefits included the development of listening skills, verbal articulation, synthesis and prioritization abilities, and acting with thoroughness in a complex environment. The prototype may also improve training quality, reduce costs, support teamwork training, and allow for contextualized scenarios. |
| (Babaita et al., 2024)/Japan | Randomized Clinical Trial | 62 students participated in the randomization/Third-year nursing students | 360° VR video and HMDs | Closed tracheal suctioning procedure (including oral suction) | Good usability, more interesting learning, immersion, and realism; allows students to reuse videos. No statistically significant difference between groups in psychomotor skill development, knowledge acquisition, or self-confidence. Over half of the participants reported motion sickness symptoms. |
| (Banville et al., 2023)/Canada | Descriptive Qualitative | 13 participants/Final-year nursing students | Virtual Care Unit (VCU) + viewer | Clinical surveillance competencies in critical care | Provided students with a sense of presence, allowing them to mentally anticipate care. Contributed to reduced stress levels, allowed for mistakes in a controlled environment, and stimulated increased concentration. |
| (Yang et al., 2024)/China | Mixed Methods | All 122 invited students participated/Third-year nursing students | vSim for Nursing (avatars)—Integrated Program | Enhancing clinical judgment in the ICU (acute pulmonary embolism) | Potential to enhance discovery and identification of critical learning points. Fosters interpretation, reflection, evaluation, and appropriate classification. The combination of vSim and in-person simulation improved clinical judgment, communication skills, operational interventions, and self-confidence. |
| (Tamilselvan et al., 2023)/Singapore | Systematic Review and Meta-synthesis | 5550 studies identified, 14 included/(N/A) | Viewer | Learning nursing care with VR | Promotes self-assessment of knowledge, motivates, and makes learning more effective and independent. Improves psychomotor competencies, decision-making, and self-confidence. Makes practice more memorable and allows for repeated practice without risk. |
| (Cheng et al., 2024)/Canada | Systematic Review | 1807 records identified, 13 included/(N/A) | 3D computer-simulated space | Basic and advanced life support training | Observed knowledge acquisition and retention, the opportunity to apply clinical reasoning and decision-making in scenarios, and promotion of training support. |
| (Plotzky et al., 2021)/Germany | Systematic Review | 13,945 records identified, 22 included in the final sample/(N/A) | 3D head-mounted displays (HMDs) | Auscultation, endotracheal suctioning, urinary catheterization, empathy, and emergency response | Studies identified the potential for procedure and skill training and providing immersion in situations difficult to replicate in traditional simulation. Makes teaching less stressful, increases self-efficacy, self-confidence, resilience, and enhances empathy. |
| (Kim & Seo, 2024)/Republic of Korea | Mixed Methods | 46 participants/Third-year nursing students | VIRTI application + 360-degree camera with HMDs | Intravenous (IV) therapy training with an infusion pump | Improved motivation to transfer learning, self-efficacy, confidence, and skills. Enabled repetitive training in an autonomous, proactive, and psychologically safe environment. Reported a sense of presence, immersion, and expectations of enhanced long-term memory. Physical side effects were noted. |
| (Harmon et al., 2021)/Australia | Scoping Review | 2841 articles identified, 4 included/(N/A) | Serious gaming and avatars | Pain education | Promotes decision-making in a realistic and safe environment and the ability to progress and improve knowledge. VR can lead to stress, eye strain, and cybersickness. |
| (Samosorn et al., 2020)/United States | Pilot Study | 31 participants/Nursing faculty and students | Virtual Oculus Rift + Touch | Airway management of an apneic and unresponsive patient | Increased knowledge and its effective transmission and the possibility of self-guided learning. VR can be positive across clinical disciplines but is not suggested to replace clinical encounters. Participants did not experience significant motion sickness. |
| (Hall et al., 2024)/Australia | Single-arm Repeated Measures Study | 79 students participated out of 219/Nursing students | VirtualU End of Life Care + 360° Video + VR goggles | Communication skills in “end-of-life care” | Improved self-assessment of knowledge, skills, and behaviors. Promoted highly beneficial and unique learning with effective engagement. Provided psychological safety for making mistakes and open discussions. Some reported discomfort, dizziness, and anxiety. |
| (Perez et al., 2022)/United States | Mixed Methods | 105 participants/Master’s and doctoral nursing students | Mursion (virtual environment and avatars) | Managing difficult conversations | Enabled management of difficult conversations and increased communication confidence. Anxiety and nervousness before the simulation were reported. |
| (Rim & Shin, 2021)/Republic of Korea | Methodological Study | 16 students participated/Nursing students | Unity 3D and Second Life platforms (avatars) | Neonatal apnea, hypoglycemia, and transfusion | Allows multiple practice attempts, independent knowledge construction, and emotional adaptation and self-regulation in unfamiliar situations. |
| (García-Pazo et al., 2023)/Spain | Cross-sectional Study | Purposive sample of 175 students/Third-year nursing students | 360° video + HMDs | Assessment of critical patients | Good usability that allows for scenario review and improves students’ perception of their skill acquisition, as well as understanding of the ICU environment and required technology. Observed learning in skin/mucous hygiene, patient mobilization, and empathy. |
| (Chao et al., 2021)/Taiwan | Randomized Clinical Trial | 47 participants recruited, 45 participated/Nursing students > 20 years with no prior nasogastric tube feeding skills | HMDs + immersive 3D video + VIVEPAPER | Nasogastric tube feeding | Improved knowledge, confidence, and satisfaction with the learning method. Exam scores in the intervention group were higher. Mild dizziness was reported but did not affect learning. |
| (Botha et al., 2021)/South Africa | Not Specified | 34 students volunteered, 6 in pilot test, 28 in final analysis/Nursing students | HMDs + Oculus Rift | Management of a patient with a foreign body airway obstruction | The system was genuinely usable with no task failures. Students had a very positive and satisfying experience, finding the system realistic and interactive with good usability. However, some reported dizziness and nausea. |
| (Y. M. Chang & Lai, 2021)/Republic of China | Qualitative research design and focus group interview | 60 students selected from 90 potential participants/Nursing students | HMD, motion sensors, and hand controls (HTC VIVE) | Nasogastric tube feeding | Good adaptation and usability of the virtual environment, though it required time. Students could learn from their mistakes and manage their own learning progress without stress. VR offers cost savings and the possibility of repeated practice. |
| (Kuyt et al., 2021)/United Kingdom | Scoping Review | 696 articles identified, 42 selected for the final sample/(N/A) | Not specified | CPR | Great potential as a blended learning strategy, useful for training and increasing confidence. No improvement in skill was noted, but there was greater knowledge application and engagement. No studies addressed the influence of training on patient outcomes. |
| (Hubail et al., 2022)/United Kingdom | Randomized Controlled Trial | 42 participants contacted, 26 attended, 7 withdrew/Adults > 18 with no prior CPR course or one taken >1 year ago | VR headset and hand sensors (HTC Vive) | CPR | CPR skill acquisition was comparable in both groups. Participants indicated a preference for hands-on training. The traditional group had a greater gain in knowledge and confidence. The VR content had clear instructions and useful feedback, leading to a positive experience. |
| (Butt et al., 2018)/United States | Mixed Methods | 20 students participated out of 36 recruited/Fifth- and sixth-semester nursing students | 3D helmets (Oculus Rift) and haptic devices (interactive glove) | Urinary catheterization | Good usability, opportunity for repeated practice, and stimulation of practice and self-confidence. Assisted in correct catheter insertion and memorization of procedural steps. The ability to demonstrate sterile technique was equal for both groups. |
| (Y. Y. Chang et al., 2024)/Taiwan | Mixed Methods | 35 students in Phase I; 128 participants in Phase II (out of 146)/Second-year nursing students | Oculus Rift headset | IV injection | Increased knowledge, motivation, memorization of skills and processes, and a sense of realism. Some steps were challenging, including smoothness of the VR, needle positioning, and patient communication. |
| (Ulrich et al., 2014)/United States | Mixed Methods | 107 students participated/Senior baccalaureate nursing students, >18 years, English-speaking | Computer monitor + Microsoft Kinect webcam | Decontamination | Sense of realism, ability to make mistakes without patient harm, and feeling of safety from contamination. Improved memory. |
| (Al-Mugheed et al., 2022)/Cyprus | Experimental | 126 students met the inclusion criteria out of 135/Third- and fourth-level nursing students | Not specified | Standard precautions | More significant results in knowledge, attitude, and compliance with standard precautions. Provided the opportunity to repeat practice multiple times, translating knowledge into practice, and preparing for professional life. |
| (Lee & Han, 2022)/South Korea | Quasi-experiment | 66 students selected, 60 participated/Nursing students with no prior VR simulation experience with mechanical ventilation | VR goggles | Mechanical ventilation | No significant difference in knowledge between groups. Greater immersion and learning satisfaction, improved clinical decision-making, critical thinking, perception, and effective for increasing self-efficacy. |
| Pattern (Type of Impact) | Advances | Gaps | Evidence for Practice | Research Recommendations |
|---|---|---|---|---|
| Increased knowledge | The use of VR led to greater knowledge acquisition, effectively linking theory with practice. | Lack of real-world interaction and absence of authentic emotional elements in clinical contexts; dependency on connectivity and need for technological adaptation. | Studies show increased knowledge retention, better comprehension of content, and greater student motivation in virtual environments. | Conduct longitudinal research to assess the long-term impact of continuous VR use on learning and develop technological solutions that increase realism and accessibility. |
| Improved self-confidence | Virtual environments allow for errors without risk to the patient, promoting psychological safety and self-confidence in skill performance. | Difficulty in initial adaptation to technological interfaces and simulation-related anxiety, especially among students with less digital familiarity. | Reports indicate increased self-confidence in procedure execution and a greater willingness to face practical challenges after VR training. | Implement emotional support and pre-training strategies to reduce barriers and facilitate student adaptation to VR; evaluate the impact on different student profiles. |
| Development of critical thinking | VR fosters reflection, evaluation, and classification of complex situations, stimulating decision-making and clinical judgment. | Need for more realistic and interactive scenarios to better simulate critical situations and enhance the development of clinical reasoning. | Significant improvement in analytical and problem-solving abilities, with immediate feedback that potentiates the development of critical thinking. | Develop more complex and realistic scenarios; evaluate the impact of VR on critical thinking development in different clinical contexts and on a larger scale. |
| Enhancement of technical skills | Provides repetitive practical training, development of psychomotor skills, leadership, and communication. | Few simulations with haptic devices; limitations in reproducing advanced psychomotor skills; insufficient time provided to learn the VR technology beforehand. | Proven effectiveness in technical skill acquisition, with performance similar to or superior to traditional methods in certain procedures. | Invest in haptic technologies, improve simulator fidelity to broaden the development of technical skills in virtual environments, and provide more time for users to familiarize themselves with the technology. |
| Strengthening of practice safety | The controlled environment reduces physical and emotional risks during learning and promotes safety for practice and error-making. | Absence of the psychological pressure typical of real scenarios, which can impact preparation for high-risk situations. Additionally, physical symptoms like nausea and dizziness can compromise user safety. | Studies indicate that VR contributes to learning safety by reducing risks associated with traditional practical training, thereby increasing students’ confidence in performing procedures. | Deepen research on the impact of physical symptoms on user safety and develop strategies to minimize these adverse effects. Explore ways to incorporate elements of emotional realism and psychological pressure to better prepare students for real-world scenarios. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Souza, L.L.; Ozorio Dutra, S.V.; da Silva Filho, J.A.A.; Silva, L.F.; Mourão, V.G.; Dantas, D.V.; Dantas, R.A.N.; Ribeiro, K.R.B. Virtual Reality in Critical Care Nursing Education: A Scoping Review. Educ. Sci. 2025, 15, 1258. https://doi.org/10.3390/educsci15091258
Souza LL, Ozorio Dutra SV, da Silva Filho JAA, Silva LF, Mourão VG, Dantas DV, Dantas RAN, Ribeiro KRB. Virtual Reality in Critical Care Nursing Education: A Scoping Review. Education Sciences. 2025; 15(9):1258. https://doi.org/10.3390/educsci15091258
Chicago/Turabian StyleSouza, Laura Lima, Samia Valeria Ozorio Dutra, José Aguinaldo Alves da Silva Filho, Lucas Ferreira Silva, Vanessa Gomes Mourão, Daniele Vieira Dantas, Rodrigo Assis Neves Dantas, and Kátia Regina Barros Ribeiro. 2025. "Virtual Reality in Critical Care Nursing Education: A Scoping Review" Education Sciences 15, no. 9: 1258. https://doi.org/10.3390/educsci15091258
APA StyleSouza, L. L., Ozorio Dutra, S. V., da Silva Filho, J. A. A., Silva, L. F., Mourão, V. G., Dantas, D. V., Dantas, R. A. N., & Ribeiro, K. R. B. (2025). Virtual Reality in Critical Care Nursing Education: A Scoping Review. Education Sciences, 15(9), 1258. https://doi.org/10.3390/educsci15091258








