Relevance of Social Medicine Skills and the Role of Teaching Formats in the Perception of Medical Students: A Retrospective Trend Study
Abstract
1. Introduction
1.1. The Role of Social Medicine
1.2. Social Medicine in Teaching
1.3. Aims
- In all subject areas, social medicine teaching leads to a self-assessed increase in knowledge.
- PBL is superior to PT in terms of student competence growth.
2. Materials and Methods
2.1. Study Design
2.2. Characteristics of the Teaching Format
- Topic 1: work incapacity
- Topic 2: rehabilitation
- Topic 3: (long-term) care level
- Topic 4: graded return to work
- Topic 5: assistive technology for activities of daily living
- Topic 1: work incapacity
- Topic 2: rehabilitation
- Topic 4: graded return to work
2.3. Survey
2.4. Statistics
- students who worked on the topic themselves (group PBL),
- those who only listened to the fellow students’ presentation (group PT).
3. Results
3.1. Response Rate and Description of Seminar Participants
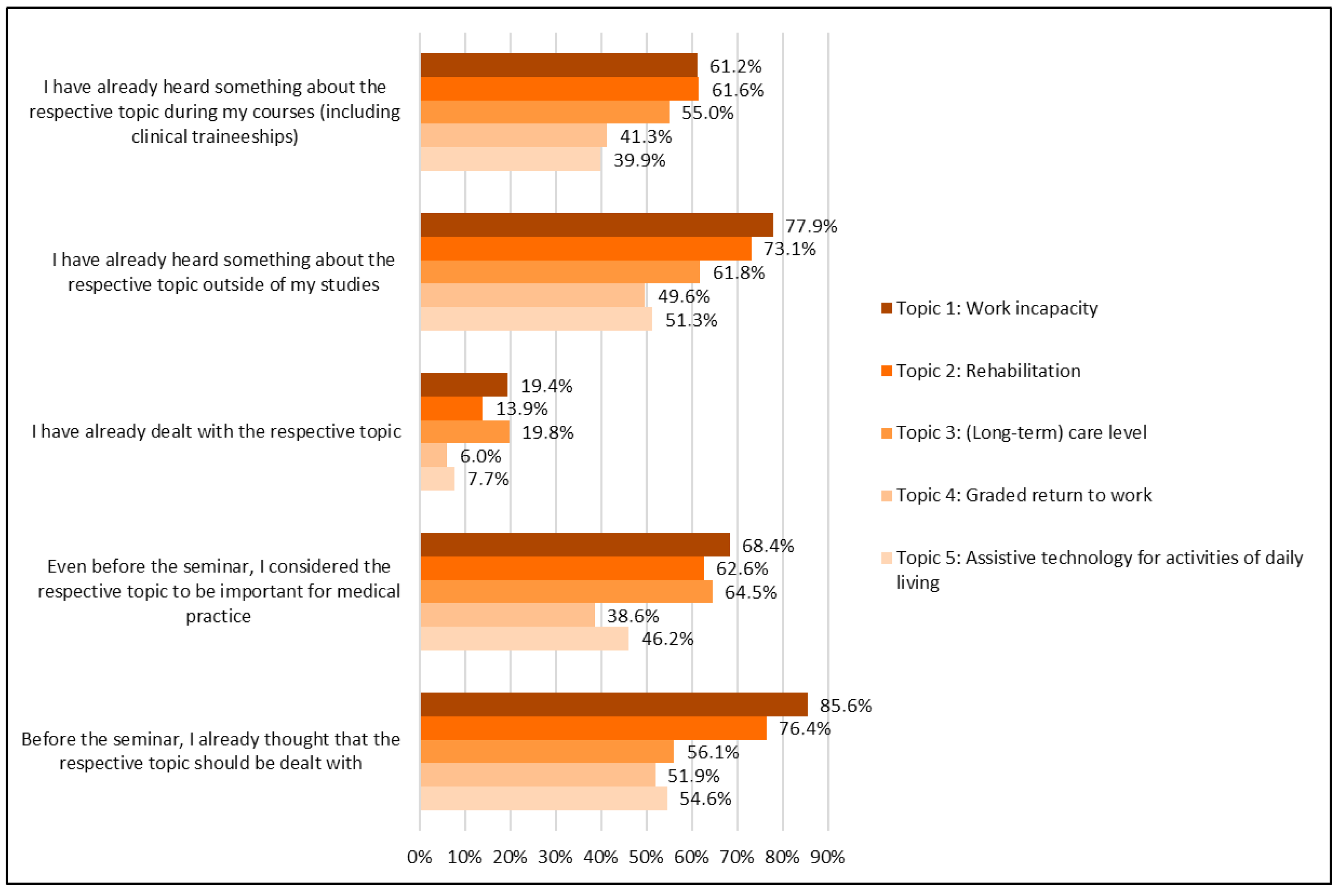
3.2. Part I: Previous Knowledge and Perceived Relevance of the Topics
3.3. Part II: Impact of the Teaching Format
3.3.1. Learning Effects Associated with the PBL Approach Regarding a Specific Topic
- Direct engagement with the topic (group PBL) led to significantly higher ratings of knowledge increase compared to students in group PT, who received information on the respective topic from the presentations by participants in group PBL. The comparison of the effect of both teaching approaches resulted in a small ES in topic 1 (0.25), moderate in topic 2 (0.49) and topic 3 (0.38), and high in topic 4 (0.66) and topic 5 (0.55).
- In addition, the feeling of being well-prepared for a later practical action was significantly higher in group PBL than group PT for topics 2, 3, 4, and 5, with moderate (topic 2 = 0.33; topic 4 = 0.42; topic 5 = 0.42) or high (topics 3 = 0.54) effects.
- Significantly higher perceptions of relevance in group PBL (“the topic seems to me to be more important for the medical activity after the seminar than before”) were noted for topics 2, 4, and 5, with a small ES for topic 2 (0.18) and topic 5 (0.26) and a moderate ES for topic 4 (0.40).
3.3.2. Perception of Knowledge Gain, Fitness for Medical Practice and Relevance of the Issue Depending on the Extent of Engagement with the Topic During the Seminar
4. Discussion
4.1. Main Results
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ADL | Assistive technology to support activities of daily living |
| CI | Confidence interval |
| DGSMP | Deutsche Gesellschaft für Sozialmedizin und Prävention (=German Association for Social Medicine and Prevention) |
| ES | Effect sizes |
| G-BA | Gemeinsamer Bundesausschuss (=Federal Joint Committee) |
| LTC | Long-term care |
| MD | Median |
| NKLM | Nationaler Kompetenzbasierter Lernzielkatalog Medizin (=German National Competence-Based Catalogues of Learning Objectives in Medicine |
| OR | Odds Ratio |
| PBL | Problem-based learning |
| PT | Peer Teaching |
| SD | Standard deviation |
| WHO | Word Health Organization |
Appendix A





References
- Andermann, A., & CLEAR Collaboration. (2016). Taking action on the social determinants of health in clinical practice: A framework for health professionals. CMAJ: Canadian Medical Association Journal = Journal de l’Association Medicale Canadienne, 188(17–18), E474–E483. [Google Scholar] [CrossRef] [PubMed]
- Baumann, W., Heipertz, W., Schliehe, F., & van Essen, J. (2001). Herausforderungen der sozial-medizinischen Beratung und Begutachtung [Challenges of social-medical consultation and assessment]. Gesundheitswesen, 63(Suppl. S1), 35–38. [Google Scholar] [CrossRef] [PubMed]
- Behmann, M., Bisson, S., & Walter, U. (2011). Social medicine in medical faculties: Realisation of the topic in the specialty “social medicine, occupational health”. Gesundheitswesen, 73, 853–885. [Google Scholar] [CrossRef]
- Benè, K. L., & Bergus, G. (2014). When learners become teachers: A review of peer teaching in medical student education. Family Medicine, 46(10), 783–787. [Google Scholar]
- Bhugra, D. (2006). All medicine is social. Journal of the Royal Society of Medicine, 107(5), 183–186. [Google Scholar] [CrossRef]
- Brennecke, R., Boschek, H. J., Geraedts, M., Scheidig, C., Swart, E., & Walter, U. (2006). Deutsche Gesellschaft für Sozialmedizin und Prävention (DGSMP) Sozialmedizinischer Stoffkatalog für die ärztliche AppO vom 27.6.2002 [German Society for Social Medicine and Prevention (DGSMP) Social medical substance catalogue for the medical AppO of 27.6.2002]. Gesundheitswesen, 68, 48–64. [Google Scholar]
- Bundesanstalt für Arbeitschutz und Arbeitsmedizin (BAUA). (2023). Volkswirtschaftliche Kosten durch Arbeitsunfähigkeit 2023. Available online: https://www.baua.de/DE/Themen/Monitoring-Evaluation/Zahlen-Daten-Fakten/Kosten-der-Arbeitsunfaehigkeit (accessed on 10 October 2025).
- Bühner, M., & Ziegler, M. (2017). Statistik für psychologen und sozialwissenschaftler [Statistics for psychologists and social scientists] (2nd ed.). Pearson. [Google Scholar]
- Davari, F. V., Teymouri, F., Amoli, H. A., Mojtabavi, H., Sharifi, A., Alaeddini, F., Ashouri, M., Zabihi, H., Shariatpanahi, G., & Zafarghandi, M. (2021). Problem-based learning as an effective method for teaching theoretical surgery courses to medical students. Journal of Education and Health Promotion, 10, 477. [Google Scholar] [CrossRef] [PubMed]
- De Jong, Z., van Nies, J. A., Peters, S. W., Vink, S., Dekker, F. W., & Scherpbier, A. (2010). Interactive seminars or small group tutorials in preclinical medical education: Results of a randomized controlled trial. BMC Medical Education, 10, 79. [Google Scholar] [CrossRef]
- Dharamsi, S., Ho, A., Spadafora, S. M., & Woollard, R. (2011). The physician as health advocate: Translating the quest for social responsibility into medical education and practice. Academic Medicine, 86(9), 1108–1113. [Google Scholar] [CrossRef]
- Doobay-Persaud, A., Adler, M. D., Bartell, T. R., Sheneman, N. E., Martinez, M. D., Mangold, K. A., Smith, P., & Sheehan, K. M. (2019). Teaching the social determinants of health in undergraduate medical education: A scoping review. Journal of General Internal Medicine, 34(5), 720–730. [Google Scholar] [CrossRef]
- Drexel, H., Vonbank, A., Fraunberger, P., Riesen, W. F., & Saely, C. H. (2015). Toward a more professional and practical medical education: A novel Central European approach. Advances in Medical Education and Practice, 6, 459–467. [Google Scholar] [CrossRef]
- Frank, J. R. (Ed.). (2005). The CanMEDS 2005 physician competency framework. Better standards. Better physicians. Better care. The Royal College of Physicians and Surgeons of Canada. [Google Scholar]
- German Pension Insurance. (2024). Reha-Bericht 2024. Available online: https://www.deutsche-rentenversicherung.de/SharedDocs/Downloads/DE/Statistiken-und-Berichte/Berichte/rehabericht_2024.html (accessed on 10 October 2025).
- German Science Council. (2014). Empfehlungen zur weiterentwicklung des medizinstudiums in deutschland auf der grundlage einer bestandsaufnahme der humanmedizinischen modellstudiengänge [Recommendations for the further development of medical study courses in Germany on the basis of an inventory of the model study programmes in human medicine]. G-BA. Available online: http://www.wissenschaftsrat.de/download/archiv/4017-14.pdf (accessed on 20 October 2021).
- Goyal, R. K., Dawson, C. A., Epstein, S. B., Brach, R. J., Finnie, S. M., Lounsbury, K. M., Lahey, T., & Eldakar-Hein, S. T. (2021). The design and implementation of a longitudinal social medicine curriculum at the University of Vermont’s Larner College of Medicine. BMC Medical Education, 21(1), 131. [Google Scholar] [CrossRef]
- Graf, J., Smolka, R., Simoes, E., Zipfel, S., Junne, F., Holderried, F., Wosnik, A., Doherty, A. M., Menzel, K., & Herrmann-Werner, A. (2017). Communication skills of medical students during the OSCE: Gender-specific differences in a longitudinal trend study. BMC Medical Education, 17(1), 75. [Google Scholar] [CrossRef] [PubMed]
- Graf, J., Weinert, K., Abele, H., & Kranz, A. (2025). How self-determined are reproductive decisions? Sociological aspects of pregnancy, birth, and breastfeeding: Implications for midwifery practice—A narrative review. Healthcare, 13(13), 1540. [Google Scholar] [CrossRef] [PubMed]
- Hattie, J. (2009). Visible learning: A synthesis of 800+ meta-analyses on achievement. Routledge. [Google Scholar]
- Hildenbrand, S., & Rieger, M. A. (2011). Berufskrankheiten-Fallseminar—Neues Lehrformat für Studierende im Fach Arbeitsmedizin [Occupational disease case seminar—New teaching format for students of occupational medicine]. In Dokumentation über die 51. Jahrestagung, Deutsche Gesellschaft für Arbeitsmedizin und Umweltmedizin e.V., 9. bis 12. März 2011 [Documentation on the 51st annual conference, german society for occupational and environmental medicine, 9 to 12 March 2011] (pp. 710–712). DGAUM. [Google Scholar]
- Hildenbrand, S., Völter-Mahlknecht, S., Simoes, E., Luntz, E., Graf, J., & Rieger, M. A. (2014, September 25–27 DocP123. ). Entwicklung eines neuen Lehrformats: Vermittlung sozialmedizinischer Skills im Humanmedizin-Studium [Development of a new teaching format: Teaching social-medical skills in study course of medicine]. Jahrestagung der Gesellschaft für Medizinische Ausbildung (GMA), Hamburg, Germany. [Google Scholar]
- Hoffman, B. D., Barnes, M., Ferrell, C., Gellin, C., Lichtenstein, C., Donnelly, J., Kaczorowski, J., & CHAMP Study Group. (2016). The community health and advocacy milestones profile: A novel tool linking community pediatrics and advocacy training to assessment of milestones-based competence in pediatric residency training. Academic Pediatrics, 16(4), 309–313. [Google Scholar] [CrossRef]
- Holtz, T. H., Holmes, S. M., Stonington, S., & Eisenberg, L. (2006). Health is still social: Contemporary examples in the age of the genome. PLoS Medicine, 3(10), e419. [Google Scholar] [CrossRef]
- Kraft, M. (2020). Interpreting effect sizes of education interventions. Educational Researcher, 49(4). [Google Scholar] [CrossRef]
- Long-Bellil, L. M., Robey, K. L., Graham, C. L., Minihan, P. M., Smeltzer, S. C., Kahn, P., & Alliance for Disability in Health Care Education. (2011). Teaching medical students about disability: The use of standardized patients. Academic Medicine: Journal of the Association of American Medical Colleges, 86(9), 1163–1170. [Google Scholar] [CrossRef]
- Ma, Y., & Lu, X. (2019). The effectiveness of problem-based learning in pediatric medical education in China: A meta-analysis of randomized controlled trials. Medicine, 98(2), e14052. [Google Scholar] [CrossRef]
- Martinez, I. L., Artze-Vega, I., Wells, A. L., Mora, J. C., & Gillis, M. (2015). Twelve tips for teaching social determinants of health in medicine. Medical Teacher, 37(7), 647–652. [Google Scholar] [CrossRef]
- Medizinischer Fakultätentag der Bundesrepublik Deutschland e. V. (2015). Nationaler kompetenzbasierter lernzielkatalog medizin (NKLM) [National competency-based catalogue of learning objectives for medicine]. Available online: https://medizinische-fakultaeten.de/wp-content/uploads/2021/06/nklm_final_2015-12-04.pdf (accessed on 31 August 2024).
- Medizinischer Fakultätentag der Bundesrepublik Deutschland e. V. (2021). Nationaler kompetenzbasierter lernzielkatalog medizin (NKLM), Version NKLM 2.0 [National competency-based catalogue of learning objectives for medicine]. Available online: https://nklm.de (accessed on 31 August 2024).
- Muschalla, B., Baron, S., & Klevers, T. (2022). Students or medical professionals: Whose knowledge improved after social-medicine training? Results from a quasi-experimental evaluation study. Social Psychiatry and Psychiatric Epidemiology, 57(7), 1505–1514. [Google Scholar] [CrossRef]
- Ortega, L. M., Westerhaus, M. J., Finnegan, A., Bhatt, A., Owilli, A. O., Turigye, B., & Louis, Y. E. (2023). Toward an integrated framework in health and human rights education: Transformative pedagogies in social medicine, collective health, and structural competency. Health and Human Rights, 25(1), 105–117. [Google Scholar]
- Pearson, M., Barker, A. M., Battistone, M. J., Bent, S., Odden, K., & O’Brien, B. (2020). Implementing an established musculoskeletal educational curriculum in a new context: A study of effectiveness and feasibility. Medical Education Online, 25(1), 1760466. [Google Scholar] [CrossRef] [PubMed]
- Prakash, P. (2005). Where is the woman in preventive and social medicine? Sociological perspectives. Economic and Political Weekly, 40(18), 1828–1834. [Google Scholar]
- Rothgang, H., Iwansky, S., Müller, R., Sauer, S., & Unger, R. (2011). BARMER GEK nursing report 2011 (Vol. 11). University of Bremen, Centre for Social Policy; Asgard-Verlag. [Google Scholar]
- Savery, J. R. (2015). Overview of Problem-Based Learning: Definitions and Distinctions. In W. Andrew, L. Heather, C. Hmelo-Silver, & P. Ertmer (Eds.), Essential readings in problem-based learning: Exploring and extending the legacy of Howard S. Barrows (pp. 5–15). Purdue University Press. [Google Scholar] [CrossRef]
- Schaeffer, D., Berens, E. M., & Vogt, D. (2017). Health literacy in the German population-results of a representative survey. Deutsches Arzteblatt International, 114, 53–60. [Google Scholar]
- Schliehe, F. (2005). Praktische sozialmedizin und rehabilitation—Zur entwicklung und den herausforderungen eines fachbereiches [Practical social medicine and rehabilitation-on the development and challenges of a specialty department]. Gesundheitswesen, 67(2), 74–80. [Google Scholar] [CrossRef]
- Siegel, J., Coleman, D. L., & James, T. (2018). Integrating social determinants of health into graduate medical education: A call for action. Academic Medicine, 93(2), 159–162. [Google Scholar] [CrossRef] [PubMed]
- Simoes, E., Graf, J., Wallwiener, D., & Brucker, S. Y. (2015). Conflicting priorities in social legislation and medicine: Gynaeco-oncology patients and their right to participate in society. Geburtshilfe Frauenheilkunde, 75(10), 1069–1074. [Google Scholar] [CrossRef]
- Simoes, E., Hildenbrand, S., & Rieger, M. A. (2012). (Inter)national and regional health goals in academic social-medical education conception for teaching medical students at the eberhard karls university tuebingen. Gesundheitswesen, 74(07), 442–448. [Google Scholar] [PubMed]
- Simoes, E., Sokolov, A. N., Graf, J., Pavlova, M. A., Brucker, S. Y., Wallwiener, D., Schmahl, F. W., & Bamberg, M. (2016). Why strive after clinical social medicine? From epidemiological association to personalized social medicine: A case of breast cancer care. Gesundheitswesen, 78(2), 97–102. [Google Scholar] [CrossRef]
- Stonington, S., & Holmes, S. M. (2006). Social medicine in the twenty-first century. PLoS Medicine, 3(10), e445. [Google Scholar] [CrossRef]
- Symons, A. B., McGuigan, D., & Akl, E. A. (2009). A curriculum to teach medical students to care for people with disabilities: Development and initial implementation. BMC Medical Education, 9, 78. [Google Scholar] [CrossRef] [PubMed]
- Trullàs, J. C., Blay, C., Sarri, E., & Pujol, R. (2022). Effectiveness of problem-based learning methodology in undergraduate medical education: A scoping review. BMC Medical Education, 22(1), 104. [Google Scholar] [CrossRef] [PubMed]
- Vanderbilt, A. A., Baugh, R. F., Hogue, P. A., Brennan, J. A., & Ali, I. I. (2016). Curricular integration of social medicine: A prospective for medical educators. Medical Education Online, 21, 30586. [Google Scholar] [CrossRef]
- van Muijen, P. M., Duijts, S. F., Kornet-van der Aa, D. A., van der Beek, A. J., & Anema, J. R. (2015). Work disability assessment of cancer survivors: Insurance physicians’ perspectives. Occupational Medicine (Oxford, England), 65(7), 558–563. [Google Scholar] [CrossRef]
- Völter-Mahlknecht, S., Hildenbrand, S., Simoes, E., Luntz, E., Graf, J., & Rieger, M. A. (2014). Teaching social medical skills to students of human medicine—A workshop report. Gesundheitswesen, 76(8/9), s605–s606. [Google Scholar]
- Westerhaus, M., Finnegan, A., Haidar, M., Kleinman, A., Mukherjee, J., & Farmer, P. (2015). The necessity of social medicine in medical education/2015. Academic Medicine, 90(5), 565–568. [Google Scholar] [CrossRef] [PubMed]
- Wilhite, J. A., Hardowar, K., Fisher, H., Porter, B., Wallach, A. B., Altshuler, L., Hanley, K., Zabar, S. R., & Gillespie, C. C. (2020). Clinical problem solving and social determinants of health: A descriptive study using unannounced standardized patients to directly observe how resident physicians respond to social determinants of health. Diagnosis (Berlin, Germany), 7(3), 313–324. [Google Scholar] [CrossRef]
- Woodward, C. A. (1996). Problem-based learning in medical education: Developing a research agenda. Advances in Health Sciences Education, 1, 83–94. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. (2010). Guidelines for preventive and social medicine/community medicine/community health curriculum in the undergraduate medical education. WHO. [Google Scholar]
- Worringen, U., Hoppe, A., Derra, C., Kalwa, M., & Brüggemann, S. (2016). Nutzen des curriculums “Sozialmedizinische leistungsbeurteilung im reha-team” für die rehabilitationspraxis [Benefits of the curriculum “social medicine for the rehabilitation team” in rehabilitation practise]. Die Rehabilitation, 55(4), 238–247. [Google Scholar] [CrossRef]
- Xiong, X., Xu, J., Luo, M., Niu, D., Bi, Q., Wang, Z., & Zhang, J. (2025). Efficacy of problem-based learning combined with case-based learning versus lecture-based learning in orthopedic education: A systematic review and meta-analysis. BMC Medical Education, 25(1), 1357. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H., Liao, A. W. X., Goh, S. H., Wu, X. V., & Yoong, S. Q. (2022). Effectiveness of peer teaching in health professions education: A systematic review and meta-analysis. Nurse Education Today, 118, 105499. [Google Scholar] [CrossRef] [PubMed]

| Questionnaire |
|---|
| Part I: Previous knowledge of the topics and their perceived theoretical and practical relevance (perspective: retrospectively: before the seminar). |
| Students answered the following questions in the questionnaire for each of the topics covered in the seminar (check if applicable) (1) |
| I have already heard something about the respective topic during my courses (including clinical traineeships) |
| I have already heard something about the respective topic outside of my studies |
| I have already dealt with the respective topic |
| Even before the seminar, I considered the respective topic to be important for medical practice |
| Before the seminar, I already thought that the respective topic should be dealt with |
| Part II: Effects on knowledge, perception of feeling well-prepared for a later practical action, and perceived relevance of the topics (perspective: after the seminar). |
| Students answered the following questions in the questionnaire for each of the topics covered in the seminar (5-point Likert scale) (2) |
| My knowledge on this subject has increased considerably |
| I feel well-prepared for a later practical action on this topic |
| The topic seems to me to be more important for medical practice now than before the seminar |
| Topic No. | PBL: n (% of Sample) |
|---|---|
| 1. Work incapacity | 119 (22.5%) |
| 2. Rehabilitation | 113 (21.3%) |
| 3. (Long-term) care level | 91 (17.1%) |
| 4. Graded return to work | 117 (22.1%) |
| 5. Assistive technology for activities of daily living | 91 (17.1%) |
| Topic No. | Mean Score (SD); Median |
|---|---|
| 1. Work incapacity | 0.62 (0.48); 1 |
| 2. Rehabilitation | 0.58 (0.49); 1 |
| 3. (Long-term) care level | 0.51 (0.50); 1 |
| 4. Graded return to work | 0.37 (0.48); 0 |
| 5. Assistive technology for activities of daily living | 0.40 (0.49); 0 |
| Means (Standard Deviations) | n Valid | p Value | Effect Size 1 | |||
|---|---|---|---|---|---|---|
| Topic | Group PBL | Group PT | Total | |||
| 1. Work incapacity | 3.32 (1.09) | 3.13 (1.07) | 3.17 (1.08) | 517 | 0.037 * | 0.18 |
| 2. Rehabilitation | 3.46 (1.08) | 3.10 (1.00) | 3.18 (1.02) | 516 | <0.001 * | 0.35 |
| 3. (Long-term) care level | 3.43 (1.25) | 3.11 (1.01) | 3.17 (1.07) | 469 | 0.030 * | 0.28 |
| 4. Graded return to work | 3.62 (1.13) | 3.09 (1.01) | 3.21 (1.06) | 509 | <0.001 * | 0.49 |
| 5. Assistive technology for activities of daily living | 3.45 (1.13) | 3.04 (1.02) | 3.13 (1.05) | 469 | <0.001 * | 0.36 |
| Items | 1. Work Incapacity | 2. Rehabilitation | 3. (Long-Term) Care Level | 4. Graded Return to Work | 5. Assistive Technology (for ADLs) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | OR | 95%-CI | n | OR | 95%-CI | n | OR | 95%-CI | n | OR | 95%-CI | n | OR | 95%-CI | |
| My knowledge on this subject has increased considerably | 520 | 1.30 | [1.07; 1.58] * | 520 | 1.76 | [1.41; 2.20] * | 470 | 1.56 | [1.25; 1.94] * | 510 | 1.95 | [1.57; 2.42] * | 469 | 1.83 | [1.45; 2.31] * |
| I feel well-prepared for a later practical action on this topic | 520 | 1.20 | [0,98; 1.46] | 519 | 1.48 | [1.19; 1.83] * | 471 | 1.82 | [1.45; 2.30] * | 511 | 1.55 | [1.26; 1.91] * | 470 | 1.61 | [1.28; 2.01] * |
| The topic seems to me to be more important for medical practice now than before the seminar | 517 | 1.12 | [0.94; 1.33] | 516 | 1.27 | [1.05; 1.53] * | 469 | 1.06 | [0.88; 1.29] | 509 | 1.40 | [1.15; 1.71] * | 469 | 1.28 | [1.05; 1.56] * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hildenbrand, S.; Graf, J.; Michaelis, M.; Wagner, A.; Völter-Mahlknecht, S.; Simoes, E.; Rieger, M.A. Relevance of Social Medicine Skills and the Role of Teaching Formats in the Perception of Medical Students: A Retrospective Trend Study. Educ. Sci. 2025, 15, 1408. https://doi.org/10.3390/educsci15101408
Hildenbrand S, Graf J, Michaelis M, Wagner A, Völter-Mahlknecht S, Simoes E, Rieger MA. Relevance of Social Medicine Skills and the Role of Teaching Formats in the Perception of Medical Students: A Retrospective Trend Study. Education Sciences. 2025; 15(10):1408. https://doi.org/10.3390/educsci15101408
Chicago/Turabian StyleHildenbrand, Sibylle, Joachim Graf, Martina Michaelis, Anke Wagner, Susanne Völter-Mahlknecht, Elisabeth Simoes, and Monika A. Rieger. 2025. "Relevance of Social Medicine Skills and the Role of Teaching Formats in the Perception of Medical Students: A Retrospective Trend Study" Education Sciences 15, no. 10: 1408. https://doi.org/10.3390/educsci15101408
APA StyleHildenbrand, S., Graf, J., Michaelis, M., Wagner, A., Völter-Mahlknecht, S., Simoes, E., & Rieger, M. A. (2025). Relevance of Social Medicine Skills and the Role of Teaching Formats in the Perception of Medical Students: A Retrospective Trend Study. Education Sciences, 15(10), 1408. https://doi.org/10.3390/educsci15101408






