Application and Challenges of the Technology Acceptance Model in Elderly Healthcare: Insights from ChatGPT
Abstract
1. Introduction
Background
2. Materials and Methods
2.1. Study Design
2.2. ChatGPT as a Study Tool
2.3. Study Procedures
2.4. Ethical Considerations
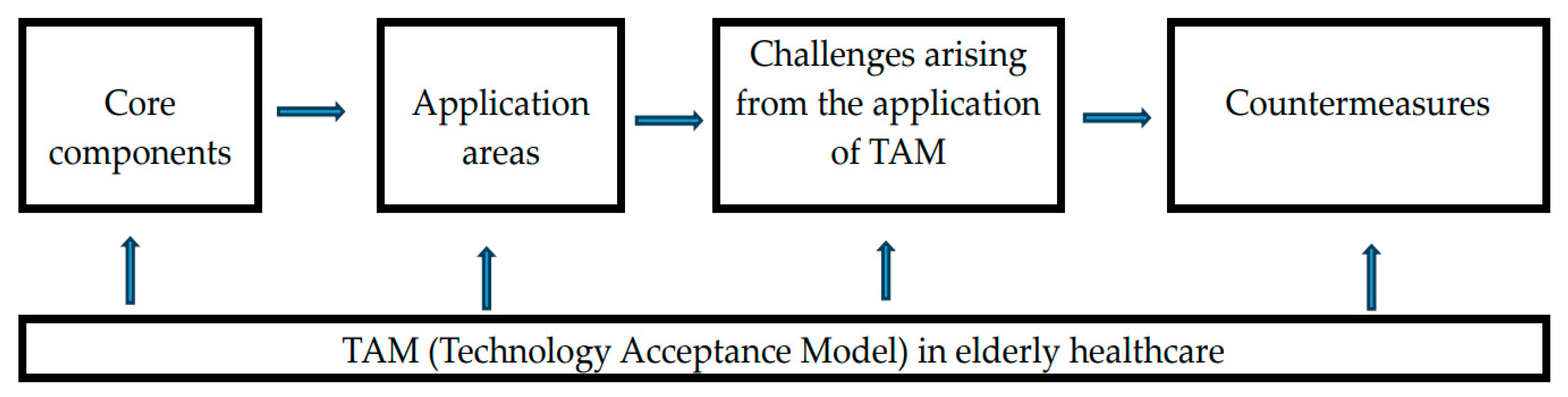
3. Results
3.1. Core Components of TAM in Elderly Healthcare
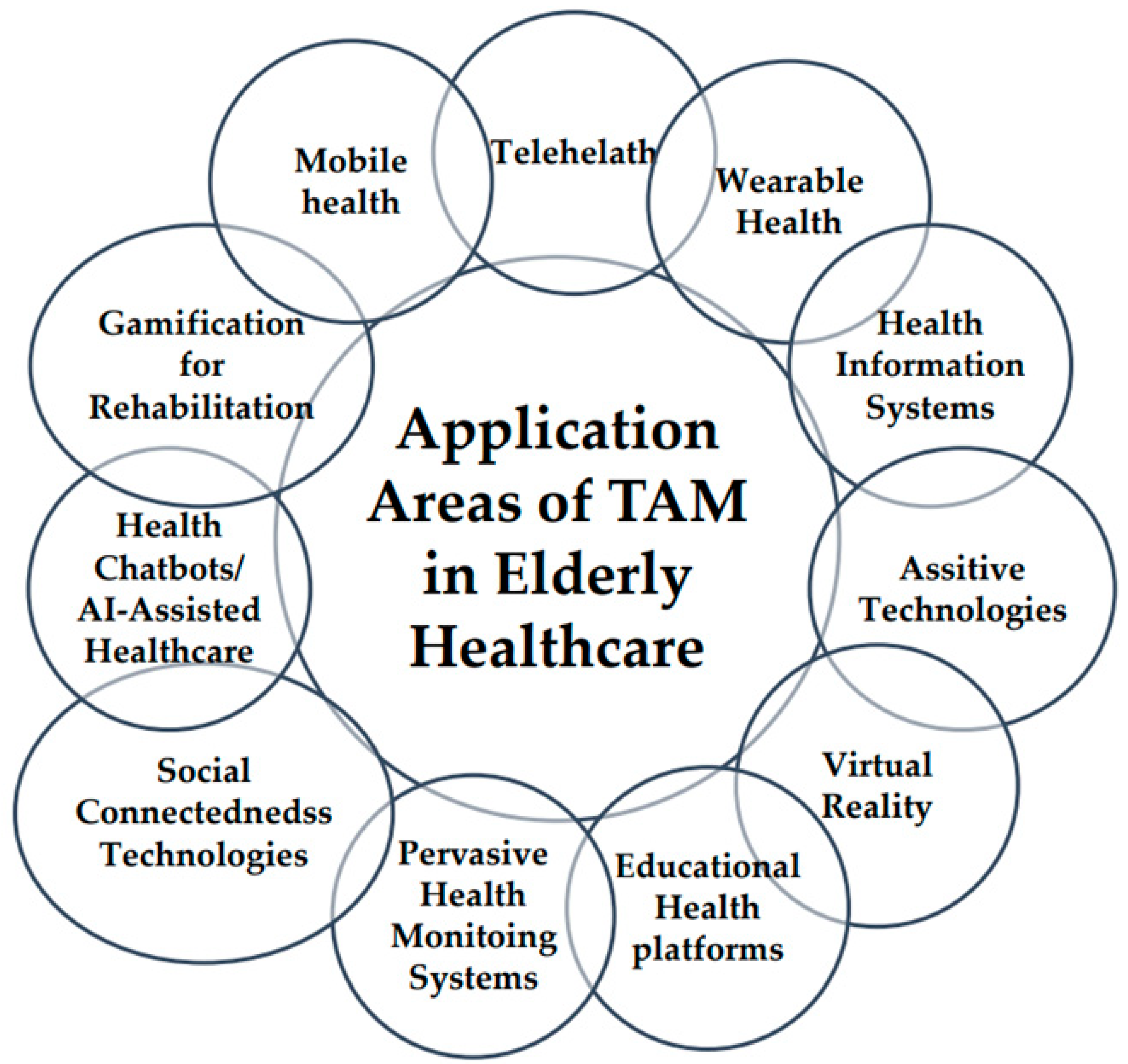
3.2. Application Areas of TAM in Elderly Healthcare
3.3. Challenges Arising from the Application of TAM in Elderly Healthcare
4. Discussion
4.1. Core Components of TAM in Elderly Healthcare
4.2. Application Areas of TAM in Elderly Healthcare
4.3. Challenges and Countermeasures for the Application of TAM in Elderly Healthcare
4.4. Implications and Recommendations for TAM in Elderly Healthcare
4.5. Strengths and Limitations of the Present Study
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Schroeder, T.; Dodds, L.; Georgiou, A.; Gewald, H.; Siette, J. Older adults and new technology: Mapping review of the factors associated with older adults’ intention to adopt digital technologies. JMIR Aging 2023, 6, e44564. [Google Scholar] [CrossRef] [PubMed]
- Ferizaj, D.; Perotti, L.; Dahms, R.; Heimann-Steinert, A. Use of technology in old age: Associations between acceptance, competence, control, interest and social indicators in individuals over 60 years old. Z. Gerontol. Geriatr. 2024, 57, 227–234. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Chow, B.C.; Park, S.; Liu, H. The usage of digital health technology among older adults in Hong Kong and the role of technology readiness and ehealth literacy: Path analysis. J. Med. Internet Res. 2023, 25, e41915. [Google Scholar] [CrossRef] [PubMed]
- Nadal, C.; Sas, C.; Doherty, G. Technology acceptance in mobile health: Scoping review of definitions, models, and measurement. J. Med. Internet Res. 2020, 22, e17256. [Google Scholar] [CrossRef] [PubMed]
- Liu, M.; Wang, C.; Hu, J. Older adults’ intention to use voice assistants: Usability and emotional needs. Heliyon 2023, 9, e21932. [Google Scholar] [CrossRef] [PubMed]
- Kwan, R.Y.C.; Yeung, J.W.Y.; Lee, J.L.C.; Lou, V.W.Q. The association of technology acceptance and physical activity on frailty in older adults during the COVID-19 pandemic period. Eur. Rev. Aging Phys. Act. 2023, 20, e24. [Google Scholar] [CrossRef]
- Mannheim, I.; Varlamova, M.; van Zaalen, Y.; Wouters, E.J.M. The role of ageism in the acceptance and use of digital technology. J. Appl. Gerontol. 2023, 42, 1283–1294. [Google Scholar] [CrossRef]
- Harris, M.T.; Rogers, W.A. Developing a healthcare technology acceptance model (H-TAM) for older adults with hypertension. Ageing Soc. 2023, 43, 814–834. [Google Scholar] [CrossRef] [PubMed]
- Murciano Hueso, A.; Martín García, A.V.; Torrijos Fincias, P. Systematic review of digital technology acceptance in older adults. Perspective of TAM models. Rev. Esp. Geriatr. Gerontol. 2022, 57, 105–117. [Google Scholar] [CrossRef]
- Moxley, J.; Sharit, J.; Czaja, S.J. The factors influencing older adults’ decisions surrounding adoption of technology: Quantitative experimental study. JMIR Aging 2022, 5, e39890. [Google Scholar] [CrossRef]
- Martín-García, A.V.; Redolat, R.; Pinazo-Hernandis, S. factors influencing intention to technological use in older adults. the tam model application. Res. Aging 2022, 44, 573–588. [Google Scholar] [CrossRef] [PubMed]
- Davis, F. A Technology Acceptance Model for Empirically Testing New End-User Information Systems: Theory and Results; Massachusetts Institute of Technology: Cambridge, MA, USA, 1986; pp. 233–250. [Google Scholar]
- Kim, J.; Park, H. Development of a health information technology acceptance model using consumers’ health behavior intention. J. Med. Internet Res. 2012, 14, e133. [Google Scholar] [CrossRef] [PubMed]
- Davis, F.D. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Q. 1989, 3, 319–340. [Google Scholar] [CrossRef]
- Akritidi, D.; Gallos, P.; Koufi, V.; Malamateniou, F. Using an extended technology acceptance model to evaluate digital health services. Stud. Health Technol. Inform. 2022, 295, 530–533. [Google Scholar] [CrossRef] [PubMed]
- Ammenwerth, E. Technology acceptance models in health informatics: TAM and UTAUT. Stud. Health Technol. Inform. 2019, 263, 64–71. [Google Scholar] [CrossRef] [PubMed]
- Hendricks, J.W.; Smith, A.; Peres, S.C.; Sasangohar, F. Workers’ acceptance of digital procedures: An application of the technology acceptance model. IISE Trans. Occup. Ergon. Hum. Factors 2023, 11, 59–68. [Google Scholar] [CrossRef]
- Witlox, M.; Kraaij, V.; Garnefski, N.; Bohlmeijer, E.; Smit, F.; Spinhoven, P. Cost-effectiveness and cost-utility of an Acceptance and commitment therapy intervention vs. a cognitive behavioral therapy intervention for older adults with anxiety symptoms: A randomized controlled trial. PLoS ONE 2022, 17, e0262220. [Google Scholar] [CrossRef] [PubMed]
- Almulhem, J.A. Factors, barriers, and recommendations related to mobile health acceptance among the elderly in Saudi Arabia: A qualitative study. Healthcare 2023, 11, 3024. [Google Scholar] [CrossRef] [PubMed]
- ChatGPT. Available online: https://chat.openai.com/c/61b4f7d9-059b-4836-a5b1-830dc3b077bf (accessed on 1 January 2024).
- Shin, H.R.; Um, S.R.; Yoon, H.J.; Choi, E.Y.; Shin, W.C.; Lee, H.Y.; Kim, Y.S. Comprehensive senior technology acceptance model of daily living assistive technology for older adults with frailty: Cross-sectional study. J. Med. Internet Res. 2023, 25, e41935. [Google Scholar] [CrossRef]
- Byrd, T.F., 4th; Kim, J.S.; Yeh, C.; Lee, J.; O’Leary, K.J. Technology acceptance and critical mass: Development of a consolidated model to explain the. actual use of mobile health care communication tools. J. Biomed. Inform. 2021, 117, e103749. [Google Scholar] [CrossRef]
- Hulsen, T. Explainable artificial intelligence (XAI): Concepts and challenges in healthcare. AI 2023, 4, 652–666. [Google Scholar] [CrossRef]
- Balki, E.; Holland, C.; Hayes, N. Use and acceptance of digital communication technology by older adults for social connectedness during the covid-19 pandemic: Mixed methods study. J. Med. Internet Res. 2023, 25, e41535. [Google Scholar] [CrossRef] [PubMed]
- Yau, Y.; Hsiao, C.H. The technology acceptance model and older adults’ exercise intentions-a systematic literature review. Geriatrics 2022, 7, 124. [Google Scholar] [CrossRef] [PubMed]
- Wei, W.; Gong, X.; Li, J.; Tian, K.; Xing, K. A study on community older people’s willingness to use smart home-an extended technology acceptance model with intergenerational relationships. Front. Public Health 2023, 11, e1139667. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.Y.W.; Sorwar, G.; Rahman, M.S.; Hoque, M.R. The role of trust and habit in the adoption of mHealth by older adults in Hong Kong: A healthcare technology service acceptance (HTSA) model. BMC Geriatr. 2023, 23, e73. [Google Scholar] [CrossRef] [PubMed]
- Turnbull, N.; Tudpor, K.; Chimphoklang, S.; Siladlao, S.; Kamonroek, N.; Tatiyaworawattanakul, K.H. Development of OSOMO prompt mobile application on elderly population for village health volunteers using the analysis, design, development, implementation, and evaluation (ADDIE) model. Stud. Health Technol. Inform. 2023, 302, 222–226. [Google Scholar] [CrossRef] [PubMed]
- Jaschinski, C.; Ben Allouch, S.; Peters, O.; Cachucho, R.; van Dijk, J.A.G.M. Acceptance of technologies for aging in place: A conceptual model. J. Med. Internet Res. 2021, 23, e22613. [Google Scholar] [CrossRef] [PubMed]
- Tural, E.; Lu, D.; Austin Cole, D. Safely and actively aging in place: Older adults’ attitudes and intentions toward smart home technologies. Gerontol. Geriatr. Med. 2021, 7, e23337214211017340. [Google Scholar] [CrossRef] [PubMed]
- Portz, J.D.; Bayliss, E.A.; Bull, S.; Boxer, R.S.; Bekelman, D.B.; Gleason, K.; Czaja, S. using the technology acceptance model to explore user experience, intent to use, and use behavior of a patient portal among older adults with multiple chronic conditions: Descriptive qualitative study. J. Med. Internet Res. 2019, 21, e11604. [Google Scholar] [CrossRef]
- Jokisch, M.R.; Schmidt, L.I.; Doh, M. Acceptance of digital health services among older adults: Findings on perceived usefulness, self-efficacy, privacy concerns, ICT knowledge, and support seeking. Front. Public Health 2022, 10, e1073756. [Google Scholar] [CrossRef]
- Nai, Z.L.; Tan, W.S.; Tov, W. Acceptance of communication technology, emotional support and subjective well-being for Chinese older adults living alone during COVID-19: A moderated mediation model. PLoS ONE 2023, 18, e0291806. [Google Scholar] [CrossRef] [PubMed]
- Doré, B.; Gaudreault, A.; Everard, G.; Ayena, J.C.; Abboud, A.; Robitaille, N.; Batcho, C.S. Acceptability, feasibility, and effectiveness of immersive virtual technologies to promote exercise in older adults: A systematic review and meta-analysis. Sensors 2023, 23, 2506. [Google Scholar] [CrossRef] [PubMed]
- Klein, B.; Schlömer, I. A robotic shower system: Acceptance and ethical issues. Z. Gerontol. Geriatr. 2018, 51, 25–31. [Google Scholar] [CrossRef] [PubMed]
- Marston, H.R.; Samuels, J. A review of age friendly virtual assistive technologies and their effect on daily living for carers and dependent adults. Healthcare 2019, 7, 49. [Google Scholar] [CrossRef]
- Yu, J.; Huang, J.; Yang, Q. Long-term adoption or abandonment of smart technology in the Chinese elderly home care environment: A qualitative research study. Healthcare 2023, 11, 2440. [Google Scholar] [CrossRef] [PubMed]
- Shaffer, K.M.; Turner, K.L.; Siwik, C.; Gonzalez, B.D.; Upasani, R.; Glazer, J.V.; Ferguson, R.J.; Joshua, C.; Low, C.A. Digital health and telehealth in cancer care: A scoping review of reviews. Lancet Digit. Health 2023, 5, e316–e327. [Google Scholar] [CrossRef] [PubMed]
- Sapci, A.H.; Sapci, H.A. Innovative assisted living tools, remote monitoring technologies, artificial intelligence-driven solutions, and robotic systems for aging societies: Systematic review. JMIR Aging 2019, 2, e15429. [Google Scholar] [CrossRef] [PubMed]
- Chagnon, M.; Levasseur, M.; Boissy, P. Telehealth interventions in occupational therapy with older adults: Results from a scoping review targeting better health promotion. Aust. Occup. Ther. J. 2024, 71, 190–208. [Google Scholar] [CrossRef] [PubMed]
- Rush, K.L.; Singh, S.; Seaton, C.L.; Burton, L.; Li, E.; Jones, C.; Davis, J.C.; Hasan, K.; Kern, B.; Janke, R. Telehealth use for enhancing the health of rural older adults: A systematic mixed studies review. Gerontologist 2022, 62, e564–e577. [Google Scholar] [CrossRef]
- Li, W.; Gui, J.; Luo, X.; Yang, J.; Zhang, T.; Tang, Q. Determinants of intention with remote health management service among urban older adults: A unified theory of acceptance and use of technology perspective. Front. Public Health 2023, 11, e1117518. [Google Scholar] [CrossRef]
- Turcotte, S.; Bouchard, C.; Rousseau, J.; DeBroux Leduc, R.; Bier, N.; Kairy, D.; Dang-Vu, T.T.; Sarimanukoglu, K.; Dubé, F.; Bourgeois Racine, C.; et al. Factors influencing older adults’ participation in telehealth interventions for primary prevention and health promotion: A rapid review. Australas J. Ageing 2024, 43, 11–30. [Google Scholar] [CrossRef] [PubMed]
- Middlemass, J.B.; Vos, J.; Siriwardena, A.N. Perceptions on use of home telemonitoring in patients with long term conditions–concordance with the Health information technology acceptance model: A qualitative collective case study. BMC Med. Inform. Decis. Mak. 2017, 17, e89. [Google Scholar] [CrossRef] [PubMed]
- Knapova, L.; Klocek, A.; Elavsky, S. The role of psychological factors in older adults’ readiness to use ehealth technology: Cross-sectional questionnaire study. J. Med. Internet Res. 2020, 22, e14670. [Google Scholar] [CrossRef] [PubMed]
- Chow, H.W.; Yang, C.C. Accuracy of optical heart rate sensing technology in wearable fitness trackers for young and older adults: Validation and comparison study. JMIR mHealth uHealth 2020, 8, e14707. [Google Scholar] [CrossRef] [PubMed]
- Miguel Cruz, A.; Lopez Portillo, H.P.; Daum, C.; Rutledge, E.; King, S.; Liu, L. Technology acceptance and usability of a mobile app to support the workflow of health care aides who provide services to older adults: Pilot mixed methods study. JMIR Aging 2022, 5, e37521. [Google Scholar] [CrossRef] [PubMed]
- Pywell, J.; Vijaykumar, S.; Dodd, A.; Coventry, L. Barriers to older adults’ uptake of mobile-based mental health interventions. Digit. Health 2020, 6, e2055207620905422. [Google Scholar] [CrossRef] [PubMed]
- Abolhassani, N.; Santos-Eggimann, B.; Chiolero, A.; Santschi, V.; Henchoz, Y. Readiness to accept health information and communication technologies: A population-based survey of community-dwelling older adults. Int. J. Med. Inform. 2019, 130, e103950. [Google Scholar] [CrossRef] [PubMed]
- Walker, B.A. The acceptance and use of virtual gaming as an intervention strategy for older adults in occupational therapy. Games Health J. 2014, 3, 333–340. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.; Li, H.J. Acceptability assessment of an executive function training game fisherman for older adults. Games Health J. 2024, 13, 25–32. [Google Scholar] [CrossRef]
- Syed-Abdul, S.; Malwade, S.; Nursetyo, A.A.; Sood, M.; Bhatia, M.; Barsasella, D.; Liu, M.F.; Chang, C.C.; Srinivasan, K.; Li, Y.J.; et al. Virtual reality among the elderly: A usefulness and acceptance study from Taiwan. BMC Geriatr. 2019, 19, e223. [Google Scholar] [CrossRef]
- Hosseini, M.; Thomas, R.; Pilutti, L.; Fallavollita, P.; Jutai, J.W. Assessing virtual reality acceptance in long-term care facilities: A quantitative study with older adults. Disabil. Rehabil. Assist. Technol. 2023, 18, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Cook, N.; Winkler, S.L. Aceptance, usability and health applications of virtual worlds by older adults: A feasibility study. JMIR Res. Protoc. 2016, 5, e81. [Google Scholar] [CrossRef] [PubMed]
- Hurmuz, M.Z.; Jansen-Kosterink, S.M.; Hermens, H.J.; van Velsen, L. Game not over: Explaining older adults’ use and intention to continue using a gamified eHealth service. Health Inform. J. 2022, 28, e14604582221106008. [Google Scholar] [CrossRef] [PubMed]
- Shore, L.; de Eyto, A.; O’Sullivan, L. Technology acceptance and perceptions of robotic assistive devices by older adults–implications for exoskeleton design. Disabil. Rehabil. Assist. Technol. 2022, 17, 782–790. [Google Scholar] [CrossRef]
- Ramírez-Correa, P.E.; Arenas-Gaitán, J.; Rondán-Cataluña, F.J.; Grandon, E.E.; Ramírez-Santana, M. Adoption of social networking sites among older adults: The role of the technology readiness and the generation to identifying segments. PLoS ONE 2023, 18, e0284585. [Google Scholar] [CrossRef] [PubMed]
- Ramírez-Correa, P.; Grandón, E.E.; Ramírez-Santana, M.; Arenas-Gaitán, J.; Rondán-Cataluña, F.J. Explaining the consumption technology acceptance in the elderly post-pandemic: Effort expectancy does not matter. Behav. Sci. 2023, 13, 87. [Google Scholar] [CrossRef] [PubMed]
- He, Y.; He, Q.; Liu, Q. Technology acceptance in socially assistive robots: Scoping review of models, measurement, and influencing factors. J. Healthc. Eng. 2022, 2022, e6334732. [Google Scholar] [CrossRef] [PubMed]
- Mois, G.; Beer, J.M. The role of healthcare robotics in providing support to older adults: A socio-ecological perspective. Curr. Geriatr. Rep. 2020, 9, 82–89. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Shen, S.; Yang, J.; Tang, Q. Internet-based medical service use and eudaimonic well-being of urban older adults: A peer support and technology acceptance model. Int. J. Environ. Res. Public Health 2021, 18, 12062. [Google Scholar] [CrossRef]
- Ha, J.; Park, H.K. Factors affecting the acceptability of technology in health care among older korean adults with multiple chronic conditions: A cross-sectional study adopting the senior technology acceptance model. Clin. Intervation Aging 2020, 15, 1873–1881. [Google Scholar] [CrossRef]
- Arnaert, A.; Sumbly, P.; da Costa, D.; Liu, Y.; Debe, Z.; Charbonneau, S. Acceptance of the apple watch series 6 for telemonitoring of older adults with chronic obstructive pulmonary disease: Qualitative descriptive study part 1. JMIR Aging 2023, 6, e41549. [Google Scholar] [CrossRef]
- Arcury, T.A.; Sandberg, J.C.; Melius, K.P.; Quandt, S.A.; Leng, X.; Latulipe, C.; Miller, D.P.J.; Smith, D.A.; Bertoni, A.G. Older adult internet use and ehealth literacy. J. Appl. Gerontol. 2020, 39, 141–150. [Google Scholar] [CrossRef] [PubMed]
- Kuo, S.H.; Liang, M.H. Development and validation of the health literacy scale for community-dwelling older adults in Taiwan. Health Promot. Int. 2023, 38, daad112. [Google Scholar] [CrossRef] [PubMed]
- Chan, D.Y.L.; Chong, C.Y.; The, P.L.; Lee, S.W.H. What drives low-income older adults’ intention to use mobility applications? Geriatr. Gerontol. Int. 2024, 24, 342–350. [Google Scholar] [CrossRef]
- Kebede, A.S.; Ozolins, L.L.; Holst, H.; Galvin, K. Digital engagement of older adults: Scoping review. J. Med. Internet Res. 2022, 24, e40192. [Google Scholar] [CrossRef] [PubMed]
- Tsai, T.H.; Lin, W.Y.; Chang, Y.S.; Chang, P.C.; Lee, M.Y. Technology anxiety and resistance to change behavioral study of a wearable cardiac warming system using an extended TAM for older adults. PLoS ONE 2020, 15, e0227270. [Google Scholar] [CrossRef]
- Dosso, J.A.; Bandari, E.; Malhotra, A.; Guerra, G.K.; Hoey, J.; Michaud, F.; Prescott, T.J.; Robillard, J.M. User perspectives on emotionally aligned social robots for older adults and persons living with dementia. J. Rehabil. Assist. Technol. Eng. 2022, 9, e20556683221108364. [Google Scholar] [CrossRef] [PubMed]
- Zhao, D.; Sun, X.; Shan, B.; Yang, Z.; Yang, J.; Liu, H.; Jiang, Y.; Hiroshi, Y. Research status of elderly-care robots and safe human-robot interaction methods. Front. Neurosci. 2023, 17, e1291682. [Google Scholar] [CrossRef] [PubMed]
- Gionfrida, L.; Nuckols, R.W.; Walsh, C.J.; Howe, R.D. Age-related reliability of b-mode analysis for tailored exosuit assistance. Sensors 2023, 23, 1670. [Google Scholar] [CrossRef]
- Chu, L.; Chen, H.W.; Cheng, P.Y.; Ho, P.; Weng, I.T.; Yang, P.L.; Chien, S.E.; Tu, Y.C.; Yang, C.C.; Wang, T.M.; et al. Identifying features that enhance older adults’ acceptance of robots: A mixed methods study. Gerontology 2019, 65, 441–450. [Google Scholar] [CrossRef]
- Stara, V.; Rampioni, M.; Moșoi, A.A.; Kristaly, D.M.; Moraru, S.A.; Paciaroni, L.; Paolini, S.; Raccichini, A.; Felici, E.; Cucchieri, G.; et al. The impact of a multicomponent platform intervention on the daily lives of older adults. Healthcare 2023, 11, 3102. [Google Scholar] [CrossRef]
- Money, A.G.; Atwal, A.; Young, K.L.; Day, Y.; Wilson, L.; Money, K.G. Using the technology acceptance model to explore community dwelling older adults’ perceptions of a 3D interior design application to facilitate pre-discharge home adaptations. BMC Med. Inform. Decis. Mak. 2015, 15, e73. [Google Scholar] [CrossRef] [PubMed]
- Peek, S.T.; Luijkx, K.G.; Rijnaard, M.D.; Nieboer, M.E.; van der Voort, C.S.; Aarts, S.; van Hoof, J.; Vrijhoef, H.J.; Wouters, E.J. Older adults’ reasons for using technology while aging in place. Gerontology 2016, 62, 226–237. [Google Scholar] [CrossRef]
- Ahadzadeh, A.S.; Pahlevan Sharif, S.; Ong, F.S.; Khong, K.W. Integrating health belief model and technology acceptance model: An investigation of health-related internet use. J. Med. Internet Res. 2015, 17, e45. [Google Scholar] [CrossRef] [PubMed]
- Wildenbos, G.A.; Peute, L.; Jaspers, M. Facilitators and barriers of electronic health record patient portal adoption by older adults: A literature study. Stud. Health Technol. Inform. 2017, 235, 308–312. [Google Scholar] [PubMed]
- Li, J.; Ma, Q.; Chan, A.H.; Man, S.S. Health monitoring through wearable technologies for older adults: Smart wearables acceptance model. Appl. Ergon. 2019, 75, 162–169. [Google Scholar] [CrossRef]
- Cimperman, M.; Makovec Brenčič, M.; Trkman, P. Analyzing older users’ home telehealth services acceptance behavior-applying an Extended UTAUT model. Int. J. Med. Inform. 2016, 90, 22–31. [Google Scholar] [CrossRef] [PubMed]
- Kim, U.; Chung, T.; Park, E. Quality characteristics and acceptance intention for healthcare kiosks: Perception of elders from South Korea based on the extended technology acceptance model. Int. J. Environ. Res. Public Health 2022, 19, 16485. [Google Scholar] [CrossRef] [PubMed]
- Venkatesh, V.; Morris, M.G.; Davis, G.B.; Davis, F.D. User acceptance of information technology: Toward a unified view. MIS Q. 2003, 27, 425–478. [Google Scholar] [CrossRef]
- Peek, S.T.; Wouters, E.J.; van Hoof, J.; Luijkx, K.G.; Boeije, H.R.; Vrijhoef, H.J. Factors influencing acceptance of technology for aging in place: A systematic review. Int. J. Med. Inform. 2014, 83, 235–248. [Google Scholar] [CrossRef]
- Wildenbos, G.A.; Peute, L.; Jaspers, M. Aging barriers influencing mobile health usability for older adults: A literature based framework (MOLD-US). Int. J. Med. Inform. 2018, 114, 66–75. [Google Scholar] [CrossRef] [PubMed]
- Mitzner, T.L.; Boron, J.B.; Fausset, C.B.; Adams, A.E.; Charness, N.; Czaja, S.J.; Sharit, J. Older adults talk technology: Technology usage and attitudes. Comput. Human. Behav. 2010, 26, 1710–1721. [Google Scholar] [CrossRef] [PubMed]

| ChatGPT’s Responses | Previous Studies * | |
|---|---|---|
| Perceived Usefulness (PU): | The degree to which elderly individuals believe that using a particular technology will enhance their healthcare experience. In the context of elderly healthcare, perceived usefulness may involve improvements in health monitoring, access to medical information, or assistance with daily living. | [8,14,15,16,24,25] |
| Perceived Ease of Use (PEOU): | The extent to which elderly individuals believe that using the technology will be free from effort. In elderly healthcare, user-friendly interfaces and intuitive designs are essential for facilitating ease of use, ensuring that the technology is accessible and navigable for older users. | [14,15,16,24,25] |
| Attitude Toward Using (ATU): | Elderly individuals’ overall evaluation or feeling about using a specific technology in the context of healthcare. Positive attitudes toward using technology are likely to enhance acceptance and adoption among the elderly. | [1,5,7,16,25,26,27,28,29,30] |
| Behavioral Intention to Use (BI): | The elderly individuals’ expressed willingness to use a particular technology in the future. Behavioral intention reflects their readiness to adopt the technology for managing their healthcare needs. | [7,25,27,31] |
| Subjective Norms (SN): | The perceived social pressure or influence from significant others (family, friends, healthcare providers) regarding the use of technology in healthcare by the elderly. Positive subjective norms can contribute to increased acceptance. | [8,32,33] |
| Image (IM): | The perceived image or reputation associated with using a specific technology. In elderly healthcare, a positive image may involve perceptions of the technology as reliable, secure, and beneficial for health and well-being. | [8,15,30,32,34,35] |
| Facilitating Conditions (FC): | The degree to which elderly individuals believe that the external conditions support the use of technology in healthcare. This could include factors such as the availability of technical support, training, or access to necessary resources. | [7,8,36] |
| ChatGPT’s Responses | Previous Studies * | |
|---|---|---|
| Adoption of Telehealth Technologies: | TAM can be employed to assess how elderly individuals perceive and accept telehealth technologies for remote consultations, monitoring, and virtual care. | [24,28,34,37,38,39,40,41,42,43,44] |
| Wearable Health Devices: | TAM can help understand the factors influencing the adoption of wearable health devices among the elderly, including smartwatches or fitness trackers that monitor vital signs and activity levels. | [28,45,46] |
| Mobile Health Applications: | Evaluating the acceptance of mobile health applications tailored for elderly users, considering factors like user-friendliness, perceived usefulness, and ease of navigation. | [4,5,15,19,24,28,47,48] |
| Health Information Systems: | TAM can be applied to assess the acceptance of electronic health records, online health portals, and other health information systems by elderly individuals. | [44,49] |
| Assistive Technologies: | Understanding how elderly individuals perceive and adopt assistive technologies, such as smart home devices, medication reminders, and other aids designed to enhance independent living. | [5,21,26,36,50] |
| Virtual Reality and Gamification for Rehabilitation: | Exploring the acceptance of virtual reality and gamified applications for rehabilitation purposes, considering factors like engagement, perceived benefits, and ease of use. | [34,36,40,50,51,52,53,54,55] |
| Health Chatbots and AI-Assisted Healthcare: | Assessing the elderly’s acceptance of AI-driven healthcare support, including health-related chatbots or virtual assistants, leveraging TAM to understand factors affecting adoption. | [39,56] |
| Social Connectedness Technologies: | Investigating the acceptance of technologies aimed at fostering social connectedness among elderly individuals, such as video calling applications or social networking platforms. | [2,24,33,57,58,59] |
| Educational Health Platforms: | Evaluating the adoption of online platforms providing health education and information tailored for the elderly population. | [1,10,60,61,62] |
| Pervasive Health Monitoring Systems: | TAM can be utilized to understand how elderly individuals perceive continuous health monitoring systems, including sensors and IoT devices, in their homes or healthcare facilities. | [9,31,32,37,39,63] |
| ChatGPT’s Responses | Previous Studies * | |
|---|---|---|
| Technological Literacy Barriers: | ChatGPT highlights challenges related to the limited technological literacy among the elderly. Issues such as unfamiliarity with digital interfaces, apprehension toward new technologies, and a lack of confidence in using electronic devices may impede the acceptance of healthcare technologies. | [1,3,6,19,25,45,46,58,64,65] |
| Digital Divide Concerns: | ChatGPT acknowledges the existence of a digital divide, where disparities in access to and proficiency in technology may disproportionately affect certain segments of the elderly population. Economic, educational, and cultural factors contribute to this divide, hindering equal opportunities for technology adoption | [18,66,67] |
| Privacy and Security Apprehensions: | Privacy and security concerns are identified as significant barriers. Elderly individuals may harbor reservations about the confidentiality of their health information when using digital platforms, leading to hesitancy in embracing healthcare technologies. | [8,15,24,35] |
| Resistance to Change: | ChatGPT recognizes that resistance to change, often rooted in established routines and a preference for traditional healthcare practices, poses a substantial challenge. Elderly individuals may resist adopting new technologies due to a perceived disruption to their familiar healthcare routines. | [8,68] |
| Limited Awareness and Information: | The model points out the challenge of limited awareness and information among the elderly regarding available healthcare technologies. Insufficient knowledge about the benefits and functionalities of digital healthcare solutions may result in a lack of interest or motivation to adopt these technologies | [11,49] |
| Health Conditions and Cognitive Impairment: | ChatGPT acknowledges that health conditions and cognitive impairment can be substantial challenges. Elderly individuals facing these issues may find it difficult to engage with or comprehend certain healthcare technologies, affecting their ability to adopt and utilize these tools effectively. | [6,18,21,69] |
| Trust and Reliability Concerns: | The model emphasizes trust and reliability concerns as critical challenges. Elderly users may hesitate to adopt healthcare technologies if they perceive them as unreliable or if there are doubts about the trustworthiness of the technology providers. | [8,27,30,70,71] |
| Lack of Tailored Interventions: | ChatGPT underscores the need for tailored interventions that specifically address the unique needs and preferences of the elderly. The absence of personalized approaches in the design and implementation of healthcare technologies may hinder acceptance. | [43,71,72,73,74] |
| Overcoming Age Stereotypes: | The model recognizes the challenge of overcoming age-related stereotypes that assume older individuals are less receptive to technological advancements. Addressing these stereotypes is crucial for promoting a more inclusive approach to technology acceptance among the elderly. | [7,15,26,71,75] |
| Integration with Traditional Healthcare: | ChatGPT suggests that integrating new technologies with traditional healthcare practices poses a challenge. Ensuring seamless compatibility, acceptance by healthcare professionals, and alignment with existing healthcare systems requires careful planning and implementation. | [1,8,76,77,78,79,80] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, S.D. Application and Challenges of the Technology Acceptance Model in Elderly Healthcare: Insights from ChatGPT. Technologies 2024, 12, 68. https://doi.org/10.3390/technologies12050068
Kim SD. Application and Challenges of the Technology Acceptance Model in Elderly Healthcare: Insights from ChatGPT. Technologies. 2024; 12(5):68. https://doi.org/10.3390/technologies12050068
Chicago/Turabian StyleKim, Sang Dol. 2024. "Application and Challenges of the Technology Acceptance Model in Elderly Healthcare: Insights from ChatGPT" Technologies 12, no. 5: 68. https://doi.org/10.3390/technologies12050068
APA StyleKim, S. D. (2024). Application and Challenges of the Technology Acceptance Model in Elderly Healthcare: Insights from ChatGPT. Technologies, 12(5), 68. https://doi.org/10.3390/technologies12050068






