The Opportunity Cost of COVID-19 Deaths in the USA
Abstract
1. Introduction
2. Data and Method
2.1. Data
2.2. Direct Medical Cost
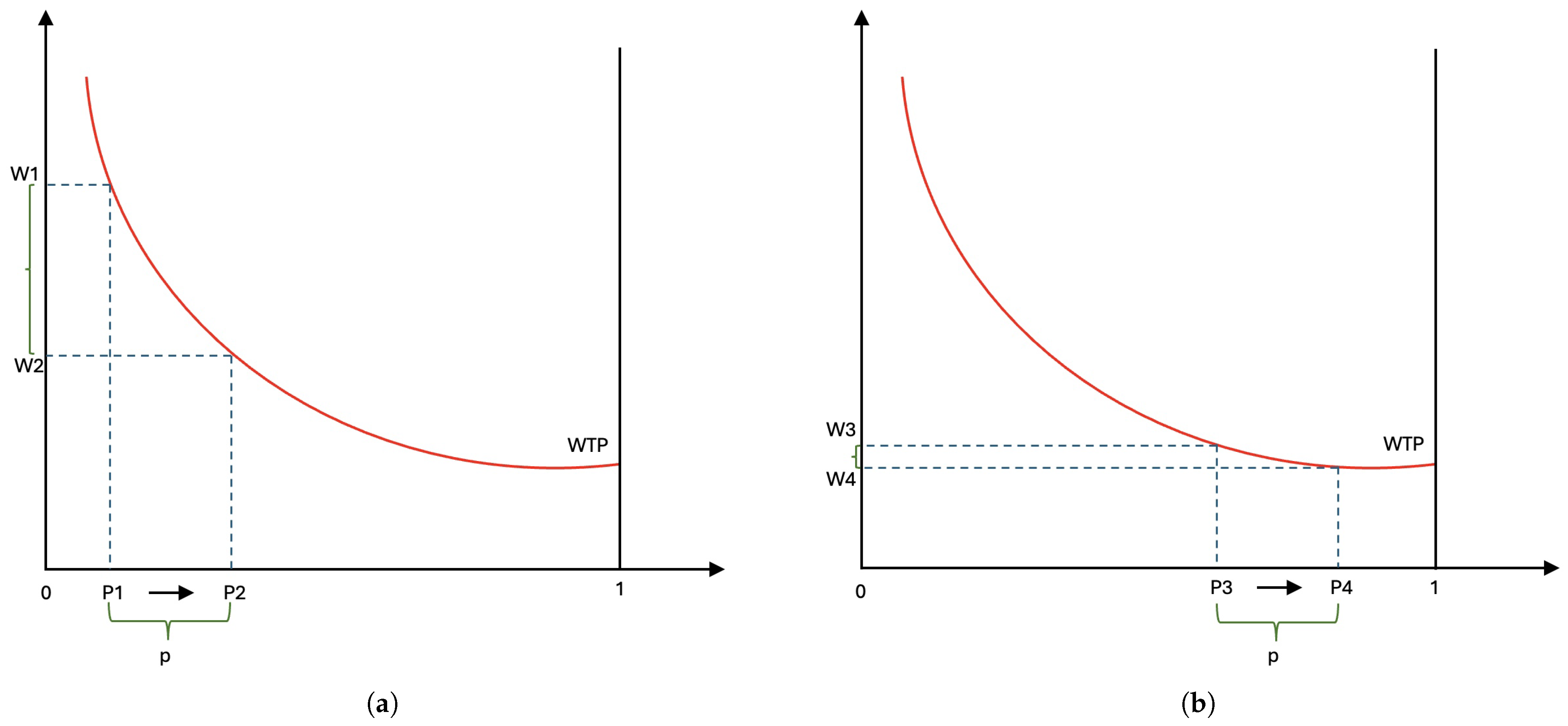
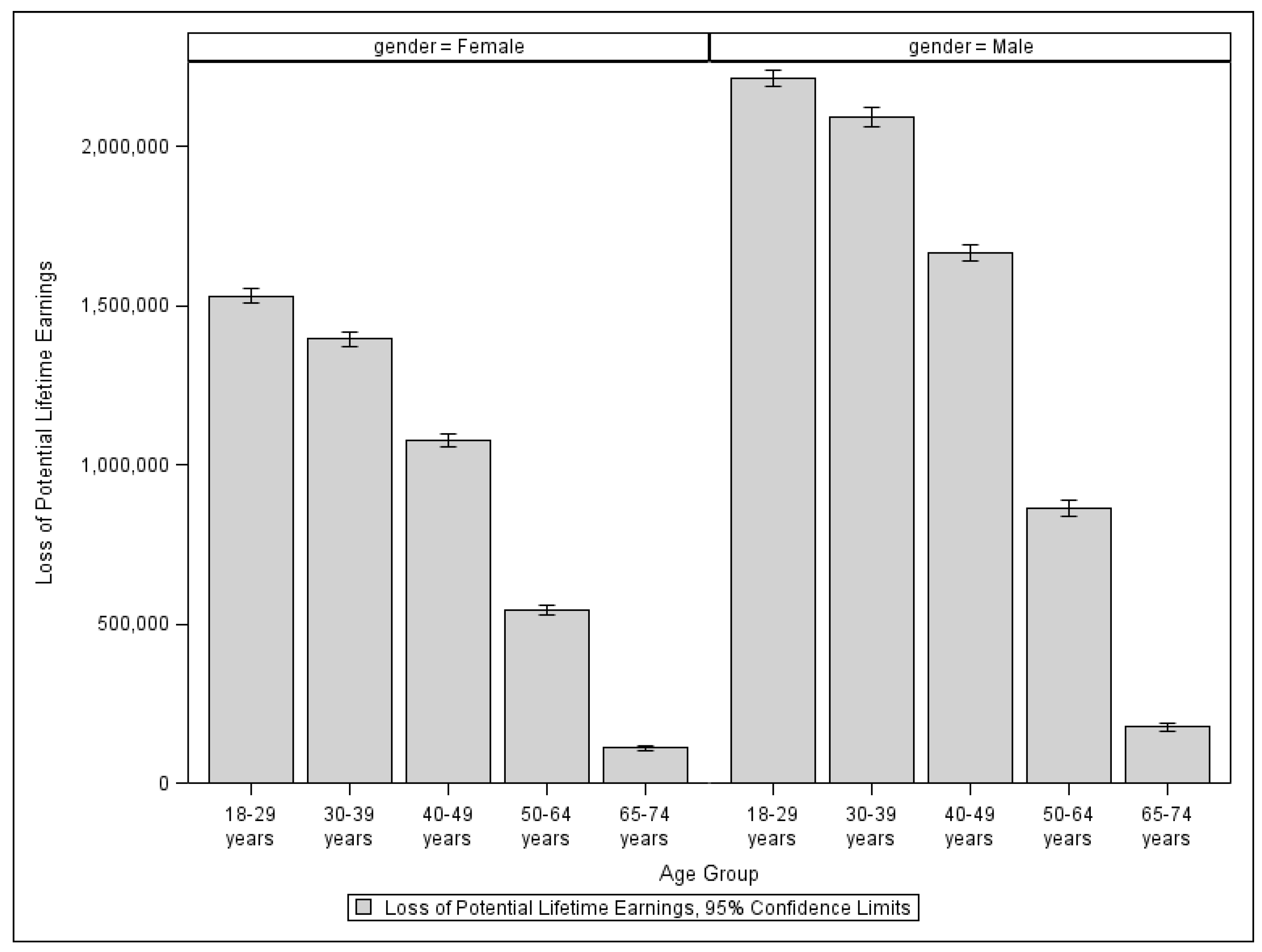
2.3. Cost of Loss Lifetime Production (Indirect Cost)
2.4. Total Economic Costs of COVID-19 Deaths
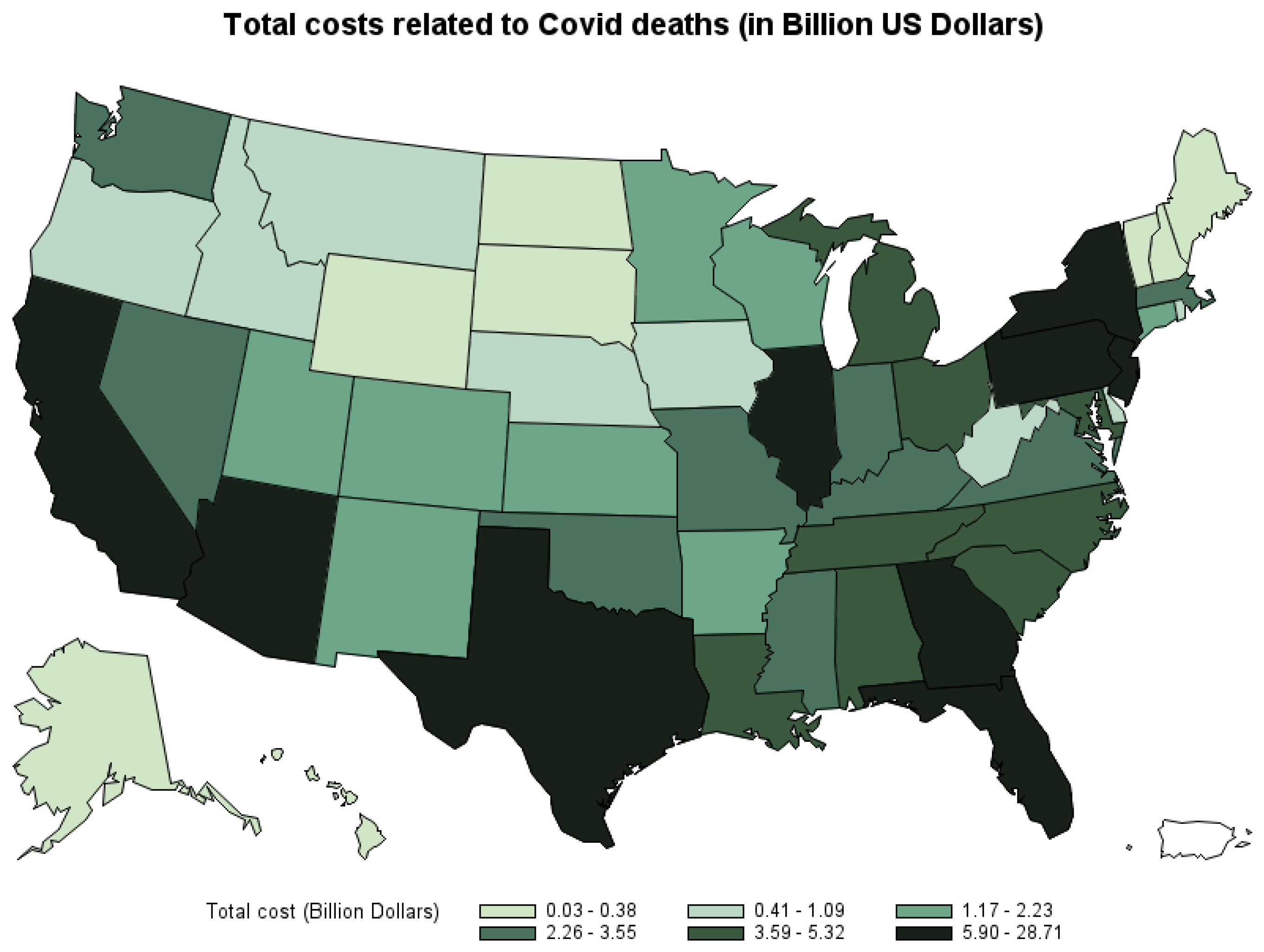
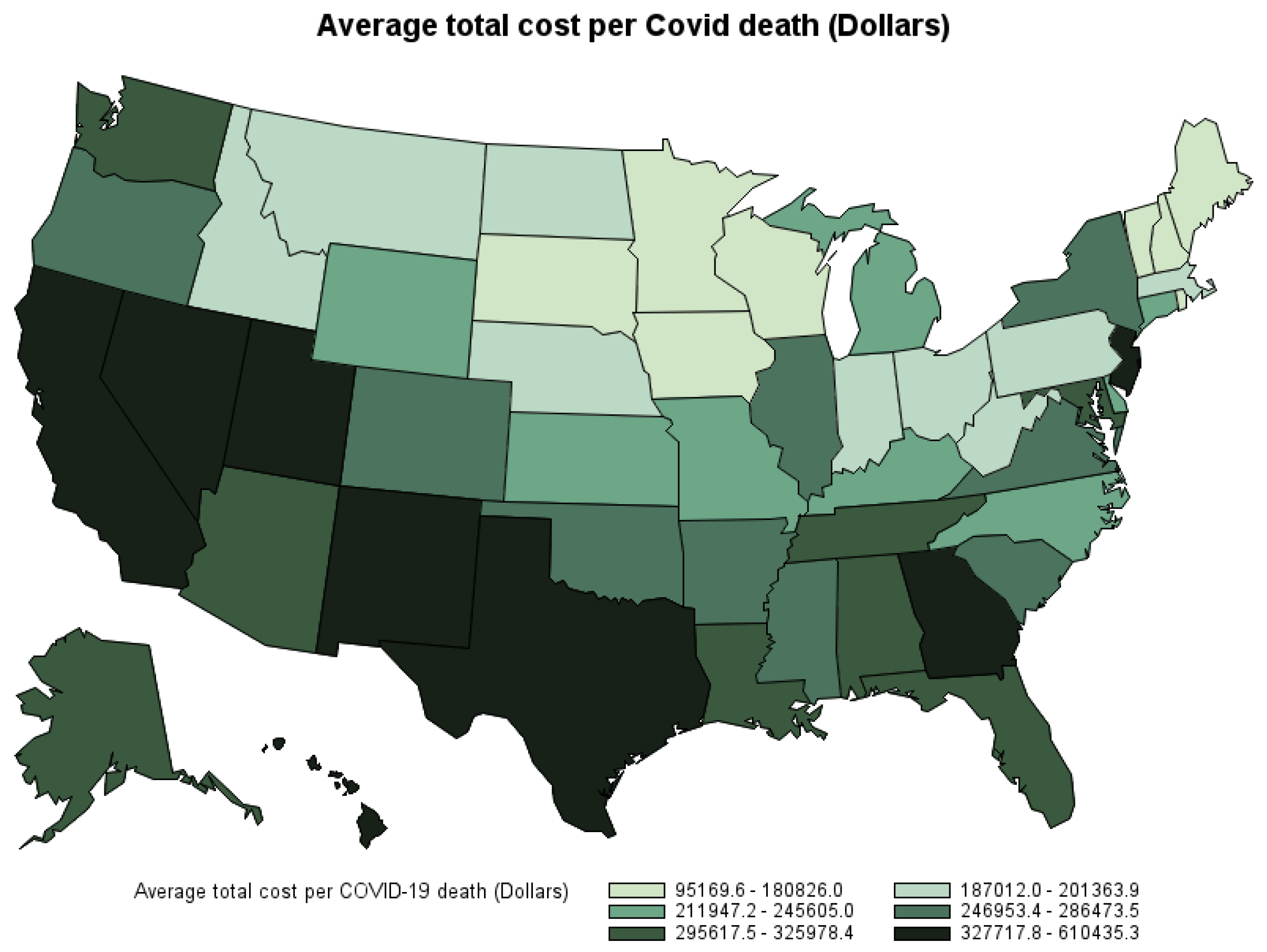
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Age | Gender | Loss of Potential Lifetime Earning (USD) | Standard Error (USD) | Lower CI (USD) | Upper CI (USD) |
|---|---|---|---|---|---|
| 18 | Female | 1,491,318 | 36,166 | 1,418,676 | 1,563,961 |
| 19 | Female | 1,507,960 | 36,731 | 1,434,184 | 1,581,735 |
| 20 | Female | 1,521,910 | 37,038 | 1,447,517 | 1,596,302 |
| 21 | Female | 1,533,211 | 37,613 | 1,457,663 | 1,608,760 |
| 22 | Female | 1,542,393 | 38,180 | 1,465,706 | 1,619,079 |
| 23 | Female | 1,549,078 | 38,673 | 1,471,401 | 1,626,754 |
| 24 | Female | 1,550,817 | 38,854 | 1,472,775 | 1,628,858 |
| 25 | Female | 1,549,554 | 39,006 | 1,471,208 | 1,627,899 |
| 26 | Female | 1,542,359 | 39,089 | 1,463,846 | 1,620,871 |
| 27 | Female | 1,533,498 | 39,156 | 1,454,852 | 1,612,145 |
| 28 | Female | 1,522,975 | 39,013 | 1,444,616 | 1,601,334 |
| 29 | Female | 1,510,721 | 38,842 | 1,432,705 | 1,588,738 |
| 30 | Female | 1,495,709 | 38,521 | 1,418,337 | 1,573,080 |
| 31 | Female | 1,478,225 | 38,015 | 1,401,870 | 1,554,579 |
| 32 | Female | 1,458,376 | 37,343 | 1,383,370 | 1,533,382 |
| 33 | Female | 1,437,059 | 36,801 | 1,363,142 | 1,510,977 |
| 34 | Female | 1,413,570 | 36,184 | 1,340,892 | 1,486,248 |
| 35 | Female | 1,388,798 | 35,588 | 1,317,317 | 1,460,279 |
| 36 | Female | 1,360,836 | 34,680 | 1,291,180 | 1,430,493 |
| 37 | Female | 1,331,105 | 33,943 | 1,262,928 | 1,399,281 |
| 38 | Female | 1,302,007 | 33,012 | 1,235,701 | 1,368,313 |
| 39 | Female | 1,270,837 | 32,319 | 1,205,921 | 1,335,753 |
| 40 | Female | 1,238,919 | 31,846 | 1,174,956 | 1,302,883 |
| 41 | Female | 1,206,101 | 30,475 | 1,144,890 | 1,267,313 |
| 42 | Female | 1,170,229 | 29,349 | 1,111,280 | 1,229,179 |
| 43 | Female | 1,136,711 | 28,736 | 1,078,994 | 1,194,429 |
| 44 | Female | 1,100,249 | 27,794 | 1,044,424 | 1,156,075 |
| 45 | Female | 1,062,874 | 26,762 | 1,009,122 | 1,116,626 |
| 46 | Female | 1,023,312 | 25,526 | 972,040 | 1,074,583 |
| 47 | Female | 982,417 | 24,537 | 933,132 | 1,031,701 |
| 48 | Female | 942,120 | 23,343 | 895,234 | 989,006 |
| 49 | Female | 900,531 | 22,095 | 856,152 | 944,910 |
| 50 | Female | 858,772 | 20,953 | 816,686 | 900,857 |
| 51 | Female | 817,467 | 20,269 | 776,756 | 858,179 |
| 52 | Female | 773,234 | 19,476 | 734,115 | 812,353 |
| 53 | Female | 729,986 | 18,082 | 693,667 | 766,305 |
| 54 | Female | 687,783 | 17,155 | 653,327 | 722,240 |
| 55 | Female | 643,948 | 16,143 | 611,523 | 676,373 |
| 56 | Female | 597,605 | 14,645 | 568,190 | 627,020 |
| 57 | Female | 551,248 | 13,893 | 523,343 | 579,154 |
| 58 | Female | 503,938 | 12,551 | 478,728 | 529,147 |
| 59 | Female | 457,291 | 11,598 | 433,996 | 480,587 |
| 60 | Female | 409,558 | 10,714 | 388,038 | 431,078 |
| 61 | Female | 360,688 | 9238 | 342,134 | 379,242 |
| 62 | Female | 310,316 | 7945 | 294,358 | 326,274 |
| 63 | Female | 261,319 | 6528 | 248,207 | 274,432 |
| 64 | Female | 210,944 | 5370 | 200,158 | 221,730 |
| 65 | Female | 162,147 | 4341 | 153,428 | 170,867 |
| 66 | Female | 111,039 | 3257 | 104,497 | 117,581 |
| 67 | Female | 56,373 | 1913 | 52,530 | 60,216 |
| 18 | Male | 2,139,678 | 42,682 | 2,053,948 | 2,225,407 |
| 19 | Male | 2,165,305 | 43,438 | 2,078,057 | 2,252,552 |
| 20 | Male | 2,186,859 | 44,180 | 2,098,120 | 2,275,598 |
| 21 | Male | 2,204,880 | 44,945 | 2,114,606 | 2,295,154 |
| 22 | Male | 2,220,791 | 45,724 | 2,128,950 | 2,312,631 |
| 23 | Male | 2,232,759 | 46,541 | 2,139,279 | 2,326,239 |
| 24 | Male | 2,239,213 | 47,028 | 2,144,754 | 2,333,672 |
| 25 | Male | 2,243,386 | 47,404 | 2,148,173 | 2,338,600 |
| 26 | Male | 2,240,402 | 47,620 | 2,144,755 | 2,336,049 |
| 27 | Male | 2,234,852 | 47,874 | 2,138,695 | 2,331,009 |
| 28 | Male | 2,226,448 | 47,897 | 2,130,244 | 2,322,652 |
| 29 | Male | 2,216,546 | 47,959 | 2,120,217 | 2,312,875 |
| 30 | Male | 2,203,549 | 47,786 | 2,107,569 | 2,299,530 |
| 31 | Male | 2,187,653 | 47,571 | 2,092,103 | 2,283,203 |
| 32 | Male | 2,167,701 | 47,295 | 2,072,706 | 2,262,696 |
| 33 | Male | 2,143,765 | 46,897 | 2,049,570 | 2,237,960 |
| 34 | Male | 2,117,179 | 46,224 | 2,024,336 | 2,210,022 |
| 35 | Male | 2,089,500 | 45,707 | 1,997,695 | 2,181,305 |
| 36 | Male | 2,055,806 | 45,133 | 1,965,153 | 2,146,458 |
| 37 | Male | 2,018,999 | 43,949 | 1,930,725 | 2,107,273 |
| 38 | Male | 1,980,941 | 43,219 | 1,894,133 | 2,067,750 |
| 39 | Male | 1,939,040 | 42,232 | 1,854,215 | 2,023,865 |
| 40 | Male | 1,894,646 | 41,165 | 1,811,964 | 1,977,328 |
| 41 | Male | 1,850,927 | 40,350 | 1,769,883 | 1,931,972 |
| 42 | Male | 1,800,477 | 38,529 | 1,723,090 | 1,877,865 |
| 43 | Male | 1,751,618 | 37,192 | 1,676,915 | 1,826,321 |
| 44 | Male | 1,696,515 | 35,389 | 1,625,434 | 1,767,597 |
| 45 | Male | 1,643,458 | 34,268 | 1,574,628 | 1,712,288 |
| 46 | Male | 1,590,482 | 33,447 | 1,523,303 | 1,657,662 |
| 47 | Male | 1,532,628 | 32,514 | 1,467,322 | 1,597,935 |
| 48 | Male | 1,473,357 | 31,168 | 1,410,754 | 1,535,959 |
| 49 | Male | 1,413,613 | 30,130 | 1,353,095 | 1,474,132 |
| 50 | Male | 1,350,678 | 29,070 | 1,292,289 | 1,409,067 |
| 51 | Male | 1,283,763 | 27,019 | 1,229,494 | 1,338,033 |
| 52 | Male | 1,218,855 | 25,578 | 1,167,480 | 1,270,229 |
| 53 | Male | 1,150,315 | 23,333 | 1,103,450 | 1,197,180 |
| 54 | Male | 1,083,208 | 21,923 | 1,039,174 | 1,127,243 |
| 55 | Male | 1,015,618 | 20,718 | 974,004 | 1,057,231 |
| 56 | Male | 944,036 | 18,804 | 906,268 | 981,804 |
| 57 | Male | 872,973 | 17,747 | 837,327 | 908,619 |
| 58 | Male | 801,887 | 16,513 | 768,719 | 835,054 |
| 59 | Male | 729,080 | 15,256 | 698,437 | 759,723 |
| 60 | Male | 654,849 | 13,908 | 626,913 | 682,785 |
| 61 | Male | 576,965 | 12,202 | 552,456 | 601,473 |
| 62 | Male | 500,863 | 10,661 | 479,450 | 522,276 |
| 63 | Male | 422,833 | 9503 | 403,744 | 441,921 |
| 64 | Male | 345,665 | 8785 | 328,020 | 363,310 |
| 65 | Male | 263,179 | 6151 | 250,825 | 275,533 |
| 66 | Male | 177,665 | 4847 | 167,929 | 187,402 |
| 67 | Male | 90,807 | 2660 | 85,464 | 96,150 |
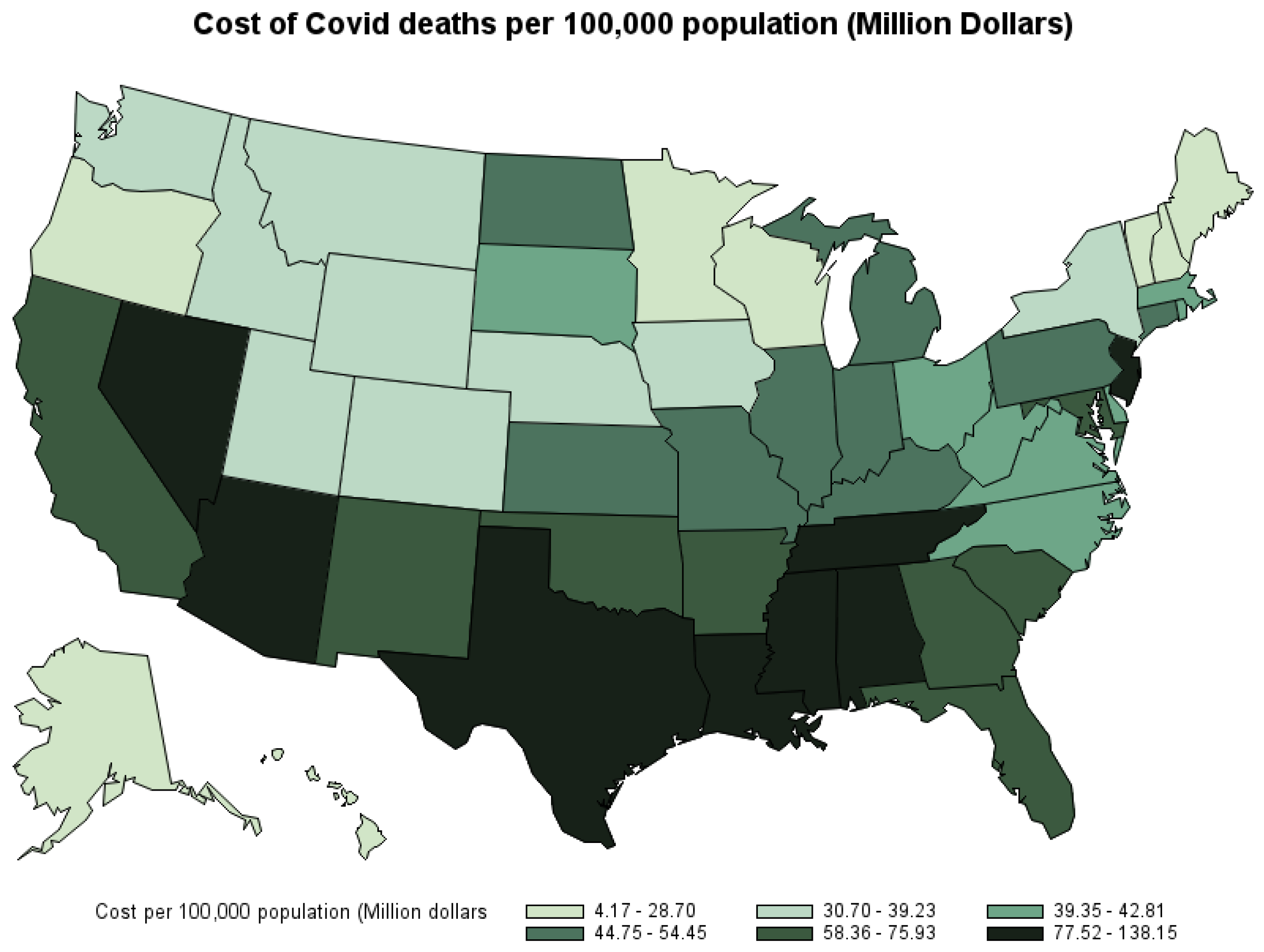
| State | COVID-19 Deaths per 100,000 Population | Total Cost of COVID-19 Deaths (USD) | Average Cost of COVID-19 Deaths (USD) | Cost of COVID-19 Deaths per 100,100 Population (USD) |
|---|---|---|---|---|
| Alabama | 292 | 4,502,349,787 | 306,619 | 89,610,000 |
| Alaska | 77 | 185,498,888 | 325,978 | 25,290,000 |
| Arizona | 256 | 5,897,429,919 | 324,354 | 82,900,000 |
| Arkansas | 274 | 2,035,898,457 | 247,094 | 67,600,000 |
| California | 185 | 28,713,952,363 | 394,271 | 72,890,000 |
| Colorado | 140 | 2,232,696,952 | 276,724 | 38,670,000 |
| Connecticut | 239 | 1,916,209,318 | 222,772 | 53,140,000 |
| Delaware | 194 | 407,998,085 | 211,947 | 41,210,000 |
| District of Columbia | 226 | 952,618,161 | 610,435 | 138,150,000 |
| Florida | 257 | 16,282,590,875 | 295,617 | 75,930,000 |
| Georgia | 222 | 8,069,050,457 | 340,959 | 75,720,000 |
| Hawaii | 58 | 339,002,342 | 400,418 | 23,290,000 |
| Idaho | 166 | 598,961,785 | 196,504 | 32,570,000 |
| Illinois | 193 | 6,765,680,713 | 274,809 | 53,030,000 |
| Indiana | 230 | 3,036,781,877 | 194,835 | 44,750,000 |
| Iowa | 212 | 1,075,754,808 | 158,994 | 33,720,000 |
| Kansas | 205 | 1,326,793,854 | 219,923 | 45,160,000 |
| Kentucky | 223 | 2,264,497,783 | 225,640 | 50,260,000 |
| Louisiana | 266 | 3,788,664,030 | 305,523 | 81,340,000 |
| Maine | 87 | 181,471,425 | 152,509 | 13,320,000 |
| Maryland | 182 | 3,604,970,718 | 321,060 | 58,360,000 |
| Massachusetts | 202 | 2,792,007,999 | 196,140 | 39,720,000 |
| Michigan | 199 | 4,906,365,831 | 244,935 | 48,690,000 |
| Minnesota | 147 | 1,471,887,690 | 175,420 | 25,790,000 |
| Mississippi | 341 | 2,890,979,794 | 286,474 | 97,630,000 |
| Missouri | 235 | 3,351,252,430 | 231,549 | 54,450,000 |
| Montana | 195 | 425,348,273 | 201,364 | 39,230,000 |
| Nebraska | 168 | 654,910,083 | 199,182 | 33,390,000 |
| Nevada | 244 | 2,532,488,374 | 333,954 | 81,570,000 |
| New Hampshire | 107 | 173,548,978 | 117,173 | 12,600,000 |
| New Jersey | 278 | 8,470,357,174 | 327,718 | 91,190,000 |
| New Mexico | 225 | 1,601,072,615 | 336,214 | 75,610,000 |
| New York | 134 | 6,675,133,362 | 246,953 | 33,040,000 |
| North Carolina | 174 | 4,468,789,224 | 245,605 | 42,810,000 |
| North Dakota | 239 | 366,888,686 | 196,816 | 47,090,000 |
| Ohio | 220 | 4,857,608,529 | 187,012 | 41,170,000 |
| Oklahoma | 272 | 2,878,615,072 | 266,876 | 72,700,000 |
| Oregon | 99 | 1,089,397,869 | 260,440 | 25,710,000 |
| Pennsylvania | 236 | 5,958,481,801 | 194,353 | 45,820,000 |
| Rhode Island | 255 | 431,828,725 | 154,611 | 39,350,000 |
| South Carolina | 248 | 3,591,425,909 | 283,365 | 70,170,000 |
| South Dakota | 251 | 379,480,965 | 170,450 | 42,800,000 |
| Tennessee | 260 | 5,322,669,598 | 298,522 | 77,520,000 |
| Texas | 246 | 28,019,667,234 | 393,611 | 96,640,000 |
| Utah | 100 | 1,166,700,588 | 358,310 | 35,660,000 |
| Vermont | 44 | 26,824,028 | 95,170 | 4,170,000 |
| Virginia | 149 | 3,552,556,141 | 276,514 | 41,160,000 |
| Washington | 100 | 2,365,287,745 | 308,106 | 30,700,000 |
| West Virginia | 207 | 718,524,922 | 193,687 | 40,060,000 |
| Wisconsin | 159 | 1,691,505,297 | 180,826 | 28,700,000 |
| Wyoming | 162 | 219,040,247 | 233,470 | 37,970,000 |
| 1 | See: https://www.ers.usda.gov/data-products/chart-gallery/gallery/chart-detail/?chartId=102643 (accessed on 28 May 2024) |
| 2 | This value is adjusted to the 2020 dollar from the reported USD 7.4 million in 2006 dollars. |
| 3 | This cost is inflated to 2020 dollars from a reported USD 9763 cost of treating pneumonia without complication (Chen et al. 2020; Rae et al. 2020). |
| 4 | This cost is inflated to the 2020 dollar from reported USD 20,292 cost of treating pneumonia with ventilator in 2018 (Rae et al. 2020). |
| 5 | This cost is inflated to 2020 dollars from reported USD 61,168 cost of treating pneumonia with ventilator in 2018 (Rae et al. 2020). |
| 6 | This average cost of a one-way ambulance trip is adjusted to 2020 dollars from reported 2015 U.S. dollar costs of USD 463 (Peterson et al. 2021). |
| 7 | See Table A1 for the calculated potential loss of lifetime earnings in the U.S. by gender and age. |
| 8 | See Table A2. |
| 9 | See Note 8. |
| 10 | See Note 8. |
References
- Adler, Matthew. 2020. What Should We Spend to Save Lives in a Pandemic? A Critique of the Value of Statistical Life. Duke Law School Public Law & Legal Theory Series No. 2020-40. Available online: https://ssrn.com/abstract=3636550 (accessed on 20 March 2024).
- Adler, Matthew D., Maddalena Ferranna, James K. Hammitt, and Nicolas Treich. 2021. Fair innings? The utilitarian and prioritarian value of risk reduction over a whole lifetime. Journal of Health Economics 75: 102412. [Google Scholar] [CrossRef] [PubMed]
- Allen, Douglas W. 2020. COVID-19 lockdown cost/benefits: A critical assessment of the literature. International Journal of the Economics of Business 29: 1–32. [Google Scholar] [CrossRef]
- Bartsch, Sarah M., Marie C. Ferguson, James A. McKinnell, Kelly J. O’shea, Patrick T. Wedlock, Sheryl S. Siegmund, and Bruce Y. Lee. 2020. The potential health care costs and resources use associated with COVID-19 in the United States. Health Affairs 39: 927–35. [Google Scholar] [CrossRef] [PubMed]
- Chen, Jiangzhuo, Anil Vullikanti, Stefan Hoops, Henning Mortveit, Bryan Lewis, Srinivasan Venkatramanan, Wen You, Stephen Eubank, Madhav Marathe, Chris Barrett, and et al. 2020. Medical costs of keeping the US economy open during COVID-19. Science Report 10: 18422. [Google Scholar] [CrossRef] [PubMed]
- Colmer, Jonathan. 2020. What is the meaning of (statistical) life? benefit–cost analysis in the time of COVID-19. Oxford Review of Economic Policy 36: S56–S63. [Google Scholar] [CrossRef]
- Doran, Christopher M., Rod Ling, Jorgen Gullestrup, Sarah Swannell, and Allison Milner. 2015. The impact of a suicide prevention strategy on reducing the economic cost of suicide in the New South Wales construction industry. Crisis 37: 121–29. [Google Scholar] [CrossRef] [PubMed]
- Finkelstein, Eric R., Phaedra S. Corso, Ted R. Miller, Ian Fiebelkorn, and Eduard Zaloshnja. 2006. Incidence and Economic Burden of Injuries in the United States. New York: Oxford University Press, vol. 61. [Google Scholar] [CrossRef]
- Herrera-Araujo, Daniel, and Lise Rochaix. 2020. Does the value per statistical life vary with age or baseline health? evidence from a compensating wage study in france. Journal of Environmental Economics and Management 103: 102338. [Google Scholar] [CrossRef]
- Lawrence, Bruce, and Ted Miller. 2014. Medical and Work Loss Cost Estimation Methods for the WISQARS Cost of Injury Module. Calverton: Pacific Institute for Research & Evaluation. [Google Scholar] [CrossRef]
- National Center for Health Statistics. 2021a. Provisional COVID-19 Deaths by Place of Deaths. Centers for Disease Control and Prevention. Available online: https://data.cdc.gov/NCHS/Provisional-COVID-19-Deaths-by-Place-of-Death-and-/uggs-hy5q (accessed on 13 October 2021).
- National Center for Health Statistics. 2021b. Provisional COVID-19 Deaths by Sex and Age. Centers for Disease Control and Prevention. Available online: https://data.cdc.gov/NCHS/Provisional-COVID-19-Deaths-by-Sex-and-Age/9bhg-hcku (accessed on 13 October 2021).
- O’Dea, Des, and Sarah Tucker. 2005. The Cost of Suicide to Society. Wellington: Ministry of Health. ISBN 0-478-29638-X. [Google Scholar]
- Oliveira, Eduardo, Amay Parikh, Arnaldo Lopez-Ruiz, Maria Carrilo, Joshua Goldberg, Martin Cearras, Khaled Fernainy, Sonja Andersen, Luis Mercado, Jian Guan, and et al. 2021. Icu outcomes and survival in patients with severe COVID-19 in the largest healthcare system in central Florida. PLoS ONE 16: e0249038. [Google Scholar] [CrossRef] [PubMed]
- Peterson, Cora, Likang Xu, and Curtis Florence. 2021. Average medical cost of fatal and non-fatal injuries by type in the USA. Injury Prevention 27: 24–33. [Google Scholar] [CrossRef] [PubMed]
- Rae, Matthew, Gary Claxton, Nisha Kurani, Daniel McDermott, and Cynthia Cox. 2020. Potential Costs of Coronavirus Treatment for People with Employer Coverage. Peterson Center on Healthcare and Kaiser Family Foundation. Available online: https://www.healthsystemtracker.org/brief/potential-costs-of-coronavirus-treatment-for-people-with-employer-coverage/ (accessed on 18 November 2021).
- Ruggles, Steven, Sarah Flood, Sophia Foster, Ronald Goeken, Jose Pacas, Megan Schouweiler, and Matthew Sobek. 2021. IPUMS USA: Version 11.0 [Dataset]. Minneapolis: IPUMS. [Google Scholar] [CrossRef]
- Sweis, Nadia J. 2022. Revisiting the value of a statistical life: An international approach during COVID-19. Risk Management 24: 259–72. [Google Scholar] [CrossRef]
- Viscusi, W. Kip. 2010. The heterogeneity of the value of statistical life: Introduction and overview. Journal of Risk and Uncertainty 40: 1–13. [Google Scholar] [CrossRef]

| Place of Death | Medical Expense (USD) |
|---|---|
| Healthcare setting, inpatient | 25,134 |
| Hospice facility | 25,134 |
| Nursing home/long-term care facility | 25,134 |
| Healthcare setting, outpatient, or emergency room | 10,065 |
| Healthcare setting, dead on arrival | 3552 |
| Decedent’s home | 3045 |
| Other | 3045 |
| Place of death unknown | 3045 |
| Place of Death | COVID-19 Death Counts | Share of Death by Place of Death | Medical Expense per COVID-19 Death (USD) | Total Medical Expense (USD) |
|---|---|---|---|---|
| Healthcare setting, inpatient | 479,481 | 67.25% | 25,134 | 12,051,275,454 |
| Nursing home/long-term care facility | 118,568 | 16.63% | 25,134 | 2,980,088,112 |
| Decedent’s home | 54,600 | 7.66% | 3045 | 166,257,000 |
| Healthcare setting, outpatient or emergency room | 23,824 | 3.34% | 10,065 | 239,788,560 |
| Hospice facility | 21,299 | 2.99% | 25,134 | 535,329,066 |
| Other | 14,382 | 2.02% | 3045 | 43,793,190 |
| Healthcare setting, dead on arrival | 676 | 0.09% | 507 | 342,732 |
| Place of death unknown | 113 | 0.02% | 3045 | 344,085 |
| Total | 712,943 | 100.00% | 95,109 | 16,017,218,199 |
| State | Total Deaths | Total Direct Medical Cost (USD) | Average Medical Cost per Death (USD) |
|---|---|---|---|
| Alabama | 14,684 | 335,914,596 | 22,879 |
| Alaska | 568 | 12,524,487 | 21,446 |
| Arizona | 18,278 | 384,108,627 | 21,013 |
| Arkansas | 8239 | 188,017,356 | 22,809 |
| California | 73,095 | 1,591,595,313 | 21,774 |
| Colorado | 8068 | 176,695,824 | 21,890 |
| Connecticut | 8600 | 200,212,527 | 23,237 |
| Delaware | 1922 | 44,267,790 | 22,701 |
| District of Columbia | 1560 | 35,602,461 | 22,605 |
| Florida | 55,324 | 1,252,787,364 | 22,644 |
| Georgia | 23,787 | 535,474,761 | 22,505 |
| Hawaii | 847 | 18,157,230 | 21,616 |
| Idaho | 3047 | 65,395,074 | 21,392 |
| Illinois | 24,724 | 555,282,804 | 22,454 |
| Indiana | 15,585 | 358,367,985 | 22,977 |
| Iowa | 6765 | 156,720,924 | 23,142 |
| Kansas | 6033 | 137,273,445 | 22,754 |
| Kentucky | 10,036 | 227,707,896 | 22,691 |
| Louisiana | 12,400 | 279,503,703 | 22,526 |
| Maine | 1189 | 27,613,206 | 23,107 |
| Maryland | 11,228 | 249,875,100 | 22,245 |
| Massachusetts | 14,233 | 328,443,684 | 23,052 |
| Michigan | 20,031 | 449,865,921 | 22,455 |
| Minnesota | 8390 | 187,674,723 | 22,356 |
| Mississippi | 10,092 | 224,361,516 | 22,243 |
| Missouri | 14,472 | 332,890,197 | 22,983 |
| Montana | 2112 | 47,708,052 | 22,557 |
| Nebraska | 3287 | 72,741,297 | 22,070 |
| Nevada | 7583 | 171,019,257 | 22,538 |
| New Hampshire | 1479 | 33,950,337 | 22,785 |
| New Jersey | 25,846 | 597,093,870 | 23,096 |
| New Mexico | 4762 | 101,993,496 | 21,414 |
| New York | 27,029 | 624,404,730 | 23,093 |
| North Carolina | 18,194 | 415,735,065 | 22,836 |
| North Dakota | 1864 | 44,627,640 | 23,929 |
| Ohio | 25,973 | 597,228,924 | 22,981 |
| Oklahoma | 10,786 | 239,988,789 | 22,242 |
| Oregon | 4183 | 88,417,209 | 21,142 |
| Pennsylvania | 30,657 | 716,436,012 | 23,363 |
| Rhode Island | 2793 | 64,983,651 | 23,267 |
| South Carolina | 12,673 | 286,061,691 | 22,546 |
| South Dakota | 2224 | 52,683,147 | 23,509 |
| Tennessee | 17,946 | 406,048,833 | 22,626 |
| Texas | 71,557 | 1,594,115,499 | 22,278 |
| Utah | 3256 | 68,389,461 | 20,991 |
| Vermont | 280 | 6,355,032 | 22,066 |
| Virginia | 12,847 | 293,500,485 | 22,832 |
| Washington | 7676 | 168,565,422 | 21,926 |
| West Virginia | 3709 | 86,712,153 | 23,341 |
| Wisconsin | 9355 | 190,410,807 | 20,367 |
| Wyoming | 937 | 20,379,852 | 21,452 |
| Age Group | COVID-19 Deaths Count | Share of Deaths by Age Group |
|---|---|---|
| 0–29 years | 3888 | 0.62% |
| 30–39 years | 11,313 | 1.59% |
| 40–49 years | 28,190 | 3.95% |
| 50–64 years | 125,812 | 17.65% |
| 65–74 years | 160,596 | 22.53% |
| 75–84 years | 187,611 | 26.32% |
| 85 years and over | 195,007 | 27.35% |
| Total | 712,930 | 100.00% |
| State | Total Deaths | Total Indirect Cost of COVID-19 Deaths (USD) | 95% CI (USD) |
|---|---|---|---|
| Alabama | 14,684 | 4,166,435,191 | (3,008,062,021–5,324,808,362) |
| Alaska | 568 | 172,974,401 | (125,693,564–220,255,239) |
| Arizona | 18,278 | 5,513,321,292 | (4,069,500,344–6,957,142,239) |
| Arkansas | 8239 | 1,847,881,101 | (1,334,086,446–2,361,675,757 ) |
| California | 73,095 | 27,122,357,050 | (20,387,642,264–33,857,071,836) |
| Colorado | 8068 | 2,056,001,128 | (1,460,383,688–2,651,618,569) |
| Connecticut | 8600 | 1,715,996,791 | (1,096,085,580–2,335,908,002) |
| Delaware | 1922 | 363,730,295 | (225,093,804–502,366,787) |
| District of Columbia | 1560 | 917,015,700 | (675,362,756–1,158,668,643) |
| Florida | 55,324 | 15,029,803,511 | (11,160,848,564–18,898,758,459) |
| Georgia | 23,787 | 7,533,575,696 | (5,514,238,899–9,552,912,493) |
| Hawaii | 847 | 320,845,112 | (248,437,213–393,253,011) |
| Idaho | 3047 | 533,566,711 | (359,187,737–707,945,684) |
| Illinois | 24,724 | 6,210,397,909 | (4,378,844,507–8,041,951,310) |
| Indiana | 15,585 | 2,678,413,892 | (1,780,999,247–3,575,828,537) |
| Iowa | 6765 | 919,033,884 | (605,718,766–1,232,349,001) |
| Kansas | 6033 | 1,189,520,409 | (836,463,614–1,542,577,203) |
| Kentucky | 10,036 | 2,036,789,887 | (1,375,667,622–2,697,912,152) |
| Louisiana | 12,400 | 3,509,160,327 | (2,545,290,376–4,473,030,279) |
| Maine | 1189 | 153,858,219 | (96,475,528–211,240,911) |
| Maryland | 11,228 | 3,355,095,618 | (2,416,361,021–4,293,830,214) |
| Massachusetts | 14,233 | 2,463,564,315 | (1,584,595,310–3,342,533,319) |
| Michigan | 20,031 | 4,456,499,910 | (3,091,646,691–5,821,353,129) |
| Minnesota | 8390 | 1,284,212,967 | (866,977,370–1,701,448,563) |
| Mississippi | 10,092 | 2,666,618,278 | (1,950,576,501–3,382,660,055) |
| Missouri | 14,472 | 3,018,362,233 | (2,072,834,084–3,963,890,382) |
| Montana | 2112 | 377,640,221 | (265,480,985–489,799,456) |
| Nebraska | 3287 | 582,168,786 | (408,242,400–756,095,172) |
| Nevada | 7583 | 2,361,469,117 | (1,721,398,266–3,001,539,969) |
| New Hampshire | 1479 | 139,598,641 | (78,470,328–200,726,954) |
| New Jersey | 25,846 | 7,873,263,304 | (5,641,688,514–10,104,838,093) |
| New Mexico | 4762 | 1,499,079,119 | (1,138,029,657–1,860,128,581) |
| New York | 27,029 | 6,050,728,632 | (4,086,848,330–8,014,608,935) |
| North Carolina | 18,194 | 4,053,054,159 | (2,838,413,869–5,267,694,450) |
| North Dakota | 1864 | 322,261,046 | (209,097,142–435,424,949) |
| Ohio | 25,973 | 4,260,379,605 | (2,823,622,302–5,697,136,908) |
| Oklahoma | 10,786 | 2,638,626,283 | (1,865,616,320–3,411,636,246) |
| Oregon | 4183 | 1,000,980,660 | (730,818,499–1,271,142,820) |
| Pennsylvania | 30,657 | 5,242,045,789 | (3,486,172,086–6,997,919,493) |
| Rhode Island | 2793 | 366,845,074 | (223,971,222–509,718,926) |
| South Carolina | 12,673 | 3,305,364,218 | (2,372,581,409–4,238,147,028) |
| South Dakota | 2224 | 326,797,818 | (216,801,414–436,794,222) |
| Tennessee | 17,946 | 4,916,620,765 | (3,504,777,870–6,328,463,659) |
| Texas | 71,557 | 26,425,551,735 | (20,080,170,825–32,770,932,644) |
| Utah | 3256 | 1,098,311,127 | (830,605,869–1,366,016,385) |
| Vermont | 280 | 20,468,996 | (9,929,398–31,008,593) |
| Virginia | 12,847 | 3,259,055,656 | (2,279,464,560–4,238,646,752) |
| Washington | 7676 | 2,196,722,323 | (1,592,870,169–2,800,574,477) |
| West Virginia | 3709 | 631,812,769 | (408,989,376–854,636,163) |
| Wisconsin | 9355 | 1,501,094,490 | (1,022,729,795–1,979,459,184) |
| Wyoming | 937 | 198,660,395 | (130,313,534–267,007,256) |
| State | Total Deaths | Loss of Potential Lifetime Earnings (Indirect Cost) per Death (USD) | 95% CI (USD) |
|---|---|---|---|
| Alabama | 14,684 | 283,740 | (204,853–362,627) |
| Alaska | 568 | 304,532 | (221,291–387,773) |
| Arizona | 18,278 | 301,637 | (222,645–380,629) |
| Arkansas | 8239 | 224,285 | (161,923–286,646) |
| California | 73,095 | 371,056 | (278,920–463,193) |
| Colorado | 8068 | 254,834 | (181,009–328,659) |
| Connecticut | 8600 | 199,535 | (127,452–271,617) |
| Delaware | 1922 | 189,246 | (117,114–261,377) |
| District of Columbia | 1560 | 587,831 | (432,925–742,736) |
| Florida | 55,324 | 271,669 | (201,736–341,601) |
| Georgia | 23,787 | 316,710 | (231,817–401,602) |
| Hawaii | 847 | 378,802 | (293,314–464,289) |
| Idaho | 3047 | 175,112 | (117,882–232,342) |
| Illinois | 24,724 | 251,189 | (177,109–325,269) |
| Indiana | 15,585 | 171,858 | (114,277–229,440) |
| Iowa | 6765 | 135,851 | (89,537–182,165) |
| Kansas | 6033 | 197,169 | (138,648–255,690) |
| Kentucky | 10,036 | 202,948 | (137,073–268,823) |
| Louisiana | 12,400 | 282,997 | (205,265–360,728) |
| Maine | 1189 | 129,401 | (81,140–177,663) |
| Maryland | 11,228 | 298,815 | (215,209–382,422) |
| Massachusetts | 14,233 | 173,088 | (111,332–234,844) |
| Michigan | 20,031 | 222,480 | (154,343–290,617) |
| Minnesota | 8390 | 153,065 | (103,335–202,795) |
| Mississippi | 10,092 | 264,231 | (193,279–335,182) |
| Missouri | 14,472 | 208,566 | (143,231–273,901) |
| Montana | 2112 | 178,807 | (125,701–231,913) |
| Nebraska | 3287 | 177,113 | (124,199–230,026) |
| Nevada | 7583 | 311,416 | (227,008–395,825) |
| New Hampshire | 1479 | 94,387 | (53,056–135,718) |
| New Jersey | 25,846 | 304,622 | (218,281–390,963) |
| New Mexico | 4762 | 314,800 | (238,981–390,619) |
| New York | 27,029 | 223,861 | (151,202–296,519) |
| North Carolina | 18,194 | 222,769 | (156,008–289,529) |
| North Dakota | 1864 | 172,887 | (112,177–233,597) |
| Ohio | 25,973 | 164,031 | (108,714–219,348) |
| Oklahoma | 10,786 | 244,634 | (172,966–316,302) |
| Oregon | 4183 | 239,297 | (174,712–303,883) |
| Pennsylvania | 30,657 | 170,990 | (113,715–228,265) |
| Rhode Island | 2793 | 131,344 | (80,190–182,499) |
| South Carolina | 12,673 | 260,819 | (187,215–334,423) |
| South Dakota | 2224 | 146,941 | (97,483–196,400) |
| Tennessee | 17,946 | 273,968 | (195,296–352,639) |
| Texas | 71,557 | 369,294 | (280,618–457,970) |
| Utah | 3256 | 337,319 | (255,100–419,538) |
| Vermont | 280 | 73,104 | (35,462–110,745) |
| Virginia | 12,847 | 253,682 | (177,432–329,933) |
| Washington | 7676 | 286,181 | (207,513–364,848) |
| West Virginia | 3709 | 170,346 | (110,269–230,422) |
| Wisconsin | 9355 | 160,459 | (109,324–211,594) |
| Wyoming | 937 | 212,018 | (139,075–284,960) |
| State | Total Direct Medical Cost (USD) | Total Indirect Cost of Loss Potential Lifetime Earnings (USD) | Total Cost (USD) |
|---|---|---|---|
| Alabama | 335,914,596 | 4,166,435,191 | 4,502,349,787 |
| Alaska | 12,524,487 | 172,974,401 | 185,498,888 |
| Arizona | 384,108,627 | 5,513,321,292 | 5,897,429,919 |
| Arkansas | 188,017,356 | 1,847,881,101 | 2,035,898,457 |
| California | 1,591,595,313 | 27,122,357,050 | 28,713,952,363 |
| Colorado | 176,695,824 | 2,056,001,128 | 2,232,696,952 |
| Connecticut | 200,212,527 | 1,715,996,791 | 1,916,209,318 |
| Delaware | 44,267,790 | 363,730,295 | 407,998,085 |
| District of Columbia | 35,602,461 | 917,015,700 | 952,618,161 |
| Florida | 1,252,787,364 | 15,029,803,511 | 16,282,590,875 |
| Georgia | 535,474,761 | 7,533,575,696 | 8,069,050,457 |
| Hawaii | 18,157,230 | 320,845,112 | 339,002,342 |
| Idaho | 65,395,074 | 533,566,711 | 598,961,785 |
| Illinois | 555,282,804 | 6,210,397,909 | 6,765,680,713 |
| Indiana | 358,367,985 | 2,678,413,892 | 3,036,781,877 |
| Iowa | 156,720,924 | 919,033,884 | 1,075,754,808 |
| Kansas | 137,273,445 | 1,189,520,409 | 1,326,793,854 |
| Kentucky | 227,707,896 | 2,036,789,887 | 2,264,497,783 |
| Louisiana | 279,503,703 | 3,509,160,327 | 3,788,664,030 |
| Maine | 27,613,206 | 153,858,219 | 181,471,425 |
| Maryland | 249,875,100 | 3,355,095,618 | 3,604,970,718 |
| Massachusetts | 328,443,684 | 2,463,564,315 | 2,792,007,999 |
| Michigan | 449,865,921 | 4,456,499,910 | 4,906,365,831 |
| Minnesota | 187,674,723 | 1,284,212,967 | 1,471,887,690 |
| Mississippi | 224,361,516 | 2,666,618,278 | 2,890,979,794 |
| Missouri | 332,890,197 | 3,018,362,233 | 3,351,252,430 |
| Montana | 47,708,052 | 377,640,221 | 425,348,273 |
| Nebraska | 72,741,297 | 582,168,786 | 654,910,083 |
| Nevada | 171,019,257 | 2,361,469,117 | 2,532,488,374 |
| New Hampshire | 33,950,337 | 139,598,641 | 173,548,978 |
| New Jersey | 597,093,870 | 7,873,263,304 | 8,470,357,174 |
| New Mexico | 101,993,496 | 1,499,079,119 | 1,601,072,615 |
| New York | 624,404,730 | 6,050,728,632 | 6,675,133,362 |
| North Carolina | 415,735,065 | 4,053,054,159 | 4,468,789,224 |
| North Dakota | 44,627,640 | 322,261,046 | 366,888,686 |
| Ohio | 597,228,924 | 4,260,379,605 | 4,857,608,529 |
| Oklahoma | 239,988,789 | 2,638,626,283 | 2,878,615,072 |
| Oregon | 88,417,209 | 1,000,980,660 | 1,089,397,869 |
| Pennsylvania | 716,436,012 | 5,242,045,789 | 5,958,481,801 |
| Rhode Island | 64,983,651 | 366,845,074 | 431,828,725 |
| South Carolina | 286,061,691 | 3,305,364,218 | 3,591,425,909 |
| South Dakota | 52,683,147 | 326,797,818 | 379,480,965 |
| Tennessee | 406,048,833 | 4,916,620,765 | 5,322,669,598 |
| Texas | 1,594,115,499 | 26,425,551,735 | 28,019,667,234 |
| Utah | 68,389,461 | 1,098,311,127 | 1,166,700,588 |
| Vermont | 6,355,032 | 20,468,996 | 26,824,028 |
| Virginia | 293,500,485 | 3,259,055,656 | 3,552,556,141 |
| Washington | 168,565,422 | 2,196,722,323 | 2,365,287,745 |
| West Virginia | 86,712,153 | 631,812,769 | 718,524,922 |
| Wisconsin | 190,410,807 | 1,501,094,490 | 1,691,505,297 |
| Wyoming | 20,379,852 | 198,660,395 | 219,040,247 |
| Cost | Mean (USD) | 95% CI (USD) |
|---|---|---|
| Total Direct medical cost of COVID-19 deaths | 16,017,218,199 | NA |
| Total Indirect cost of COVID-19 deaths | 181,883,632,555 | ( 131,234,177,661–232,533,087,449) |
| Total economic cost of COVID-19 deaths | 197,900,850,754 | ( 147,251,395,860–248,550,305,648) |
| Average Cost | Mean (USD) | 95% CI (USD) |
|---|---|---|
| Average direct medical cost per death | 22,466 | NA |
| Average indirect cost per death | 255,121 | ( 184,077–326,165) |
| Average total economic cost per death | 277,587 | ( 206,543–348,631) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pham, T.; Ruhil, A.V.S.; Jolley, G.J. The Opportunity Cost of COVID-19 Deaths in the USA. Economies 2024, 12, 146. https://doi.org/10.3390/economies12060146
Pham T, Ruhil AVS, Jolley GJ. The Opportunity Cost of COVID-19 Deaths in the USA. Economies. 2024; 12(6):146. https://doi.org/10.3390/economies12060146
Chicago/Turabian StylePham, Tuyen, Anirudh V. S. Ruhil, and G. Jason Jolley. 2024. "The Opportunity Cost of COVID-19 Deaths in the USA" Economies 12, no. 6: 146. https://doi.org/10.3390/economies12060146
APA StylePham, T., Ruhil, A. V. S., & Jolley, G. J. (2024). The Opportunity Cost of COVID-19 Deaths in the USA. Economies, 12(6), 146. https://doi.org/10.3390/economies12060146






