PRN Medicines Optimization and Nurse Education
Abstract
1. Burden of Medication Errors
is an avoidable adverse effect of healthcare, whether or not it is obvious or harmful to the patient something incorrectly done through ignorance or inadvertence; a mistake, e.g., in calculation, judgement, speech, writing, action, or a failure to complete a planned action as intended, or the use of an incorrect plan of action to achieve a given aim [5] (p. 6013).
2. Nurses’ Roles in Medicines Management
3. PRN Medication
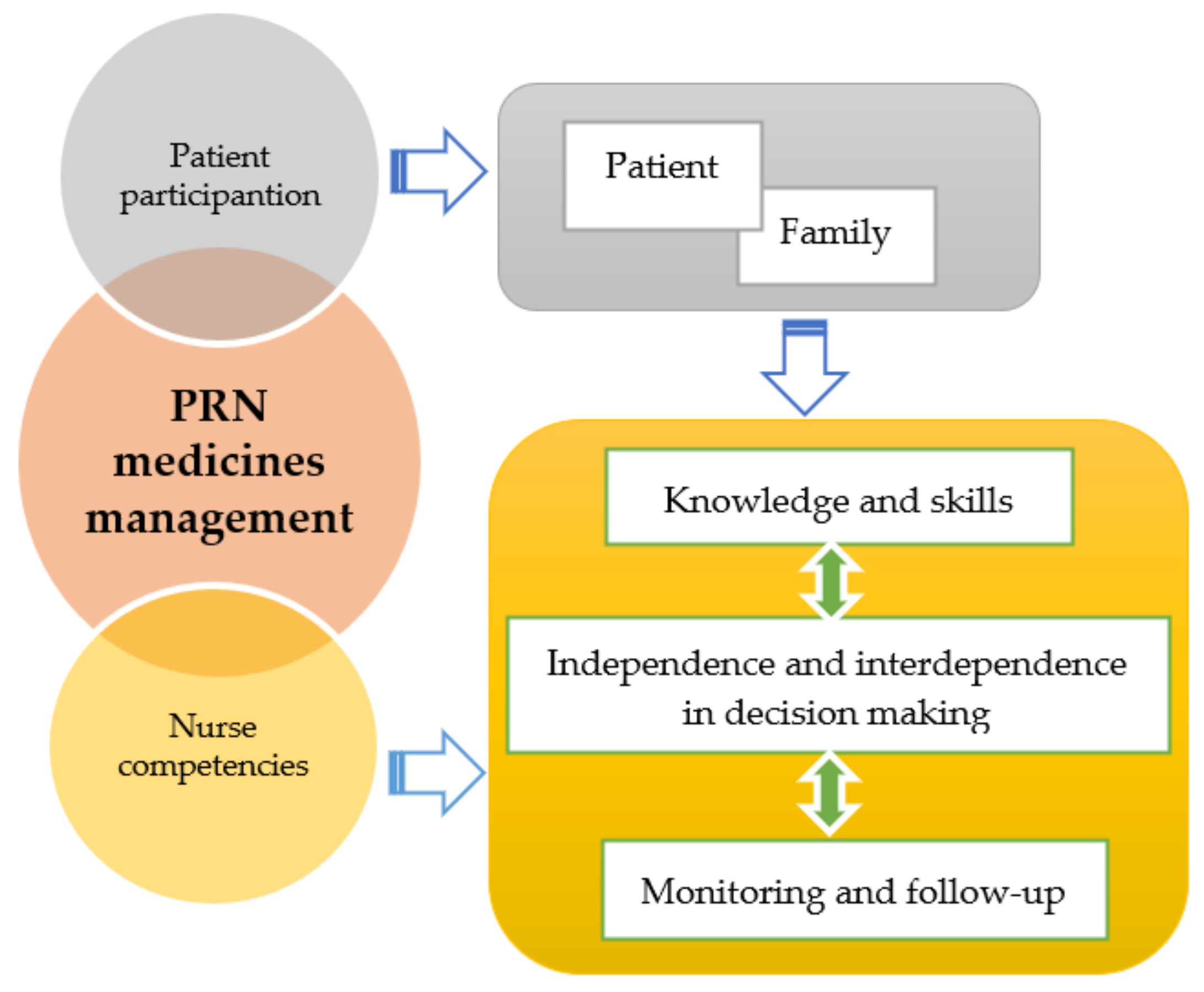
4. A Model for Education in PRN Medicines Management
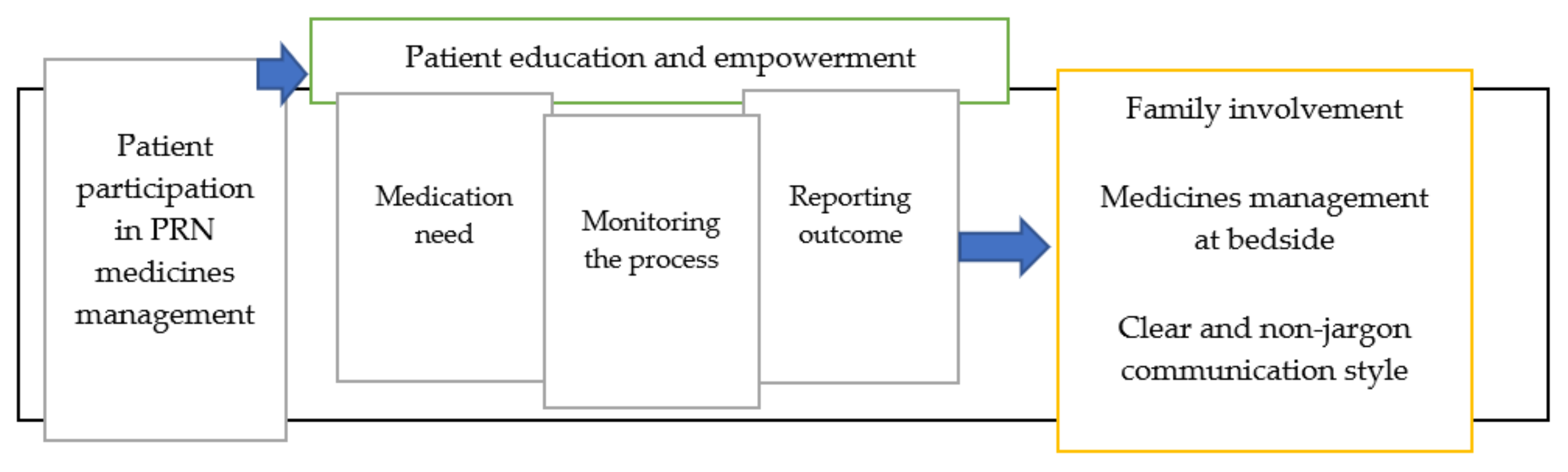
4.1. Patient Participation
4.2. Nurse Competencies
- Pharmacology knowledge;
- Medicine typologies;
- Pharmacokinetics;
- Administration method/dosage, interactions, circumstances that modify medicines management, contraindications, ADRs;
- Safe medicine management, and medication administration skills;
- Taking into account patient characteristics such as age, pathology and health condition in medicines management [76] (pp. 26–27);
- Taking a standardized medication history for medication reconciliation and detecting probable discrepancies [77].
4.2.1. Knowledge and Skills
- Circumstances affecting the use of PRN medications, including clinical and laboratory parameters;
- Doses, including the exact time and the maximum dose in a 24-hour period;
- Evaluation of the effectiveness of PRN medications after a determined time period [18];
4.2.2. Independence and Interdependence in Decision Making
4.2.3. Monitoring and Follow-Up
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Panagioti, M.; Khan, K.; Keers, R.N.; Abuzour, A.; Phipps, D.; Kontopantelis, E.; Bower, P.; Campbell, S.; Haneef, R.; Avery, A.J.; et al. Prevalence, severity, and nature of preventable patient harm across medical care settings: Systematic review and meta-analysis. BMJ 2019, 366, l4185. [Google Scholar] [CrossRef] [PubMed]
- Rodziewicz, T.L.; Hipskind, J.E. Medical Error Prevention. In StatPearls; StatPearls Publishing LLC.: Treasure Island, FL, USA, 2020. [Google Scholar]
- Sunshine, J.E.; Meo, N.; Kassebaum, N.J.; Collison, M.L.; Mokdad, A.H.; Naghavi, M. Association of Adverse Effects of Medical Treatment With Mortality in the United States: A Secondary Analysis of the Global Burden of Diseases, Injuries, and Risk Factors Study. JAMA Netw. Open 2019, 2, e187041. [Google Scholar] [CrossRef] [PubMed]
- Makary, M.A.; Daniel, M. Medical error—The third leading cause of death in the US. BMJ 2016, 353, i2139. [Google Scholar] [CrossRef] [PubMed]
- Aronson, J.K. Medication errors: Definitions and classification. Br. J. Clin. Pharmacol. 2009, 67, 599–604. [Google Scholar] [CrossRef]
- Hofer, T.P.; Kerr, E.A.; Hayward, R.A. What is an error? Eff. Clin. Pract. 2000, 3, 261–269. [Google Scholar]
- Carver, N.; Gupta, V.; Hipskind, J.E. Medical Error. In StatPearls; StatPearls Publishing LLC.: Treasure Island, FL, USA, 2020. [Google Scholar]
- NCC MERP: National Co-ordinating Council for Medication Error Reporting and Prevention. NCC MERP: About Medication Errors. What is a Medication Error? 2018. Available online: http://www.nccmerp.org/about-medication-errors (accessed on 26 September 2020).
- Bouvy, J.C.; De Bruin, M.L.; Koopmanschap, M.A. Epidemiology of adverse drug reactions in Europe: A review of recent observational studies. Drug Saf. 2015, 38, 437–453. [Google Scholar] [CrossRef]
- Hazell, L.; Shakir, S.A. Under-reporting of adverse drug reactions: A systematic review. Drug Saf. 2006, 29, 385–396. [Google Scholar] [CrossRef]
- Wu, L.; Ingle, T.; Liu, Z.; Zhao-Wong, A.; Harris, S.; Thakkar, S.; Zhou, G.; Yang, J.; Xu, J.; Mehta, D.; et al. Study of serious adverse drug reactions using FDA-approved drug labeling and MedDRA. BMC Bioinform. 2019, 20, 97. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Reporting and Learning Systems for Medication Errors: The Role of Pharmacovigilance Centres. 2014. Available online: https://www.who.int/medicines/areas/quality_safety/safety_efficacy/emp_mes/en/ (accessed on 17 September 2020).
- Khalil, H.; Bell, B.; Chambers, H.; Sheikh, A.; Avery, A.J. Professional, structural and organisational interventions in primary care for reducing medication errors. Cochrane Database Syst. Rev. 2017, 10, Cd003942. [Google Scholar] [CrossRef]
- Kavanagh, C. Medication governance: Preventing errors and promoting patient safety. Br. J. Nurs. 2017, 26, 159–165. [Google Scholar] [CrossRef]
- Palese, A.; Gonella, S.; Grassetti, L.; Mansutti, I.; Brugnolli, A.; Saiani, L.; Terzoni, S.; Zannini, L.; Destrebecq, A.; Dimonte, V. Multi-level analysis of national nursing students’ disclosure of patient safety concerns. Med. Educ. 2018, 52, 1156–1166. [Google Scholar] [CrossRef] [PubMed]
- Vaismoradi, M.; Salsali, M.; Marck, P. Patient safety: Nursing students’ perspectives and the role of nursing education to provide safe care. Int. Nurs. Rev. 2011, 58, 434–442. [Google Scholar] [CrossRef]
- GuKG, N. Gesundheits-und Krankenpflegegesetz 1997, BGBI.INr.108/1997i.d.F.BGBl.INr.8/2016. 1997. Available online: https://www.ris.bka.gv.at/Dokumente/BgblAuth/BGBLA_2016_I_75/BGBLA_2016_I_75.pdf (accessed on 17 September 2020).
- Health Information and Quality Authority (HIQA). Medicines Management Guidance. 2015. Available online: https://www.hiqa.ie/sites/default/files/2017-01/Medicines-Management-Guidance.pdf (accessed on 17 September 2020).
- Covell, C.L.; Ritchie, J.A. Nurses’ responses to medication errors: Suggestions for the development of organizational strategies to improve reporting. J. Nurs Care Qual. 2009, 24, 287–297. [Google Scholar] [CrossRef] [PubMed]
- Rohde, E.; Domm, E. Nurses’ clinical reasoning practices that support safe medication administration: An integrative review of the literature. J. Clin. Nurs. 2018, 27, e402–e411. [Google Scholar] [CrossRef] [PubMed]
- Asensi-Vicente, J.; Jiménez-Ruiz, I.; Vizcaya-Moreno, M.F. Medication Errors Involving Nursing Students: A Systematic Review. Nurse Educ. 2018, 43, E1–E5. [Google Scholar] [CrossRef]
- Cronenwett, L.R.; Bootman, J.L.; Wolcott, J.; Aspden, P.; Institute of Medicine Board on Health Care Services; Committee on Identifying and Preventing Medication Errors (Eds.) Preventing Medication Errors (Quality Chasm); National Academies Press: Washington, DC, USA, 2007. Available online: https://www.nap.edu/initiative/committee-on-identifying-and-preventing-medication-errors (accessed on 17 September 2020).
- World Health Organization (WHO). Patient Safety: Data and Statistics. 2020. Available online: https://www.euro.who.int/en/health-topics/Health-systems/patient-safety/data-and-statistics (accessed on 17 September 2020).
- Escrivá Gracia, J.; Brage Serrano, R.; Fernández Garrido, J. Medication errors and drug knowledge gaps among critical-care nurses: A mixed multi-method study. BMC Health Serv. Res. 2019, 19, 640. [Google Scholar] [CrossRef]
- Moyen, E.; Camiré, E.; Stelfox, H.T. Clinical review: Medication errors in critical care. Crit. Care 2008, 12, 208. [Google Scholar] [CrossRef]
- Slight, S.P.; Tolley, C.L.; Bates, D.W.; Fraser, R.; Bigirumurame, T.; Kasim, A.; Balaskonis, K.; Narrie, S.; Heed, A.; Orav, E.J.; et al. Medication errors and adverse drug events in a UK hospital during the optimisation of electronic prescriptions: A prospective observational study. Lancet Digit. Health 2019, 1, e403–e412. [Google Scholar] [CrossRef]
- Berland, A.; Bentsen, S.B. Medication errors in home care: A qualitative focus group study. J Clin. Nurs. 2017, 26, 3734–3741. [Google Scholar] [CrossRef]
- Vaismoradi, M.; Vizcaya Moreno, F.; Sletvold, H.; Jordan, S. PRN Medicines Management for Psychotropic Medicines in Long-Term Care Settings: A Systematic Review. Pharmacy 2019, 7, 157. [Google Scholar] [CrossRef]
- Ferrah, N.; Lovell, J.J.; Ibrahim, J.E. Systematic Review of the Prevalence of Medication Errors Resulting in Hospitalization and Death of Nursing Home Residents. J. Am. Geriatr. Soc. 2017, 65, 433–442. [Google Scholar] [CrossRef] [PubMed]
- Pegram, A.; Bloomfield, J. Medicines management. Nurs. Stand. 2015, 29, 36–43. [Google Scholar] [CrossRef]
- Shahbazi, S.; Valizadeh, S.; Borimnejad, L.; Rahmani, A.; Vaismoradi, M. Living With Moral Distress: The Perspectives and Experiences of Iranian Nurse Preceptors. Res. Theory Nurs. Pract. 2018, 32, 355–369. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). WHO Launches Global Effort to Halve Medication-Related Errors in 5 Years. 2017. Available online: http://www.who.int/mediacentre/news/releases/2017/medication-related-errors/en/ (accessed on 17 September 2020).
- Martin, K.; Arora, V.; Fischler, I.; Tremblay, R. Descriptive analysis of pro re nata medication use at a Canadian psychiatric hospital. Int. J. Ment. Health Nurs. 2017, 26, 402–408. [Google Scholar] [CrossRef]
- Vaismoradi, M.; Amaniyan, S.; Jordan, S. Patient Safety and Pro Re Nata Prescription and Administration: A Systematic Review. Pharmacy 2018, 6, 95. [Google Scholar] [CrossRef]
- Adelaide, D.; Rawther, F. Audit: Prescribing PRN medication. Psychiatr. Danub. 2017, 29, 568–570. [Google Scholar]
- Griffiths, A.W.; Surr, C.A.; Alldred, D.P.; Baker, J.; Higham, R.; Spilsbury, K.; Thompson, C.A. Pro re nata prescribing and administration for neuropsychiatric symptoms and pain in long-term care residents with dementia and memory problems: A cross-sectional study. Int. J. Clin. Pharm. 2019, 41, 1314–1322. [Google Scholar] [CrossRef]
- Picton, L.; Ilomäki, J.; Keen, C.S.; Lalic, S.; Adams, B.; Clinnick, L.M.; Kirkpatrick, C.M.; Ryan-Atwood, T.; Turner, J.P.; Bell, J.S. Rates of PRN Medication Administration in Australian Residential Aged Care. J. Am. Med. Dir. Assoc. 2020. [Google Scholar] [CrossRef]
- Stasinopoulos, J.; Bell, J.S.; Ryan-Atwood, T.E.; Tan, E.C.K.; Ilomäki, J.; Cooper, T.; Robson, L.; Sluggett, J.K. Frequency of and factors related to pro re nata (PRN) medication use in aged care services. Res. Soc. Adm. Pharm. 2018, 14, 964–967. [Google Scholar] [CrossRef]
- Martin, K.; Ham, E.; Hilton, N.Z. Staff and patient accounts of PRN medication administration and non-pharmacological interventions for anxiety. Int. J. Ment. Health Nurs. 2018, 27, 1834–1841. [Google Scholar] [CrossRef]
- Jordan, S.; Banner, T.; Gabe-Walters, M.; Mikhail, J.M.; Panes, G.; Round, J.; Snelgrove, S.; Storey, M.; Hughes, D. Nurse-led medicines’ monitoring in care homes, implementing the Adverse Drug Reaction (ADRe) Profile improvement initiative for mental health medicines: An observational and interview study. PLoS ONE 2019, 14, e0220885. [Google Scholar] [CrossRef] [PubMed]
- Jordan, S.; Logan, P.A.; Panes, G.; Vaismoradi, M.; Hughes, D. Adverse Drug Reactions, Power, Harm Reduction, Regulation and the ADRe Profiles. Pharmacy 2018, 6, 102. [Google Scholar] [CrossRef] [PubMed]
- Baumann, S.L.; Greif, N. The use of PRNs medications with hospitalized older adults. Geriatr. Nurs. 2017, 38, 596–598. [Google Scholar] [CrossRef]
- Tong, Y.; Chen, J.; Chai, L.; Yang, L.; Zhang, C.; Liu, M. Current State of Pain Resource Nurse (PRN) Programs and Experiences of PRNs in China. Pain Manag. Nurs. 2019, 20, 174–182. [Google Scholar] [CrossRef] [PubMed]
- Hipp, K.; Kuosmanen, L.; Repo-Tiihonen, E.; Leinonen, M.; Louheranta, O.; Kangasniemi, M. Patient participation in pro re nata medication in psychiatric inpatient settings: An integrative review. Int. J. Ment. Health Nurs. 2018, 27, 536–554. [Google Scholar] [CrossRef]
- Usher, K.; Holmes, C.; Lindsay, D.; Luck, L. PRN psychotropic medications: The need for nursing research. Contemp. Nurse 2003, 14, 248–257. [Google Scholar] [CrossRef]
- Abdallah, M.S.; Sheikh, M.A.; Alaqqad, A.; Alharthy, A.; Aldossari, M.; Alodat, M.; Kurdi, M.; Salem, S.; Mady, A.F. PRN Medications Ordering Practice at a Large Intensive Care Unit in Saudi Arabia. J. Intensiv. Crit. Care 2016, 2, 1–5. [Google Scholar] [CrossRef]
- Asogwa, K.; Okudo, J.; Idowu, J. The use and effectiveness of pro re nata psychotropic medications in children and adolescents: A systematic review. Indian J. Psychiatry 2017, 59, 264–274. [Google Scholar] [CrossRef]
- Jimu, M.; Doyle, L. The Administration of Pro re nata Medication by Mental Health Nurses: A Thematic Analysis. Issues Ment. Health Nurs. 2019, 40, 511–517. [Google Scholar] [CrossRef]
- Dörks, M.; Allers, K.; Hoffmann, F. Pro Re Nata Drug Use in Nursing Home Residents: A Systematic Review. J. Am. Med. Dir. Assoc. 2019, 20, 287–293. [Google Scholar] [CrossRef]
- Salazar, A.; Karmiy, S.J.; Forsythe, K.J.; Amato, M.G.; Wright, A.; Lai, K.H.; Lambert, B.L.; Liebovitz, D.M.; Eguale, T.; Volk, L.A.; et al. How often do prescribers include indications in drug orders? Analysis of 4 million outpatient prescriptions. Am. J. Health Pharm. 2019, 76, 970–979. [Google Scholar] [CrossRef] [PubMed]
- Dörks, M.; Schmiemann, G.; Hoffmann, F. Pro re nata (as needed) medication in nursing homes: The longer you stay, the more you get? Eur. J. Clin. Pharmacol. 2016, 72, 995–1001. [Google Scholar] [CrossRef] [PubMed]
- Martin, K.; Ham, E.; Hilton, N.Z. Documentation of psychotropic pro re nata medication administration: An evaluation of electronic health records compared with paper charts and verbal reports. J. Clin. Nurs. 2018, 27, 3171–3178. [Google Scholar] [CrossRef]
- Paton, C.; Barnes, T.R.; Cavanagh, M.R.; Taylor, D.; Lelliott, P. High-dose and combination antipsychotic prescribing in acute adult wards in the UK: The challenges posed by p.r.n. prescribing. Br. J. Psychiatry 2008, 192, 435–439. [Google Scholar] [CrossRef]
- Hammer, A.; Wagner, A.; Rieger, M.A.; Manser, T. Assessing the quality of medication documentation: Development and feasibility of the MediDocQ instrument for retrospective chart review in the hospital setting. BMJ Open 2019, 9, e034609. [Google Scholar] [CrossRef]
- Tyrrell-Bunge, E.; de Carvalho, A.F.; Scott, C.; Tomlin, S.; Treasure, J.; Himmerich, H. A three level-intervention to reduce PRN medication on a specialist eating disorders ward for adult female patients with anorexia nervosa. Psychiatr. Danub. 2018, 30, 107–108. [Google Scholar]
- Flinkman, M.; Leino-Kilpi, H.; Numminen, O.; Jeon, Y.; Kuokkanen, L.; Meretoja, R. Nurse Competence Scale: A systematic and psychometric review. J. Adv. Nurs. 2017, 73, 1035–1050. [Google Scholar] [CrossRef]
- Goedhart, N.S.; van Oostveen, C.J.; Vermeulen, H. The effect of structural empowerment of nurses on quality outcomes in hospitals: A scoping review. J. Nurs. Manag. 2017, 25, 194–206. [Google Scholar] [CrossRef]
- Nilsen, M.K.; Sletvold, H.; Olsen, R.M. ‘To give or not to give medication, that is the question.’ Healthcare personnel’s perceptions of factors affecting pro re nata medication in sheltered housing for older adults—A focus-group interview study. BMC Health Serv. Res. 2020, 20, 622. [Google Scholar] [CrossRef]
- Náfrádi, L.; Nakamoto, K.; Schulz, P.J. Is patient empowerment the key to promote adherence? A systematic review of the relationship between self-efficacy, health locus of control and medication adherence. PLoS ONE 2017, 12, e0186458. [Google Scholar] [CrossRef] [PubMed]
- Holmqvist, M.; Thor, J.; Ros, A.; Johansson, L. Older persons’ experiences regarding evaluation of their medication treatment—An interview study in Sweden. Health Expect. 2019, 22, 1294–1303. [Google Scholar] [CrossRef]
- Look, K.A.; Stone, J.A. Medication management activities performed by informal caregivers of older adults. Res. Soc. Adm. Pharm. 2018, 14, 418–426. [Google Scholar] [CrossRef] [PubMed]
- Manias, E.; Bucknall, T.; Hughes, C.; Jorm, C.; Woodward-Kron, R. Family involvement in managing medications of older patients across transitions of care: A systematic review. BMC Geriatr. 2019, 19, 95. [Google Scholar] [CrossRef] [PubMed]
- Pohontsch, N.J.; Löffler, A.; Luck, T.; Heser, K.; Parker, D.; Haenisch, B.; Riedel-Heller, S.G.; Jessen, F.; Scherer, M. Informal caregivers’ perspectives on health of and (potentially inappropriate) medication for (relatively) independent oldest-old people-a qualitative interview study. BMC Geriatr. 2018, 18, 169. [Google Scholar] [CrossRef]
- Dolu, İ.; Naharcı, M.İ.; Logan, P.A.; Paal, P.; Vaismoradi, M. Transitional ‘hospital to home’ care of older patients: Healthcare professionals’ perspectives. Scand. J. Caring Sci. 2020. [Google Scholar] [CrossRef]
- Richard, C.; Glaser, E.; Lussier, M.-T. Communication and patient participation influencing patient recall of treatment discussions. Health Expect 2017, 20, 760–770. [Google Scholar] [CrossRef]
- Tobiano, G.; Chaboyer, W.; Teasdale, T.; Raleigh, R.; Manias, E. Patient engagement in admission and discharge medication communication: A systematic mixed studies review. Int. J. Nurs. Stud. 2019, 95, 87–102. [Google Scholar] [CrossRef]
- Kim, J.M.; Suarez-Cuervo, C.; Berger, Z.; Lee, J.; Gayleard, J.; Rosenberg, C.; Nagy, N.; Weeks, K.; Dy, S. Evaluation of Patient and Family Engagement Strategies to Improve Medication Safety. Patient 2018, 11, 193–206. [Google Scholar] [CrossRef]
- Prey, J.E.; Polubriaginof, F.; Grossman, L.V.; Masterson Creber, R.; Tsapepas, D.; Perotte, R.; Qian, M.; Restaino, S.; Bakken, S.; Hripcsak, G.; et al. Engaging hospital patients in the medication reconciliation process using tablet computers. J. Am. Med. Inform. Assoc. 2018, 25, 1460–1469. [Google Scholar] [CrossRef] [PubMed]
- Ringdal, M.; Chaboyer, W.; Ulin, K.; Bucknall, T.; Oxelmark, L. Patient preferences for participation in patient care and safety activities in hospitals. BMC Nurs. 2017, 16, 69. [Google Scholar] [CrossRef] [PubMed]
- McTier, L.; Botti, M.; Duke, M. Patient participation in medication safety during an acute care admission. Health Expect. 2015, 18, 1744–1756. [Google Scholar] [CrossRef]
- Oxelmark, L.; Ulin, K.; Chaboyer, W.; Bucknall, T.; Ringdal, M. Registered Nurses’ experiences of patient participation in hospital care: Supporting and hindering factors patient participation in care. Scand. J. Caring Sci. 2018, 32, 612–621. [Google Scholar] [CrossRef]
- Bucknall, T.; Digby, R.; Fossum, M.; Hutchinson, A.M.; Considine, J.; Dunning, T.; Hughes, L.; Weir-Phyland, J.; Manias, E. Exploring patient preferences for involvement in medication management in hospitals. J. Adv. Nurs. 2019, 75, 2189–2199. [Google Scholar] [CrossRef] [PubMed]
- Tobiano, G.; Bucknall, T.; Marshall, A.; Guinane, J.; Chaboyer, W. Nurses’ views of patient participation in nursing care. J. Adv. Nurs. 2015, 71, 2741–2752. [Google Scholar] [CrossRef]
- Fukada, M. Nursing Competency: Definition, Structure and Development. Yonago Acta Med. 2018, 61, 1–7. [Google Scholar] [CrossRef]
- European Council. European Council Directive 2013/55/EU on the recognition of professional qualifications. Off. J. Eur. Union 2013, 354, 132–169. [Google Scholar]
- European Federation of Nurses. EFN Guideline for the implementation of Article 31 of the Mutual Recognition of Professional Qualifications Directive 2005/36/EC, Amended by Directive 2013/55/EU. EFN Guideline to Implement Article 31 into National Nurses’ Education Programmes. 2015. Available online: http://www.efnweb.be/?page_id=6897 (accessed on 19 October 2020).
- Holt, K.M.; Thompson, A.N. Implementation of a Medication Reconciliation Process in an Internal Medicine Clinic at an Academic Medical Center. Pharmacy 2018, 6, 26. [Google Scholar] [CrossRef]
- Murphy, M.L. Mentoring students in medicines management. Nurs. Stand. 2012, 26, 51–56. [Google Scholar] [CrossRef]
- Amaniyan, S.; Pouyesh, V.; Bashiri, Y.; Snelgrove, S.; Vaismoradi, M. Comparison of the Conceptual Map and Traditional Lecture Methods on Students’ Learning Based on the VARK Learning Style Model: A Randomized Controlled Trial. SAGE Open Nurs. 2020, 6. [Google Scholar] [CrossRef]
- Sulosaari, V.; Huupponen, R.; Hupli, M.; Puukka, P.; Torniainen, K.; Leino-Kilpi, H. Factors associated with nursing students’ medication competence at the beginning and end of their education. BMC Med. Educ. 2015, 15, 223. [Google Scholar] [CrossRef] [PubMed]
- Fothergill Bourbonnais, F.; Caswell, W. Teaching successful medication administration today: More than just knowing your ‘rights’. Nurse Educ. Pract. 2014, 14, 391–395. [Google Scholar] [CrossRef] [PubMed]
- Preston, P.; Leone-Sheehan, D.; Keys, B. Nursing student perceptions of pharmacology education and safe medication administration: A qualitative research study. Nurse Educ. Today 2019, 74, 76–81. [Google Scholar] [CrossRef]
- Evans, C.B.; Mixon, D.K. The Evaluation of Undergraduate Nursing Students’ Knowledge of Post-op Pain Management after Participation in Simulation. Pain Manag. Nurs. 2015, 16, 930–937. [Google Scholar] [CrossRef]
- Armitage, G.; Knapman, H. Adverse events in drug administration: A literature review. J. Nurs. Manag. 2003, 11, 130–140. [Google Scholar] [CrossRef]
- Edwards, S.; Axe, S. The 10 ‘R’s of safe multidisciplinary drug administration. Nurse Prescr. 2015, 13, 398–406. [Google Scholar] [CrossRef]
- Vaismoradi, M. Call for Role Development and Application of the Monitoring Profile in ADEs and ADRs. Pharmacy 2018, 6, 118. [Google Scholar] [CrossRef]
- Hewitt, J.; Tower, M.; Latimer, S. An education intervention to improve nursing students’ understanding of medication safety. Nurse Educ. Pract. 2015, 15, 17–21. [Google Scholar] [CrossRef]
- Krivanek, M.J.; Dolansky, M.A.; Kukla, A.; Ramic, M.; Guliano, J.; Waite, P.; Small, D. Perspectives From Academic and Practice Leaders on Nursing Student’s Education and Role in Medication Reconciliation. J. Prof. Nurs. 2019, 35, 75–80. [Google Scholar] [CrossRef] [PubMed]
- Latimer, S.; Hewitt, J.; Stanbrough, R.; McAndrew, R. Reducing medication errors: Teaching strategies that increase nursing students’ awareness of medication errors and their prevention. Nurse Educ. Today 2017, 52, 7–9. [Google Scholar] [CrossRef] [PubMed]
- Green, C. Contemporary issues: The pre-licensure nursing student and medication errors. Nurse Educ. Today 2018, 68, 23–25. [Google Scholar] [CrossRef]
- Brusamento, S.; Kyaw, B.M.; Whiting, P.; Li, L.; Tudor Car, L. Digital Health Professions Education in the Field of Pediatrics: Systematic Review and Meta-Analysis by the Digital Health Education Collaboration. J. Med. Internet Res. 2019, 21, e14231. [Google Scholar] [CrossRef]
- Gluyas, H.; Morrison, P. Human factors and medication errors: A case study. Nurs. Stand. 2014, 29, 37–42. [Google Scholar] [CrossRef]
- Zarifsanaiey, N.; Amini, M.; Saadat, F. A comparison of educational strategies for the acquisition of nursing student’s performance and critical thinking: Simulation-based training vs. integrated training (simulation and critical thinking strategies). BMC Med. Educ. 2016, 16, 294. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Ye, X.; Chen, W. Practice and effectiveness of “nursing case-based learning” course on nursing student’s critical thinking ability: A comparative study. Nurse Educ. Pract. 2019, 36, 91–96. [Google Scholar] [CrossRef] [PubMed]
- Jordan, S. Teaching pharmacology by case study. Nurse Educ. Today 1997, 17, 386–393. [Google Scholar] [CrossRef]
- Musharyanti, L.; Claramita, M.; Haryanti, F.; Dwiprahasto, I. Why do nursing students make medication errors? A qualitative study in Indonesia. J. Taibah Univ. Med. Sci. 2019, 14, 282–288. [Google Scholar] [CrossRef]
- Hayes, C.; Power, T.; Davidson, P.M.; Daly, J.; Jackson, D. Learning to liaise: Using medication administration role-play to develop teamwork in undergraduate nurses. Contemp. Nurse 2019, 55, 278–287. [Google Scholar] [CrossRef]
- Simones, J.; Neal, D.l.; Schug, V.; Blazovich, L.M.; Pivec, C.; Daniels, J.; Becker, M.K.; Schulenberg, C.; Lehman, S.M.; Ohman, L.A.; et al. Student nurses’ thinking during medication administration. J. Nurs. Educ. Pract. 2014, 4, 136–146. [Google Scholar] [CrossRef]
- Laurant, M.; van der Biezen, M.; Wijers, N.; Watananirun, K.; Kontopantelis, E.; van Vught, A.J. Nurses as substitutes for doctors in primary care. Cochrane Database Syst. Rev. 2018, 7, CD001271. [Google Scholar] [CrossRef]
- Green, C. Medication Simulation: Enhancing Nursing Students’ Clinical Environmental Awareness through Self-Care and Promotion of Patient Safety. Whitireia Nurs. Health J. 2018, 25, 37–51. [Google Scholar]
- Shahsavari, H.; Zare, Z.; Parsa-Yekta, Z.; Griffiths, P.; Vaismoradi, M. Learning situations in nursing education: A concept analysis. Res. Theory Nurs. Pract. Int. J. 2018, 32, 23–45. [Google Scholar] [CrossRef]
- Hewitt, T.; Chreim, S.; Forster, A. Double checking: A second look. J. Eval. Clin. Pract. 2016, 22, 267–274. [Google Scholar] [CrossRef] [PubMed]
- Koyama, A.K.; Maddox, C.-S.S.; Li, L.; Bucknall, T.; Westbrook, J.I. Effectiveness of double checking to reduce medication administration errors: A systematic review. BMJ Qual. Saf. 2020, 29, 595. [Google Scholar] [CrossRef] [PubMed]
- Durham, B. The nurse’s role in medication safety. Nursing 2015, 45. [Google Scholar] [CrossRef]
- Härkänen, M.; Blignaut, A.; Vehviläinen-Julkunen, K. Focus group discussions of registered nurses’ perceptions of challenges in the medication administration process. Nurs. Health Sci. 2018, 20, 431–437. [Google Scholar] [CrossRef] [PubMed]
- Niederhauser, A.; Zimmermann, C.; Fishman, L.; Schwappach, D.L.B. Implications of involving pharmacy technicians in obtaining a best possible medication history from the perspectives of pharmaceutical, medical and nursing staff: A qualitative study. BMJ Open 2018, 8, e020566. [Google Scholar] [CrossRef]
- Tang, C.J.; Zhou, W.T.; Chan, S.W.; Liaw, S.Y. Interprofessional collaboration between junior doctors and nurses in the general ward setting: A qualitative exploratory study. J. Nurs. Manag. 2018, 26, 11–18. [Google Scholar] [CrossRef]
- Wilson, A.J.; Palmer, L.; Levett-Jones, T.; Gilligan, C.; Outram, S. Interprofessional collaborative practice for medication safety: Nursing, pharmacy, and medical graduates’ experiences and perspectives. J. Interprof. Care 2016, 30, 649–654. [Google Scholar] [CrossRef]
- Goolsarran, N.; Hamo, C.E.; Lane, S.; Frawley, S.; Lu, W.-H. Effectiveness of an interprofessional patient safety team-based learning simulation experience on healthcare professional trainees. BMC Med Educ. 2018, 18, 192. [Google Scholar] [CrossRef]
- Hwang, J.I.; Yoon, T.Y.; Jin, H.J.; Park, Y.; Park, J.Y.; Lee, B.J. Patient safety competence for final-year health professional students: Perceptions of effectiveness of an interprofessional education course. J. Interprof. Care 2016, 30, 732–738. [Google Scholar] [CrossRef]
- Irajpour, A.; Farzi, S.; Saghaei, M.; Ravaghi, H. Effect of interprofessional education of medication safety program on the medication error of physicians and nurses in the intensive care units. J. Educ. Health Promot. 2019, 8, 196. [Google Scholar] [CrossRef] [PubMed]
- Weintraub, W.S.; Fahed, A.C.; Rumsfeld, J.S. Translational Medicine in the Era of Big Data and Machine Learning. Circ. Res. 2018, 123, 1202–1204. [Google Scholar] [CrossRef] [PubMed]
- Musy, S.N.; Simon, M. Big Data in Healthcare: New Methods of Analysis. In Big Data-Enabled Nursing: Education, Research and Practice; Delaney, C.W., Weaver, C.A., Warren, J.J., Clancy, T.R., Simpson, R.L., Eds.; Springer International Publishing: Cham, Switzerland, 2017; pp. 79–101. [Google Scholar]
- Brady, A.M.; Malone, A.M.; Fleming, S. A literature review of the individual and systems factors that contribute to medication errors in nursing practice. J. Nurs. Manag. 2009, 17, 679–697. [Google Scholar] [CrossRef] [PubMed]
- Mallick-Searle, T.; Chang, H. The importance of nurse monitoring for potential opioid abuse in their patients. J. Appl. Biobehav. Res. 2018, 23, e12129. [Google Scholar] [CrossRef]
- Dirik, H.F.; Samur, M.; Seren Intepeler, S.; Hewison, A. Nurses’ identification and reporting of medication errors. J. Clin. Nurs. 2019, 28, 931–938. [Google Scholar] [CrossRef]
- Jordan, S.; Jordan, M.; Logan, P.; Vaismoradi, M.; Hughes, D. Adverse Drug Reactions: Power, harm reduction, regulation and the ADRe profile. Atlas Sci. 2020, 1–3. Available online: https://atlasofscience.org/adverse-drug-reactions-power-harm-reduction-regulation-and-the-adre-profile/ (accessed on 14 October 2020). [CrossRef]
- Hughes, D.; Jordan, M.; Logan, P.A.; Willson, A.; Snelgrove, S.; Storey, M.; Vaismoradi, M.; Jordan, S. Looking for the “Little Things”: A Multi-Disciplinary Approach to Medicines Monitoring for Older People Using the ADRe Resource. Geriatrics 2020, 5, 79. [Google Scholar] [CrossRef]
| Competency Category | Principles | Educational Strategy |
|---|---|---|
| Knowledge and skills | Selection of appropriate medications; Team work and interprofessional communication; Guidelines and policies; Rights of medicines management; Condition, dose and effectiveness of medications; Medication-taking history; Medication calculation and administration | Provision of opportunities to practice at bedside; Computer-based methods; High-fidelity simulation; Problem-based learning; Reflection and discussion; Supervision and role model; Case study learning |
| Independence and interdependence in decision making | Making independent clinical decisions; Feeling of responsibility; Linking between interventions and patient’s well-being; Double checking; Nurse-patient collaboration; Involvement of healthcare staff; Use of interprofessional communication tools; Valuing and respecting skills and responsibilities; Use of information technology | Self-reflection and criticism; Provision of controlled decision-making situations; Being mentored by clinical nurses; Provision of safe environment for the medication process; Interprofessional education; |
| Monitoring and follow up | Assessing care outcomes before, during and after medication; Monitoring abuse; Use of monitoring tools and profiles; | Monitoring patients for the signs and symptoms of known adverse side effects and reporting anything that may be related to the PRN medicine to pharmacists or prescribers. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vaismoradi, M.; Jordan, S.; Vizcaya-Moreno, F.; Friedl, I.; Glarcher, M. PRN Medicines Optimization and Nurse Education. Pharmacy 2020, 8, 201. https://doi.org/10.3390/pharmacy8040201
Vaismoradi M, Jordan S, Vizcaya-Moreno F, Friedl I, Glarcher M. PRN Medicines Optimization and Nurse Education. Pharmacy. 2020; 8(4):201. https://doi.org/10.3390/pharmacy8040201
Chicago/Turabian StyleVaismoradi, Mojtaba, Sue Jordan, Flores Vizcaya-Moreno, Ingrid Friedl, and Manela Glarcher. 2020. "PRN Medicines Optimization and Nurse Education" Pharmacy 8, no. 4: 201. https://doi.org/10.3390/pharmacy8040201
APA StyleVaismoradi, M., Jordan, S., Vizcaya-Moreno, F., Friedl, I., & Glarcher, M. (2020). PRN Medicines Optimization and Nurse Education. Pharmacy, 8(4), 201. https://doi.org/10.3390/pharmacy8040201









