Extended Access to Hormonal Contraception in Pharmacies: A Survey among Swiss Pharmacists
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Participants
3.2. Current Practice
3.3. Pharmacists’ Interest in Providing Hormonal Contraception Service
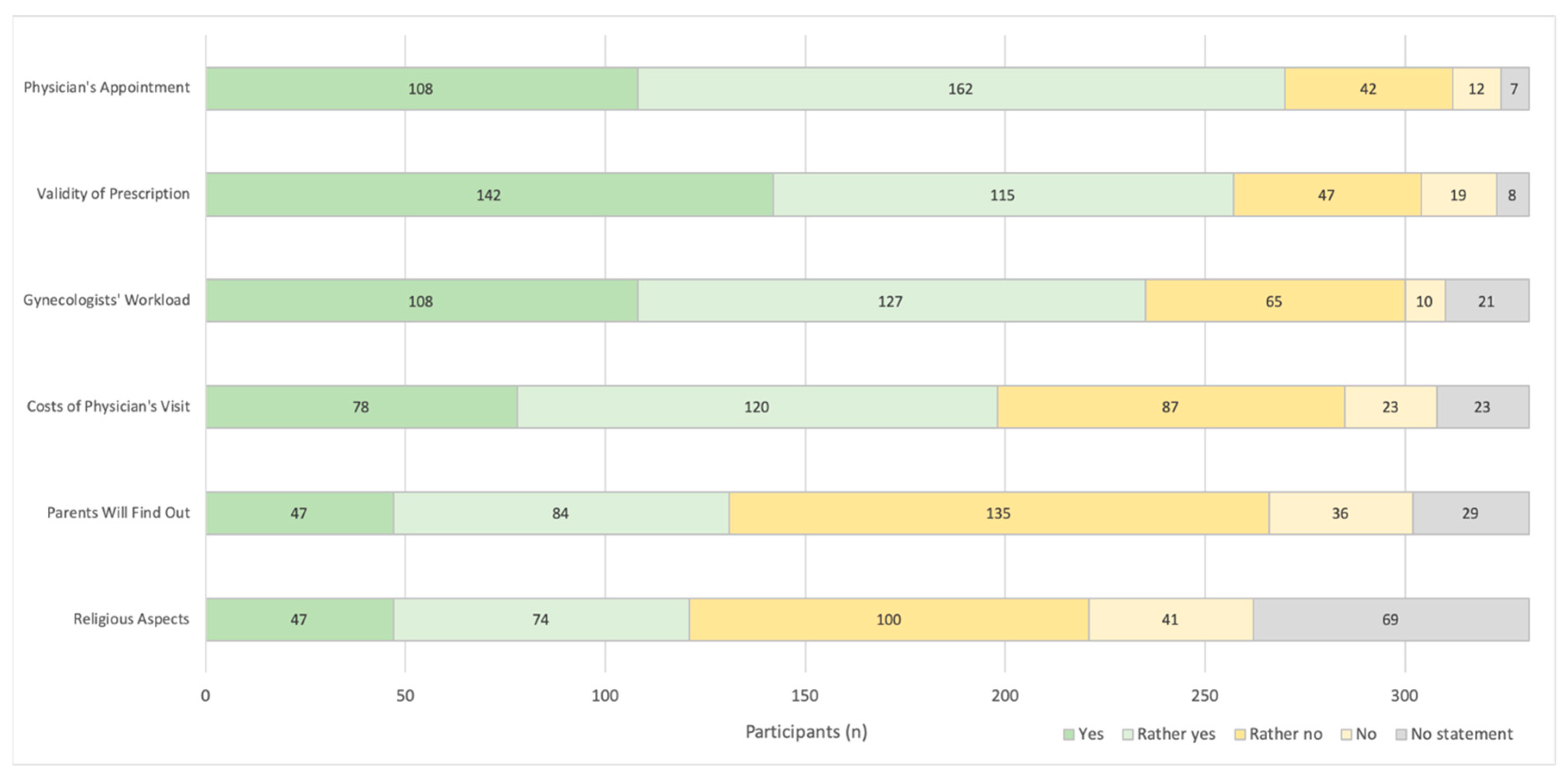
3.4. Potential Barriers to Access Hormonal Contraception
3.5. Extended Access to Hormonal Contraception
3.5.1. Different Models and Inter-Professional Collaboration
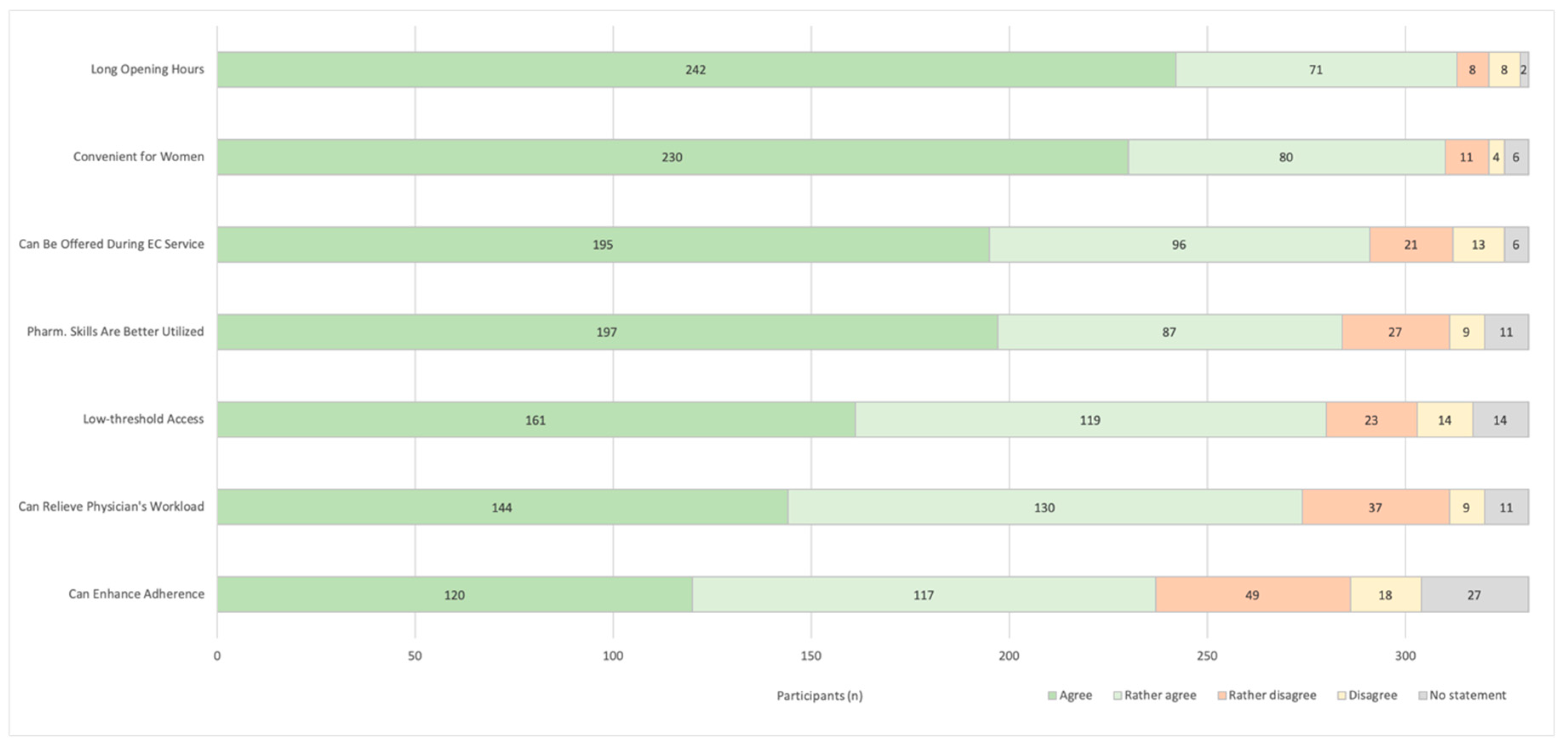
3.5.2. Advantages of Pharmacy Access
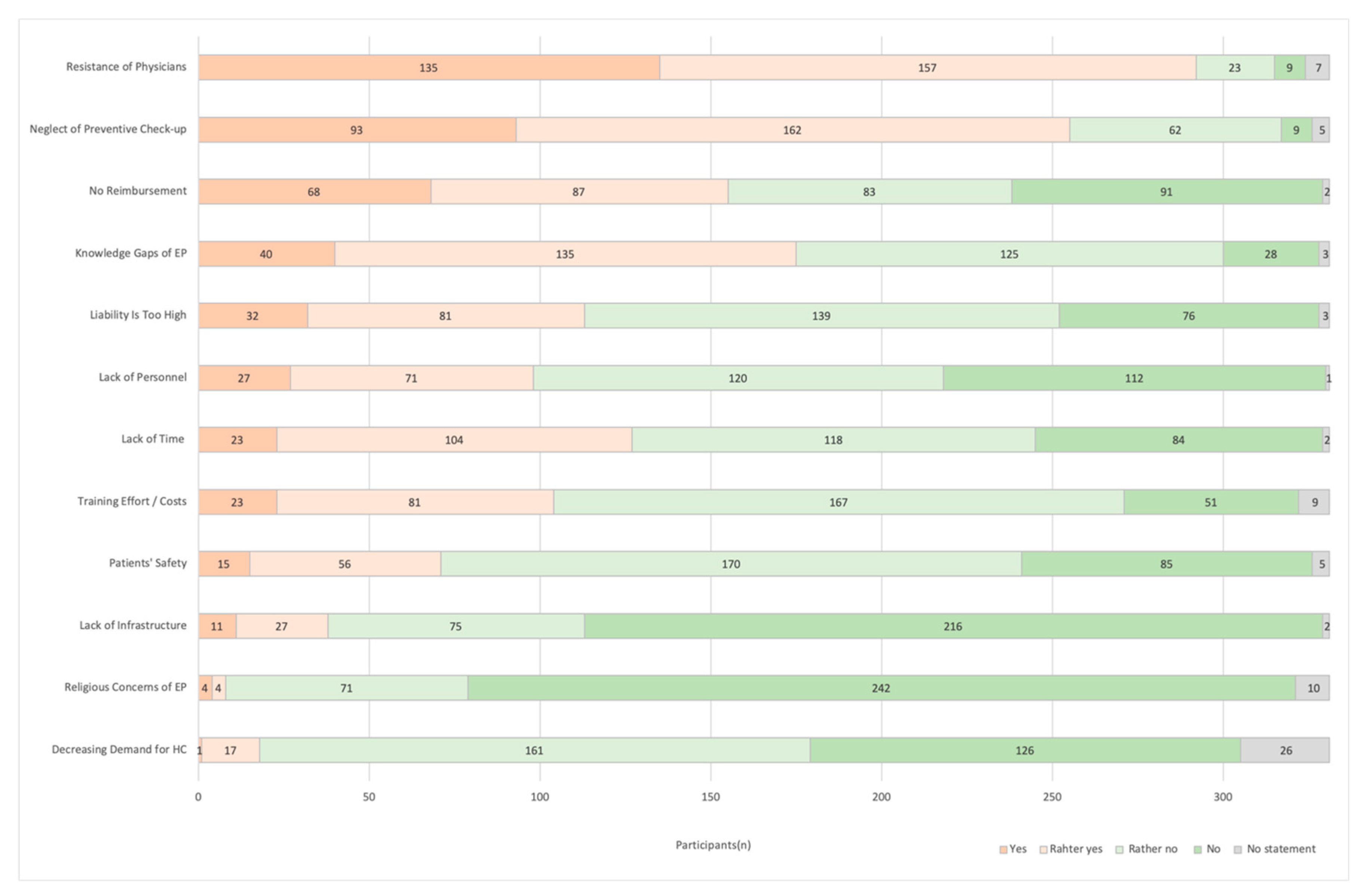
3.5.3. Pharmacist’s Concerns
3.5.4. Patients’ Safety
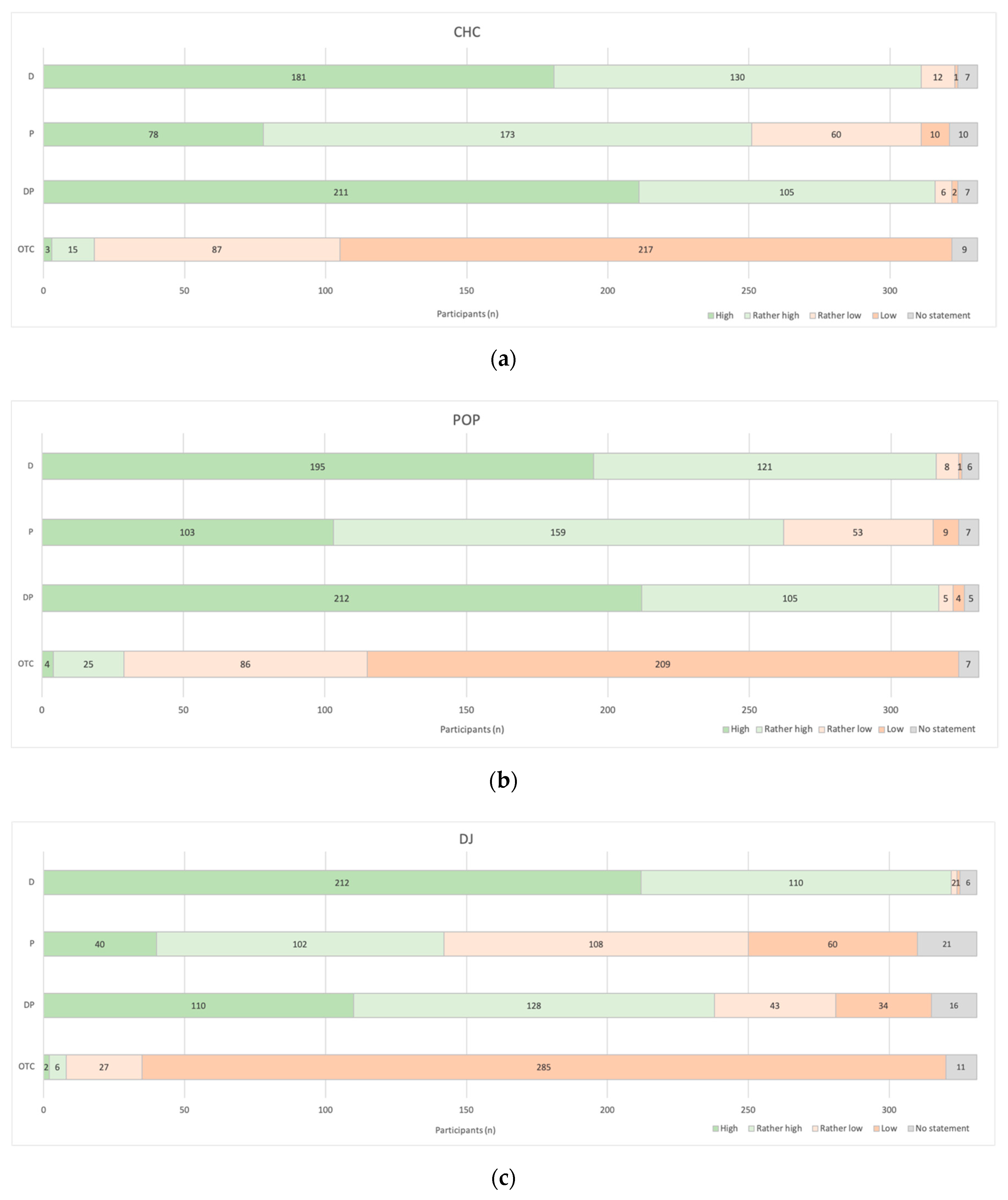
3.6. Knowledge and Skills
4. Discussion
4.1. Interpretation
4.2. Strengths and Limitations
4.3. Open Question and Further Research
4.4. Relevance of these Findings
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Christin-Maitre, S. History of oral contraceptive drugs and their use worldwide. Best Pract. Res. Clin. Endocrinol. Metab. 2013, 27, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Moffat, R.; Sartorius, G.; Raggi, A.; Draths, R.; Bitzer, J. Evidenzbasierte Kontrazeptionsberatung. Swiss Med. Forum 2019, 19, 286–291. [Google Scholar] [CrossRef]
- The American College of Obstetricians and Gynecologists (ACOG). Commitee Opinion: Over-the-Counter Access to Hormonal Contraception. Obstet. Gynecol. 2019, 134, e96–e105. [Google Scholar] [CrossRef] [PubMed]
- European Medicines Agency (EMA). Combined Hormonal Contraceptives. Available online: https://www.ema.europa.eu/en/human-regulatory/post-authorisation/referral-procedures/combined-hormonal-contraceptives (accessed on 27 April 2020).
- World Health Organization (WHO). Selected Practice Recommendations for Contraceptive Use, 3rd ed.; Reproductive Health and Research; WHO: Geneva, Switzerland, 2016; ISBN 978-92-4-156540-0. [Google Scholar]
- Grossman, D. Over-the-Counter Access to Oral Contraceptives. Obstet. Gynecol. Clin. N. Am. 2015, 42, 619–629. [Google Scholar] [CrossRef] [PubMed]
- Rafie, S.; Richards, E.; Rafie, S.; Landau, S.; Wilkinson, T. Pharmacist Outlooks on Prescribing Hormonal Contraception Following Statewide Scope of Practice Expansion. Pharmacy 2019, 7, 96. [Google Scholar] [CrossRef] [PubMed]
- Grindlay, K.; Burns, B.; Grossman, D. Prescription requirements and over-the-counter access to oral contraceptives: A global review. Contraception 2013, 88, 91–96. [Google Scholar] [CrossRef] [PubMed]
- New Zealand Medicines and Medical Devices Safety Authority Medicines Classification—Oral Contraception Recommendation Made. Available online: www.medsafe.govt.nz (accessed on 2 July 2020).
- Gumbie, M.; Parkinson, B.; Cutler, H.; Gauld, N.; Mumford, V. Is Reclassification of the Oral Contraceptive Pill from Prescription to Pharmacist-Only Cost Effective? Application of an Economic Evaluation Approach to Regulatory Decisions. PharmacoEconomics 2019, 37, 1049–1064. [Google Scholar] [CrossRef]
- Nieuwinckel, S.; Cornwell, S.; De Meyer, G.R.Y.; De Loof, H. Hormonal contraception without a prescription: Opinions of pharmacists, general practitioners and gynaecologists in Flanders, Belgium. Eur. J. Contracept. Reprod. Health Care 2019, 24, 85–96. [Google Scholar] [CrossRef]
- Parsons, J.; Adams, C.; Aziz, N.; Holmes, J.; Jawad, R.; Whittlesea, C. Evaluation of a community pharmacy delivered oral contraception service. J. Fam. Plann. Reprod. Health Care 2013, 39, 97–101. [Google Scholar] [CrossRef]
- Gill, J.; Taylor, D. Improving Access to Contraception: Extended community pharmacy services would improve quality and outcomes. Lond. Sch. Econ. 2017. [Google Scholar] [CrossRef]
- Stippler, A.; Eckstein, N.; Kroth, E. Oral contraceptives as potential OTC-products: The views of German pharmacies, physicians, patients and stakeholders. SelfCare 2020, 11, 25–35. [Google Scholar]
- World Health Organization (WHO). Medical Eligibility Criteria for Contraceptive Use, 5th ed.; Reproductive Health and Research; WHO: Geneva, Switzerland, 2015; ISBN 978-92-4-154915-8. [Google Scholar]
- Gardner, J.S.; Downing, D.F.; Blough, D.; Miller, L.; Le, S.; Shotorbani, S. Pharmacist prescribing of hormonal contraceptives: Results of the Direct Access study. J. Am. Pharm. Assoc. 2008, 48, 212–226. [Google Scholar] [CrossRef] [PubMed]
- Mobark, D.M.; Al-Tabakha, M.M.; Hasan, S. Assessing hormonal contraceptive dispensing and counseling provided by community pharmacists in the United Arab Emirates: A simulated patient study. Pharm. Pract. (Granada) 2019, 17, 1465. [Google Scholar] [CrossRef] [PubMed]
- Stewart, F.H.; Harper, C.C.; Ellertson, C.E.; Grimes, D.A.; Sawaya, G.F.; Trussell, J. Clinical Breast and Pelvic Examination Requirements for Hormonal Contraception: Current Practice vs. Evidence. JAMA 2001, 285, 2232. [Google Scholar] [CrossRef] [PubMed]
- Hannaford, P.C.; Webb, A.M.C. Evidence-guided prescribing of combined oral contraceptives: Consensus statement. Contraception 1996, 54, 125–129. [Google Scholar] [CrossRef]
- Shotorbani, S.; Miller, L.; Blough, D.K.; Gardner, J. Agreement between women’s and providers’ assessment of hormonal contraceptive risk factors. Contraception 2006, 73, 501–506. [Google Scholar] [CrossRef]
- Kennedy, C.E.; Yeh, P.T.; Gonsalves, L.; Jafri, H.; Gaffield, M.E.; Kiarie, J.; Narasimhan, M.L. Should oral contraceptive pills be available without a prescription? A systematic review of over-the-counter and pharmacy access availability. BMJ Glob. Health 2019, 4, e001402. [Google Scholar] [CrossRef]
- Landau, S.C.; Tapias, M.P.; McGhee, B.T. Birth control within reach: A national survey on women’s attitudes toward and interest in pharmacy access to hormonal contraception. Contraception 2006, 74, 463–470. [Google Scholar] [CrossRef]
- Grossman, D.; Grindlay, K.; Li, R.; Potter, J.E.; Trussell, J.; Blanchard, K. Interest in over-the-counter access to oral contraceptives among women in the United States. Contraception 2013, 88, 544–552. [Google Scholar] [CrossRef]
- The American College of Obstetricians and Gynecologists (ACOG). Statement on Pharmacist Prescribing Laws. Available online: www.acog.org (accessed on 24 November 2019).
- McIntosh, J.; Rafie, S.; Wasik, M.; McBane, S.; Lodise, N.M.; El-Ibiary, S.Y.; Forinash, A.; Kachlic, M.D.; Rowe, E.; Besinque, K. Changing Oral Contraceptives from Prescription to Over-the-Counter Status: An Opinion Statement of the Women’s Health Practice and Research Network of the American College of Clinical Pharmacy. Pharmacotherapy 2011, 31, 424–437. [Google Scholar] [CrossRef]
- Newman, T.V.; Hernandez, I.; Keyser, D.; Rodriguez, A.S.-J.; Swart, E.C.S.; Shrank, W.H.; Parekh, N. Optimizing the Role of Community Pharmacists in Managing the Health of Populations: Barriers, Facilitators, and Policy Recommendations. JMCP 2019, 25, 995–1000. [Google Scholar] [CrossRef] [PubMed]
- Leuthold, C.; Bugnon, O.; Berger, J. The Role of Community Pharmacists in Travel Health and Vaccination in Switzerland. Pharmacy 2018, 6, 125. [Google Scholar] [CrossRef] [PubMed]
- The Pharmacy Guild of Australia. Sexual Health. Available online: www.findapharmacy.com (accessed on 19 June 2020).
- Burson, R.C.; Buttenheim, A.M.; Armstrong, A.; Feemster, K.A. Community pharmacies as sites of adult vaccination: A systematic review. Hum. Vaccines Immunother. 2016, 12, 3146–3159. [Google Scholar] [CrossRef] [PubMed]
- Babar, Z.-U.-D. Encyclopedia of Pharmacy Practice and Clinical Pharmacy, 1st ed.; Academic Press: Cambridge, MA, USA, 2019; ISBN 978-0-12-812736-0. [Google Scholar]
- European Medicines Agency (EMA). EMA Recommends Availability of EllaOne Emergency Contraceptive without Prescription. Available online: https://www.ema.europa.eu/en/news/ema-recommends-availability-ellaone-emergency-contraceptive-without-prescription (accessed on 27 April 2020).
- Federal Office of Public Health (FOPH). Simplified Supply of Medicinal Products Subject to Prescription. Available online: www.bag.admin.ch (accessed on 17 April 2020).
- Yous, T. Eine zukünftige Dienstleistung für Schweizer Apotheken? PharmaJournal 2020, 4, 25–26. [Google Scholar]
- Leiner, D.J. SoSci Survey—Professionelle Onlinebefragung Made in Germany. Available online: https://www.soscisurvey.de/ (accessed on 21 October 2020).
- Rafie, S.; Cieri-Hutcherson, N.E.; Frame, T.R.; Griffin, B.; Harris, J.B.; Horlen, C.; Shealy, K.; Stein, A.B.; Stone, R.H.; Vest, K.; et al. Pharmacists’ Perspectives on Prescribing and Expanding Access to Hormonal Contraception in Pharmacies in the United States. J. Pharm. Pract. 2019. [Google Scholar] [CrossRef]
- Kallus, W.K. Erstellung von Fragebogen, 2nd ed.; Utb GmbH: Wien, Austria, 2016; ISBN 978-3-8252-4465-1. [Google Scholar]
- Landau, S.; Besinque, K.; Chung, F.; Dries-Daffner, I.; Maderes, N.M.; McGhee, B.T.; Foster, D.G. Pharmacist interest in and attitudes toward direct pharmacy access to hormonal contraception in the United States. J. Am. Pharm. Assoc. 2009, 49, 43–50. [Google Scholar] [CrossRef]
- Hilverding, A.T.; DiPietro Mager, N.A. Pharmacists’ attitudes regarding provision of sexual and reproductive health services. J. Am. Pharm. Assoc. 2017, 57, 493–497. [Google Scholar] [CrossRef]
- Norman, W.V.; Soon, J.A.; Panagiotoglou, D.; Albert, A.; Zed, P.J. The acceptability of contraception task-sharing among pharmacists in Canada—The ACT-Pharm study. Contraception 2015, 92, 55–61. [Google Scholar] [CrossRef]
- Rafie, S.; El-Ibiary, S.Y. Student pharmacist perspectives on providing pharmacy-access hormonal contraception services. J. Am. Pharm. Assoc. 2011, 51, 762–765. [Google Scholar] [CrossRef]
- Vu, K.; Rafie, S.; Grindlay, K.; Gutierrez, H.; Grossman, D. Pharmacist Intentions to Prescribe Hormonal Contraception Following New Legislative Authority in California. J. Pharm. Pract. 2019, 32, 54–61. [Google Scholar] [CrossRef]
| Age (years) | n(%) |
| <30 | 64 (19%) |
| 30–39 | 115 (35%) |
| 40–49 | 65 (20%) |
| 50–59 | 62 (19%) |
| ≥60 | 25 (7%) |
| Average Age (SD) | 41 (12) |
| Median (min–max) | 38 (24–77) |
| Gender | n(%) |
| Female | 257 (78%) |
| Male | 74 (22%) |
| Work Setting | n(%) |
| Community Pharmacy | 304 (92%) |
| Hospital Pharmacy | 6 (2%) |
| Industry/Authority | 7 (2%) |
| Others (e.g., University) | 14 (4%) |
| Pharmacy Location | n(%) |
| Countryside | 94 (28%) |
| Urban | 237 (72%) |
| ≥1 Per Day | ≥1 Per Week | ≥1 Per Month | Never | |
|---|---|---|---|---|
| HC with Rx | 271 (82%) | 53 (16%) | 7 (2%) | 0 (0%) |
| HC without Rx | 29 (9%) | 130 (39%) | 161 (49%) | 11 (3%) |
| EC | 16 (5%) | 141 (43%) | 174 (52%) | 0 (0%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yous, T.; Allemann, S.; Lutters, M. Extended Access to Hormonal Contraception in Pharmacies: A Survey among Swiss Pharmacists. Pharmacy 2020, 8, 210. https://doi.org/10.3390/pharmacy8040210
Yous T, Allemann S, Lutters M. Extended Access to Hormonal Contraception in Pharmacies: A Survey among Swiss Pharmacists. Pharmacy. 2020; 8(4):210. https://doi.org/10.3390/pharmacy8040210
Chicago/Turabian StyleYous, Tamara, Samuel Allemann, and Monika Lutters. 2020. "Extended Access to Hormonal Contraception in Pharmacies: A Survey among Swiss Pharmacists" Pharmacy 8, no. 4: 210. https://doi.org/10.3390/pharmacy8040210
APA StyleYous, T., Allemann, S., & Lutters, M. (2020). Extended Access to Hormonal Contraception in Pharmacies: A Survey among Swiss Pharmacists. Pharmacy, 8(4), 210. https://doi.org/10.3390/pharmacy8040210





