Cultural Humility: A Proposed Model for a Continuing Professional Development Program
Abstract
1. Introduction
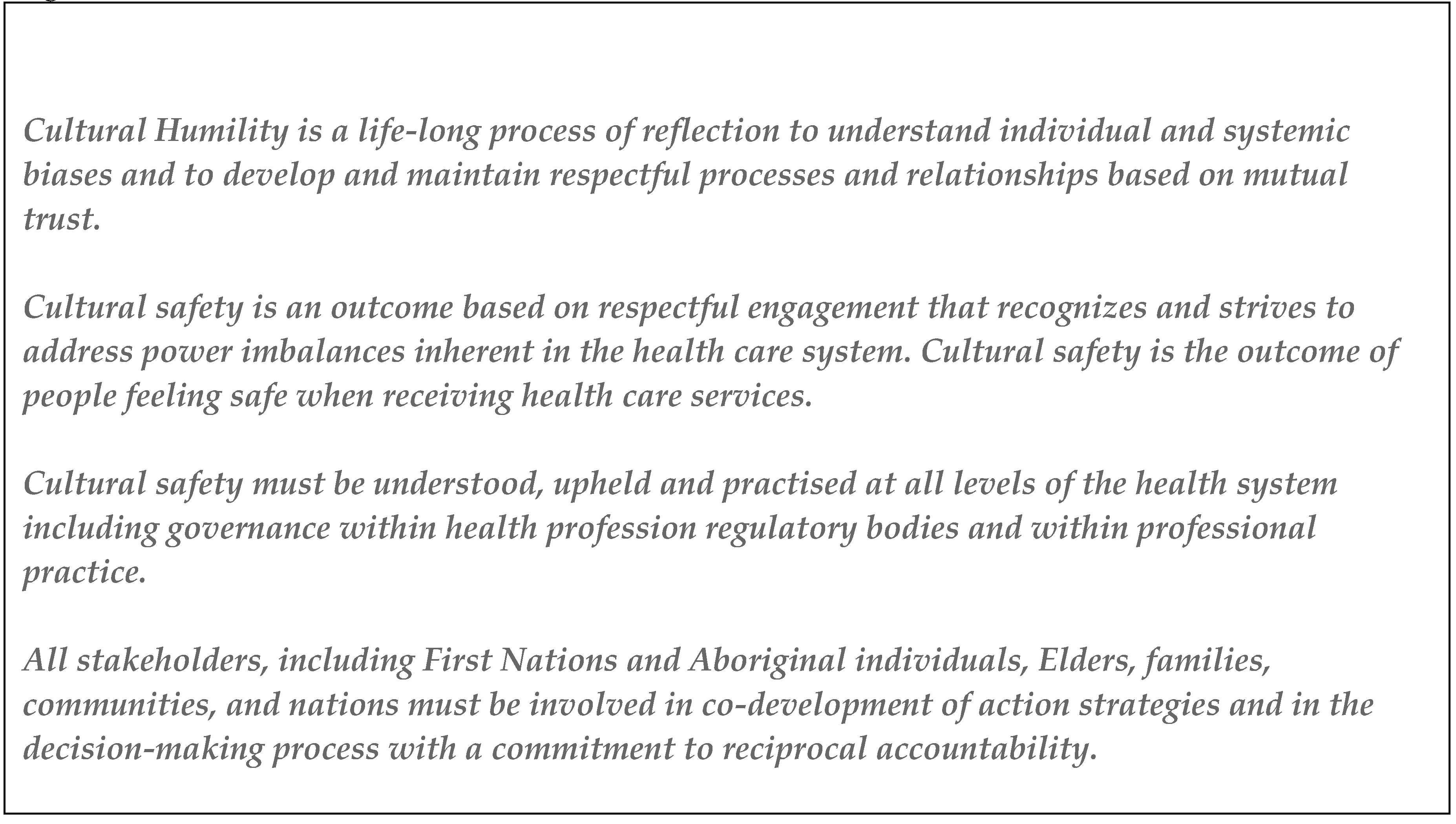
2. Cultural Competence
3. Cultural Safety
- Recognising and responding to the specific health needs of Aboriginal and Torres Strait Islander people, and other populations identified as experiencing healthcare inequity.
- Ensuring that all individuals are treated with respect and consideration of their beliefs, cultures and practices.
- Delivering healthcare equitably.
- Conducting regular review of self, co-workers and the workplace for cultural and social responsiveness.
[In Australia] Cultural safety is determined by Aboriginal and Torres Strait Islander individuals, families and communities. Culturally safe practise is the ongoing critical reflection of practitioner knowledge, skills, attitudes, practising behaviours and power differentials in delivering safe, accessible and responsive healthcare free of racism [18].
4. Cultural Humility
Cultural humility incorporates a lifelong commitment to self-evaluation and critique, to redressing the power imbalances in the physician-patient dynamic, and to developing mutually beneficial and non-paternalistic partnerships with communities on behalf of individuals and defined populations [20].
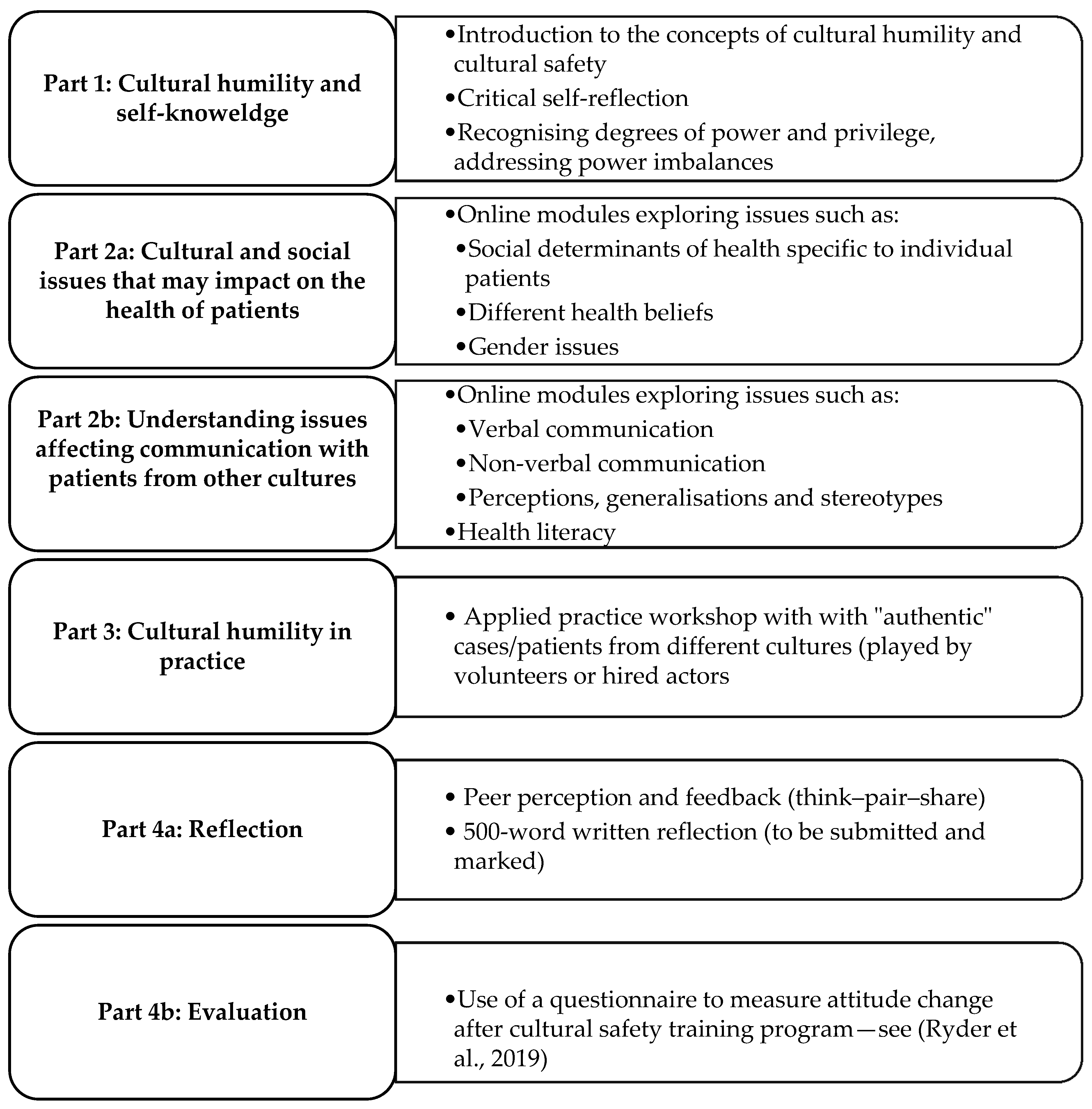
5. Cultural Humility CPD
Group 3: quality or practice—improvement facilitated (three Board CPD credits per hour of activity)
Descriptor: activities where an assessment of existing practice (as an individual or within a pharmacy practice), and the needs for, and barriers to changes in this practice, is carried out before the development of a particular activity. As a result, the activity addresses identified continuing professional development needs with a reflection post-activity to evaluate practice change or outcomes resulting from the activity. Such an activity most likely will extend over a number of weeks or months [43].
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Curtis, E.; Jones, R.; Tipene-Leach, D.; Walker, C.; Loring, B.; Paine, S.J.; Reid, P. Why cultural safety rather than cultural competency is required to achieve health equity: A literature review and recommended definition. Int. J. Equity Health 2019, 18, 174. [Google Scholar] [CrossRef] [PubMed]
- Laverty, M.; McDermott, D.R.; Calma, T. Embedding cultural safety in Australia’s main health care standards. Med. J. Aust. 2017, 207, 15–16. [Google Scholar] [CrossRef] [PubMed]
- Worldometer. Australia Population. Available online: https://www.worldometers.info/world-population/australia-population/ (accessed on 10 October 2020).
- Department of Home Affairs. Multicultural Australia: United, Strong, Successful. Australian Government: 2020. Available online: https://www.homeaffairs.gov.au/mca/Statements/english-multicultural-statement.pdf (accessed on 8 October 2020).
- Australian Bureau of Statistics. Cultural Diversity in Australia. Available online: http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/by%20Subject/2071.0~2016~Main%20Features~Cultural%20Diversity%20Article~20?OpenDocument&ref=story (accessed on 12 October 2020).
- International Work Groups for Indigenous Affairs. Indigenous People’s in Australia. Available online: https://www.iwgia.org/en/australia/3642-iw-2020-australia.html (accessed on 12 October 2020).
- College of Pharmacists of British Columbia. Commitment to Cultural Safety and Humility. Available online: https://www.bcpharmacists.org/humility (accessed on 28 September 2020).
- World Health Organisation. Human Rights and Health. Available online: https://www.who.int/news-room/fact-sheets/detail/human-rights-and-health (accessed on 10 October 2020).
- Etchason, J.; Armour, B.; Ofili, E.; Rust, G.; Mayberry, R.; Sanders, L.; Pitts, M.M. Racial and ethnic disparities in health care. JAMA 2001, 285, 883. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Clarke, A.; Goddu, A.; Nocon, R.; Stock, N.; Chyr, L.; Akuoko, J.; Chin, M. Thirty years of disparities intervention research: What are we doing to close racial and ethnic gaps in health care? Med. Care 2013, 51, 1020–1026. [Google Scholar] [CrossRef]
- Leach, M.J.; Gillam, M.; Gonzalez-Chica, D.A.; Walsh, S.; Muyambi, K.; Jones, M. Health care need and health disparities: Findings from the Regional South Australia Health (RESONATE) survey. Health Soc. Care Community 2020. [Google Scholar] [CrossRef]
- Durie, M. (Ed.) Cultural Competence and Medical Practice in New Zealand. In Proceedings of the Australian and New Zealand Boards and Council Conference, Wellington, New Zealand, 21 November 2001. [Google Scholar]
- Jowsey, T. Three zones of cultural competency: Surface competency, bias twilight, and the confronting midnight zone. BMC Med. Educ. 2019, 19, 306. [Google Scholar] [CrossRef]
- Fisher-Borne, M.; Cain, J.M.; Martin, S.L. From mastery to accountability: Cultural humility as an alternative to cultural competence. Soc. Work Educ. 2014, 34, 1–17. [Google Scholar] [CrossRef]
- Tascon, S.; Gatwiri, K. Towards cultural humility: Theorising cultural competence as institutionalised whiteness. Soc. Work Policy Stud. Soc. Justice Pract. Theory 2020, 3, 1–16. [Google Scholar]
- Pharmaceutical Society of Australia. Professional Practice Standards; Pharmaceutical Society of Australia: Canberra, Australia, 2019. [Google Scholar]
- Browne, A.J.; Varcoe, C.; Smye, V.; Reimer-Kirkham, S.; Lynam, M.J.; Wong, S. Cultural safety and the challenges of translating critically oriented knowledge in practice. Nurs. Philos. 2009, 10, 167–179. [Google Scholar] [CrossRef]
- Australian Health Practitioner Regulation Agency. National Scheme’s Aboriginal and Torres Strait Islander Health and Cultural Safety Strategy 2020–2025; Australian Health Practitioner Regulation Agency: Canberra, Australia, 2018. [Google Scholar]
- Unite for Sight. Cultural Differences and Cultural Understanding. Available online: http://www.uniteforsight.org/cultural-competency/module7 (accessed on 10 October 2020).
- Tervalon, M.; Murray-García, J. Cultural humility versus cultural competence: A critical distinction in defining physician training outcomes in multicultural education. J. Health Care Poor Underserved 1998, 9, 117–125. [Google Scholar] [CrossRef]
- Foronda, C. A theory of cultural humility. J. Transcult. Nurs. 2019, 31, 7–12. [Google Scholar] [CrossRef] [PubMed]
- Chang, E.; Simon, M.; Dong, X. Integrating cultural humility into health care professional education and training. Adv. Health Sci. Educ. 2012, 17, 269–278. [Google Scholar] [CrossRef] [PubMed]
- Pharmaceutical Society of Australia. National Competency Standards Framework for Pharmacists in Australia; Pharmaceutical Society of Australia: Canberra, Australia, 2016. [Google Scholar]
- Pérez, M.A. Cultural Competence in Health Education and Health Promotion, 2nd ed.; Wiley: Hoboken, NJ, USA, 2013. [Google Scholar]
- Weller, S.C.; Pachter, L.M.; Trotter, R.T.; Baer, R.D.; Klein, R.E.; Garcia de Alba Garcia, J.E.; Glazer, M.; Castillo, Z. Empacho in four Latino groups: A study of intra- and inter-cultural variation in beliefs. Med. Anthropol. 1993, 15, 109–136. [Google Scholar] [CrossRef] [PubMed]
- Minnican, C.; O’Toole, G. Exploring the incidence of culturally responsive communication in Australian healthcare: The first rapid review on this concept. BMC Health Serv. Res. 2020, 20, 20. [Google Scholar] [CrossRef] [PubMed]
- Wittink, H.; Oosterhaven, J. Patient education and health literacy. Musculoskelet. Sci. Pract. 2018, 38, 120–127. [Google Scholar] [CrossRef]
- Villaire, M.; Mayer, G. Low health literacy: The impact on chronic illness management. Prof. Case Manag. 2007, 12, 213–218. [Google Scholar] [CrossRef]
- Alpers, L.M. Distrust and patients in intercultural healthcare: A qualitative interview study. Nurs. Ethics 2018, 25, 313–323. [Google Scholar] [CrossRef]
- Mackert, M.; Ball, J.; Lopez, N. Health literacy awareness training for healthcare workers: Improving knowledge and intentions to use clear communication techniques. Patient Educ. Couns. 2011, 85, e225–e228. [Google Scholar] [CrossRef]
- Markova, T. Effective communication and delivery of culturally competent health care. Urol. Nurs. 2007, 27, 239–242. [Google Scholar]
- Thompson, W.; Nissen, L.M.; Hayward, K. Clinical pharmacy: Pharmacists’ understanding of their CPD obligations. Aust. J. Pharm. 2013, 94, 58–60. [Google Scholar]
- Fleming, T.; Creedy, D.K.; West, R. The influence of yarning circles: A cultural safety professional development program for midwives. Women Birth 2019, 33, 175–185. [Google Scholar] [CrossRef] [PubMed]
- Van Hoof, T.; Meehan, T. Integrating essential components of quality improvement into a new paradigm for continuing education. J. Contin. Educ. Health Prof. 2017, 37, 274–280. [Google Scholar] [CrossRef] [PubMed]
- Continuing education meetings and workshops: Effects on professional practice and health care outcomes (Cochrane review). J. Contin. Educ. Health Prof. 2001, 21, 187–188. [CrossRef]
- Kane, G.M. Interactive learning in continuing professional development: At least 25 per cent of time. Ann. R Coll Physicians Surg. Can. 2000, 33, 526. [Google Scholar]
- Rhodes, C.M. Culturally responsive teaching with adult learners: A review of the literature. Int. J. Adult Vocat. Educ. Technol. 2018, 9, 33–41. [Google Scholar] [CrossRef]
- Velott, D.; Sprow Forté, K. Toward health equity: Mindfulness and cultural humility as adult education: Toward health equity. New Dir. Adult Contin. Educ. 2019, 2019, 57–66. [Google Scholar] [CrossRef]
- Jones, J.; Bion, J.; Brown, C.; Willars, J.; Brookes, O.; Tarrant, C. Reflection in practice: How can patient experience feedback trigger staff reflection in hospital acute care settings? Health Expect. 2019, 23, 396–404. [Google Scholar] [CrossRef]
- Marshall, S.J.; Biddle, S.J.H. The transtheoretical model of behavior change: A meta-analysis of applications to physical activity and exercise. Ann. Behav. Med. 2001, 23, 229–246. [Google Scholar] [CrossRef]
- Gregory, H.; Van Orden, O.; Jordan, L.; Portnoy, G.A.; Welsh, E.; Betkowski, J.; Charles, J.W.; Diclemente, C.C. New directions in capacity building: Incorporating cultural competence into the interactive systems framework. Am. J. Community Psychol. 2012, 50, 321–333. [Google Scholar] [CrossRef]
- Moon, J. Using reflective learning to improve the impact of short courses and workshops. J. Contin. Educ. Health Prof. 2004, 24, 4–11. [Google Scholar] [CrossRef]
- Pharmacy Board of Australia. Continuing Professional Development for Pharmacists and Pharmacy Interns: Frequently Asked Questions; Pharmacy Board of Australia: Canberra, Australia, 2015. [Google Scholar]
| Stage | Stage Characteristics |
|---|---|
| Precontemplation | Not thinking about change; satisfied with status-quo. |
| Contemplation | Thinking about change, but not yet sure. |
| Preparation | Would like to change; may be planning and trying out changes |
| Action | Beginning to change. Specific, overt behavioural modifications have been made. Observable changes take place. |
| Maintenance | Have successfully implemented change. Consolidation of the behaviours initiated during the action stage. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cox, J.L.; Simpson, M.D. Cultural Humility: A Proposed Model for a Continuing Professional Development Program. Pharmacy 2020, 8, 214. https://doi.org/10.3390/pharmacy8040214
Cox JL, Simpson MD. Cultural Humility: A Proposed Model for a Continuing Professional Development Program. Pharmacy. 2020; 8(4):214. https://doi.org/10.3390/pharmacy8040214
Chicago/Turabian StyleCox, Jennifer L., and Maree Donna Simpson. 2020. "Cultural Humility: A Proposed Model for a Continuing Professional Development Program" Pharmacy 8, no. 4: 214. https://doi.org/10.3390/pharmacy8040214
APA StyleCox, J. L., & Simpson, M. D. (2020). Cultural Humility: A Proposed Model for a Continuing Professional Development Program. Pharmacy, 8(4), 214. https://doi.org/10.3390/pharmacy8040214






