Revisiting the Food- and Nutrition-Related Curriculum in Healthcare Education: An Example for Pharmacy Education
Abstract
1. Introduction
2. Methods
2.1. Study Design and Setting
2.2. Data Collection
2.3. Analysis
3. Results
3.1. Origin of the Cases
3.2. Case Subjects
3.3. Ability of Pharmacy Interns to Discuss Nutritional Cases
3.4. Looking Up Additional Information
4. Discussion
4.1. Study Setting in Belgium
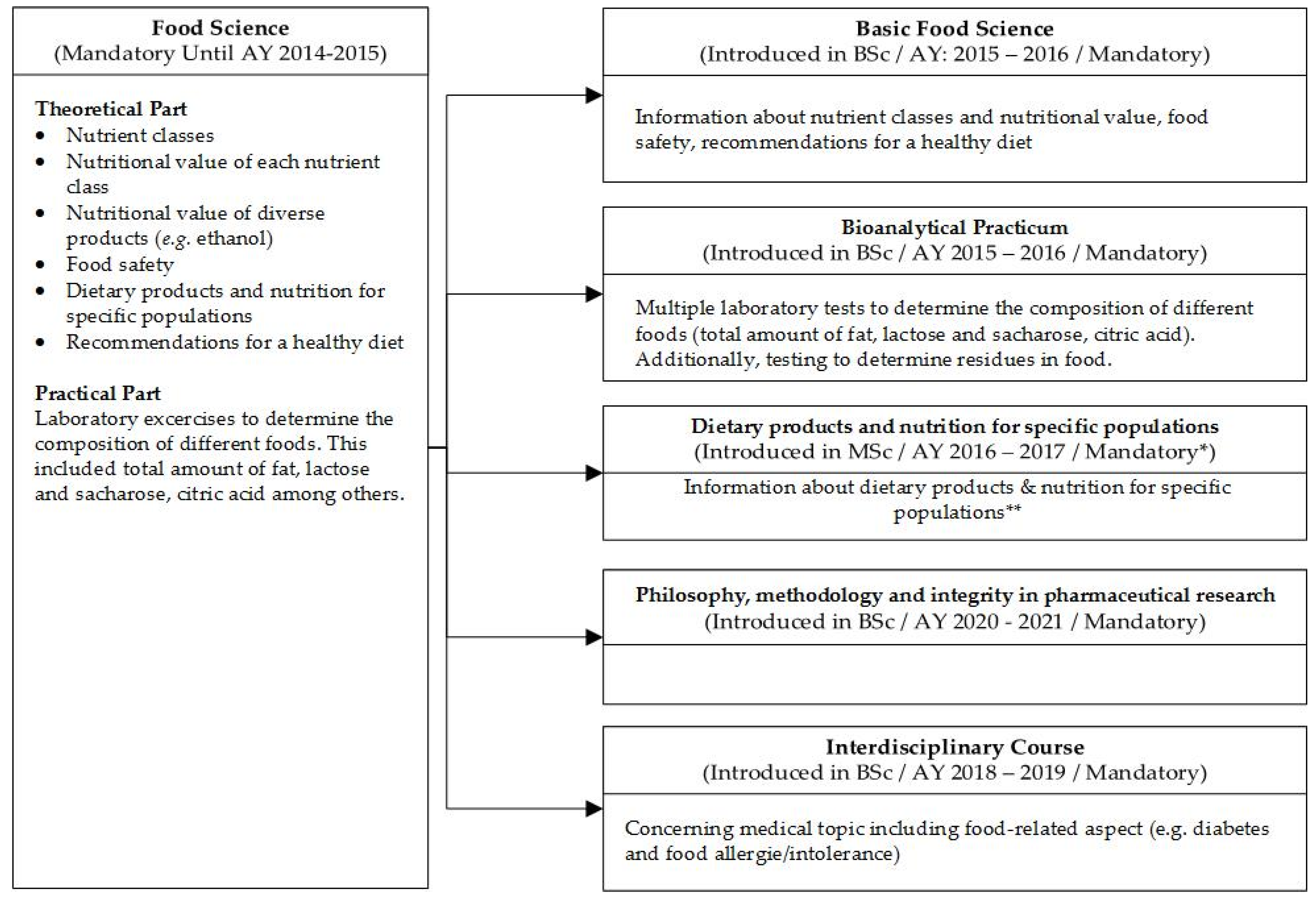
4.2. How Is Food Science Taught in Health Education?
4.3. What Does This Study Add?
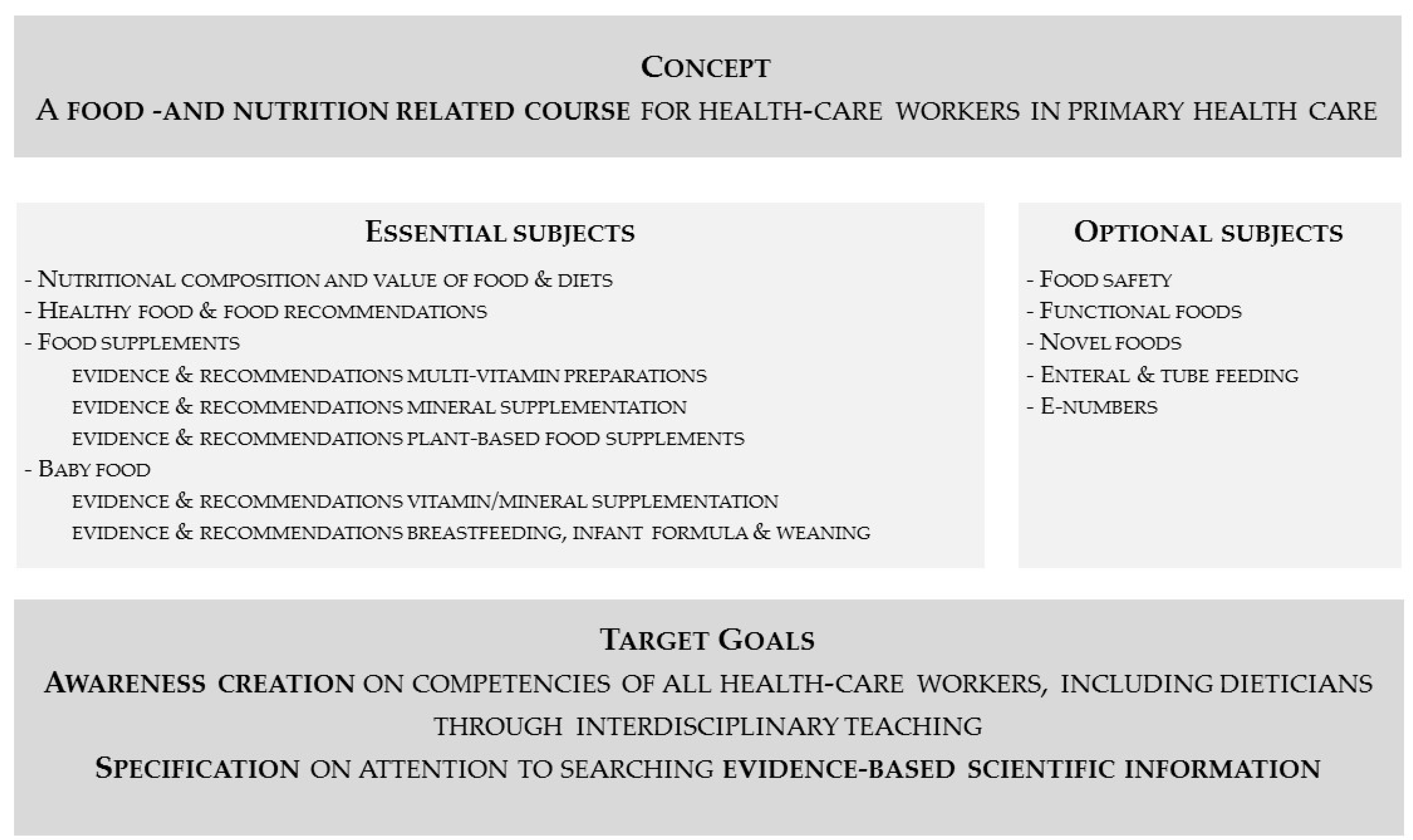
5. Specific Recommendations for Health Education
Strengths and Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Ramachandran, D.; Kite, J.; Vassallo, A.J.; Chau, J.Y.; Partridge, S.; Freeman, B.; Gill, T. Food trends and popular nutrition advice online—implications for public health. Online J. Public Health Inform. 2018, 10, e213. [Google Scholar] [CrossRef] [PubMed]
- Ventura, V.; Cavaliere, A.; Ianno, B. #socialfood: Virtuous or vicious? A systematic review. Trends Food Sci. Technol. 2021, 110, 674–686. [Google Scholar]
- Pilar, L.; Stanislavska, L.K.; Kvasnicka, R. Healthy food on the twitter social network: Vegan, homemade, and organic food. Int. J. Environ. Res. Public Health 2021, 18, 3815. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Celemín, L.; Jung, A. What should be the role of the media in nutrition communication? Br. J. Nutr. 2006, 96 (Suppl. 1), S86–S88. [Google Scholar] [CrossRef]
- Eskola, M.; Elliott, C.T.; Hajslova, J.; Steiner, D.; Krska, R. Towards a dietary-exposome assessment of chemicals in food: An update on the chronic health risks for the european consumer. Crit. Rev. Food Sci. Nutr. 2020, 60, 21. [Google Scholar] [CrossRef] [PubMed]
- Piepoli, M.F.; Hoes, A.W.; Agewall, S.; Albus, C.; Brotons, C.; Catapano, A.L.; Cooney, M.-T.; Corrà, U.; Cosyns, B.; Deaton, C.; et al. 2016 european guidelines on cardiovascular disease prevention in clinical practice: The sixth joint task force of the european society of cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of 10 societies and by invited experts) developed with the special contribution of the european association for cardiovascular prevention & rehabilitation (eacpr). Eur. Heart J. 2016, 37, 2315–2381. [Google Scholar] [PubMed]
- American Diabetes Association. 3. Prevention or delay of type 2 diabetes: Standards of medical care in diabetes—2019. Diabetes Care 2019, 42, S29–S33. [Google Scholar] [CrossRef] [PubMed]
- Marcus, C. Strategies for improving the quality of verbal patient and family education: A review of the literature and creation of the educate model. Health Psychol. Behav. Med. 2014, 2, 482–495. [Google Scholar] [CrossRef] [PubMed]
- Vermeir, P.; Vandijck, D.; Degroote, S.; Peleman, R.; Verhaeghe, R.; Mortier, E.; Hallaert, G.; Van Daele, S.; Buylaert, W.; Vogelaers, D. Communication in healthcare: A narrative review of the literature and practical recommendations. Int. J. Clin. Pract. 2015, 69, 1257–1267. [Google Scholar] [CrossRef] [PubMed]
- Charuel, A.; Prevost, V. Conseils nutritionnels à l’officine dans le cadre du programme national nutrition santé. Ann. Pharm. Française 2014, 72, 337–347. [Google Scholar] [CrossRef] [PubMed]
- Douglas, P.L.; McCarthy, H.; McCotter, L.E.; Gallen, S.; McClean, S.; Gallagher, A.M.; Ray, S. Nutrition education and community pharmacy: A first exploration of current attitudes and practices in northern ireland. Pharmacy 2019, 7, 27. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-Llimos, F. The pharmacist guide to implementing pharmaceutical care. Pharm. Pract. Internet 2018, 16. [Google Scholar] [CrossRef]
- Riziv. Available online: https://www.riziv.fgov.be/nl/themas/kost-terugbetaling/verzekerbaarheid/Paginas/aansluiten-ziekenfonds.aspx (accessed on 9 May 2019).
- Available online: https://www.riziv.fgov.be/ (accessed on 9 May 2019).
- University of Bonn. Available online: https://www.uni-bonn.de/studying/vor-dem-studium/courses/pharmazie-en (accessed on 9 May 2019).
- Philipps-Universität Marburg. Available online: https://www.uni-marburg.de/en/studying/degree-programs/sciences/pharmacyse (accessed on 9 May 2019).
- University of Montpellier. Available online: https://pharmacie.edu.umontpellier.fr/ (accessed on 9 May 2019).
- University of Lille. Available online: https://www.univ-lille.fr/home/courses/joint-programmes/ (accessed on 9 May 2019).
- University of Utrecht. Available online: https://www.uu.nl/en/organisation/faculty-of-science/about-us/organisation/schools/school-of-pharmacy (accessed on 9 May 2019).
- University of Groningen. Available online: https://www.rug.nl/bachelors/pharmacy/?lang=en&gclid=EAIaIQobChMIq4Tyitfo6wIVFud3Ch1pnw3iEAAYASAAEgKkavD_BwE (accessed on 9 May 2019).
- University of Greenwich. Available online: https://www.gre.ac.uk/subjects/pharmacy (accessed on 9 May 2019).
- University College London. Available online: https://www.ucl.ac.uk/pharmacy/study (accessed on 9 May 2019).
- Eshelman School of Pharmacy. Available online: https://pharmacy.unc.edu/education/pharmd/curriculum/ (accessed on 9 May 2019).
- University of Minnesota. Available online: https://www.pharmacy.umn.edu/degrees-and-programs/doctor-pharmacy/curriculum/elective-courses (accessed on 9 May 2019).
- Axon, D.R.; Vanova, J.; Edel, C.; Slack, M. Dietary supplement use, knowledge, and perceptions among student pharmacists. Am. J. Pharm. Educ. 2017, 81, 92. [Google Scholar] [CrossRef] [PubMed]
- Scaletta, A.; Ghelani, N.; Sunny, S. Complementary and alternative medicine education in U.S. Schools and colleges of pharmacy. Curr. Pharm. Teach. Learn. 2017, 9, 521–527. [Google Scholar] [CrossRef] [PubMed]
- Pokladnikova, J.; Lie, D. Comparison of attitudes, beliefs, and resource-seeking behavior for cam among first- and third-year czech pharmacy students. Am. J. Pharm. Educ. 2008, 72. [Google Scholar] [CrossRef] [PubMed]
- James, P.B.; Bah, A.J. Awareness, use, attitude and perceived need for complementary and alternative medicine (cam) education among undergraduate pharmacy students in sierra leone: A descriptive cross-sectional survey. BMC Complement. Altern. Med. 2014, 14. [Google Scholar] [CrossRef] [PubMed]
- BMJ Publishing Group—BMJ Best Practice. Available online: https://bestpractice.bmj.com (accessed on 9 May 2019).
- Up To Date. Available online: https://www.uptodate.com (accessed on 9 May 2019).
- Cochrane Library. Available online: https://www.cochranelibrary.com/ (accessed on 9 May 2019).
- Moreira, N.C.F.; Krausch-Hofmann, S.; Matthys, C.; Vereecken, C.; Vanhauwaert, E.; Declercq, A.; Bekkering, G.E.; Duyck, J. Risk factors for malnutrition in older adults: A systematic review of the literature based on longitudinal data. Adv. Nutr. 2016, 7, 507–522. [Google Scholar] [CrossRef] [PubMed]
| Category or Nutritional Topic | N°, (%) |
|---|---|
| Food Supplements | 379 (37.8) |
| - Multivitamin preparations | 52 |
| - Vitamin D, calcium, or combinations | 45 |
| - Preconception, pregnancy, or breastfeeding vitamins | 34 |
| - Vitamins to improve sleep, diminish fatigue, or give an energy boost | 30 |
| - Magnesium | 28 |
| - Vitamins for studying | 27 |
| - Supplements for specific indications (menopause, arthritis, diarrhea, bladder infection, etc.) | 23 |
| - Red yeast rice for hypercholesterolemia or Q10 when statin use | 22 |
| - Iron and vitamin B12 | 15 |
| - Hair and nail vitamins | 14 |
| - Omega 3, 6, or 9 | 13 |
| - Vitamin C | 7 |
| - Other | 69 |
| Baby Food | 187 (18.6) |
| - Formula for insatiety | 37 |
| - Formula for constipation, diarrhea, colic, or combinations | 27 |
| - Switching from formula to follow-on formula or growing-up milk | 26 |
| - Formula for reflux and regurgitation | 21 |
| - Formula for allergy prevention of treatment | 19 |
| - Switching from breastmilk to formula | 18 |
| - Switching from milk to solid foods | 5 |
| - Formula supplementation when insufficient milk supply | 5 |
| - Other (preparation, recommendations, etc.) | 29 |
| Healthy Food and Food/Nutritional Recommendations | 106 (10.6) |
| - Food recommendations in function of disease (constipation, heartburn, gout, diarrhea, migraine, hypertension, hypercholesterolemia, etc.) | 59 |
| - Food recommendations in function of vitamin or mineral deficiency (iron, B12, D, folic acid, etc.) | 18 |
| - Food recommendations in function of colonoscopy, bowel examination, or gastric bypass | 10 |
| - Balanced diet | 6 |
| - Food restrictions during pregnancy | 5 |
| - Other | 8 |
| Weight Loss Diets and Products | 78 (7.8) |
| - Weight-loss pills or supplements | 24 |
| - Meal replacements | 20 |
| - Specific diets (low-carb, soup diet, high protein, etc.) | 9 |
| - Light products and sugar substitutes | 3 |
| - Other | 22 |
| High-Protein Foods/Drinks | 63 (6.27) |
| - Food replacement in illness | 29 |
| - Weight gain | 12 |
| - Food supplements for the geriatric population | 11 |
| - Other | 11 |
| Food for Athletes | 48 (4.78) |
| - Supplements for endurance training | 28 |
| - Supplements for building up muscle mass | 10 |
| - Other | 10 |
| Interactions between Drugs and Food | 44 (4.38) |
| - Combination of antibiotics and dairy | 16 |
| - Combination of medication and alcohol | 8 |
| - Combination of food supplements and food | 6 |
| - Combination of medication and grapefruit | 3 |
| - Other | 11 |
| Food Allergies and Intolerances | 33 (3.29) |
| - Gluten | 6 |
| - Lactose | 5 |
| - Other (cow’s milk protein allergy, wheat allergy, etc.) | 7 |
| - Presence of allergens in drugs | 15 |
| Vegetarianism and Veganism | 16 (1.59) |
| - Vitamin or mineral deficiency | 11 |
| - Other | 5 |
| Food Safety | 11 (1.09) |
| Diabetes and Diet | 11 (1.09) |
| Food for the Geriatric Population | 9 (0.90) |
| Ingredients in Food | 8 (0.80) |
| Functional Foods/Nutraceuticals | 5 (0.50) |
| Diet for Phenylketonuria | 3 (0.30) |
| Enteral and Tube Feeding | 1 (0.10) |
| Novel Foods and Hype-Surrounding Superfoods | 1 (0.10) |
| E-Numbers | 1 (0.10) |
| Category | Number of Cases (%) | Percentage of Cases in Which the Intern Had Enough Knowledge to Discuss the Case Immediately | Percentage of Cases in Which the Intern Had Enough Knowledge to Discuss the Case after Research (%) |
|---|---|---|---|
| Food supplements | 38% (n = 379) | 49% | 96% |
| Baby food | 19% (n = 187) | 47% | 97% |
| Healthy food and food/nutritional recommendations | 11% (n = 106) | 46% | 93% |
| Weight-loss diets and products | 8% (n = 78) | 44% | 95% |
| High-protein foods/drinks | 6% (n = 63) | 47% | 95% |
| Food for athletes | 5% (n = 48) | 21% | 96% |
| Interactions between drugs and food | 4% (n = 44) | 54% | 93% |
| Food allergies and intolerances | 3% (n = 33) | 18% | 94% |
| Vegetarianism and veganism | 2% (n = 16) | 25% | 94% |
| Food safety | 1% (n = 11) | 27% | 100% |
| Diabetes and diet | 1% (n = 11) | 45% | 100% |
| Food for the geriatric population | 0.9% (n = 9) | 33% | 100% |
| Ingredients in food | 0.8% (n = 8) | 37% | 87% |
| Functional foods/Nutraceuticals | 0.5% (n = 5) | 60% | 100% |
| Diet for phenylketonuria | 0.3% (n = 3) | 0% | 100% |
| Enteral and tube feeding | 0.1% (n = 1) | 0% | 100% |
| Novel foods and hype-surrounding superfoods | 0.1% (n = 1) | 0% | 100% |
| E-numbers | 0.1% (n = 1) | 0% | 100% |
| Category | Number of Cases (%) | Category | Number of Cases (%) |
|---|---|---|---|
| No sufficient knowledge to answer immediately | 557 (55%) | Used additional sources of information | 552/557 (99%) |
| Used no additional sources of information | 5/557 (1%) | ||
| Sufficient knowledge to answer immediately | 447 (51%) | Used additional sources of information | 228/447 (51%) |
| Used no additional sources of information | 219/447 (49%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tommelein, E.; De Boevre, M.; Vanhie, L.; Van Tongelen, I.; Boussery, K.; De Saeger, S. Revisiting the Food- and Nutrition-Related Curriculum in Healthcare Education: An Example for Pharmacy Education. Pharmacy 2021, 9, 104. https://doi.org/10.3390/pharmacy9020104
Tommelein E, De Boevre M, Vanhie L, Van Tongelen I, Boussery K, De Saeger S. Revisiting the Food- and Nutrition-Related Curriculum in Healthcare Education: An Example for Pharmacy Education. Pharmacy. 2021; 9(2):104. https://doi.org/10.3390/pharmacy9020104
Chicago/Turabian StyleTommelein, Eline, Marthe De Boevre, Lize Vanhie, Inge Van Tongelen, Koen Boussery, and Sarah De Saeger. 2021. "Revisiting the Food- and Nutrition-Related Curriculum in Healthcare Education: An Example for Pharmacy Education" Pharmacy 9, no. 2: 104. https://doi.org/10.3390/pharmacy9020104
APA StyleTommelein, E., De Boevre, M., Vanhie, L., Van Tongelen, I., Boussery, K., & De Saeger, S. (2021). Revisiting the Food- and Nutrition-Related Curriculum in Healthcare Education: An Example for Pharmacy Education. Pharmacy, 9(2), 104. https://doi.org/10.3390/pharmacy9020104








