1. Introduction
For well over a century now, US medical education has carried an urgency to reform [
1,
2]. In May 1893, the Cleveland Medical Gazette suggested that “
every physician must take a personal interest in the question of the making of doctors” because “…
if his competitors are men of little education and culture, his own standing as a physician is lowered” [
3].
The need to adapt to rapidly changing expectations and circumstances has created an almost permanent state of reform. Without adaptation and innovation, “
we ossify and stagnate” [
4]. A decade ago, an urgent call by the Carnegie Foundation proposed selecting new, post-Flexnerian goals in medical education [
5]. Responding to this Call for Reform of Medical School and Residency, a comprehensive assessment of the medical education literature and practices listed various forms of curricular and pedagogical integration as one of their prime recommendations [
6].
Although curricular integration is an increasingly popular topic, it is not always well defined. [
7]. For the purposes of this paper, we would employ Huber’s definition of integration as a deliberate “
process where learners are making connections among concepts and experiences so that information and skills can be applied to novel and complex issues or challenges” [
8]. Since the 1990s, horizontal, spiral and vertical integration have become increasingly popular strategies in international medical education [
9]. Our group was primarily interested in the vertical form of integration, intentionally connecting relevant points of basic and clinical science knowledge across years of medical studies [
10].
Basic science remains a key part of today’s medical education, as it promotes critical appraisal, problem solving and decision making [
11,
12]. Recalling these foundational principles may allow students to develop their own concepts, which will provide a basis to help solve problems in contexts different from the original situation [
13]. Integration of basic science with experiential clinical medical education will facilitate knowledge transfer, an attribute of more advanced medical thinking [
14]. It may also allow reinforcement of core concepts in an age, where UME curricular times are ever shorter [
15].
Transfer of foundational knowledge to aid bedside clinical problem-solving is, however, challenged by limited recall [
15], poor application of pathophysiology or diminishing interest in basic sciences. Curricular integration leads to deeper learning and higher diagnostic accuracy. Moreover, basic science benefits learners through building coherent long-term concepts [
16,
17]. Literature suggest, integration was a valued and highly desired part of the medical school curriculum by recently graduated young attendings [
18].
Curricular integration efforts are introduced at program, course or individual event levels [
19,
20]. Ultimately, integration within and among disciplines is an institution-level challenge [
4]. Optimal learning methods, however, are not yet well defined.
In the current study, we have used VI as an instructional strategy and a guide to selecting content for faculty and to recruiting a multi-specialty group of facilitators [
21] for a new workshop linking Y3 clinical material with Y1-2 pre-clinical concepts. We were interested in seeing if a progressive buildup of integrated concepts [
16] may lead to improved retention by our learners. We were also aiming to compare two learning methods in search of an optimal format for future similar events.
A small-group, case-based collaborative approach previously reporting high levels of student engagement was selected as an alternative to a standard form of classroom didactic teaching [
22]. We hypothesized that utilizing this approach in the context of a complex disease, such as cancer, may offer a good platform for teaching vertically integrated material. We examined whether it may help students to actively engage with pre-clinical material and help them better understand a clinical case, similar to their bedside experience as M3s. We were also curious whether modifying the physical arrangement of the classroom space to accommodate small collaborative groups (SG) versus learning in a standard, classroom-sized group (StdG) may show differences in the outcomes of VI-designed active learning.
To sum up our research goals:
Determine the feasibility of delivering a new, case-based vertically integrated event with a multi-disciplinary, community-based hospital faculty;
Assess student perception of this innovation and measure immediate and delayed retention (efficacy) of this event;
Compare the outcomes of our VI strategy in two intentionally different physical learning spaces (a small-group collaborative setting versus a standard, didactic lecture format of a single group), in the hopes of finding the optimal learning environment for future integrated teaching events.
2. Materials and Methods
In synch with the constructivist theory of learning, we designed the workshop around the theme of cancer [
23]. It represents a complex medical condition where foundational knowledge, clinical care aspects and humanistic values can all be integrated, and their assimilation during the learning process constructs a new, higher level of knowledge for the participants.
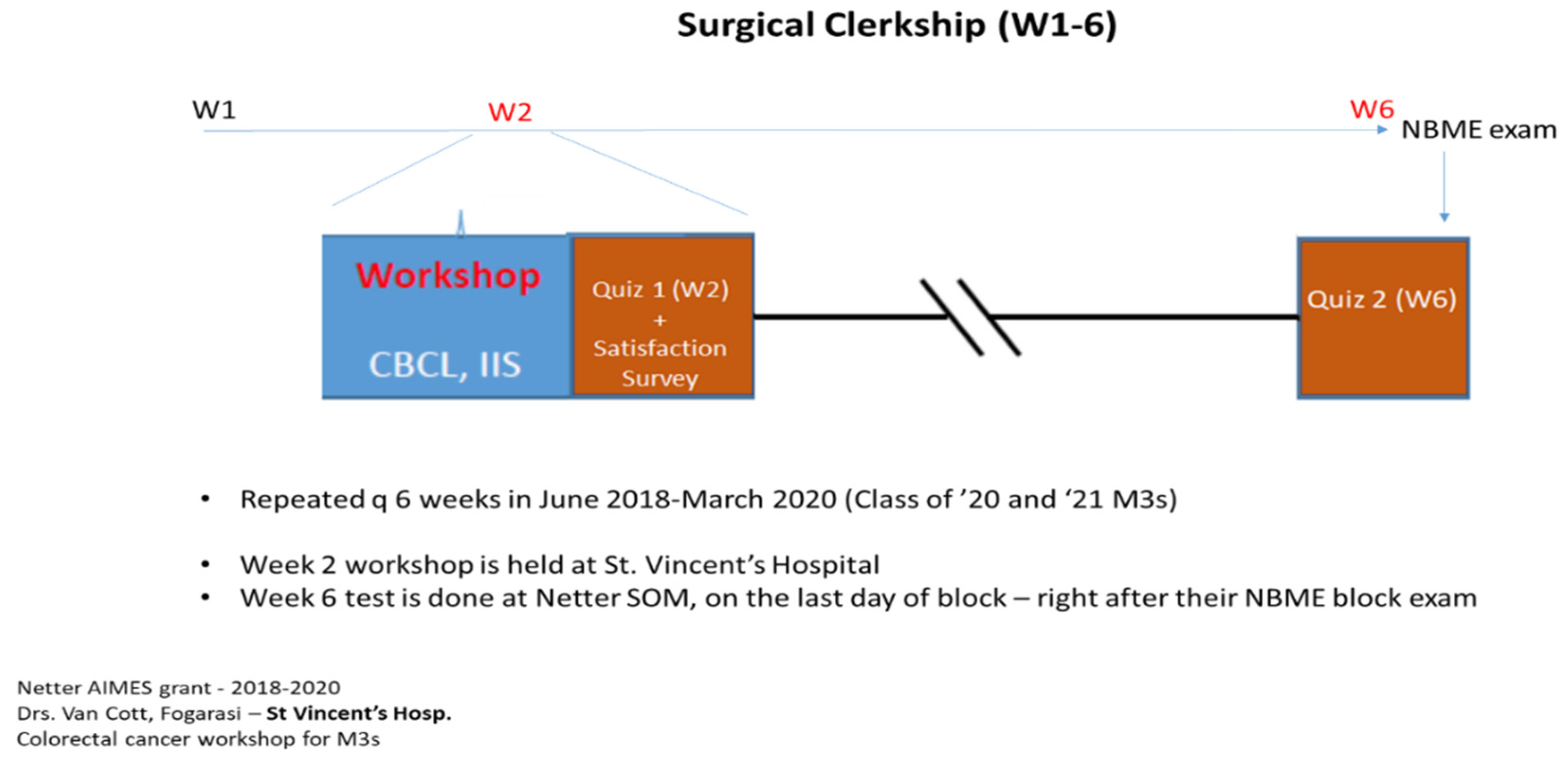
Workshop material was selected for this event to fit into a series of half-day learning sessions during Y3 Surgery clerkship at St. Vincent Medical Center, Bridgeport, CT, a major teaching affiliate of the Frank H. Netter MD School of Medicine. Topics were solicited from clinical teaching faculty by discussing perceived gaps in knowledge during prior classes moving through their surgical clerkship and sharing these with basic science colleagues who made considerable efforts to actually teach these topics in the year prior. During AY 2018/19 and 2019/20, unselected groups of M3s participated in this mandatory event on Week 2 of the clerkship, then answered a brief recall test four weeks later at the conclusion of the clerkship. (
Figure 1). The program began with Block 3 in 2018 and the series was cut short slightly by the COVID-19 pandemic, cancelling clinical rotations in Spring 2020, but by that time, data on all but two groups of students were available.
Each student group on surgical clerkship had 8–13 members. Workshops were taught using identical material, but in alternating blocks, it was either delivered by arranging classroom furniture to accommodate a single large group (
standard group, StdG) or by arranging seating to facilitate work in smaller, 3–4 member groups (
small group, SG). In parallel with this, the role of the facilitator changed from a didactic lecturer (in StdG) to a facilitator of collaborative learning in the small groups (SG). In the latter format, students were explicitly instructed to follow specific collaborative rules, as proposed by Krupat et al. [
22]. Due to the random number of students on clerkship in each group, the two teaching formats represented more two parallel learning methods, rather than a control and an experimental group.
Data on 136 students (67 in Y1, the rest in Y2) are reported here. Learning in SGs was also facilitated by using a voluntary pre-class warm-up exercise (similar to TBL’s individual readiness assurance test, IRAT). A question sheet with vertically integrated, case-based items was utilized during class to further promote discussion and vertical integration of knowledge. Students in SGs were instructed to answer these questions first individually, then pass them around to look at each other’s notes before developing a joint statement of their SG. These were then presented by each table to the entire class and commented on by the facilitators to eventually result in a classroom-level consensus. Meanwhile, StdGs were taught in an informal, discursive but somewhat more didactic classroom format, without the above additional facilitating tools.
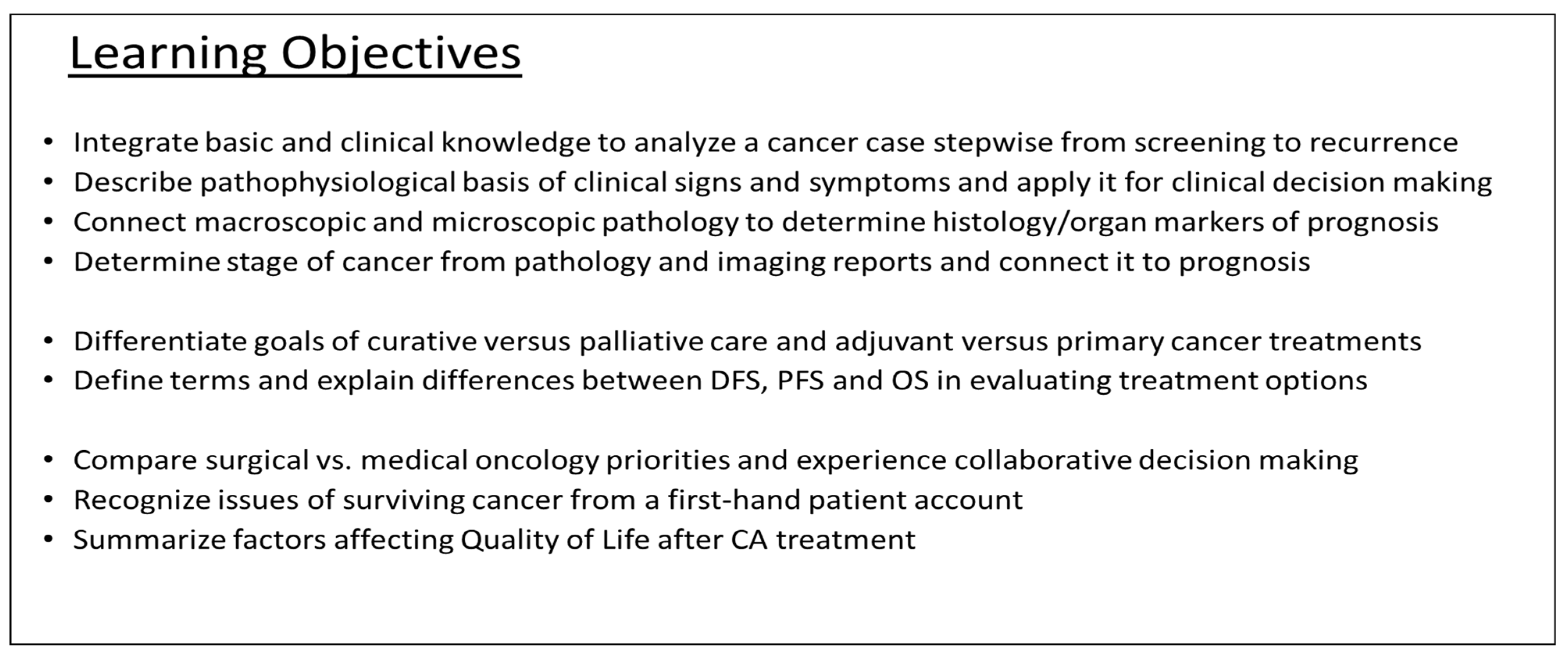
The workshop followed a single, complex case of cancer from screening to diagnosis, and to curative-intent then palliative treatment, concluding with a discussion of issues of survivorship and common social issues around cancer care. Course material was created by inserting selected concepts from Y1–Y2 pre-clinical material—on case-relevant pathophysiology, anatomy, genetics and pathology topics—to serve students’ better performance at key decision-points of this Y3-level clinical case.
The session utilized several strategic integrative tools, listed below [
24]:
Share expectations for the workshop upfront.
Build links into the case to connect pre-existing pre-clinical knowledge to learners’ recent clinical experiences (e.g., about cancer genetics, pathology of polyps, regional abdominal anatomy and RBC physiology).
Engage students by realizing the relevance of pre-clinical knowledge to the case (Lynch syndrome, US Preventive Services Task Force /USPSTF/screening guidelines)
Mobilize learners by setting clear expectations to have them act on their knowledge (e.g., using prior knowledge of splanchnic vessels and regional nodal stations to design the optimal extent of colorectal cancer surgery and set appropriate follow-up times in a patient with a hereditary cancer syndrome).
Provide a reflective opportunity (satisfaction surveys) to collect feedback and to foster awareness of the benefits of VI.
Faculty experienced in multiple specialties delivered sequential parts of the case, including parts facilitated by a medical oncologist (also with a pre-clinical teaching background); an abdominal surgeon; a clinical pathologist and an oncology-trained social worker. The case was taught in four subsections (screening/symptoms; pathology/diagnosis/staging; treatment and surveillance; work-up of recurrence and care of relapsed disease). Beginning in Y2, a fifth section was added, including a case discussion with a social worker, enriched by a video-taped patient testimony to prompt students to discuss survivorship issues. Learning Objectives are in
Figure 2.
The event was evaluated both with an anonymous satisfaction survey and using a pair of learning surveys, measuring immediate post-event retention (Week 2) and delayed retention (at Week 6, at block’s end). Statistical analysis compared mean scores of satisfaction and retention among small and standard groups. We compared the overall, pooled performance of all SGs versus StdGs. As we suspected that natural attrition would have a negative effect on basic science recall as students move away from Y1-2 preclinical learning, we also compared paired scores between SGs and StdGs taught in the early-, mid- and late-part of their Y3.
The first Learning Survey (immediate retention test) was distributed immediately at the end of the primary event. The second (late retention test) was given at the conclusion of the surgery block (right after students completed their block exam). Both times, a five-item (non-identical) short narrative, untimed quiz was distributed, and responses were evaluated by searching for key-terms. Questions for the retention test were constructed using the main concepts covered in the workshop. Scoring was as follows: each full and completely correct answer with proper use of key terms—2 points, partial answers—1 point, missing or incorrect answers received no points. Thus, the maximum score for both the Week 2 and Week 6 quizzes was 10 (5 of 5 fully correct answers).
Feasibility was assessed by observing the learners for stated Block Goals about participating in interdisciplinary care, collaborative work and applying previously learned facts of anatomy, physiology and human development. Our teaching faculty informally shared their opinion about the sustainability of this multi-specialty effort, as it required coordination of students’ arrival and return to their multiple clinical sites as well as harmonization of faculty members’ schedules.
The project was supported by an institutional grant (Quinnipiac University—AIMES Grant 2018-2020) and was awarded an IRB educational exemption (Quinnipiac University HEC/IRB protocol # 09918).
3. Results
3.1. Satisfaction Survey—Kirkpatrick Level I—Was the Training Valuable?
Immediately following the workshop, we asked how the learners liked the event. A total of 136 surveys were collected. The data analysis reflected a prominent level of overall student satisfaction with the vertically integrated workshop (
Table 1). A total of 93% of M3s agreed that the event was “
worth my time” (64/69 in SG and 63/67 in StdG); 96% of learners suggested it has “
increased my fund of knowledge” (66/69 SG vs. 64/67 StdG).
Level of faculty involvement was deemed adequate both by students attending SG (81%) or StdG (78%). Agreement with the statement “
Individual student input mattered in at least 50% of class-time” was seen in 91% versus 85% of students (63/69 SG and 57/67 StdG).
A total of 93% (64/69) versus 94% (63/67) of students in the two groups reported they would like to “see further learning events utilizing vertically integrated teaching”. Of these students, there was a significantly stronger endorsement—“we absolutely need more VI”—by students in SGs (52%, 36/69) as compared to StdGs (31% 21/67, p-value = 0.014)—suggesting additional value, if VI was delivered in a small-group, collaborative format.
A significant difference was also notable in stating future preferences for optimal learning. Students’ current experience with group size clearly mattered: 88% (61/69) of those who experienced the event in small groups versus 42% (28/67) of those who learned in standard-size groups stated they would prefer to be taught in small-sized groups in future workshops. (p-value < 0.00001).
In the narrative part of the survey, students were asked to list some highlights of the VI workshop. Common themes cited by students included the benefit of a “longitudinal case from presentation to palliation”, “using basic concepts as they relate to clinic”, “integrating pathophysiology and survivorship skills to allow for holistic care”, appreciating seeing how a “multispecialty team collaborate”, commenting on the patient’s survivorship-themed video they enjoyed “hearing the patient’s experience” and on the overall format “small group collaboration allows individual input”.
3.2. Learning Survey—Kirkpatrick Level II—Did Knowledge Improve, as a Result of the Training?
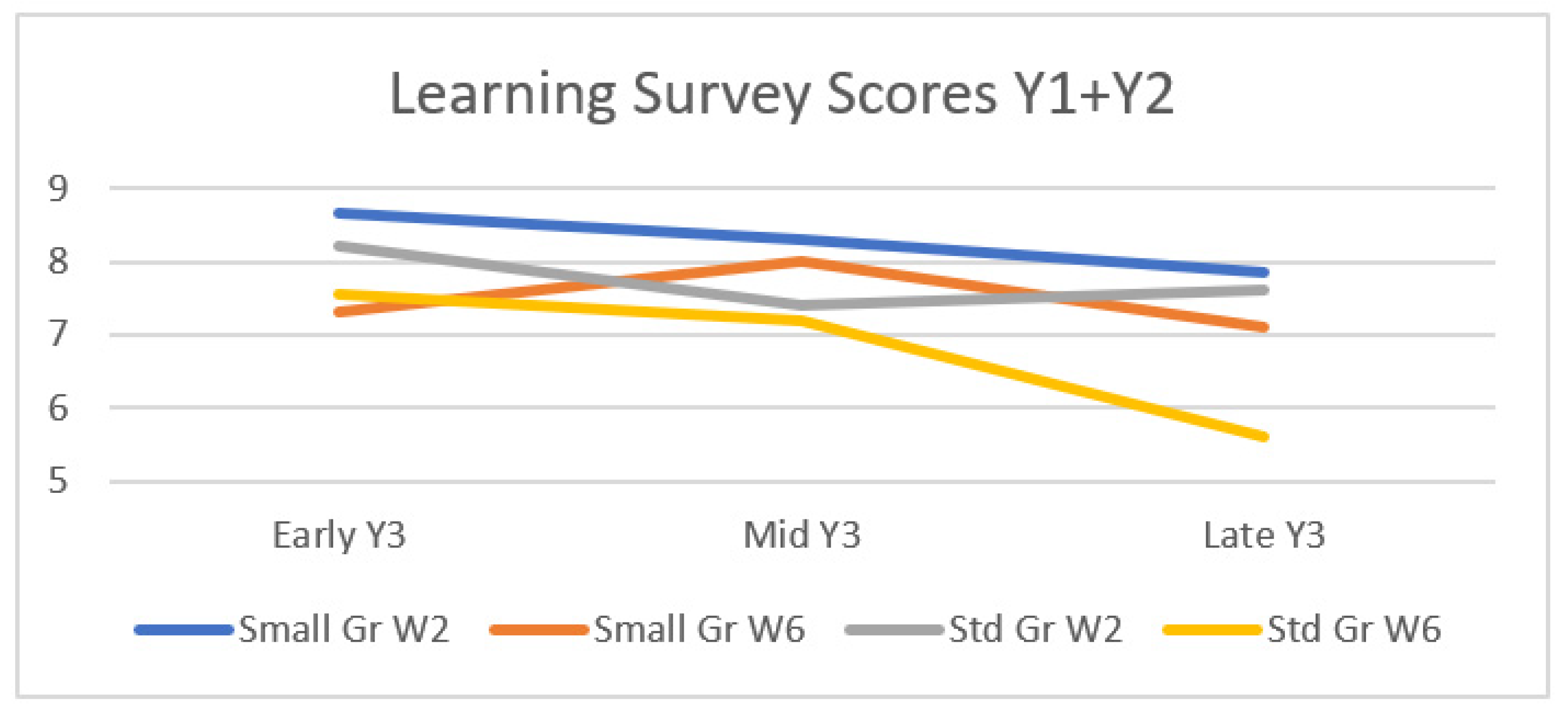
An immediate post-event quiz (on Week 2, at the time of the workshop) and a delayed learning quiz (on Week 6) were used to assess if learners had gained proper knowledge right after the workshop and whether they maintained it over time. High overall scores support a high value of learning during the vertically integrated workshop.
As expected, students scored significantly higher on Week 2 than on Week 6 (average score of 7.94 vs. 7.10, p < 0.05). The loss of almost a point amounts to a 10% drop in recall in 4 weeks.
The form of instruction favored learning in small groups (
Figure 3 and
Table 2). Students in small groups (SG, blue bars) have done better overall, with a combined W2+6 test average of 7.83 points, whereas those in standard-sized groups (StdG, red bars) had averaged 7.2 (
p = 0.007). Note, the SG vs. StdG overall performance (W2+6 combined) is reflected by the average of the values of the two blue bars or the two red bars in
Figure 3.
When analyzing early versus late recall, both the immediate and the late scores were significantly better in SGs: in Week 2, the average score in SG vs. StdG was 8.23 (95% CI: 7.83–8.61) vs. 7.66 (7.26–8.06) (p = 0.046), in Week 6, the average score in SG vs. StdG was 7.43 (6.99–7.88) vs. 6.77 (6.34–7.20). p = 0.035.
When comparing the rates of loss in the two groups from W2→W6, the difference was non-significant (p = 0.812), suggesting that both groups were forgetting at about the same rate. It is not surprising to not have long-standing benefits from a single intervention. This also suggests that while learning in SGs has achieved a higher immediate post-event recall score, it failed to translate that into an improved retention rate when retesting students 4 weeks later.
Student groups participating in the workshop early in the year almost always did better than students who took the same class in the middle or later part of the year, despite being given the same basic science refresher data during the workshop (
Figure 4). This ongoing drop in average scores from the beginning to the end of the year probably reflects natural attrition of basic science knowledge through Year 3.
3.3. Other Information
Finally, a word on student behavior: Active learning for students in SGs was explicitly encouraged and they were instructed to follow the CBCL format (case-based collaborative learning), as reported by Krupat et al. [
22]. They were also aided by a pre-printed Integration Worksheet, to facilitate the insertion of basic science concepts into the case. Nevertheless, students in the StdG were also often observed to show some level of spontaneous small-group formation during the open-discussion times of the workshop. This was neither encouraged, nor discouraged by faculty and typically occurred through forming pairs or trios working together on their own, while others remained engaged but solved their questions individually. While this offered variable levels of student interaction, the SGs benefitted from a more vigorous peer-teaching period, often observable as group debate, intense search for supportive data in the literature, and eventual joint creation of consensus statements, with nearly all small group members participating. In the second year of the project, detailed observations by an independent, trained observer recorded more student interactions and less single-student domination of the discourse in the small groups than in the more traditional, larger group setting.
4. Discussion
A single institution multi-specialty team created material for a new cancer workshop delivering a case-based, 360-degree colorectal cancer event from screening to surgery and to palliative care during our Y3 surgical clerkship. By vertically integrating case-relevant Y1–2 basic science material into the exercise, the event was built to bridge knowledge gaps between the pre-clinical and clinical years.
Employing Harden’s integration ladder [
25], we utilized multiple elements, such as nesting (importing), co-teaching, coordinated mixing and multidisciplinary elements (by looking at the case from pathological, epidemiological, medical, surgical and social work perspectives). We found that several integrative tools reported in the literature were beneficial for us as well (sharing expectations, intentionally linking pre-clinical material with the case, increasing practical relevance of basic science knowledge by having students act on it as the case moved, fostering the benefits of VI and allowing for reflection and feedback) [
24].
We focused on integrating case-relevant anatomy, pathology and pathophysiology material, as these were highly valued by our own teaching faculty, as well as listed among the top items that recent graduates had listed as topics that they wish they had learned more of [
19]. These fields are also the most sought-after basic science principles by clerkship directors, integration of which can lead to better diagnostic competence [
26,
27].
Besides our interest in assessing the overall level of learning and satisfaction using a VI strategy, we were curious to also compare retention using either a standard classroom teaching method or a small-group collaborative learning method. This allowed us to check on the contribution of distinct physical learning environments, allowing for different facilitation formats when a VI-based strategy is used. While not intended as a strict controlled study, comparing learning outcomes in the two intentionally altered learning spaces helped us gain some insight about preferred settings for future VI-based events.
Our findings suggest that a vertically integrated workshop is a feasible way of teaching about a complex disease with significant illness experiences, such as cancer. Students reported exceedingly high levels of satisfaction with the event, gained new knowledge and skills, and retained it at acceptable levels. Vertical integration was an excellent way to demonstrate teamwork, to role-model multi-disciplinary collaboration and mutual respect among specialists, all of which were appreciated by our learners and were learning goals of the surgical clerkship. We found that by intentionally recapping only basic science information that was case-relevant, students remained highly engaged not only with anatomy, pathology and pathophysiology but also with topics covering epidemiology, genetics, molecular mechanism and pharmacology throughout the 4-hour workshop. Learners used the pre-clinical material to participate in vigorous discussions and to argue their group’s cases well in front of the class, leading to the creation of several well-founded consensus statements. We found that VI in this form, avoiding formal didactic teaching of chapters and instead focusing on immediate applicable preclinical material was valued highly by M3 students.
The Learning Environment (LE) is a complex entity, which describes the “dynamic, co-constructed perceptions, experiences and behaviors of participants in the physical and virtual spaces within which learning occurs” [
28]. Here, we focused on both the social aspects and the physical space attributes of the LE. By intentionally arranging the physical space to accommodate small groups, we also succeeded in establishing a positive learning climate with both high safety and brisk interactions (
Figure 5).
Students clearly endorsed vertical integrative learning. A large majority would welcome seeing similar integrated teaching events in their clinical curriculum. Indeed, following this event, a second VI case in pediatrics was introduced to M3s at our school with success [
29]. The vast majority of workshop participants in small groups would again prefer SG collaborative learning over traditional class-based learning when the VI strategy is used. Importantly, more than half of those students taught in standard-size groups also signaled their future preference for smaller groups as well.
Knowledge scores, as measured by a 5-item brief narrative quiz both at the end of the session and at 4 weeks, were high, suggesting an overall good transfer of knowledge. Recall of the material taught after 4 weeks—as measured by the late test scores—was improved in SGs, albeit the difference between the groups was small and became significant only after pooling two years of student data (results from over 130 students). The rate of loss of content knowledge from Week 2—6 was also similar in both groups, with no sign that a single collaborative learning event using SGs could prevent or slow the rate of attrition. Perhaps this loss is not impacted by the method of instruction but instead attributable to normal attrition over time, as well as the intense educational experience of a surgical clerkship. Our findings are similar to a striking study among Dutch medical students, where unprepared testing of M2s demonstrated an over 50% loss of Y1 knowledge after just 8–10 months [
30]. It also suggests that, although vertically integrated information can increase recall for a single event, if we are to help students take the Step 1 exam at the end of Y3, a concerted (longitudinal, year-long) effort would be needed to keep basic science topics fresh [
31].
As the rate of loss was similar but students in SGs started off with higher scores on their immediate post-event testing, the score difference remained in place by week 6 as well, favoring SG learning. As expected, there was a continuous decline in pre-clinical science knowledge throughout Y3, reflected by higher average test scores on workshops given earlier in the year than in mid-course or by the end of Y3. All this calls for further curricular improvements, especially considering that some learners would take Step 1 at the end of Y3.
4.1. Limitations
Our study initially had a smaller sample size and required an extension to a second year to note significant differences. It is also quite possible that a single, 4-hour intervention during a very educationally dense surgical clerkship may have limited/minimal durable impact overall.
Due to logistical issues (students after their 6-week surgical rotation were dispersed to many different specialties), we were limited as to the latest time of the repeat testing, and we were not able to assess any potential longer-term (recall) benefits of teaching with a VI strategy.
The feasibility of multi-specialty teaching has very real practical aspects. In discussing its sustainability over time, we acknowledge that repeating the event every six weeks for two years in this format was rather resource-intensive. We had to bring together faculty from different departments (some requiring travel), using up a half-day of curricular time, and pull students from multiple clinical rotations to a single site to attend it. The latter may be less of an issue in the post-COVID era, with an affinity for tele-learning, although this will surely bring up its own issues [
32].
Although the pandemic forced us to cancel the last two workshop events, the study was almost complete by the time that hospital-based M3 teaching ceased, and we are grateful that we were able to conclude this project.
4.2. Next Steps
Recording and scoring observable in-class engagement levels of individual learners could allow matching these with post-event retention and possible identification of optimal learning behaviors. Study of student-, group- or entire classroom-level behavior patterns, may then permit intentional design of new and optimized activities to facilitate more active learning. Ultimately, the hope is to explore, if higher in-class engagement might lead to more optimal educational outcomes in the form of improved retention and better test scores.
The role of the physical learning space to further improve learning outcomes and increase student engagement is a somewhat under-explored area [
33]. Reflecting on the role of the physical space in shaping the overall learning environment in our study, some may consider deliberately designing new curricular events with a triple focus; not only setting learning objectives (L.O.s) and pairing them with the best-fitting pedagogical approaches, but also placing the event into an optimal classroom design.
Pairing of L.O.s with an effort to optimize the physical space of delivery (e.g., group sizes, seating forms, intentional variation of classroom furniture during longer events to facilitate collaborative work versus didactic learning)—could create a “director’s script”, moving us from the simple delivery of material to truly learner-centered active learning. In fact, one might create a hybrid classroom choreography with changing spatial classroom arrangements within which periods of didactic teaching may alternate with parts favoring dialogue, visualization and peer-to-peer communication to best serve the delivery of materials.
Elevating vertical integration from single-sessions to a course level of integration, advancing up the integration ladder [
25], would be beneficial. If the positive outcomes of integrated teaching are consistently verified in other M3 events, expanding our VI strategy to a centralized, program-level instructional method may facilitate improvement on standardized exams, as already seen elsewhere [
31,
34]. To further explore this, our school has listed improving vertical and horizontal integration of the curriculum as one of its goals in its Better Netter ’23 strategic plan.