The Pharmacy Game-GIMMICS® a Simulation Game for Competency-Based Education
Abstract
1. Introduction
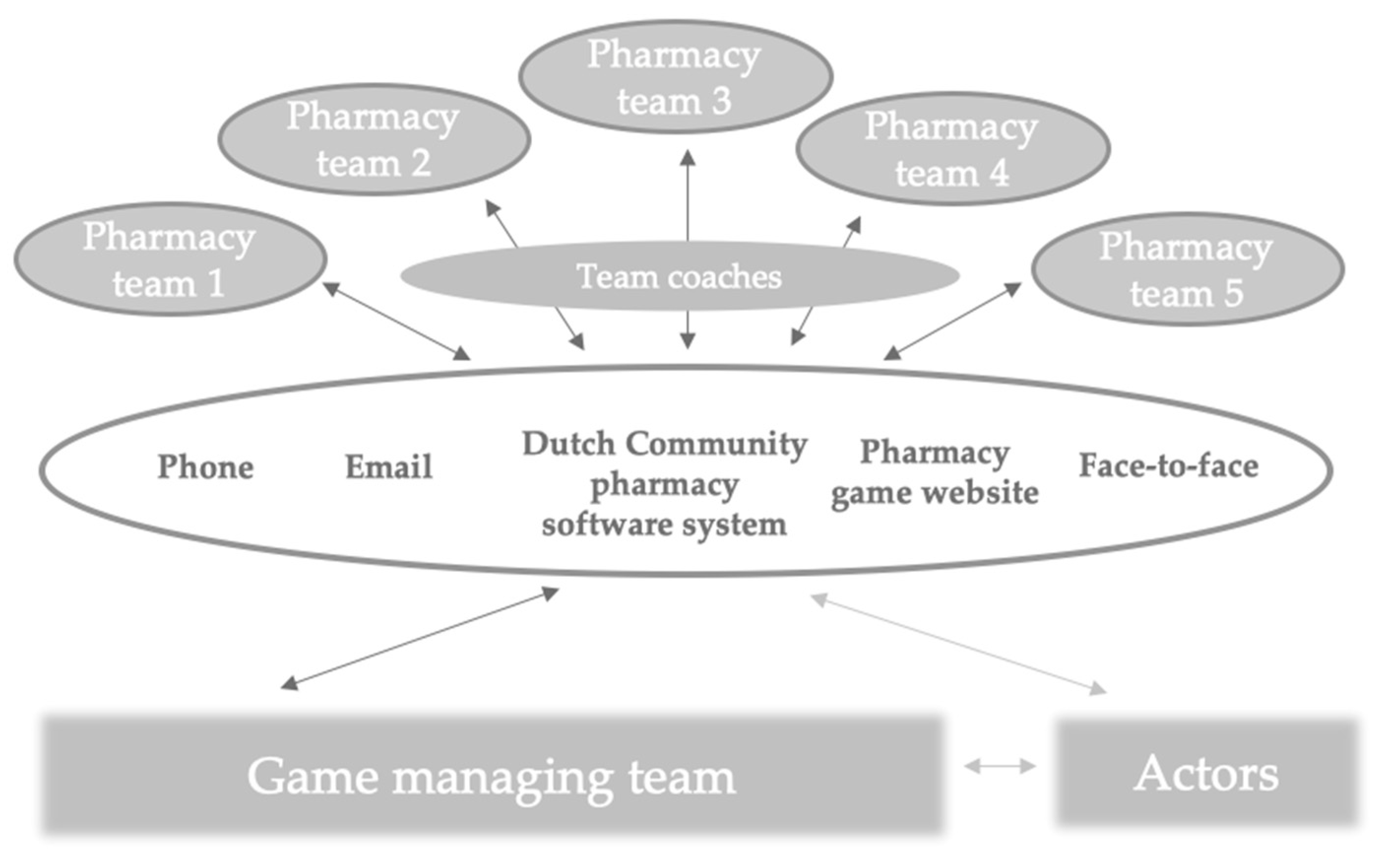
2. The Pharmacy Game, GIMMICS®
Game and Simulation Elements in the Pharmacy Game
3. Learning Goals and Activities
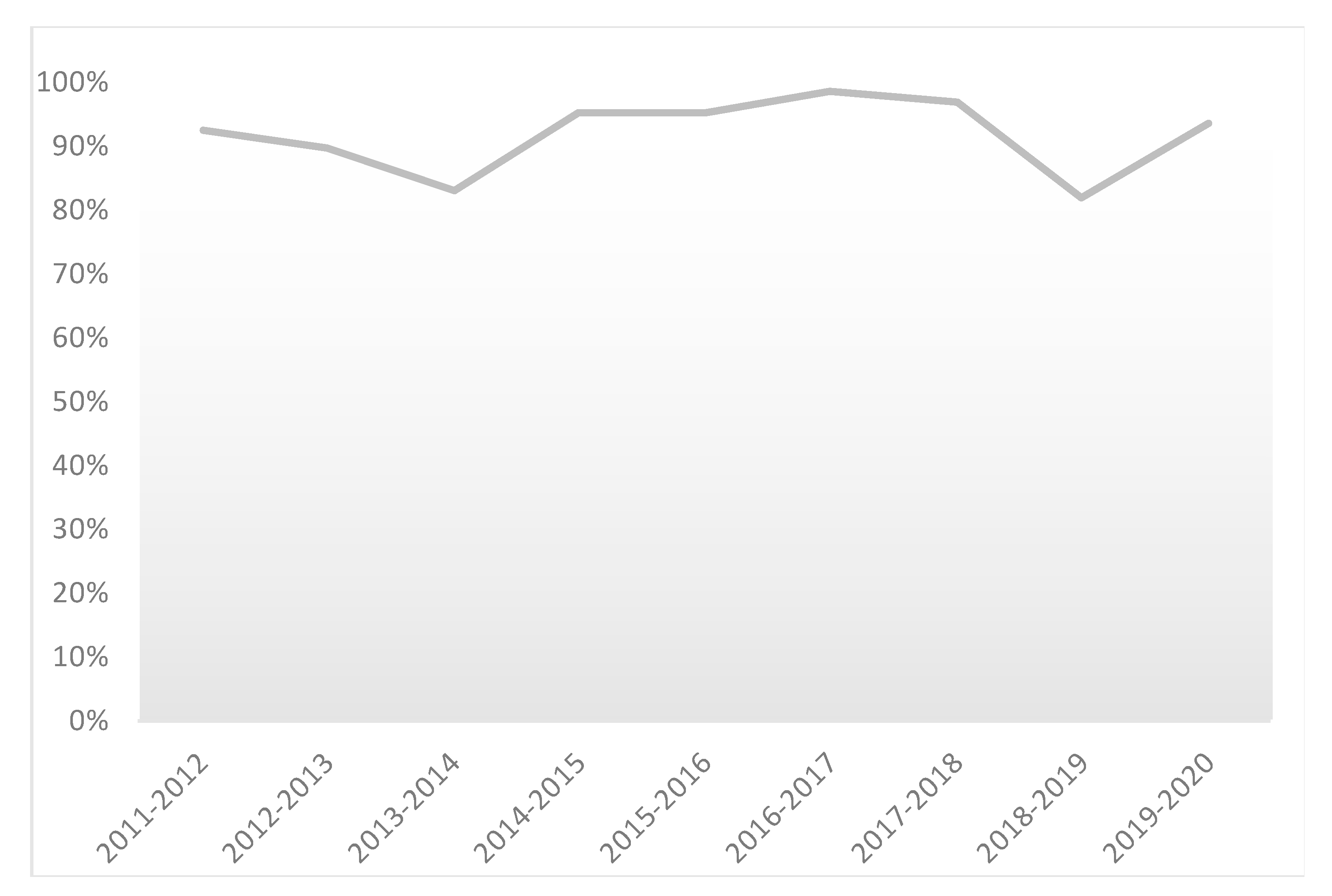
3.1. Learning Goals
3.1.1. Collaboration
3.1.2. Leadership
- Leading from a vision;
- Coaching and managing individuals;
- Taking responsibility;
- Entrepreneurship and innovation.
3.1.3. Communication
3.1.4. Pharmaceutical Expertise
3.2. Organizing the Practical Teaching
4. Assessments
4.1. Example of a Patient Case
4.1.1. The Case
4.1.2. The Assessment
5. Tools and Functionalities
5.1. Online Operational Tool
5.1.1. Case Management System (CAMS)
5.1.2. Actor Registration System (ARS)
5.1.3. Prescription Generator
6. Evaluation of the Pharmacy Game, GIMMICS® by Students
7. Discussion
8. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| Week | Game-Day | Type of Activity | Content |
|---|---|---|---|
| 1 | 1 | Study day | Introduction, mission and vision, business plan |
| 2 | Study day | Pharmacy information system | |
| 3 | Study day | Health insurance | |
| 4 | Study day | Preparations | |
| 5 | Study day | DiSC typology | |
| 2 | 6 | Practical day | Practicing day with open hour for questions |
| 7 | Study day | Financing, psychiatry and prescriptions | |
| 8 | Study day | Quality Management System | |
| 9 | Practical day | Official opening of the pharmacies | |
| 10 | Practical day | Prescriptions, cases, and quality Quality Management System in practice | |
| 3 | 11 | Practical day | Prescriptions and cases |
| 12 | Practical day | Prescriptions and cases | |
| 13 | Study day | Employment | |
| 14 | Practical day | Polypharmacy consultations, prescriptions, and case descriptions, and cases | |
| 15 | Study day | DiSC typology and teambuilding | |
| 4 | 16 | Study day | Leadership, euthanasia, medical devices |
| 17 | Practical day | Polypharmacy consultations, prescriptions, and cases | |
| 18 | Study day | Clinical pharmacy and mid-evaluation | |
| 19 | Practical day | Job interviews and terms of employment, prescriptions, and cases | |
| 20 | Practical day | Polypharmacy, prescriptions, and cases | |
| 5 | 21 | Practical day | Prescriptions and cases |
| 22 | Pharmacotherapeutic consultation | Euthanasia and privacy | |
| 23 | Practical day | Prescriptions and cases | |
| 24 | Final interview | Company representatives visit | |
| 25 | Self-reflection | Cases overview with the students and delivering the self-reflection |
References
- Wiedenmayer, K.; Summers, R.S.; Mackie, C.A.; Gous, A.G.S.; Everard, M. DEVELOPING PHARMACY PRACTICE—A FOCUS ON PATIENT CARE. HANDBOOK—2006 EDITION. 97; World Health Organization: Geneva, Switzerland; International Pharmaceutical Federation: The Hague, The Netherlands, 2006. [Google Scholar]
- Dent, J.A.; Harden, R.M. A Practical Guide for Medical Teachers; Churchill Livingstone: London, UK; Elsevier: New York, NY, USA, 2013. [Google Scholar]
- David, A. Kolb, Experiential Learning: Experience as the Source of Learning and Development. Available online: https://b-ok.cc/book/3508789/beb71f (accessed on 18 August 2020).
- Katajavuori, N.; Salminen, O.; Vuorensola, K.; Huhtala, H.; Vuorela, P.; Hirvonen, J. Competence-Based Pharmacy Education in the University of Helsinki. Pharmacy 2017, 5, 29. [Google Scholar] [CrossRef] [PubMed]
- Croft, H.; Gilligan, C.; Rasiah, R.; Levett-Jones, T.; Schneider, J. Current Trends and Opportunities for Competency Assessment in Pharmacy Education-A Literature Review. Pharmacy 2019, 7, 67. [Google Scholar] [CrossRef] [PubMed]
- Koster, A.; Schalekamp, T.; Meijerman, I. Implementation of Competency-Based Pharmacy Education (CBPE). Pharmacy 2017, 5, 10. [Google Scholar] [CrossRef] [PubMed]
- Katoue, M.G.; Schwinghammer, T.L. Competency-based education in pharmacy: A review of its development, applications, and challenges. J. Eval. Clin. Pract. 2020, 26, 1114–1123. [Google Scholar] [CrossRef] [PubMed]
- Volmer, D.; Sepp, K.; Veski, P.; Raal, A. The Implementation of Pharmacy Competence Teaching in Estonia. Pharmacy 2017, 5, 18. [Google Scholar] [CrossRef] [PubMed]
- Stupans, I.; Atkinson, J.; Meštrović, A.; Nash, R.; Rouse, M.J. A Shared Focus: Comparing the Australian, Canadian, United Kingdom and United States Pharmacy Learning Outcome Frameworks and the Global Competency Framework. Pharmacy 2016, 4, 26. [Google Scholar] [CrossRef] [PubMed]
- Westein, M.P.D.; de Vries, H.; Floor, A.; Koster, A.S.; Buurma, H. Development of a Postgraduate Community Pharmacist Specialization Program Using CanMEDS Competencies, and Entrustable Professional Activities. Am. J. Pharm. Educ. 2019, 83. [Google Scholar] [CrossRef]
- Koster, A.S.; Mantel-Teeuwisse, A.K.; Woerdenbag, H.J.; Mulder, W.M.C.; Wilffert, B.; Schalekamp, T.; Buurma, H.; Wilting, I.; Westein, M.P. Alignment of CanMEDS-Based Undergraduate and Postgraduate Pharmacy Curricula in The Netherlands. Pharmacy 2020, 8, 117. [Google Scholar] [CrossRef]
- Cravens, M.G.; Benner, K.; Beall, J.; Worthington, M.; Denson, B.; Youngblood, A.Q.; Zinkan, J.L.; Tofil, N.M. Knowledge Gain of Pharmacy Students and Pharmacists Comparing Simulation Versus Traditional Learning Methodology. J. Pediatr. Pharmacol. Ther. 2016, 21, 476–485. [Google Scholar] [CrossRef]
- Akl, E.A.; Kairouz, V.F.; Sackett, K.M.; Erdley, W.S.; Mustafa, R.A.; Fiander, M.; Gabriel, C.; Schünemann, H. Educational games for health professionals. Cochrane Database Syst. Rev. 2013, 3, CD006411. [Google Scholar]
- Kayyali, R.; Harrap, N.; Albayaty, A.; Savickas, V.; Hammell, J.; Hyatt, F.; Elliott, K.; Richardson, S. Simulation in pharmacy education to enhance interprofessional education. Int. J. Pharm. Pract. 2019, 27, 295–302. [Google Scholar] [CrossRef] [PubMed]
- Kane-Gill, S.L.; Smithburger, P.L. Transitioning knowledge gained from simulation to pharmacy practice. Am. J. Pharm. Educ. 2011, 75, 210. [Google Scholar] [CrossRef]
- Komperda, K.; Lempicki, K. Effectiveness of a Medication Reconciliation Simulation in an Introductory Pharmacy Practice Experience Course. Am. J. Pharm. Educ. 2019, 83, 6628. [Google Scholar] [CrossRef]
- Lin, K.; Travlos, D.V.; Wadelin, J.W.; Vlasses, P.H. Simulation and introductory pharmacy practice experiences. Am. J. Pharm. Educ. 2011, 75, 209. [Google Scholar] [CrossRef]
- Lucas, C.; Williams, K.; Bajorek, B. Virtual Pharmacy Programs to Prepare Pharmacy Students for Community and Hospital Placements. Am. J. Pharm. Educ. 2019, 83, 7011. [Google Scholar] [CrossRef]
- Tait, L.; Lee, K.; Rasiah, R.; Cooper, J.M.; Ling, T.; Geelan, B.; Bindoff, I. Simulation and Feedback in Health Education: A Mixed Methods Study Comparing Three Simulation Modalities. Pharmacy 2018, 6, 41. [Google Scholar] [CrossRef]
- Vyas, D.; Bray, B.S.; Wilson, M.N. Use of simulation-based teaching methodologies in US colleges and schools of pharmacy. Am. J. Pharm. Educ. 2013, 77, 53. [Google Scholar] [CrossRef]
- Gaba, D.M. The future vision of simulation in health care. BMJ Qual. Saf. 2004, 13 (Suppl. 1), i2–i10. [Google Scholar] [CrossRef]
- Okuda, Y.; Bryson, E.O.; DeMaria Jr, S.; Jacobson, L.; Quinones, J.; Shen, B.; Levine, A.I. The utility of simulation in medical education: What is the evidence? Mt. Sinai J. Med. 2009, 76, 330–343. [Google Scholar] [CrossRef] [PubMed]
- Bajis, D.; Chaar, B.; Basheti, I.A.; Moles, R. Pharmacy students’ medication history taking competency: Simulation and feedback learning intervention. Curr. Pharm. Teach. Learn. 2019, 11, 1002–1015. [Google Scholar] [CrossRef]
- Fejzic, J.; Barker, M.; Hills, R.; Priddle, A. Communication Capacity Building through Pharmacy Practice Simulation. Am. J. Pharm. Educ. 2016, 80, 28. [Google Scholar] [CrossRef][Green Version]
- Blanié, A.; Amorim, M.-A.; Benhamou, D. Comparative value of a simulation by gaming and a traditional teaching method to improve clinical reasoning skills necessary to detect patient deterioration: A randomized study in nursing students. BMC Med. Educ. 2020, 20, 53. [Google Scholar] [CrossRef]
- Kuipers, D.A.; Terlouw, G.; Wartena, B.O.; van ’t Veer, J.T.; Prins, J.T.; Pierie, J.P.E. The Role of Transfer in Designing Games and Simulations for Health: Systematic Review. JMIR Serious Games 2017, 5. [Google Scholar] [CrossRef]
- Bedwell, W.L.; Pavlas, D.; Heyne, K.; Lazzara, E.H.; Salas, E. Toward a Taxonomy Linking Game Attributes to Learning: An Empirical Study. Simul. Gaming 2012. [Google Scholar] [CrossRef]
- Cain, J.; Piascik, P. Are Serious Games a Good Strategy for Pharmacy Education? Am. J. Pharm. Educ. 2015, 79, 47. [Google Scholar] [CrossRef]
- Gorbanev, I.; Agudelo-Londoño, S.; González, R.A.; Cortes, A.; Pomares, A.; Delgadillo, V.; Yepes, F.J.; Muñoz, Ó. A systematic review of serious games in medical education: Quality of evidence and pedagogical strategy. Med. Educ. Online 2018, 23, 1438718. [Google Scholar] [CrossRef]
- Graafland, M.; Schraagen, J.M.; Schijven, M.P. Systematic review of serious games for medical education and surgical skills training. Br. J. Surg. 2012, 99, 1322–1330. [Google Scholar] [CrossRef]
- Gleason, B.L.; Peeters, M.J.; Resman-Targoff, B.H.; Karr, S.; McBane, S.; Kelley, K.; Thomas, T.; Denetclaw, T.H. An active-learning strategies primer for achieving ability-based educational outcomes. Am. J. Pharm. Educ. 2011, 75, 186. [Google Scholar] [CrossRef]
- van der Werf, J.; Dekens-Konter, J.; Brouwers, J. A new model for teaching Pharmaceutical Care Services Management. Pharm. Educ. 2004. [Google Scholar] [CrossRef]
- Cavenett, S. Creating a learning environment using game development. AAEE 2016: The changing role of the engineering educator for developing the future engineer. In Proceedings of the 27th Australasian Association for Engineering Education Conference, Coffs Harbour, Australia, 4–7 December 2016; pp. 1–12. [Google Scholar]
- Jarvis, P. Adult Learning in the Social Context; Taylor & Francis: Oxfordshire, UK, 2012. [Google Scholar]
- Sillius, A. Gimmics: How to Organize, Manage and Control a Pharmacy Practice Game; Science Education and Communication: Groningen, The Netherlands, 2005. [Google Scholar]
- Franklyn-Stokes, A.; Newstead, S.E. Undergraduate cheating: Who does what and why? Stud. High. Educ. 1995, 20, 159–172. [Google Scholar] [CrossRef]
- Fuqua, R.M.; Bryan, J. The Psychology of Leadership Selection: DiSC Results and Leadership Success in Health Care. Adv. Soc. Sci. Res. J. 2017, 4. [Google Scholar] [CrossRef]
- Mengel, T. Outcome-based project management education for emerging leaders—A case study of teaching and learning project management. Int. J. Proj. Manag. 2008, 26, 275–285. [Google Scholar] [CrossRef]
- Hasan, S.; Hilal, D.A. Enhancing Student Communication Skills Through Arabic Language Competency and Simulated Patient Assessments. Am. J. Pharm. Educ. 2017, 81. [Google Scholar] [CrossRef] [PubMed]
- Folmer, H. Dysmenorroe. NHG-Richtlijnen. 2004. Available online: https://richtlijnen.nhg.org/behandelrichtlijnen/dysmenorroe (accessed on 30 August 2020).
- Nederland, Z. Ibuprofen. Available online: https://www.farmacotherapeutischkompas.nl/bladeren/preparaatteksten/i/ibuprofen (accessed on 30 August 2020).
- Noble, C.; Coombes, I.; Nissen, L.; Shaw, P.N.; Clavarino, A. Making the transition from pharmacy student to pharmacist: Australian interns’ perceptions of professional identity formation. Int. J. Pharm. Pract. 2015, 23, 292–304. [Google Scholar] [CrossRef] [PubMed]
- Hirsch, A.C.; Parihar, H.S. A capstone course with a comprehensive and integrated review of the pharmacy curriculum and student assessment as a preparation for advanced pharmacy practice experiences. Am. J. Pharm. Educ. 2014, 78, 192. [Google Scholar] [CrossRef]
- Khan, K.Z.; Ramachandran, S.; Gaunt, K.; Pushkar, P. The Objective Structured Clinical Examination (OSCE): AMEE Guide No. 81. Part I: An historical and theoretical perspective. Med. Teach 2013, 35, e1437–e1446. [Google Scholar] [CrossRef]
- Davies, J.G.; Ciantar, J.; Jubraj, B.; Bates, I.P. Use of a multisource feedback tool to develop pharmacists in a postgraduate training program. Am. J. Pharm. Educ. 2013, 77, 52. [Google Scholar] [CrossRef]
- Patel, J.P.; Sharma, A.; West, D.; Bates, I.P.; Davies, J.G.; Abdel-Tawab, R. An evaluation of using multi-source feedback (MSF) among junior hospital pharmacists. Int. J. Pharm. Pract. 2011, 19, 276–280. [Google Scholar] [CrossRef]
- Tochel, C.; Haig, A.; Hesketh, A.; Cadzow, A.; Beggs, K.; Colthart, I.; Peacock, H. The effectiveness of portfolios for post-graduate assessment and education: BEME Guide No 12. Med. Teach. 2009, 31, 299–318. [Google Scholar] [CrossRef]
- Jarrett, J.B.; Berenbrok, L.A.; Goliak, K.L.; Meyer, S.M.; Shaughnessy, A.F. Entrustable Professional Activities as a Novel Framework for Pharmacy Education. Am. J. Pharm. Educ. 2018, 82, 6256. [Google Scholar] [CrossRef]
- Hattie, J.; Timperley, H. The Power of Feedback. Rev. Educ. Res. 2007, 77, 81–112. [Google Scholar] [CrossRef]
- Miller, G.E. The assessment of clinical skills/competence/performance. Acad. Med. 1990, 65 (Suppl. 9), S63–S67. [Google Scholar] [CrossRef] [PubMed]
- Albarqouni, L.; Hoffmann, T.; Glasziou, P. Evidence-based practice educational intervention studies: A systematic review of what is taught and how it is measured. BMC Med. Educ. 2018, 18. [Google Scholar] [CrossRef]
| Learning Goal | Examples of Activities from the Game |
|---|---|
| Collaboration |
|
| Leadership |
|
| Communication |
|
| Pharmaceutical expertise |
|
| Individual Score Activity | Points/Patients | Competence | Frequency/Quantity |
|---|---|---|---|
| Communication with GP | +/−20 | 2 | 3–4 assignments per student 2 GPs, 2 h/day each (11 days) |
| Actor (counter, telephone, email) | +/−40 | 1 & 2 | 5–6 assignments per student 3 actors, 2-3 h case/day (11 days, 33 cases) |
| Euthanasia case requested | +/−20 | 2 | 1 student in each pharmacy addresses the GP request for euthanasia |
| Euthanasia case proceed | +/−40 | 1 & 2 | 1 student in each pharmacy attends the GP when coming to collect the euthanasia and discuss final advice |
| Case “auction” | +/−40 | 1 & 2 | 1 student in each pharmacy order (form a fictional foundation in Pildorp) materials, such as inhalation, wound care, homeopathy, phytotherapy, and other products that are fitting the mission/vision of their pharmacy |
| Evening-, night-, and weekend-service case | +/−40 | 1 & 2 | 2 students in each pharmacy and each pharmacy is called twice |
| Medication review patient—meeting 1 (patient) | +/−20 | 2 | 1 student in each pharmacy does medication review in communication with a patient |
| Medication review patient—meeting 2/3 (GP/patient) | +/−40 | 1 & 2 | 1 student in each pharmacy does medication review in communication with GP, and once more in communication with a patient |
| Team score activity | |||
| Working on prescriptions | +/−60 | 1 | 30-40 prescriptions per pharmacy/day (11 days) |
| Writing business plan | +/−100 | 3 & 4 | Once |
| Writing annual report | +/−100 | 3 & 4 | Once |
| Pharmacy opening | +/−40 | 3 & 4 | Once |
| Innovation project | +100 | 3 & 4 | The insurance company of the inhabitants of Pildorp (represented by real pharmacist or entrepreneur) can give one pharmacy a prize of maximum +100 points, for best innovative health-project |
| Quality; risk-analyses | +/−40 | 3 & 4 | Once, the students should perform a risk analysis to increase pharmacy quality. This is done using the quality management system |
| Quality; intern audit self-care/pharmacy-based preparations | +/−40 | 3 & 4 | Once, over self-care and once over pharmacy-based preparations. The student assesses the procedure in the pharmacy in these fields using the quality management system and records data over adherence to the requirements |
| Quality; use of the quality management system | +/−1 | 3 & 4 | Once, gaining 1 point if registering a fault, complain, or a compliment in the quality management system |
| Quality; complaints and errors analysis | +/−40 | 3 & 4 | Once, students should analyze the errors/complaints/compliments with an indication for possible policy change and further needed actions in that regard |
| Vacancy text | +/−40 | 2 & 3 | Once, placing a vacancy for a pharmacy assistant/technician |
| Job interviews | +/−60 | 4 | Once, interviewing a new potential pharmacy assistant/technician |
| PAE | +/−40 | 1 | Optional activity, students may choose from various lectures to attend and gain points for “keeping their licenses” |
| FTO preparation | +/−20 | 3 & 4 | Once, students prepare for the pharmacotherapeutic consultation with GPs |
| FTO content | +/−40 | 1 | Once, consultation-content assessed |
| FTO presentation/execution | +/−40 | 3 & 4 | Once, students attending and actively participating the pharmacotherapeutic consultation with the GPs |
| FTO minutes | +/−20 | 2 | Once, students should provide minutes from the meeting |
| Speed dates | +/−40 | 3 & 4 | Once, student’s meeting with pharmacy-chain representatives |
| Small project | +/−40 | 3 & 4 | Individual-pharmacy projects: Ramadan in the pharmacy, an injection day for diabetics, an information evening for pregnant women, etc. |
| Big project | +/−100 | 3 & 4 | Activities requiring project management: cooperation with a nursing home, cooperation with an asylum seekers’ center, etc. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fens, T.; Dantuma-Wering, C.M.; Taxis, K. The Pharmacy Game-GIMMICS® a Simulation Game for Competency-Based Education. Pharmacy 2020, 8, 198. https://doi.org/10.3390/pharmacy8040198
Fens T, Dantuma-Wering CM, Taxis K. The Pharmacy Game-GIMMICS® a Simulation Game for Competency-Based Education. Pharmacy. 2020; 8(4):198. https://doi.org/10.3390/pharmacy8040198
Chicago/Turabian StyleFens, Tanja, Claudia M. Dantuma-Wering, and Katja Taxis. 2020. "The Pharmacy Game-GIMMICS® a Simulation Game for Competency-Based Education" Pharmacy 8, no. 4: 198. https://doi.org/10.3390/pharmacy8040198
APA StyleFens, T., Dantuma-Wering, C. M., & Taxis, K. (2020). The Pharmacy Game-GIMMICS® a Simulation Game for Competency-Based Education. Pharmacy, 8(4), 198. https://doi.org/10.3390/pharmacy8040198






