A Research Partnership to Enhance Postgraduate Pharmacy Residency Training Outcomes
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Collection and Analysis
2.2. Description of the Postgraduate Year Two (PGY2) Ambulatory Care Pharmacy Program Residency Program
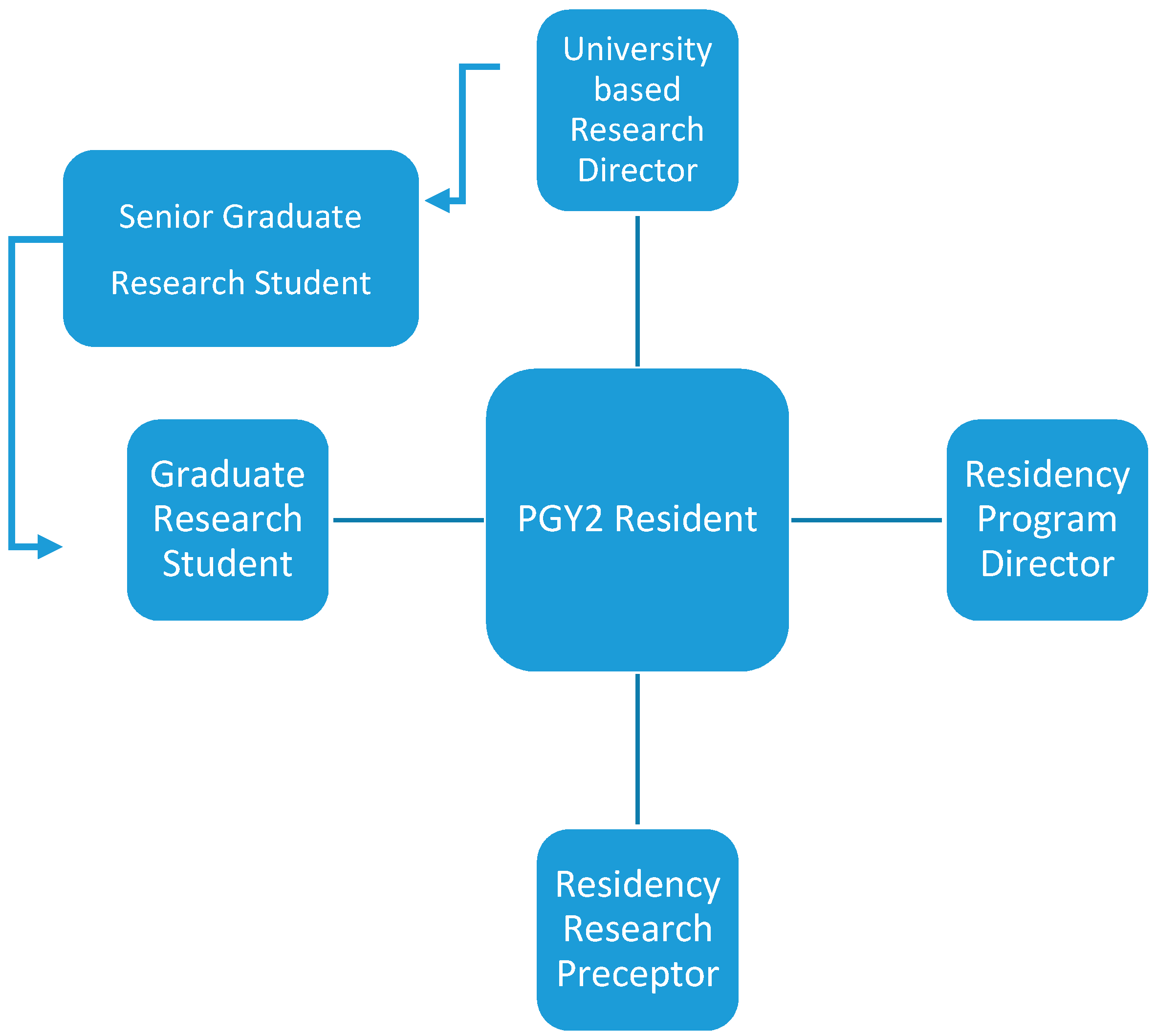
2.3. Description of the Postgraduate Year Two (PGY2) Residency Research Team
2.4. Description of the University-Based Research Team
2.5. Description of the Research Learning Experience
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- American Society of Health-System Pharmacists. Guidance Document for the ASHP Accreditation Standard for Postgraduate Year Two Pharmacy Residency Programs. Available online: https://www.ashp.org/-/media/assets/professional-development/residencies/docs/pgy2-guidance-document.ashx?la=en&hash=52D0B7CE0253D49A6298C0F068D07F3BA9E3608E (accessed on 18 May 2020).
- Hoffman, J.M.; Thomley, S.; Vermeulen, L.; Smith, K.M. Pharmacy residency training in academic medical centers. Am. J. Health Pharm. 2004, 61, 2528–2533. [Google Scholar] [CrossRef] [PubMed]
- Irwin, A.N.; Olson, K.L.; Joline, B.R.; Witt, D.M.; Patel, R.J. Challenges to publishing pharmacy resident research projects from the perspectives of residency program directors and residents. Pharm. Pr. 2013, 11, 166–172. [Google Scholar] [CrossRef] [PubMed]
- Shafeeq, H.; Hammond, D.A.; Swanson, J.M.; Li, C.; Devlin, J.W. Critical Care PGY-2 Graduate Perceptions and Practices Regarding Residency Project Publication. Am. J. Pharmaceut. Educ. 2019, 83, 6515. [Google Scholar] [CrossRef] [PubMed]
- Streetman, D.S.; McCreadie, S.R.; McGregory, M.; Ellis, J.J. Evaluation of clinical research knowledge and interest among pharmacy residents: Survey design and validation. Am. J. Health Pharm. 2006, 63, 2372–2377. [Google Scholar] [CrossRef]
- Ellis, J.; McCreadie, S.R.; McGregory, M.; Streetman, D.S. Effect of pharmacy practice residency training on residents’ knowledge of and interest in clinical research. Am. J. Health Pharm. 2007, 64, 2055–2063. [Google Scholar] [CrossRef]
- Mueller, E.W.; Bishop, J.R.; Kanaan, A.O.; Kiser, T.H.; Phan, H.; Yang, K.Y. Research Fellowship Programs as a Pathway for Training Independent Clinical Pharmacy Scientists. Pharmacother. J. Hum. Pharmacol. Drug Ther. 2015, 35, e13–e19. [Google Scholar] [CrossRef]
- O’Dell, K.M.; Shah, S.A. Evaluation of pharmacy practice residents’ research abstracts and publication rate. J. Am. Pharm. Assoc. 2012, 52, 524–527. [Google Scholar] [CrossRef]
- Olson, K.L.; Irwin, A.N.; Billups, S.J.; Delate, T.; Johnson, S.G.; Kurz, D.; Witt, D.M. Impact of a clinical pharmacy research team on pharmacy resident research. Am. J. Health Pharm. 2015, 72, 309–316. [Google Scholar] [CrossRef]
- American Society of Health-System Pharmacists. Accreditation Standards for Post Graduate Year 1 (PGY1) and Post Graduate Year 2 (PGY2) Pharmacy Residencies. Available online: http://www.ashp.org/menu/Accreditation/ResidencyAccreditation.aspx# (accessed on 18 May 2020).
- The Collaborative Institutional Training Initiative. Available online: https://about.citiprogram.org/en/homepage/ (accessed on 2 March 2020).
- University of Arizona. Research Gateway. Available online: https://rgw.arizona.edu (accessed on 3 March 2020).
- Kaiser Permanente Colorado. ASPIRE: A Structured Program to Guide Resident Experience in Research. Available online: http://aspirekpco.weebly.com (accessed on 28 February 2020).
- Rodrigues, C.R.; Harrington, A.R.; Murdock, N.; Holmes, J.T.; Borzadek, E.Z.; Calabro, K.; Martin, J.; Slack, M.K. Effect of Pharmacy-Supported Transition-of-Care Interventions on 30-Day Readmissions: A Systematic Review and Meta-analysis. Ann. Pharmacother. 2017, 51, 866–889. [Google Scholar] [CrossRef]
- Tetuan, C.; Axon, D.R.; Bingham, J.; Boesen, K.; Lipsy, R.; Scovis, N.; Taylor, A.M.; Warholak, T.; Lott, B.E.; Leal, S. Assessing the Effect of a Telepharmacist’s Recommendations During an Integrated, Interprofessional Telehealth Appointment and Their Alignment with Quality Measures. J. Manag. Care Spéc. Pharm. 2019, 25, 1334–1339. [Google Scholar] [CrossRef]
- Jamjoom, O.; Marupuru, S.; Taylor, A.M.; Warholak, T.; Scovis, N.; Bingham, J.M. Evaluating provider acceptance of pharmacist interventions in the Discharge Companion Program and its association with readmission reduction. J. Am. Pharm. Assoc. 2020, 60, e47–e51. [Google Scholar] [CrossRef] [PubMed]
- Morris, C.T.; Hatton, R.C.; Kimberlin, C.L. Factors associated with the publication of scholarly articles by pharmacists. Am. J. Health Pharm. 2011, 68, 1640–1645. [Google Scholar] [CrossRef] [PubMed]
- Bookstaver, P.B.; Miller, A.D.; Felder, T.M.; Tice, D.L.; Norris, L.; Sutton, S.S. Assessing Pharmacy Residents’ Knowledge of Biostatistics and Research Study Design. Ann. Pharmacother. 2012, 46, 991–999. [Google Scholar] [CrossRef]
- Swanoski, M.T.; Akers, M.F.; Amaro, M.L.; Huot, K.L.; Lutfiyya, M.N. Incorporating Research into a Postgraduate Year 1 Pharmacy Residency. Am. J. Pharm. Educ. 2012, 76. [Google Scholar] [CrossRef] [PubMed]
- Clarke, M.; Powell, S. Goal setting in a layered relationship mentoring model. In Beyond Goals: Effective Strategies for Coaching and Mentoring; David, S., Clutterbuck, D., Megginson, D., Eds.; Taylor and Francis Group: Abingdon, UK, 2013; pp. 289–310. [Google Scholar]
- Ehrich, L.C.; Handsford, B.; Tennent, L. Educational mentoring: Is it worth the effort? Educ. Res. Perspec. 2003, 30, 42–75. [Google Scholar]
- Raub, J.N.; Thurston, T.M.; Fiorvento, A.D.; Mynatt, R.P.; Wilson, S.S. Implementation and outcomes of a pharmacy residency mentorship program. Am. J. Health Pharm. 2015, 72, S1–S5. [Google Scholar] [CrossRef]
- Kane-Gill, S.L.; Reddy, P.; Gupta, S.R.; Bakst, A.W. Guidelines for Pharmacoeconomic and Outcomes Research Fellowship Training Programs: Joint Guidelines from the American College of Clinical Pharmacy and the International Society of Pharmacoeconomics and Outcomes Research. Pharmacother. J. Hum. Pharmacol. Drug Ther. 2008, 28, 1552. [Google Scholar] [CrossRef]
- Vouri, S.M.; Stranges, P.M.; Burke, J.M.; Micek, S.; Pitlick, M.K.; Wenger, P. The importance of research during pharmacy residency training. Curr. Pharm. Teach. Learn. 2015, 7, 892–898. [Google Scholar] [CrossRef]
- Almodóvar, A.S.; Nahata, M.C. Associations Between Chronic Disease, Polypharmacy, and Medication-Related Problems Among Medicare Beneficiaries. J. Manag. Care Spéc. Pharm. 2019, 25, 573–577. [Google Scholar] [CrossRef]
- Silva-Almodóvar, A.; Nahata, M.C. Potentially Unsafe Chronic Medication Use Among Older Adult Chronic Opioid Users. Pharmacother. J. Hum. Pharmacol. Drug Ther. 2019, 39, 140–149. [Google Scholar] [CrossRef]
- Silva-Almodóvar, A.; Axon, D.R.; Coleman, A.; Warholak, T.; Nahata, M.C. The Effect of Plan Type and Comprehensive Medication Reviews on High-Risk Medication Use. J. Manag. Care Spéc. Pharm. 2018, 24, 416–422. [Google Scholar] [CrossRef]
- Silva-Almodóvar, A.; Chang, H.-C.K.; Matsunami, M.; Coleman, A.; Nahata, M.C. Confidence in skills applied to patient care among PharmD students in telehealth medication management programs versus other settings. Curr. Pharm. Teach. Learn. 2018, 10, 558–565. [Google Scholar] [CrossRef] [PubMed]
- Silva-Almodóvar, A.; Surve, S.; Axon, D.R.; Cooper, D.; Nahata, M.C. Self-Directed Engagement with a Mobile App (Sinasprite) and Its Effects on Confidence in Coping Skills, Depression, and Anxiety: Retrospective Longitudinal Study. JMIR mHealth uHealth 2018, 6, e64. [Google Scholar] [CrossRef] [PubMed]
| Objective | Description of Activities |
|---|---|
| Analyzing |
|
| Creating |
|
| Evaluating |
|
| Program Year | Research Dissemination | Program Feedback | Proposed Changes for the Next Program Year |
|---|---|---|---|
| Year 1 2012–2013 |
|
|
|
| Year 2 2013–2014 |
|
|
|
| Year 3 2014–2015 |
|
|
|
| Year 4 2015–2016 |
|
|
|
| Year 5 2016–2017 |
|
|
|
| Year 6 2017–2018 * |
|
|
|
| Year 7 2018–2019 |
|
|
|
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bingham, J.M.; Silva Almodovar, A.; Taylor, A.M.; Axon, D.R.; Nahata, M.C.; Leal, S.; Warholak, T.; Scovis, N. A Research Partnership to Enhance Postgraduate Pharmacy Residency Training Outcomes. Pharmacy 2020, 8, 134. https://doi.org/10.3390/pharmacy8030134
Bingham JM, Silva Almodovar A, Taylor AM, Axon DR, Nahata MC, Leal S, Warholak T, Scovis N. A Research Partnership to Enhance Postgraduate Pharmacy Residency Training Outcomes. Pharmacy. 2020; 8(3):134. https://doi.org/10.3390/pharmacy8030134
Chicago/Turabian StyleBingham, Jennifer M., Armando Silva Almodovar, Ann M. Taylor, David R. Axon, Milap C. Nahata, Sandra Leal, Terri Warholak, and Nicole Scovis. 2020. "A Research Partnership to Enhance Postgraduate Pharmacy Residency Training Outcomes" Pharmacy 8, no. 3: 134. https://doi.org/10.3390/pharmacy8030134
APA StyleBingham, J. M., Silva Almodovar, A., Taylor, A. M., Axon, D. R., Nahata, M. C., Leal, S., Warholak, T., & Scovis, N. (2020). A Research Partnership to Enhance Postgraduate Pharmacy Residency Training Outcomes. Pharmacy, 8(3), 134. https://doi.org/10.3390/pharmacy8030134






