Insights from Regulatory Data on Development Needs of Community Pharmacy Professionals
Abstract
1. Introduction
2. Materials and Methods
2.1. Jurisprudence (JP) Exam Data for Applicants (Pharmacists and Pharmacy Technicians)
2.2. Practice Assessment Data for Pharmacists and Pharmacy Technicians
2.3. Operational Assessment Data for Community Pharmacies
2.4. Conduct Data for Pharmacists and Pharmacy Technicians
3. Results
3.1. Jurisprudence Exam
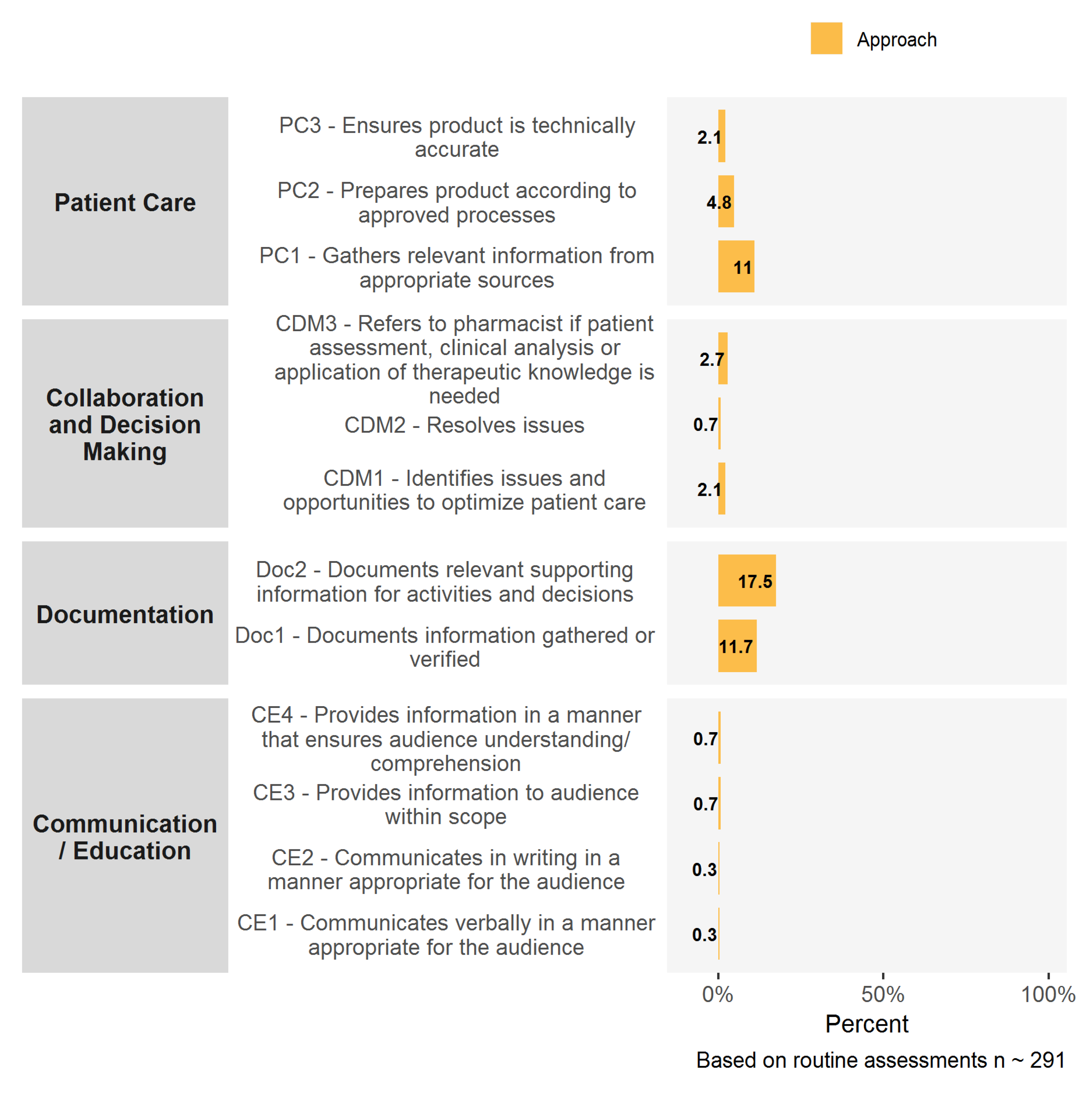
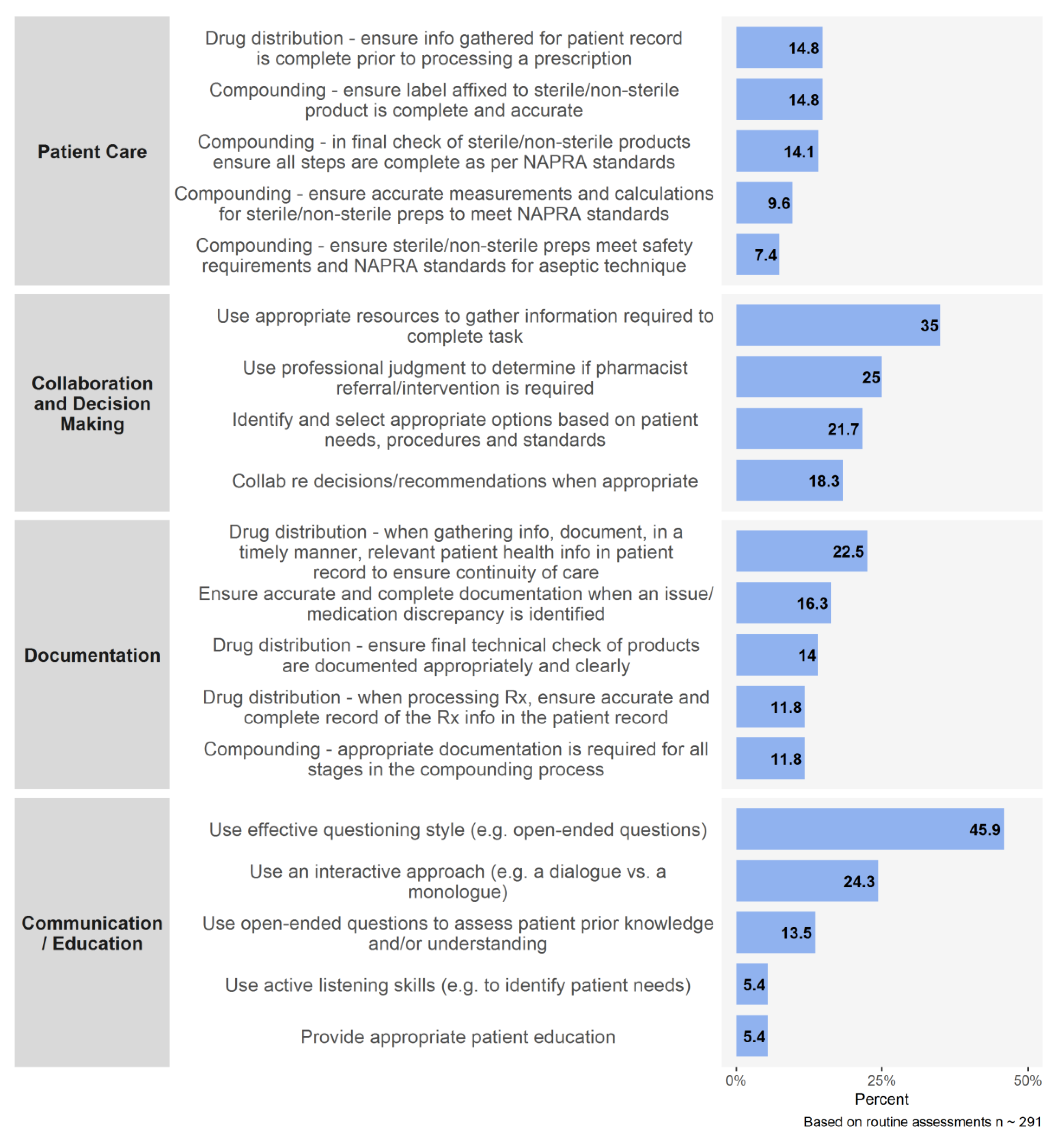
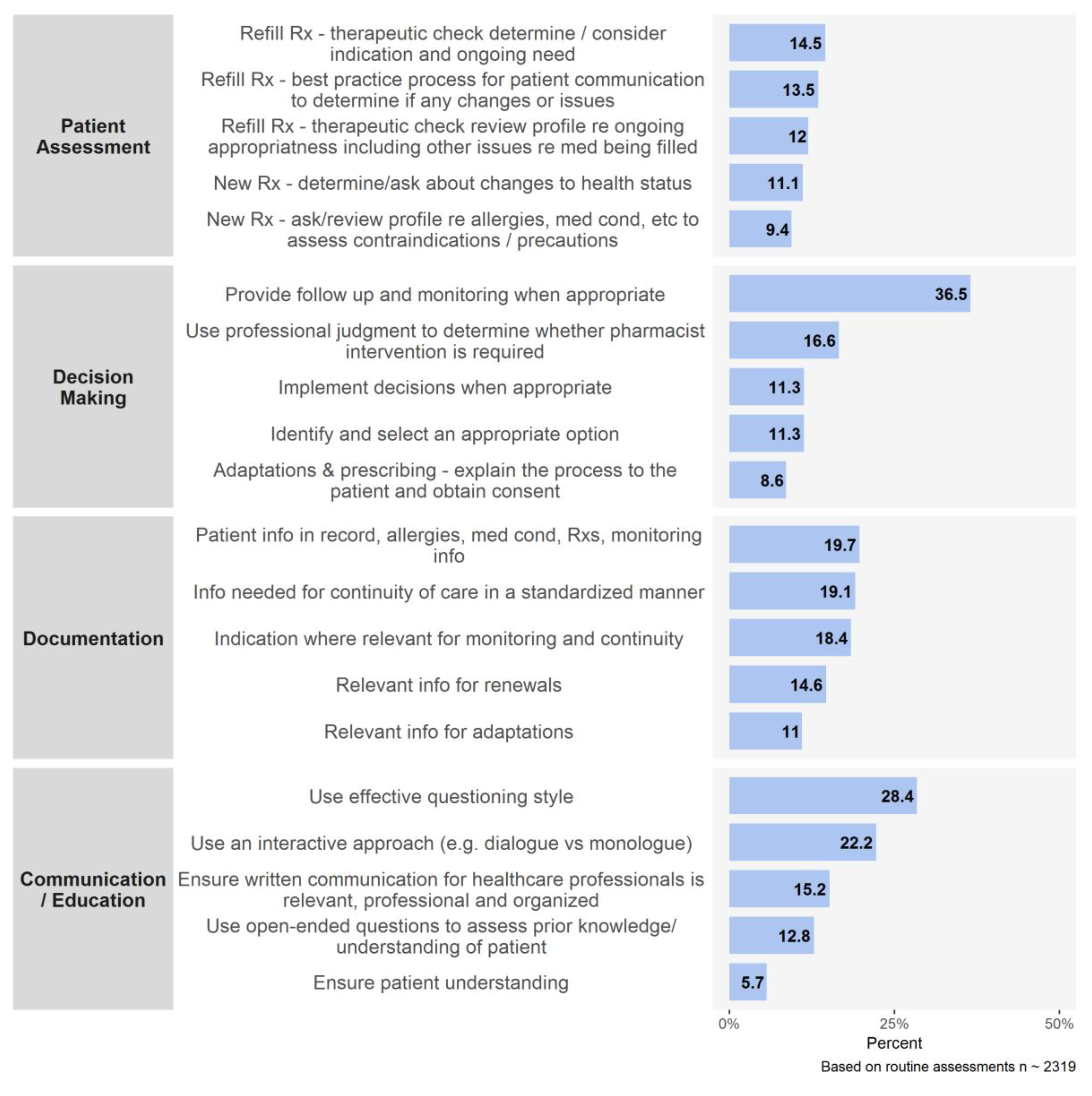
3.2. Practice Assessments
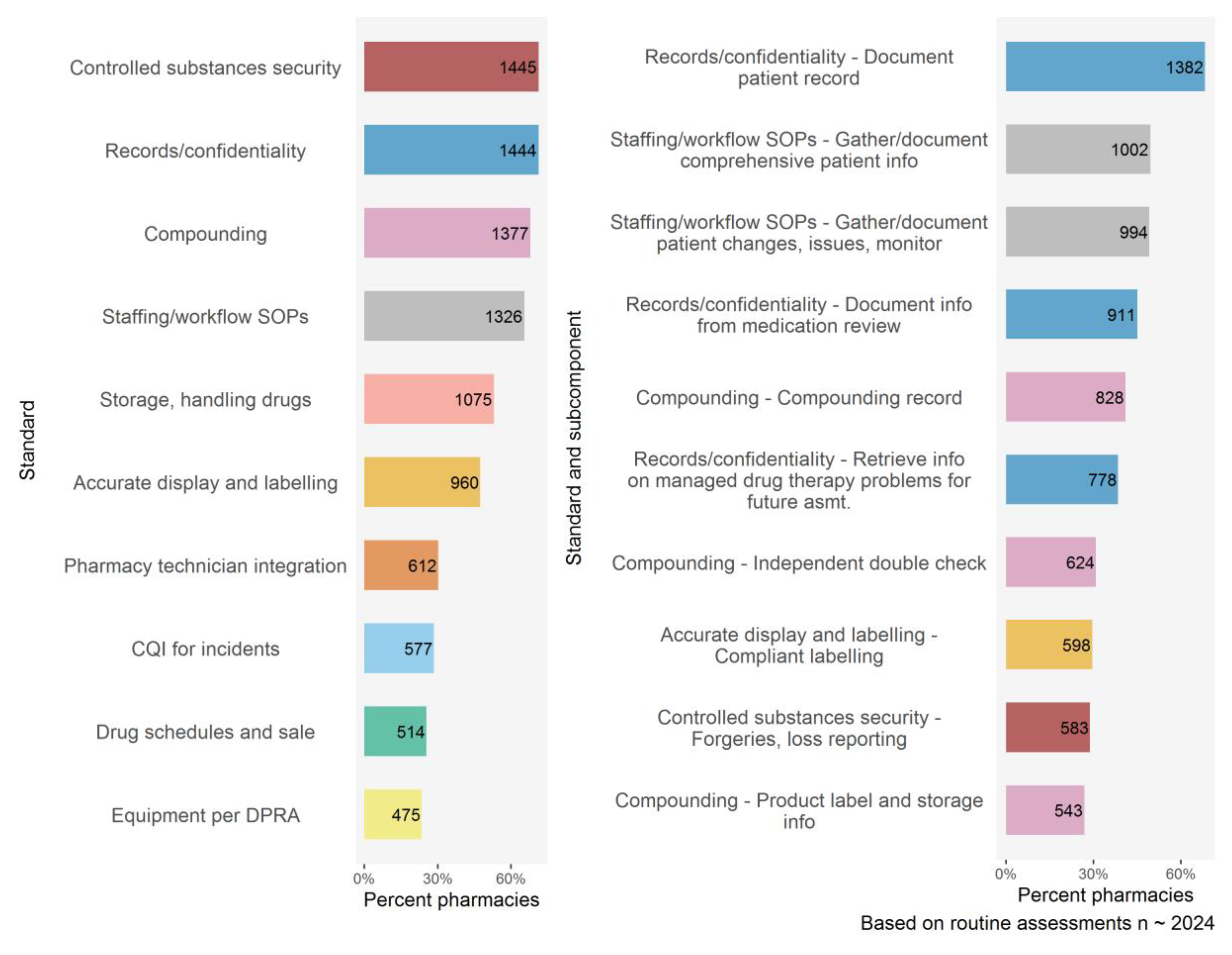
3.3. Operational Assessments
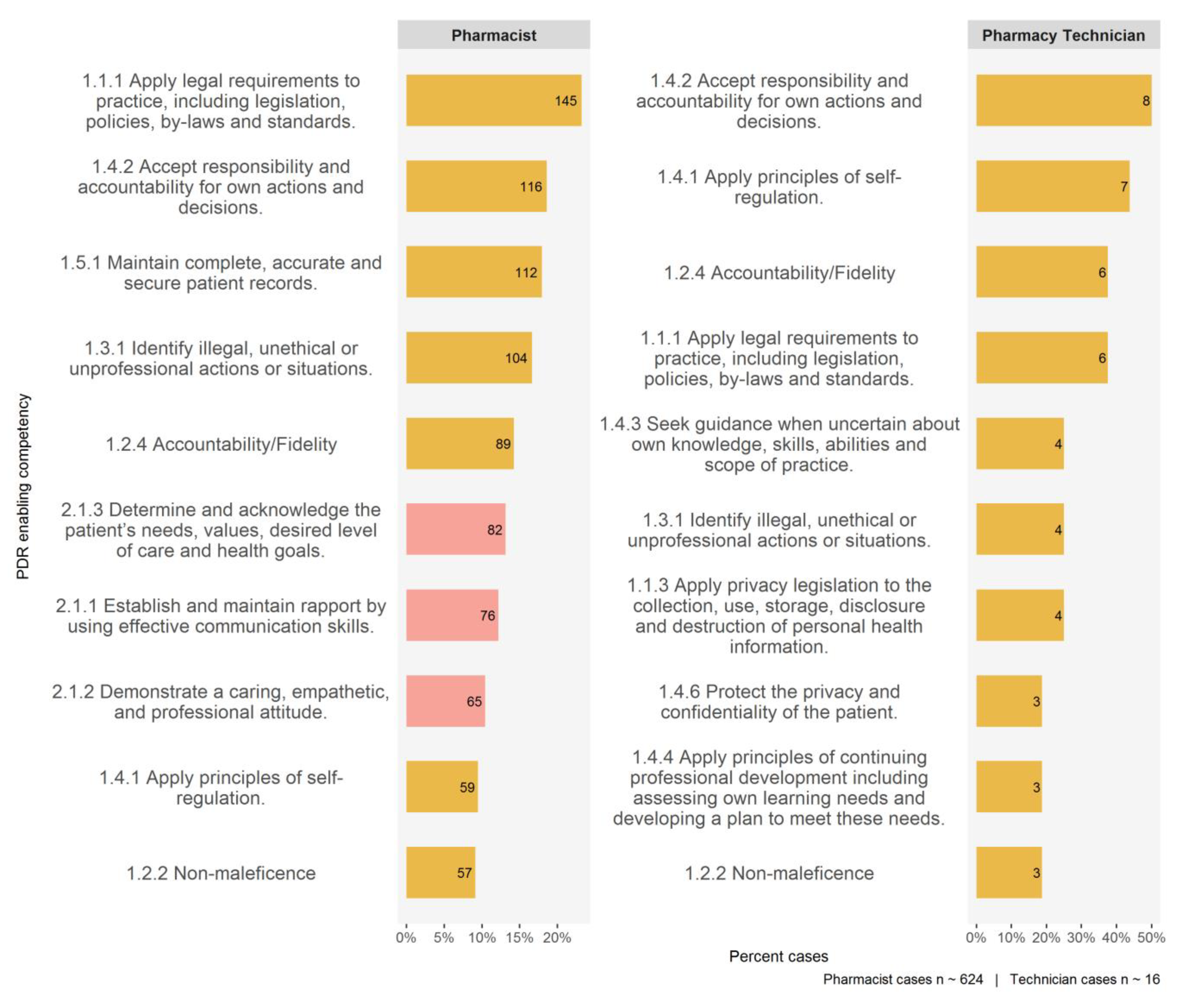
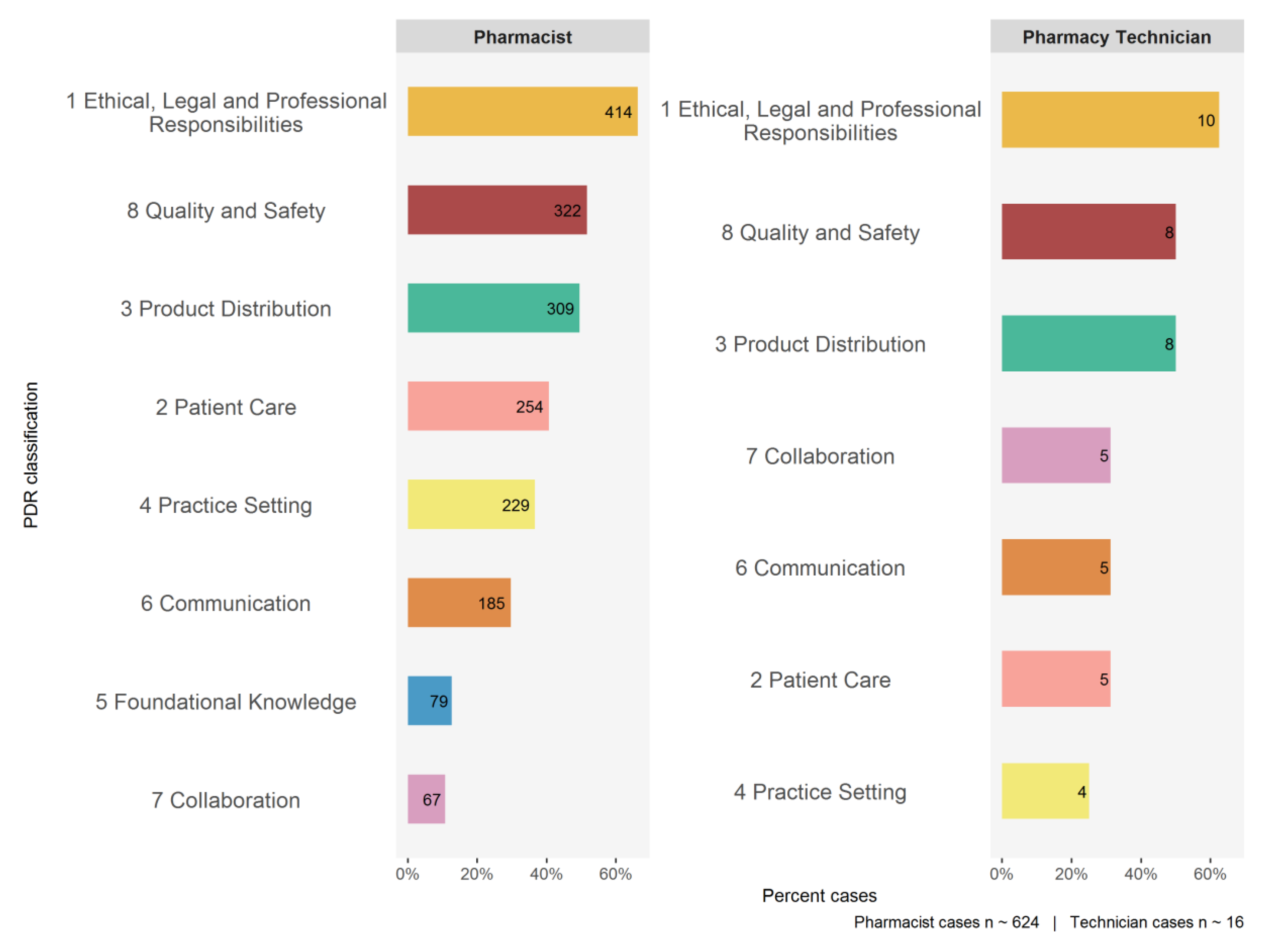
3.4. Conduct
4. Discussion
- Requirement 10—Comprehensiveness of Clinical Records and Requirement [26] calls for all PPMS to provide users with the ability to create, access and update records of assessment, care plans, interventions and follow up by pharmacy professionals and all information indicated in provincial pharmacy standards of practice; and
- Requirement 17—Prescription Indications [26] necessitates all PPMS to provide users with the ability to input an indication or treatment objective for each prescription.
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A


References
- Winkelbauer, S. An authentic, practice-based assessment as a catalyst for continuous professional development. Pharmacy 2020, 8, 15. [Google Scholar] [CrossRef] [PubMed]
- National Association of Pharmacy Regulatory Authorities (NAPRA). Professional Competencies for Canadian Pharmacists at Entry to Practice 2014. 2014. Available online: https://napra.ca/pharmacists/professional-competencies-canadian-pharmacists-entry-practice-2014 (accessed on 7 February 2020).
- Hanna, A.; Hanna, L. Topic analysis of UK fitness to practice cases: What lessons can be learnt? Pharmacy 2019, 7, 130. [Google Scholar] [CrossRef] [PubMed]
- Williams, S. Independent Review of General Chiropractic Council Fitness to Practise Cases 2010–2013; General Chiropractic Council: London, UK, March 2014; Available online: https://www.gcc-uk.org/assets/publications/Thematic_review_of_ftp_cases_2010-2013_PUBLIC_FINAL.pdf (accessed on 19 June 2020).
- Phipps, D.L.; Noyce, P.R.; Walshe, K.; Parker, D.; Ashcroft, D.M. Pharmacists subjected to disciplinary action: Characteristics and risk factors. Int. J. Pharm. Pract. 2011, 19, 367–373. [Google Scholar] [CrossRef] [PubMed]
- Phipps, D.L.; Walshe, K.; Parker, D.; Noyce, P.R.; Ashcroft, D.M. Job characteristics, well-being and risky behaviour amongst pharmacists. Psychol. Health Med. 2016, 21, 932–944. [Google Scholar] [CrossRef] [PubMed]
- Ontario College of Pharmacists. Self-Assessment Tool. Available online: https://www.ocpinfo.com/practice-education/qa-program/self-assessment/ (accessed on 10 March 2020).
- Austin, Z.; Marini, A.; Macleod Glover, N.; Croteau, D. Continuous professional development: A qualitative study of pharmacists’atitudes, behaviors, and preferences in Ontario, Canada. Am. J. Pharm. Educ. 2005, 69, 4. [Google Scholar] [CrossRef]
- Ontario College of Pharmacists. Self-Assessment Tool. Available online: https://www.ocpinfo.com/regulations-standards/professional-responsibility-in-practice/ (accessed on 5 January 2020).
- Ontario College of Pharmacists. Examination Blueprint. Available online: https://www.ocpinfo.com/registration/registration-requirements/jp-exam/jp-exam-blueprint/ (accessed on 11 January 2020).
- Ontario College of Pharmacists. Pharmacist Practice Assessment Criteria. Available online: https://www.ocpinfo.com/library/practice-related/download/PracticeAssessmentCriteria.pdf (accessed on 5 January 2020).
- Ontario College of Pharmacists. Pharmacy Technician Practice Assessment Criteria. Available online: https://www.ocpinfo.com//library/practice-related/download/PharmacyTechnicianPracticeAssessmentCriteria.pdf (accessed on 5 January 2020).
- Ontario College of Pharmacists. Designated Managers. Available online: https://www.ocpinfo.com/practice_resource/designated-managers/ (accessed on 5 January 2020).
- Ontario College of Pharmacists. Community Pharmacy Assessment Criteria. Updated January 2020 Community Pharmacy Assessment Criteria. Available online: https://www.ocpinfo.com/wp-content/uploads/documents/CommunityPharmacyAssessmentCriteria.pdf (accessed on 5 January 2020).
- Ontario College of Pharmacists. Committees. Available online: https://www.ocpinfo.com/about/council-committees/committees/ (accessed on 5 January 2020).
- Carpenter, J.; Bithel, J. Bootstrap confidence intervals: When, which, what? A practical guide for medical statisticians. Stat. Med. 2000, 19, 1141–1164. [Google Scholar] [CrossRef]
- Efron, B. Better bootstrap confidence intervals. J. Am. Stat. Assoc. 1987, 82, 171–200. [Google Scholar] [CrossRef]
- Ontario College of Pharmacists. Public Register. Available online: http://members.ocpinfo.com/tcpr/public/pr/en/ (accessed on 10 January 2020).
- Perrier, D.G.; Winslade, N.; Pugsley, J.; Lavack, L.; Strand, L.M. Designing a pharmaceutical care curriculum. Am. J. Pharm. Educ. 1995, 59, 113–124. [Google Scholar]
- The Canadian Council for Accreditation of Pharmacy Programs. Accreditation-Standards for Canadian-First Professional Degree in Pharmacy Programs. Available online: http://ccapp-accredit.ca/wp-content/uploads/2016/01/Accreditation-Standards-for-Canadian-First-Professional-Degree-in-Pharmacy-Programs.pdf (accessed on 5 January 2020).
- National Association of Pharmacy Regulatory Authorities. Model Standards of Practice for Canadian Pharmacists. Available online: https://napra.ca/sites/default/files/2017-09/Model_Standards_of_Prac_for_Cdn_Pharm_March09_layout2017_Final.pdf (accessed on 7 February 2020).
- Zubin, A.; Gregory, P. Understanding psychological engagement and flow in community pharmacy practice. Res. Soc. Admin. Pharm. 2020, 16, 488–496. [Google Scholar] [CrossRef]
- Ontario College of Pharmacists. Quality Indicators for Pharmacy. Available online: https://www.ocpinfo.com/wp-content/uploads/2019/08/QualityIndicatorsLeaflet.pdf (accessed on 10 March 2020).
- Zubin, A.; Gregory, P. Learning needs of pharmacists for an evolving scope of practice. Pharmacy 2019, 7, 140. [Google Scholar] [CrossRef] [PubMed]
- Canadian Pharmacists Association. Documenting Pharmacy Interventions in a Busy Dispensary. Available online: https://www.pharmacists.ca/cpha-ca/assets/File/education-practice-resources/WebinarSlides-DocumentingInterventions.pdf (accessed on 15 March 2020).
- National Association of Pharmacy Regulatory Authorities. Pharmacy Practice Management Systems: Requirements to Support NAPRA’s “Model Standards of Practice for Canadian Pharmacists”. Available online: https://napra.ca/sites/default/files/documents/NAPRA_Pharmacy_Practice_Management_Systems_November2013_b.pdf (accessed on 10 January 2020).
- Schindel, T.J.; Yuksel, N.; Breault, R.; Daniels, J.; Varnhagen, S.; Hughes, C.A. Pharmacists’ learning needs in the era of expanding scopes of practice: Evolving practices and changing needs. Res. Soc. Admin. Pharm. 2019, 15, 448–458. [Google Scholar] [CrossRef] [PubMed]
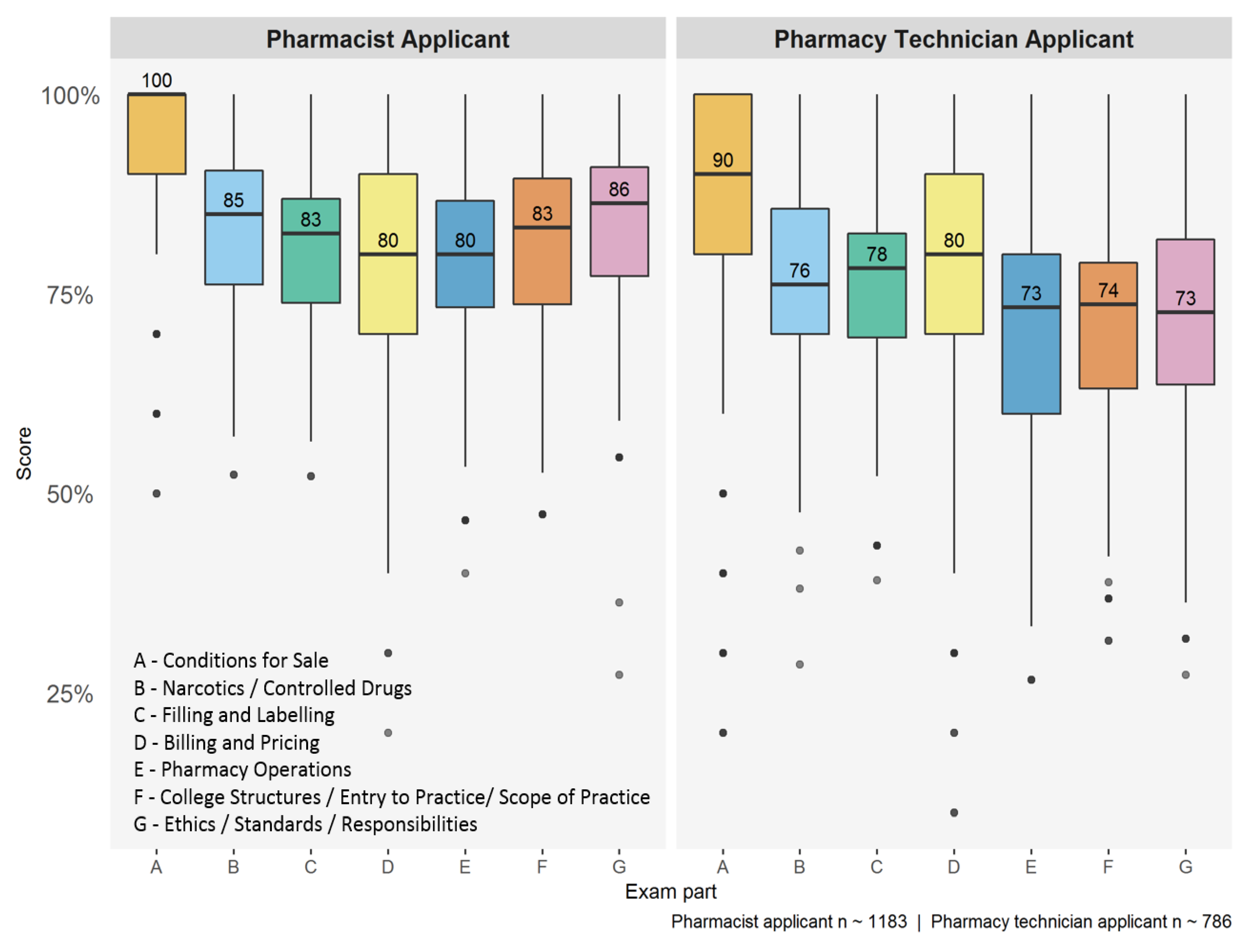


| Member Type | Exam Section | Median Score (%) | Mean Score (95% CI) |
|---|---|---|---|
| Pharmacist applicant | A: Conditions for Sale B: Narcotics/Controlled Drugs C: Filling and Labeling D: Billing and Pricing E: Pharmacy Operations F: College Structures/Entry to Practice/Scope of Practice G: Ethics/Standards/Responsibilities | 100.0 85.0 82.6 80.0 80.0 83.3 86.4 | 93.4 (92.9, 93.9) 83.1 (82.6, 83.6) 81.5 (81.0, 82.0) 81.9 (81.1, 82.7) 79.5 (78.8, 80.2) 81.4 (80.8, 82.0) 83.3 (82.8, 83.9) |
| Pharmacy technician applicant | A: Conditions for Sale B: Narcotics/Controlled Drugs C: Filling and Labeling D: Billing and Pricing E: Pharmacy Operations F: College Structures/Entry to Practice/Scope of Practice G: Ethics/Standards/Responsibilities | 90.0 76.2 78.3 80.0 73.3 73.7 72.7 | 83.2 (82.1, 84.3) 76.2 (75.5, 77.0) 75.9 (75.2, 76.6) 77.4 (76.3, 78.5) 71.6 (70.7, 72.5) 71.4 (70.6, 72.3) 72.4 (71.6, 73.2) |
| Domain | Indicator/Recommendation | Assessments (%) |
|---|---|---|
| Patient Assessment | PA1—gather info from patient 1 | 56.8 |
| Decision Making | DM3—monitor patient progress 1 | 47.5 |
| Provide monitoring and follow up 2 | 36.5 | |
| Documentation | Doc1—info in patient record 1 | 80.5 |
| Doc2—decisions and rationale 1 | 68.4 | |
| Doc3—communication with patient/healthcare team 1 | 52.2 | |
| Patient info in record (e.g., allergies, medical conditions) 2 | 19.7 | |
| Info needed for continuity of care 2 | 19.1 | |
| Communication/Education | Use effective questioning style 2 | 28.4 |
| Use an interactive approach 2 | 22.2 |
| Domain | Indicator/Recommendation | Assessments (%) |
|---|---|---|
| Patient Care | PC1—gather info from appropriate sources 1 | 11.0 |
| PC2—prepare product according to approved processes 1 | 4.8 | |
| Collaboration and Decision Making | CDM3—refer to pharmacist when needed 1 | 2.7 |
| Use appropriate resources to gather info required for task 2 | 35.0 | |
| Use prof. judgement to determine if pharmacist intervention is required 2 | 25.0 | |
| Documentation | Doc1—document info gathered or verified 1 | 11.7 |
| Doc2—document supporting info for activities and decisions 1 | 17.5 | |
| Document patient health info for continuity of care 2 | 22.5 | |
| Communication/Education | Use effective questioning style 2 | 45.9 |
| Use an interactive approach 2 | 24.3 |
| Standard and Subcomponent | Unmet (%) |
|---|---|
| Compounding | 68.0 |
| Full compounding record must be present | 40.9 |
| Controlled substances security | 71.4 |
| Records/confidentiality | 71.3 |
| Document patient record | 68.2 |
| Document information from medication review | 45.0 |
| Staffing/workflow SOPs | 65.5 |
| Gather and document comprehensive patient info | 49.5 |
| Gather and document changes to patient info | 49.1 |
| Storage, handling drugs | 53.1 |
| Category | Description | Cases (%) |
|---|---|---|
| PDR classification | Ethical, Legal and Professional Responsibilities | 66.3 |
| Quality and Safety | 51.6 | |
| Product Distribution | 49.5 | |
| Patient Care | 40.7 | |
| Practice Setting | 36.7 | |
| PDR key competency | Contribute to a culture of patient safety | 38.1 |
| Dispense a product safely and accurately | 36.8 | |
| Apply principles of professionalism | 35.2 | |
| Uphold ethical principles | 30.4 | |
| Practice within legal requirements | 30.3 | |
| PDR enabling competency | Apply legal requirements to practice | 23.2 |
| Accept responsibility and accountability for own actions and decisions | 18.6 | |
| Maintain complete, accurate and secure patient records | 17.9 | |
| Identify illegal or unethical actions or situations | 16.7 | |
| Accountability/fidelity | 14.3 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Morris, K.; Arzoomanian, A. Insights from Regulatory Data on Development Needs of Community Pharmacy Professionals. Pharmacy 2020, 8, 111. https://doi.org/10.3390/pharmacy8030111
Morris K, Arzoomanian A. Insights from Regulatory Data on Development Needs of Community Pharmacy Professionals. Pharmacy. 2020; 8(3):111. https://doi.org/10.3390/pharmacy8030111
Chicago/Turabian StyleMorris, Katherine, and Anita Arzoomanian. 2020. "Insights from Regulatory Data on Development Needs of Community Pharmacy Professionals" Pharmacy 8, no. 3: 111. https://doi.org/10.3390/pharmacy8030111
APA StyleMorris, K., & Arzoomanian, A. (2020). Insights from Regulatory Data on Development Needs of Community Pharmacy Professionals. Pharmacy, 8(3), 111. https://doi.org/10.3390/pharmacy8030111





