The Consequences of General Medication Beliefs Measured by the Beliefs about Medicine Questionnaire on Medication Adherence: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Inclusion Criteria
2.2. Exclusion Criteria
2.3. Study Selection
2.4. Data Extraction Process
2.5. Risk of Bias in Individual Studies
3. Results
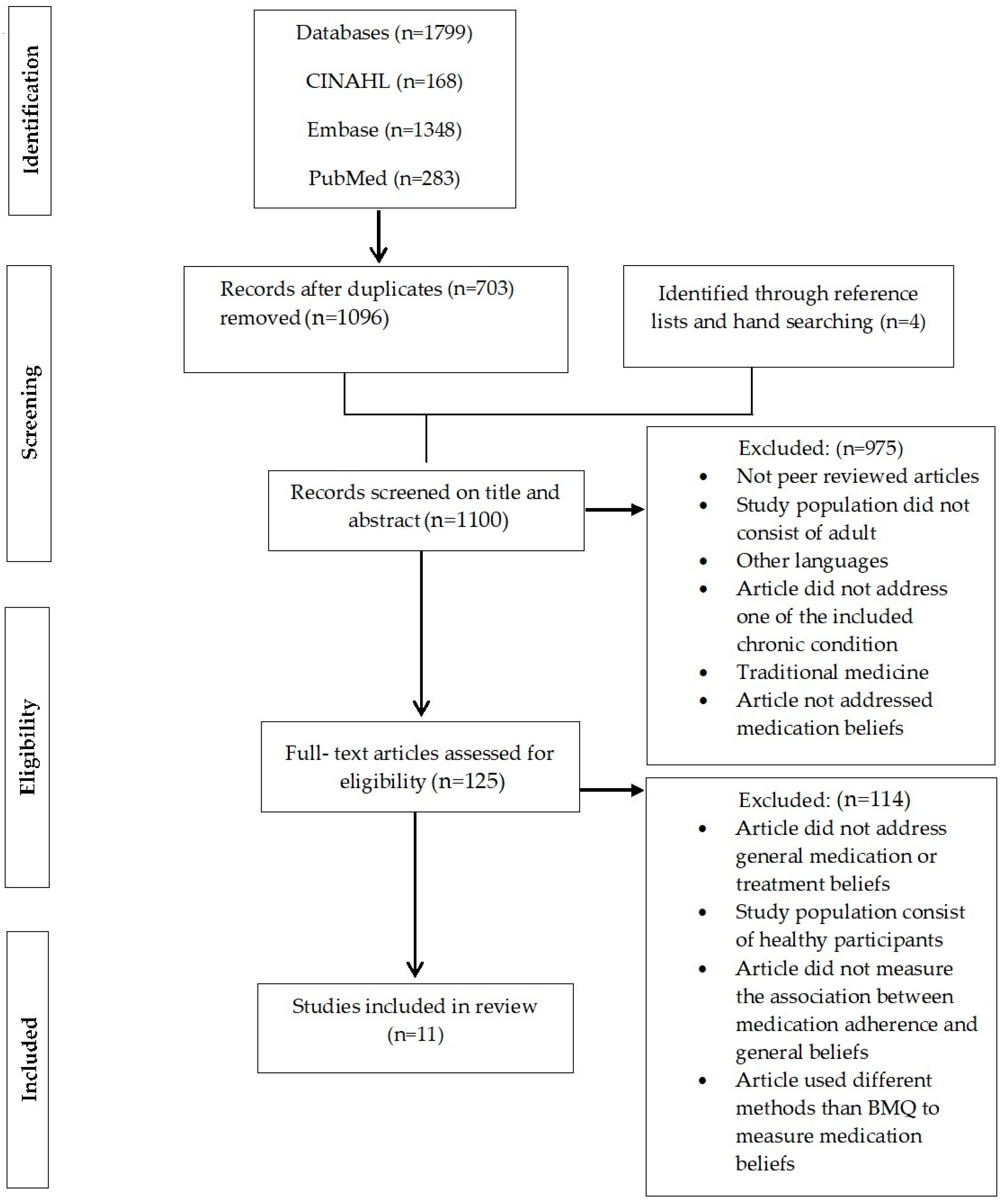
3.1. Article Selection
3.2. Risk of Bias across Studies
3.3. Tools Used to Measure Medication Adherence
3.4. Findings of Individual Studies
3.4.1. General-Harm
3.4.2. General-Overuse
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Australian Institute for Health and Welfare. Chronic Disease—Australia’s Biggest Health Challenge. 2014. Available online: https://www.aihw.gov.au/getmedia/8f7bd3d6-9e69-40c1-b7a8-40dca09a13bf/4_2-chronic-disease.pdf.aspx (accessed on 4 January 2020).
- Lemay, J.; Waheedi, M.; Al-Sharqawi, S.; Bayoud, T. Medication adherence in chronic illness: Do beliefs about medications play a role? Patient Prefer. Adherence 2018, 12, 1687–1698. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. Adherence to Long-Term Therapies:Evidence for Action. Available online: https://apps.who.int/medicinedocs/pdf/s4883e/s4883e.pdf (accessed on 9 January 2020).
- Presley, B.; Groot, W.; Pavlova, M. Pharmacy-led interventions to improve medication adherence among adults with diabetes: A systematic review and meta-analysis. Res. Soc. Adm. Pharm. 2019, 15, 1057–1067. [Google Scholar] [CrossRef] [PubMed]
- Bae, S.G.; Kam, S.; Park, K.S.; Kim, K.Y.; Hong, N.S.; Kim, K.S.; Lee, Y.M.; Lee, W.K.; Choe, M.S.P. Factors related to intentional and unintentional medication nonadherence in elderly patients with hypertension in rural community. Patient Prefer. Adherence 2016, 10, 1979–1989. [Google Scholar] [CrossRef]
- Horne, R.; Chapman, S.C.E.; Parham, R.; Freemantle, N.; Forbes, A.; Cooper, V. Understanding patients’ adherence-related beliefs about medicines prescribed for long-term conditions: A meta-analytic review of the necessity-concerns framework. PLoS ONE 2013, 8, e80633. [Google Scholar] [CrossRef] [PubMed]
- Horne, R.; Weinman, J. Patients’ beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illness. J. Psychosom. Res. 1999, 47, 555–567. [Google Scholar] [CrossRef]
- McQuaid, E.L.; Landier, W. Cultural issues in medication adherence: Disparities and directions. J. Gen. Intern. Med. 2018, 33, 200–206. [Google Scholar] [CrossRef] [PubMed]
- Hsiao, C.Y.; Chang, C.; Chen, C.D. An investigation on illness perception and adherence among hypertensive patients. Kaohsiung J. Med. Sci. 2012, 28, 442–447. [Google Scholar] [CrossRef]
- Mann, D.M.; Ponieman, D.; Leventhal, H.; Halm, E.A. Predictors of adherence to diabetes medications: The role of disease and medication beliefs. J. Behav. Med. 2009, 32, 278–284. [Google Scholar] [CrossRef]
- Krauskopf, K.; Federman, A.D.; Kale, M.S.; Sigel, K.M.; Martynenko, M.; O’Conor, R.; Wolf, M.S.; Leventhal, H.; Wisnivesky, J.P. Chronic obstructive pulmonary disease illness and medication beliefs are associated with medication adherence. COPD 2015, 12, 151–164. [Google Scholar] [CrossRef]
- Feehan, M.; Ranker, L.; Durante, R.; Cooper, D.K.; Jones, G.J.; Young, D.C.; Munger, M.A. Adherence to controller asthma medications: 6-month prevalence across a US community pharmacy chain. J. Clin. Pharm. Ther. 2015, 40, 590–593. [Google Scholar] [CrossRef]
- Foot, H.; La Caze, A.; Gujral, G.; Cottrell, N. The necessity–concerns framework predicts adherence to medication in multiple illness conditions: A meta-analysis. Patient Educ. Counsel. 2016, 99, 706–717. [Google Scholar] [CrossRef] [PubMed]
- Gatt, I.; West, L.M.; Calleja, N.; Briffa, C.; Cordina, M. Psychometric properties of the belief about medicines questionnaire (BMQ) in the Maltese language. Pharm. Pract. 2017, 15, 886. [Google Scholar] [CrossRef]
- Horne, R.; Graupner, L.d.; Frost, S.; Weinman, J.; Wright, S.M.; Hankins, M. Medicine in a multi-cultural society: The effect of cultural background on beliefs about medications. Soc. Sci. Med. 2004, 59, 1307–1313. [Google Scholar] [CrossRef] [PubMed]
- Andersson, K.; Jonsson, A.K. Beliefs about medicines are strongly associated with medicine-use patterns among the general population. Int. J. Clin. Pract. 2016, 70, 277–285. [Google Scholar] [CrossRef]
- Gast, A.; Mathes, T. Medication adherence influencing factors—An (updated) overview of systematic reviews. Syst. Rev. 2019, 8, 112. [Google Scholar] [CrossRef] [PubMed]
- Shahin, W.; Kennedy, G.A.; Stupans, I. The impact of personal and cultural beliefs on medication adherence of patients with chronic illnesses: A systematic review. Patient Prefer. Adherence 2019, 13, 1019–1035. [Google Scholar] [CrossRef]
- Hsu, C.; Lemon, J.M.; Wong, E.S.; Carson-Cheng, E.; Perkins, M.; Nordstrom, M.S.; Liu, C.-F.; Sprague, C.; Bryson, C.L. Factors affecting medication adherence: Patient perspectives from five veterans affairs facilities. BMC Health Serv. Res. 2014, 14, 533. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann. Intern. Med. 2009, 151, 264–269. [Google Scholar] [CrossRef]
- Hong, Q.N.; Fàbregues, S.; Bartlett, G.; Boardman, F.; Cargo, M.; Dagenais, P.; Gagnon, M.P.; Griffiths, F.; Nicolau, B.; O’Cathain, A.; et al. The mixed methods appraisal tool (MMAT) version 2018 for information professionals and researchers. Educ. Inf. 2018, 34, 285–291. [Google Scholar] [CrossRef]
- Coyne, E.; Rands, H.; Frommolt, V.; Kain, V.; Plugge, M.; Mitchell, M. Investigation of blended learning video resources to teach health students clinical skills: An integrative review. Nurs. Educ. Today 2018, 63, 101–107. [Google Scholar] [CrossRef]
- Fischer, W.; Brandstetter, S.; Brandl, M.; Finger, T.; Bohmer, M.M.; Pfeifer, M.; Apfelbacher, C. Specific, but not general beliefs about medicines are associated with medication adherence in patients with COPD, but not asthma: Cohort study in a population of people with chronic pulmonary disease. J. Psychosom. Res. 2018, 107, 46–52. [Google Scholar] [CrossRef] [PubMed]
- Pereira, M.D.G.; Ferreira, G.; Machado, J.C.; Pedras, S. Beliefs about medicines as mediators in medication adherence in type 2 diabetes. Int. J. Nurs. Pract. 2019, 25, e12768. [Google Scholar] [CrossRef] [PubMed]
- Olorunfemi, O.; Ojewole, F. Medication belief as correlate of medication adherence among patients with diabetes in Edo State, Nigeria. Nurs. Open 2019, 6, 197–202. [Google Scholar] [CrossRef] [PubMed]
- Yousefabadi, S.R.; Arbabshastan, M.E.; Sarani, A.; Rigi, K. Why medication adherence in hypertensive patients? Drug Invent. Today 2018, 10, 651–658. [Google Scholar]
- Sweileh, W.M.; Zyoud, S.H.; Abu Nab’a, R.J.; Deleq, M.I.; Enaia, M.I.; Nassar, S.M.; Al-Jabi, S.W. Influence of patients’ disease knowledge and beliefs about medicines on medication adherence: Findings from a cross-sectional survey among patients with type 2 diabetes mellitus in Palestine. BMC Public Health 2014, 14, 94. [Google Scholar] [CrossRef]
- Ross, S.; Walker, A.; MacLeod, M.J. Patient compliance in hypertension: Role of illness perceptions and treatment beliefs. J. Hum. Hypertens. 2004, 18, 607–613. [Google Scholar] [CrossRef]
- Wilhelm, M.; Rief, W.; Doering, B.K. It’s all a matter of necessity and concern: A structural equation model of adherence to antihypertensive medication. Patient Educ. Couns. 2018, 101, 497–503. [Google Scholar] [CrossRef]
- Wei, L.; Champman, S.; Li, X.; Li, X.; Li, S.; Chen, R.; Bo, N.; Chater, A.; Horne, R. Beliefs about medicines and non-adherence in patients with stroke, diabetes mellitus and rheumatoid arthritis: A cross-sectional study in China. BMJ Open 2017, 7, e017293. [Google Scholar] [CrossRef]
- Rajpura, J.; Nayak, R. Medication adherence in a sample of elderly suffering from hypertension: Evaluating the influence of illness perceptions, treatment beliefs, and illness burden. J. Manag. Care Pharm. JMCP 2014, 20, 58–65. [Google Scholar] [CrossRef]
- Al-Ruthia, Y.; Hong, S.; Graff, C.; Kocak, M.; Solomon, D.; Nolly, R. Examining the relationship between antihypertensive medication satisfaction and adherence in older patients. Res. Soc. Adm. Pharm. 2017, 13, 602–613. [Google Scholar] [CrossRef]
- Stewart, D.W.; DePue, J.; Rosen, R.K.; Bereolos, N.; Goldstein, M.G.; Tuitele, J.; Nu’usolia, O.; McGarvey, S.T. Medication-taking beliefs and diabetes in American Samoa: A qualitative inquiry. Transl. Behav. Med. 2012, 3, 30–38. [Google Scholar] [CrossRef] [PubMed]
- Kumar, K.; Greenfield, S.; Raza, K.; Gill, P.; Stack, R. Understanding adherence-related beliefs about medicine amongst patients of South Asian origin with diabetes and cardiovascular disease patients: A qualitative synthesis. BMC Endocr. Disord. 2016, 16, 24. [Google Scholar] [CrossRef] [PubMed]
- Welz, A.N.; Emberger-Klein, A.; Menrad, K. The importance of herbal medicine use in the German health-care system: Prevalence, usage pattern, and influencing factors. BMC Health Serv. Res. 2019, 19, 952. [Google Scholar] [CrossRef] [PubMed]
- AlRawi, S.N.; Khidir, A.; Elnashar, M.S.; Abdelrahim, H.A.; Killawi, A.K.; Hammoud, M.M.; Fetters, M.D. Traditional Arabic & Islamic medicine: Validation and empirical assessment of a conceptual model in Qatar. BMC Complement. Altern. Med. 2017, 17, 157. [Google Scholar] [CrossRef]
- Horne, R. Patients’ beliefs about treatment: The hidden determinant of treatment outcome? J. Psychosom. Res. 1999, 47, 491–495. [Google Scholar] [CrossRef]
- Algier, L.A.; Hanoglu, Z.; Özden, G.; Kara, F. The use of complementary and alternative (non-conventional) medicine in cancer patients in Turkey. Eur. J. Oncol. Nurs. 2005, 9, 138–146. [Google Scholar] [CrossRef]
- Jimmy, B.; Jose, J. Patient medication adherence: Measures in daily practice. Oman Med. J. 2011, 26, 155–159. [Google Scholar] [CrossRef]
- Hong, S.H. Potential for physician communication to build favorable medication beliefs among older adults with hypertension: A cross-sectional survey. PLoS ONE 2019, 14, e0210169. [Google Scholar] [CrossRef]
- Tucker, J.D.; Cheng, Y.; Wong, B.; Gong, N.; Nie, J.-B.; Zhu, W.; McLaughlin, M.M.; Xie, R.; Deng, Y.; Huang, M.; et al. Patient–physician mistrust and violence against physicians in Guangdong Province, China: A qualitative study. BMJ Open 2015, 5, e008221. [Google Scholar] [CrossRef]
- Ruksakulpiwat, S.; Liu, Z.; Yue, S.; Fan, Y. The association among medication beliefs, perception of illness and medication adherence in ischemic stroke patients: A cross-sectional study in China. Patient Prefer. Adherence 2020, 14, 235–247. [Google Scholar] [CrossRef]
- Epstein, R.M.; Franks, P.; Fiscella, K.; Shields, C.G.; Meldrum, S.C.; Kravitz, R.L.; Duberstein, P.R. Measuring patient-centered communication in patient–physician consultations: Theoretical and practical issues. Soc. Sci. Med. 2005, 61, 1516–1528. [Google Scholar] [CrossRef] [PubMed]
- Aflakseir, A. Role of illness and medication perceptions on adherence to medication in a group of Iranian patients with type 2 diabetes. J. Diabetes 2012, 4, 243–247. [Google Scholar] [CrossRef]
- Morgado, M.; Rolo, S. Factors influencing medication adherence and hypertension management revisited: Recent insights from cancer survivors. Hypertens. Res. 2012, 35, 894–896. [Google Scholar] [CrossRef] [PubMed]
- Cea-Calvo, L.; Marín-Jiménez, I.; de Toro, J.; Fuster-RuizdeApodaca, M.J.; Fernández, G.; Sánchez-Vega, N.; Orozco-Beltrán, D. Association between non-adherence behaviors, patients’ experience with healthcare and beliefs in medications: A survey of patients with different chronic conditions. Curr. Med. Res. Opin. 2019. [Google Scholar] [CrossRef] [PubMed]
- Bussell, J.K.; Cha, E.; Grant, Y.E.; Schwartz, D.D.; Young, L.A. Ways health care providers can promote better medication adherence. Clin. Diabetes 2017, 35, 171–177. [Google Scholar] [CrossRef] [PubMed]
- Putsch, R.W., III; Joyce, M. Dealing with patients from other cultures. In Clinical Methods: The History, Physical, and Laboratory Examinations, 3rd ed.; Walker, H.K., Hall, W.D., Hurst, J.W., Eds.; Butterworths: Boston, MA, USA, 1990. Available online: https://www.ncbi.nlm.nih.gov/books/NBK340/ (accessed on 5 January 2020).
| Database | Search Terms |
|---|---|
| PubMed | (((((hypertension) OR (diabetes mellitus)) OR (asthma)) OR (chronic obstructive pulmonary disease)) AND (((((overuse beliefs) OR (harm beliefs)) OR (beliefs about medicine questionnaire)) OR (medication beliefs)) OR (general beliefs))) AND ((medication compliance [MeSH Terms]) OR (medication adherence [MeSH Terms])) |
| CINAHL with full text | beliefs about medicine questionnaire OR medication beliefs OR therapeutic beliefs OR overuse beliefs OR harm beliefs AND ((drug OR therapeutic OR medication)) AND (compliance OR adherence OR persistence)) AND ((chronic obstructive pulmonary disease) OR diabetes OR hypertension OR asthma) |
| EMBASE | ‘ ‘medication compliance’ OR ‘medication adherence’ OR ‘therapeutic adherence’ OR (therapeutic AND (‘adherence’/exp OR adherence)) OR ‘treatment adherence’/exp OR ‘treatment adherence’ OR ((‘treatment’/exp OR treatment) AND (‘adherence’/exp OR adherence)) OR ‘medication persistence’ OR ‘medication’/exp OR medication OR ‘persistence’/exp OR persistence AND ‘treatment beliefs’ OR ((‘treatment’/exp OR treatment) AND (‘beliefs’/exp OR beliefs)) OR ‘medication beliefs’ OR ((‘medication’/exp OR medication) AND (‘beliefs’/exp OR beliefs)) OR ‘therapeutic beliefs’ OR (therapeutic AND (‘beliefs’/exp OR beliefs)) OR ‘beliefs about medicines questionnaire’/exp OR ‘beliefs about medicines questionnaire’ OR ‘general beliefs’ OR (general AND (‘beliefs’/exp OR beliefs)) OR ‘harm beliefs’ OR (harm AND (‘beliefs’/exp OR beliefs)) OR ‘overuse beliefs’ OR (overuse AND (‘beliefs’/exp OR beliefs)) AND (‘hypertension’/exp OR hypertension OR ‘chronic obstructive pulmonary disease’/exp OR ‘chronic obstructive pulmonary disease’ OR (chronic AND obstructive AND pulmonary AND (‘disease’/exp OR disease)) OR ‘asthma’/exp OR asthma OR ‘diabetes’/exp OR diabetes) |
| Methodological Quality Criteria | Lemay et al. [2] | Pereira et al. [24] | Olorunfemi and Ojewole [25] | Yousefabadi et al. [26] | Sweileh et al. [27] | Ross, Walker and MacLeod [28] | Wilhelm, Rief, and Doering [29] | Wei et al. [30] | Rajpura and Nayak [31] | Al-Ruthia et al. [32] |
|---|---|---|---|---|---|---|---|---|---|---|
| Is the sampling strategy relevant to address the research question? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Is the sample representative of the target population? | Unknown | No | No | Unknown | No | Yes | No | Yes | No | No |
| Are the measurements appropriate? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Is the risk of non-response bias low? | Yes | Yes | Unknown | Unknown | Unknown | Yes | Yes | Yes | Yes | Yes |
| Is the statistical analysis appropriate to answer the research question? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Total score | 75% (High quality) | 75% (High quality) | 50% (Medium quality) | 50% (Medium quality) | 50% (Medium quality) | 100% (High quality) | 75% (High quality) | 100% (High quality) | 75% (High quality) | 75% (High quality) |
| Reference | Chronic Condition | Demographics Characteristics | Duration of Illness | Measurement of Medication Adherence | Association with Medication Adherence | Statistical Analysis | ||
|---|---|---|---|---|---|---|---|---|
| Age Mean (SD) | Male N (%) | Settings | ||||||
| [30] | Diabetes Mellitus type 2 | 62.5 (13.9) | 174 (55.2) | Two large urban hospitals in Hefei and Tianjin, China | 5 years | Medication Adherence Report Scale |
| r = 0.49, p < 0.01 |
| r = 0.49, p < 0.01 | |||||||
| [24] | Diabetes Mellitus type 2 | 59.2 years | 225 (58.1) | 40 healthcare centers of the northern region of Portugal. | No more than 1 year | Medication Adherence Scale |
| r = −0.13, p < 0.01 |
| [29] | Hypertension | 53.93 (15.46) | 133 (51.3) | Link to the survey was spread via various mail distributors (e.g., the German Society for Hypertension). The link was also printed on flyers that were distributed to pharmacies and hospitals in Germany. | 9 years | Rief adherence index (RAI) |
| β = 0.61, p < 0.001 |
| [32] | Hypertension | 60 years | 43 (22.6) | Seniors centers in Memphis (USA) | - | Morisky Medication Adherence Scale (MMAS-8) |
| p = 0.167 |
| p = 0.323 | |||||||
| [27] | Diabetes Mellitus type 2 | 58.3 (10.4) | 189 (46.7) | Al-Makhfia governmental diabetes primary healthcare clinic in Nablus, Palestine | 8.5 | Morisky Medication Adherence Scale (MMAS-8) |
| OR, 1.0 95% CI (0.94–1.1) p = 0.95 |
| OR, 1.1 95% CI (1.1–1.2) p < 0.001 | |||||||
| [31] | Hypertension | >55 years | 75 (64.1) | Adult day care center in New York City (USA) | >7 years | Morisky Medication Adherence Scale (MMAS-4) |
| β = −0.074, p = 0.473 |
| β = −0.071, p = 0.396 | |||||||
| [2] | Cardiovascular, Diabetes | >18 years | 444 (56.7) | Primary healthcare, Kuwait | - | Medication Adherence Report Scale |
| β = −0.46, p < 0.05 |
| [25] | Diabetes Mellitus type 2 | >27 years | 80 (44.4) | Diabetic clinic in three hospitals in Benin-city, Nigeria | - | Morisky Medication Adherence Scale (MMAS-4) |
| r = −0.208 p = 0.005 |
| [28] | Hypertension | 59.92 (12.16) | 267 (51.9) | A secondary care hypertension clinic and shared care scheme, UK | - | Morisky Medication Adherence Scale (MMAS-4) |
| p > 0.05 |
| p > 0.05 | |||||||
| [23] | Asthma | 56.7 (15.9) | 203 (50.5) | Different hospitals, primary care, and specialists practices in the area of Regensburg, Germany | 9.94 | Medication Adherence Report Scale |
| OR, 0.5 95% CI [0.3–1.03], p = 0.02 |
| OR, 0.56 95% CI [0.34–0.93] p < 0.01 | |||||||
| [26] | Hypertension | >30 years | 251 (56.3) | All health centers and clinics of internal and heart diseases under coverage of Zahedan University of Medical Sciences based in Zahedan, Iran | <15 years | Medication Adherence Questionnaire |
| p = 0.02 |
| p = 0.1 | |||||||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shahin, W.; Kennedy, G.A.; Stupans, I. The Consequences of General Medication Beliefs Measured by the Beliefs about Medicine Questionnaire on Medication Adherence: A Systematic Review. Pharmacy 2020, 8, 147. https://doi.org/10.3390/pharmacy8030147
Shahin W, Kennedy GA, Stupans I. The Consequences of General Medication Beliefs Measured by the Beliefs about Medicine Questionnaire on Medication Adherence: A Systematic Review. Pharmacy. 2020; 8(3):147. https://doi.org/10.3390/pharmacy8030147
Chicago/Turabian StyleShahin, Wejdan, Gerard A. Kennedy, and Ieva Stupans. 2020. "The Consequences of General Medication Beliefs Measured by the Beliefs about Medicine Questionnaire on Medication Adherence: A Systematic Review" Pharmacy 8, no. 3: 147. https://doi.org/10.3390/pharmacy8030147
APA StyleShahin, W., Kennedy, G. A., & Stupans, I. (2020). The Consequences of General Medication Beliefs Measured by the Beliefs about Medicine Questionnaire on Medication Adherence: A Systematic Review. Pharmacy, 8(3), 147. https://doi.org/10.3390/pharmacy8030147






