Role of Pharmacists in Hormonal Contraceptive Access: A Survey of North Carolina Pharmacists
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Demographics and Baseline Characteristics
3.2. Perceived Benefits and Barriers of Pharmacist-Prescribed Hormonal Contraception
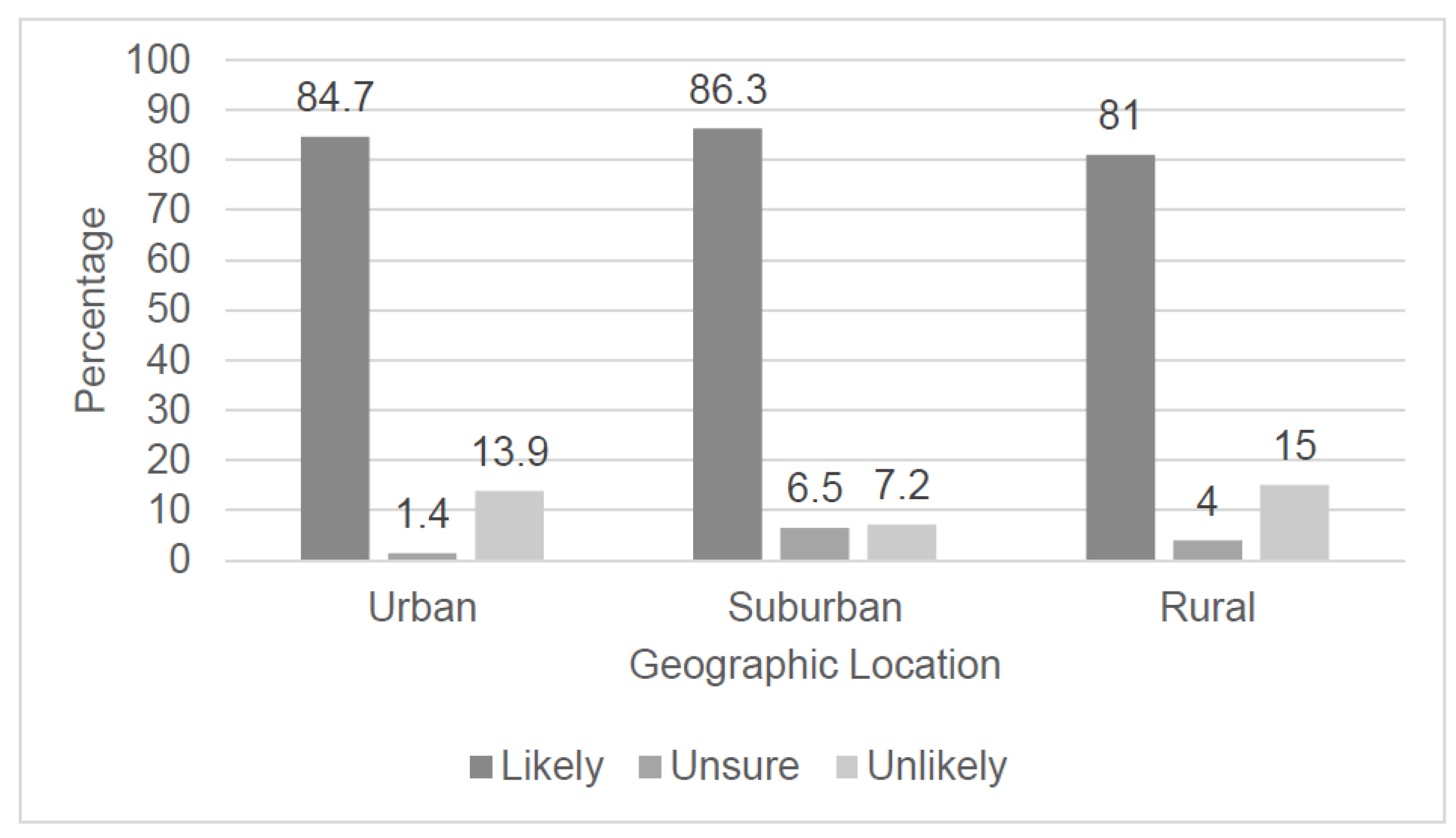
3.3. Pharmacist Interest and Comfort Level in Prescribing
3.4. Pharmacist Opinion of Prescriptive Classification of Hormonal Contraceptives
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Kost, K. Unintended Pregnancy Rates at the State Level: Estimates for 2010 and Trends Since 2002. New York: Guttmacher Institute. 2015. Available online: http://www.guttmacher.org/pubs/StateUP10.pdf (accessed on 15 September 2020).
- Finer, L.B.; Zolna, M.R. Declines in unintended pregnancy in the United States, 2008–2011. NEJM 2016, 374, 843–852. [Google Scholar] [CrossRef] [PubMed]
- Office of Disease Prevention and Health Promotion (ODPHP). Healthy People 2020: Family Planning. Available online: https://www.healthypeople.gov/2020/topics-objectives/topic/family-planning (accessed on 15 September 2020).
- Centers for Disease Control and Prevention (CDC). The 6/18 Initiative: Accelerating Evidence into Action. Available online: https://www.cdc.gov/sixeighteen/ (accessed on 15 September 2020).
- North Carolina Division of Public Health. Healthy North Carolina 2020: Focus Areas, Objectives, and Evidence-based Strategies Summary Tables. Available online: https://publichealth.nc.gov/hnc2020/foesummary.htm (accessed on 15 September 2020).
- American College of Obstetricians and Gynecologists. Access to Contraception. Committee Opinion No. 615. Obstet. Gynecol. 2015, 125, 250–255. [Google Scholar] [CrossRef] [PubMed]
- Tak, C.R.; Kessler, L.T.; Scott, M.A.; Gunning, K.M. Pharmacist-prescribed hormonal contraception: A review of the current landscape. J. Am. Pharm. Assoc. 2019. [Google Scholar] [CrossRef] [PubMed]
- National Alliance of State Pharmacy Associations (NASPA). Pharmacists Authorized to Prescribe Birth Control in More States. Available online: https://naspa.us/2017/05/pharmacists-authorized-prescribe-birth-control-states/ (accessed on 15 September 2020).
- North Carolina Board of Pharmacy. 21 NCAC 46.3101 Clinical Pharmacist Practitioner. 2017. Available online: http://www.ncbop.org/LawsRules/Rules.pdf (accessed on 15 September 2020).
- North Carolina Department of Health and Human Services. Provider Recruitment and Placement. Available online: https://www.ncdhhs.gov/divisions/office-rural-health/office-rural-health-programs/provider-recruitment-and-placement#:~:text=The%20shortage%20of%20primary%20health,uninsured%20and%20low%2Dincome%20patients (accessed on 18 August 2020).
- Vu, K.; Rafie, S.; Grindlay, K.; Gutierrez, H.; Grossman, D. Pharmacist intentions to prescribe hormonal contraception following new legislative authority in California. J. Pharm. Pract. 2019, 32, 54–61. [Google Scholar] [CrossRef] [PubMed]
- University of North Carolina The Cecil, G.; Sheps Center for Health Services Research. Pharmacists in North Carolina: Steady Numbers, Changing Roles. Available online: https://www.shepscenter.unc.edu/wp-content/uploads/2014/03/Pharmacists-in-North-Carolina-Steady-Numbers-Changing-Roles.pdf (accessed on 18 August 2020).
- Rodriguez, M.I.; McConnell, K.J.; Swartz, J.; Edelman, A.B. Pharmacist prescription of hormonal contraception in Oregon: Baseline knowledge and interest in provision. J. Am. Pharm. Assoc. 2016, 56, 521–526. [Google Scholar] [CrossRef] [PubMed]
- Landau, S.; Besinque, K.; Chung, F.; Dries-Daffner, I.; Maderes, N.M.; McGhee, B.T.; Foster, D.G. Pharmacist interest in attitudes toward direct pharmacy access to hormonal contraception in the United States. J. Am. Pharm. Assoc. 2009, 49, 43–50. [Google Scholar] [CrossRef] [PubMed]
- Gomez, A.M. Availability of Pharmacist-prescribed contraception in California. JAMA 2017, 318, 2253–2254. [Google Scholar] [CrossRef] [PubMed]
- Rafie, S.; Richards, E.; Rafie, S.; Landau, S.C.; Wilkinson, T.A. Pharmacist outlooks on prescribing hormonal contraception following statewide scope of practice expansion. Pharmacy 2019, 7, 96. [Google Scholar] [CrossRef] [PubMed]
- Anderson, L.; Hartung, D.M.; Middleton, L.; Rodriguez, M.I. Pharmacist provision of hormonal contraception in the Oregon Medicaid population. Obstet. Gynecol. 2019, 133, 1231–1237. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, M.I.; Hersh, A.; Anderson, L.B.; Hartung, D.M.; Edelman, A.B. Association of Pharmacist Prescription of Hormonal Contraception With Unintended Pregnancies and Medicaid Costs. Obstet. Gynecol. 2019, 133, 1238–1246. [Google Scholar] [CrossRef] [PubMed]
- Rafie, S.; Cieri-Hutcherson, N.E.; Frame, T.R.; Griffin, B.; Harris, J.B.; Horlen, C.; Shealy, K.; Stein, A.B.; Stone, R.H.; Vest, K.; et al. Pharmacists’ Perspectives on Prescribing and Expanding Access to Hormonal Contraception in Pharmacies in the United States. J. Pharm. Pract. 2019. [Google Scholar] [CrossRef] [PubMed]
- Rafie, S. An OTC Birth Control Pill Could Become a Reality. Available online: https://www.pharmacytimes.com/contributor/sally-rafie-pharmd/2017/01/an-otc-birth-control-pill-could-become-a-reality (accessed on 15 September 2020).
| Total, N (%) | Community-Based Pharmacist, N (%) | Non Community Pharmacist, N (%) | p Value | |
|---|---|---|---|---|
| All Pharmacist Characteristics (n = 713) | ||||
| Age | ||||
| <40 years old | 372 (52.1) | 207 (55.6) | 165 (44.4) | 0.07 |
| 40–59 years old | 220 (30.9) | 101 (45.9) | 119 (54.1) | |
| ≥60 years old | 102 (14.3) | 52 (51) | 50 (49) | |
| Missing | 19 (2.7) | |||
| Gender | ||||
| Female | 462 (64.8) | 224 (48.5) | 238 (51.5) | 0.01 |
| Missing | 13 (1.8) | |||
| Years as Licensed Pharmacist | ||||
| ≤10 years | 340 (47.7) | 196 (57.6) | 144 (42.4) | 0.01 |
| 11–20 years | 122 (17.1) | 59 (48.4) | 63 (51.6) | |
| ≥20 years | 242 (33.9) | 110 (45.5) | 132 (54.5) | |
| Missing | 9 (1.3) | |||
| Pharmacy Education/Training | ||||
| Doctor of Pharmacy (PharmD) degree | 515 (72.2) | 260 (50.5) | 255 (49.5) | 0.23 |
| Post-Graduate Year 1 (PGY1) Residency | 122 (17.1) | 14 (11.5) | 108 (88.5) | <0.0001 |
| Missing | 5 (7) | |||
| Previous Education/Training | ||||
| Reviewed prescribing protocols during pharmacy school | 298 (41.8) | 156 (52.3) | 142 (41.9) | 0.82 |
| Continuing Education course | 229 (32.7) | 126 (55) (55.1) | 103 (45) | 0.25 |
| None | 308 (43.2) | 153 (49.7) | 155 (50.3) | 0.31 |
| Other | 15 (2.1) | 8 (53.3) | 7 (46.7) | 0.91 |
| Missing | 13 (1.8) | |||
| Geographic Location of Practice Site | ||||
| Urban | 208 (29.2) | 88 (42.3) | 120 (57.7) | 0.0002 |
| Suburban | 271 (38) | 152 (56.1) | 119 (43.9) | |
| Rural | 191 (26.8) | 119 (62.3) | 72 (37.7) | |
| Missing | 43 (6) | |||
| Primary Practice Site a | ||||
| Community Practice—Chain | 251 (35.2) | 251 (35.2) | -- | N/A |
| Community Practice—Independent | 118 (16.5) | 118 (16.5) | -- | |
| Community Pharmacy Owner | 15 (2.1) | 15 (2.1) | -- | |
| Clinical Pharmacist—Hospital | 92 (12.9) | -- | 92 (12.9) | |
| Clinical Pharmacist—Ambulatory Care | 64 (9) | -- | 64 (9) | |
| Staff Hospital Pharmacist | 57 (8) | -- | 57 (8) | |
| Industry | 28 (3.9) | -- | 28 (3.9) | |
| Long-Term Care Pharmacy | 26 (3.6) | -- | 26 (3.6) | |
| Hospital Pharmacy Administration | 25 (3.5) | -- | 25 (3.5) | |
| Academia | 22 (3.1) | -- | 22 (3.1) | |
| Missing | 4 (0.6) | |||
| Community Pharmacy Characteristics (n = 384) | ||||
| Clinical Services Offered by Pharmacy | ||||
| Immunizations | 298 (77.6) | 298 (77.6) | -- | N/A |
| Medication Therapy Management | 207 (53.9) | 207 (53.9) | -- | N/A |
| Missing | 49 (12.8) | |||
| Emergency Contraception Available for Sale | ||||
| Yes | 293 (76.3) | 293 (76.3) | -- | N/A |
| Missing | 23 (6) | |||
| Privacy of Counseling Area | ||||
| Private | 88 (22.9) | 88 (22.9) | -- | N/A |
| Semi-private | 154 (40.1) | 154 (40.1) | -- | |
| Not private | 115 (29.9) | 115 (29.9) | -- | |
| Missing | 24 (6.3) | |||
| Statement | Community-Based Pharmacists (n = 384), N (%) | Noncommunity Pharmacists (n = 329), N (%) | p Value |
|---|---|---|---|
| Pharmacists are well-trained/educated to prescribe hormonal contraception. | 149 (38.8) | 160 (48.6) | 0.15 |
| Prescribing hormonal contraception allows pharmacists to practice at a higher level. | 257 (66.9) | 268 (81.4) | 0.02 |
| Increased access to hormonal contraception is an important public health issue. | 249 (64.8) | 258 (78.4) | 0.04 |
| Prescribing hormonal contraception will strengthen relationships with local physicians and clinics. | 138 (35.9) | 116 (35.3) | 0.18 |
| Rural areas would benefit from pharmacist-prescribed hormonal contraception. | 256 (66.7) | 267 (81.2) | 0.02 |
| Prescribing hormonal contraception will increase business/revenue in my pharmacy. | 205 (53.4) | -- | N/A |
| Prescribing hormonal contraception will help recruit pharmacists to work in our store. | 51 (13.3) | -- | N/A |
| Patients will benefit from improved access to hormonal contraception. | 264 (68.8) | -- | N/A |
| As a pharmacist, I enjoy individual patient contact. | 300 (78.1) | -- | N/A |
| Pharmacy access to hormonal contraception may foster increased use and adherence. | 267 (69.5) | -- | N/A |
| There are significant barriers to pharmacist-prescribed hormonal contraception within community pharmacies. | -- | 166 (50.5) | N/A |
| Additional training or education should be required for pharmacists to prescribe hormonal contraceptives. | -- | 273 (83) | N/A |
| There would be high acceptance of prescribing hormonal contraception amongst community pharmacists. | -- | 145 (44.1) | N/A |
| Barrier (n = 384) | Community-Based Pharmacists, N (%) |
|---|---|
| Added responsibility and liability | 268 (69.8) |
| Time constraints | 258 (67.2) |
| Need for pharmacist training | 251 (65.4) |
| Resistance from physicians | 216 (56.3) |
| Reimbursement barriers | 209 (54.4) |
| Inadequate privacy for counseling | 190 (49.5) |
| Pharmacist disinterest in prescribing hormonal contraception | 150 (39.1) |
| Resistance from management | 76 (19.8) |
| Resistance from patients | 61 (15.9) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Seamon, G.J.; Burke, A.; Tak, C.R.; Lenell, A.; Marciniak, M.W.; Scott, M.A. Role of Pharmacists in Hormonal Contraceptive Access: A Survey of North Carolina Pharmacists. Pharmacy 2020, 8, 191. https://doi.org/10.3390/pharmacy8040191
Seamon GJ, Burke A, Tak CR, Lenell A, Marciniak MW, Scott MA. Role of Pharmacists in Hormonal Contraceptive Access: A Survey of North Carolina Pharmacists. Pharmacy. 2020; 8(4):191. https://doi.org/10.3390/pharmacy8040191
Chicago/Turabian StyleSeamon, Gwen J, Allison Burke, Casey R Tak, Amy Lenell, Macary Weck Marciniak, and Mollie Ashe Scott. 2020. "Role of Pharmacists in Hormonal Contraceptive Access: A Survey of North Carolina Pharmacists" Pharmacy 8, no. 4: 191. https://doi.org/10.3390/pharmacy8040191
APA StyleSeamon, G. J., Burke, A., Tak, C. R., Lenell, A., Marciniak, M. W., & Scott, M. A. (2020). Role of Pharmacists in Hormonal Contraceptive Access: A Survey of North Carolina Pharmacists. Pharmacy, 8(4), 191. https://doi.org/10.3390/pharmacy8040191




