A Descriptive Quantitative Analysis on the Extent of Polypharmacy in Recipients of Ontario Primary Care Team Pharmacist-Led Medication Reviews
Abstract
1. Introduction
- What are the characteristics of patients on ≥3 chronic or concurrent medications who received a medication review conducted by Ontario primary care team pharmacists?
- What is the average number of medications per patient visiting a pharmacist in primary care?
- What proportion of patients that have been prescribed ≥3 chronic or concurrent medications have been identified with (a) DTPs and (b) medications discrepancies by Ontario primary care team pharmacists?
2. Materials and Methods
2.1. Study Design
2.2. Study Sample
2.3. Intervention Studied and Justification
2.4. Recruitment and Informed Consent
2.5. Data Collection and Management
- Polypharmacy was defined as the use of five or more prescribed drugs per day [15].
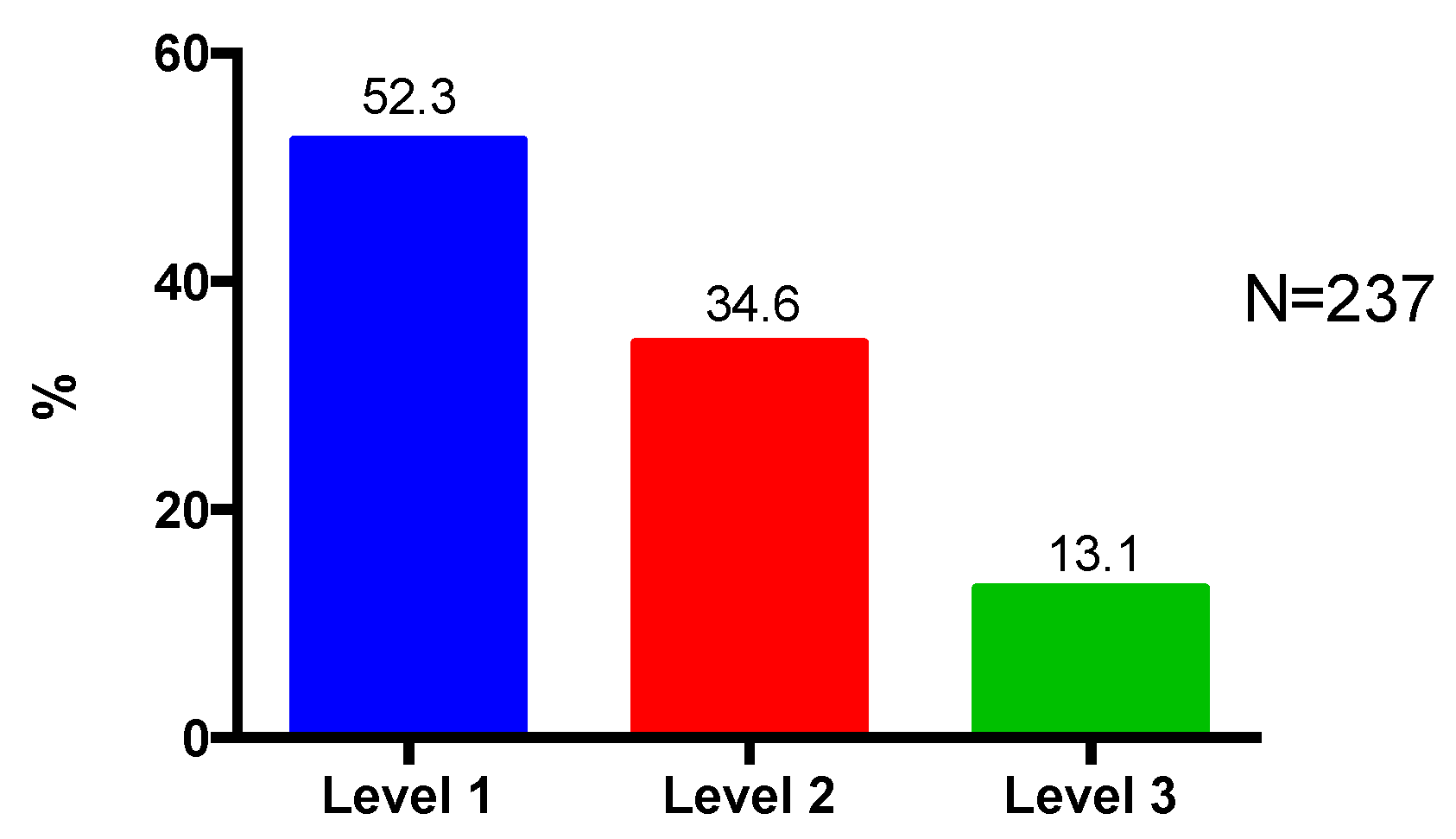
- Patient complexity was categorized into three complexity levels as described in Appendix A, Table A1 [31]. A higher assigned level of complexity represents a patient with greater health and pharmaceutical complexity.
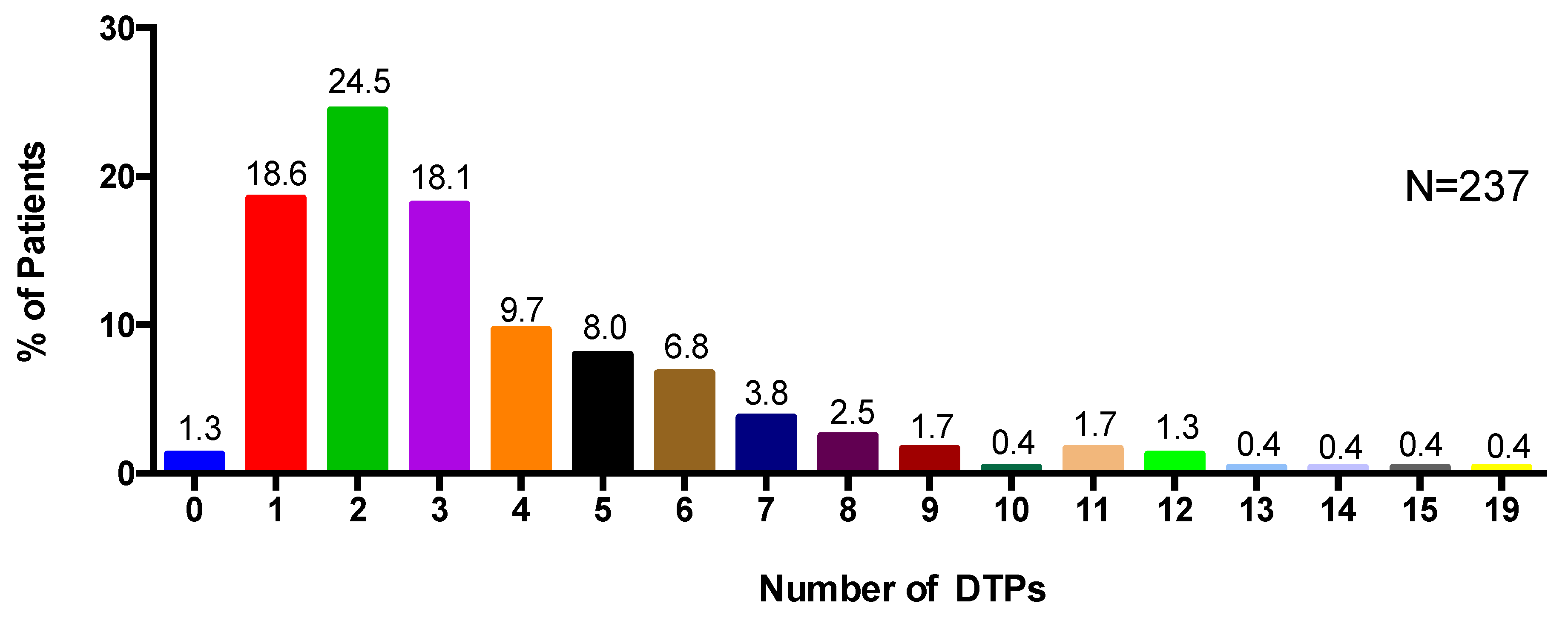
- DTPs were broadly defined as ‘an actual or potential undesirable event experienced by a patient which involves, or is suspected to involve, drug therapy and that interferes with achieving the desired goals of therapy’ classified according to the codes in Appendix A, Table A2 [32,33].
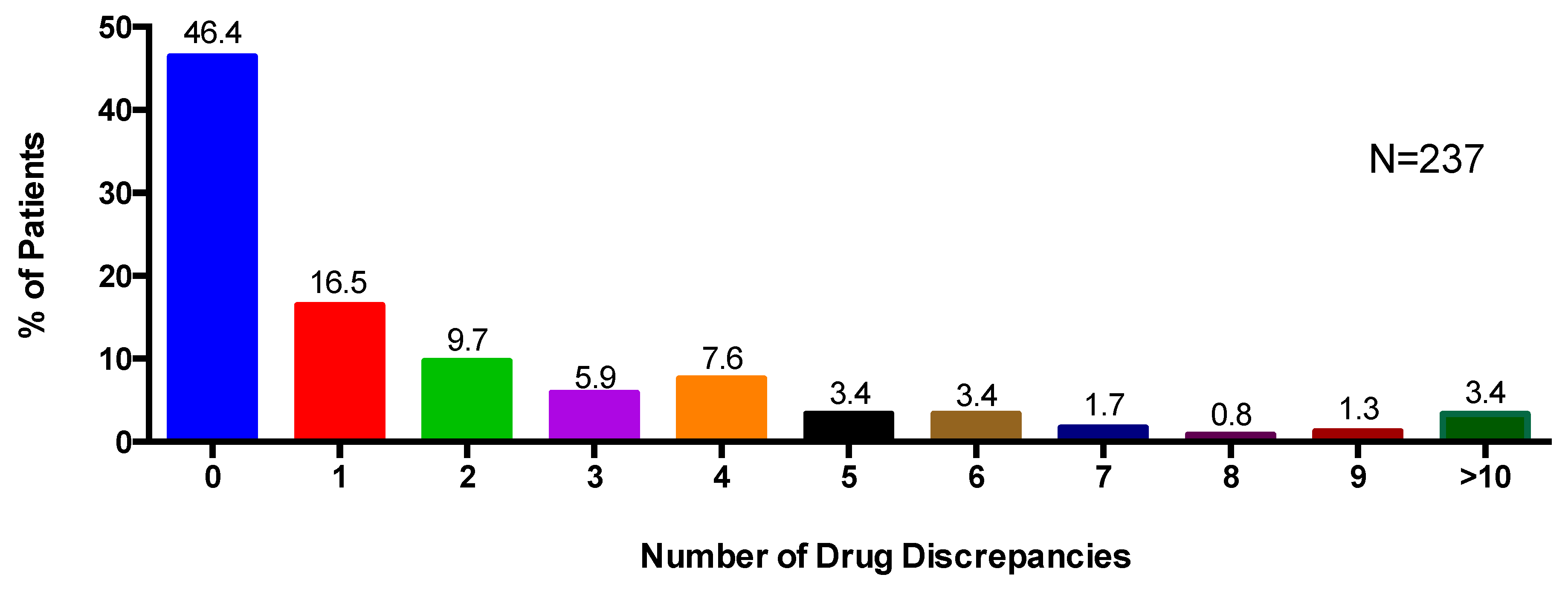
- Medication discrepancies were broadly defined as ‘any preventable event that may cause or lead to potentially inappropriate medication (PIM) use or patient harm while the medication is in control of the healthcare provider, patient or consumer’ [34]. The discrepancies in the data capture forms asked the pharmacist to classify the discrepancy as drug name, drug dose, drug frequency, or other.
- Pharmacists classified medications into general categories (ex. Medications for diabetes, medications for cardiovascular disease, etc.) based on their professional judgement and experience.
- Pharmacists noted discrepancies between the electronic medical record (EMR), and information identified during pharmacist medication review.
2.6. Data Analysis
3. Results
3.1. Patient Characteristics
3.2. Types of Medications, Polypharmacy and Patient Complexity
3.3. Number of Medication Discrepancies
3.4. Number of Drug Therapy Problems
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A. Definitions and Classifications
| Complexity Level | Factors |
|---|---|
| Level 1—low | The task (e.g., medication assessment, focused drug question) is clear (well defined). All patient-related factors are present and easily interpreted. |
| Level 2—moderate | The task referred to the pharmacist is unclear or not well defined. The pharmacist has to collect initial information before clearly defining the task. The patient is taking multiple medications and has multiple medical conditions requiring drug therapy. The clinical knowledge/skill required to address the task is complex. The DTPs identified are complex. |
| Level 3—high | Both the case scenario and the clinical knowledge are complex and ill-defined and multiple DTPs that are codependent are present. |
| Type of DTPs | Factors |
|---|---|
| Type 1 | Receiving/taking drug with no valid indication |
| Type 2 | Requires drug therapy for an indication and is not receiving/taking therapy |
| Type 3 | Not receiving/taking appropriate drug or drug product |
| Type 4 | Receiving/taking too little drug |
| Type 5 | Receiving/taking too much drug |
| Type 6 | Not receiving/taking prescribed drugs appropriately |
| Type 7 | Experiencing an adverse drug reaction (not dose-related) |
| Type 8 | Experiencing a drug–drug, drug–food, or drug–laboratory reaction |
| Type 99 Other | Other; examples include requesting further assessment from physician; laboratory parameters elevated or problematic and pharmacist recommends non-drug therapy; requesting laboratory monitoring to be completed |
| 0 | Unsure |
| 10 | Not a DTP |
References
- Ronksley, P.E.; Sanmartin, C.; Campbell, D.J.; Weaver, R.G.; Allan, G.M.; McBrien, K.A.; Tonelli, M.; Manns, B.J.; Hennessy, D.; Hemmelgarn, B.R. Perceived barriers to primary care among western Canadians with chronic conditions. Health Rep. 2014, 25, 3–10. [Google Scholar] [PubMed]
- Roberts, K.C.; Rao, D.P.; Bennett, T.L.; Loukine, L.; Jayaraman, G.C. Prevalence and patterns of chronic disease multimorbidity and associated determinants in Canada. Health Promot. Chronic Dis. Prev. Can. 2015, 35, 87–94. [Google Scholar] [CrossRef] [PubMed]
- Dagli, R.J.; Sharma, A. Polypharmacy: A global risk factor for elderly people. J. Int. Oral. Health 2014, 6, i–ii. [Google Scholar]
- Jacob, L.; Breuer, J.; Kostev, K. Prevalence of chronic diseases among older patients in German general practices. Ger. Med. Sci. 2016, 14. [Google Scholar] [CrossRef]
- Lefèvre, T.; d’Ivernois, J.F.; De Andrade, V.; Crozet, C.; Lombrail, P.; Gagnayre, R. What do we mean by multimorbidity? An analysis of the literature on multimorbidity measures, associated factors, and impact on health services organization. Rev. Epidemiol. Sante Publique 2014, 62, 305–314. [Google Scholar] [CrossRef]
- Boyd, C.M.; Fortin, M. Future of Multimorbidity Research: How Should Understanding of Multimorbidity Inform Health System Design? Public Health Rev. 2010, 32, 451–474. [Google Scholar] [CrossRef]
- Navickas, R.; Petric, V.K.; Feigl, A.B.; Seychell, M. Multimorbidity: What do we know? What should we do? J. Comorb. 2016, 6, 4–11. [Google Scholar] [CrossRef]
- Johnston, M.C.; Crilly, M.; Black, C.; Prescott, G.J.; Mercer, S.W. Defining and measuring multimorbidity: A systematic review of systematic reviews. Eur. J. Public Health 2019, 29, 182–189. [Google Scholar] [CrossRef] [PubMed]
- Griffith, L.E.; Gruneir, A.; Fisher, K.; Panjwani, D.; Gafni, A.; Patterson, C.; Markle-Reid, M.; Ploeg, J. Insights on multimorbidity and associated health service use and costs from three population-based studies of older adults in Ontario with diabetes, dementia and stroke. BMC Health Serv. Res. 2019, 19, 313. [Google Scholar] [CrossRef]
- Smith, S.M.; Soubhi, H.; Fortin, M.; Hudon, C.; O’Dowd, T. Managing patients with multimorbidity: Systematic review of interventions in primary care and community settings. BMJ 2012, 354, e5205. [Google Scholar] [CrossRef] [PubMed]
- Masnoon, N.; Shakib, S.; Kalisch-Ellett, L.; Caughey, G.E. What is polypharmacy? A systematic review of definitions. BMC Geriatr. 2017, 17, 230. [Google Scholar] [CrossRef] [PubMed]
- Van den Akker, M.; Buntinx, F.; Metsemakers, J.F.; Roos, S.; Knottnerus, J.A. Multimorbidity in general practice: Prevalence, incidence, and determinants of co-occurring chronic and recurrent diseases. J. Clin. Epidemiol. 1998, 51, 367–375. [Google Scholar] [CrossRef]
- Wehling, M. Multimorbidity and polypharmacy: How to reduce the harmful drug load and yet add needed drugs in the elderly? Proposal of a new drug classification: Fit for the aged. J. Am. Geriatr. Soc. 2009, 57, 560–561. [Google Scholar] [CrossRef]
- Hajjar, E.R.; Cafiero, A.C.; Hanlon, J.T. Polypharmacy in elderly patients. Am. J. Geriatr. Pharmacother. 2007, 5, 345–351. [Google Scholar] [CrossRef]
- Kwan, D.; Farrell, B. Polypharmacy: Optimizing medication use in elderly patients. Can. Geriatr. J. 2014, 4, 21–27. [Google Scholar]
- Bushardt, R.L.; Massey, E.B.; Simpson, T.W.; Ariail, J.C.; Simpson, K.N. Polypharmacy: Misleading, but manageable. Clin. Interv. Aging 2008, 3, 383–389. [Google Scholar] [CrossRef] [PubMed]
- Maher, R.L.; Hanlon, J.; Hajjar, E.R. Clinical consequences of polypharmacy in elderly. Exp. Opin. Drug Saf. 2014, 13, 57–65. [Google Scholar] [CrossRef] [PubMed]
- Freund, J.; Meiman, J.; Kraus, C. Using electronic medical record data to characterize the level of medication use by age-groups in a network of primary care clinics. J. Prim. Care Commun. Health 2013, 4, 286–293. [Google Scholar] [CrossRef]
- Mangin, D.; Bahat, G.; Golomb, B.A.; Mallery, L.H.; Moorhouse, P.; Onder, G.; Petrovic, M.; Garfinkel, D. International Group for Reducing Inappropriate Medication Use & Polypharmacy (IGRIMUP): Position Statement and 10 Recommendations for Action. Drugs Aging 2018, 35, 575–587. [Google Scholar] [CrossRef]
- Van den Akker, M.; Buntinx, F.; Roos, S.; Knottnerus, J.A. Problems in determining occurrence rates of multimorbidity. J. Clin. Epidemiol. 2001, 54, 675–679. [Google Scholar] [CrossRef]
- Boult, C.; Wieland, G.D. Comprehensive primary care for older patients with multiple chronic conditions: “Nobody rushes you through”. JAMA 2010, 304, 1936–1943. [Google Scholar] [CrossRef] [PubMed]
- Rosser, W.W.; Colwill, J.M.; Kasperski, J.; Wilson, L. Progress of Ontario’s Family Health Team model: A patient-centered medical home. Ann. Fam. Med. 2011, 9, 165–171. [Google Scholar] [CrossRef] [PubMed]
- Abdin, S.M.; Grenier-Gosselin, L.; Guénette, L. Impact of pharmacists’ interventions on the pharmacotherapy of patients with complex needs monitored in multidisciplinary primary care teams. Int. J. Pharm. Pract. 2019, 28, 75–83. [Google Scholar] [CrossRef]
- Beuscart, J.B.; Petit, S.; Gautier, S.; Wierre, P.; Balcaen, T.; Lefebvre, J.M.; Kambia, N.; Bertoux, E.; Mascaut, D.; Barthélémy, C.; et al. Polypharmacy in older patients: Identifying the need for support by a community pharmacist. BMC Geriatr. 2019, 19, 277. [Google Scholar] [CrossRef] [PubMed]
- Canadian Pharmacists Association. Pharmacists Scope of Practice in Canada. Available online: https://www.pharmacists.ca/cpha-ca/assets/Image/pharmacy-in-canada/Scope-of-Practice-in-Canada_May2020.jpg (accessed on 22 June 2020).
- Ontario College of Pharmacists. Initiating, Adapting and Renewing Prescriptions. Available online: https://www.ocpinfo.com/regulations-standards/practice-policies-guidelines/adapting-renewing-prescriptions/ (accessed on 22 June 2020).
- Gillespie, U.; Dolovich, L.; Dahrouge, S. Activities performed by pharmacists integrated in family health teams: Results from a web-based survey. Can. Pharm. J. 2017, 150, 407–416. [Google Scholar] [CrossRef]
- Hatah, E.; Braund, R.; Duffull, S.; Tordoff, J. General practitioners ‘views of pharmacists’ current and potential contributions to medication review and prescribing in New Zealand. J. Prim. Health Care 2013, 5, 223–233. [Google Scholar] [CrossRef]
- Ontario Primary Care Team Pharmacists. OPEN Network. Available online: http://www.ontarioprimarycareteampharmacists.ca/ (accessed on 22 June 2020).
- Harris, P.A.; Taylor, R.; Minor, B.L.; Elliott, V.; Fernandez, M.; O’Neal, L.; McLeod, L.; Delacqua, G.; Delacqua, F.; Kirby, J.; et al. REDCap Consortium. The REDCap consortium: Building an international community of software platform partners. J. Biomed. Inf. 2019, 95, 103208. [Google Scholar] [CrossRef]
- Kennie, N.; Dolovich, L. Reliability testing of a case-leveling framework for assigning level of difficulty of pharmacist’s initial patient medication assessments. J. Am. Pharm. Assoc. 2008, 48, 640–647. [Google Scholar] [CrossRef]
- Cippole, R.; Strand, L.; Morley, P. Pharmaceutical Care Practice: The Patient Centered Approach to Medication Management, 3rd ed.; McGraw Hill Education: New York, NY, USA, 2012. [Google Scholar]
- Strand, L.M.; Morley, P.C.; Cipolle, R.J.; Ramsey, R.; Lamsam, G.D. Drug-related problems: Their structure and function. DICP 1990, 24, 1093–1097. [Google Scholar] [CrossRef]
- American Society of Health-System Pharmacists. Suggested definitions and relationships among medication misadventures, medication errors, adverse drug events and adverse drug reactions. Am. J. Health Syst. Pharm. 1998, 55, 165–166. [Google Scholar] [CrossRef]
- Willcox, S.M.; Himmelstein, D.U.; Woolhandler, S. Inappropriate drug prescribing for the community-dwelling elderly. JAMA 1994, 272, 292–296. [Google Scholar] [CrossRef] [PubMed]
- Steinman, M.A.; Fick, D.M. Using Wisely: A Reminder on the Proper Use of the American Geriatrics Society Beers Criteria®. J. Am. Geriatr. Soc. 2019, 67, 644–646. [Google Scholar] [CrossRef] [PubMed]
- By the 2019 American Geriatrics Society Beers Criteria® Update Expert Panel. American Geriatrics Society 2019 Updated AGS Beers Criteria® for Potentially Inappropriate Medication Use in Older Adults. J. Am. Geriatr. Soc. 2019, 67, 674–694. [Google Scholar] [CrossRef] [PubMed]
- Roux, B.; Sirois, C.; Simard, M.; Gagnon, M.E.; Laroche, M.L. Potentially inappropriate medications in older adults: A population-based cohort study. Fam. Pract. 2020, 37, 173–179. [Google Scholar] [CrossRef]
- Trumic, E.; Pranjic, N.; Begic, L.; Bečić, F. Prevalence of polypharmacy and drug interaction among hospitalized patients: Opportunities and responsabilities in pharmaceutical care. Mater. Sociomed. 2012, 24, 68–72. [Google Scholar] [CrossRef]
- Viktil, K.K.; Blix, H.S.; Moger, T.A.; Reikvam, A. Polypharmacy as commonly defined is an indicator of limited value in the assessment of drug-related problems. Br. J. Clin. Pharmacol. 2007, 63, 187–195. [Google Scholar] [CrossRef]
- Nolan, L.; O’Malley, K. Prescribing for the elderly: Part I. Sensitivity of the elderly to adverse drug reactions. J. Am. Geriatr. Soc. 1988, 36, 142–149. [Google Scholar] [CrossRef]
- Kellaway, G.S.; McCrae, E. Intensive monitoring for adverse drug effects in patients discharged from acute medical wards. N. Z. Med. J. 1973, 78, 525–528. [Google Scholar] [PubMed]
- Rambhade, S.; Chakarborty, A.; Shrivastava, A.; Patil, U.K.; Rambhade, A. A survey on polypharmacy and use of inappropriate medications. Toxicol. Int. 2012, 19, 68–73. [Google Scholar] [CrossRef]
- Kohn, L.; Corrigan, J.; Donaldson, M. To err is Human: Building a Safer Health System; Institute of Medicine National Academy Press: Washington, DC, USA, 1999. [Google Scholar]
- Stawicki, S.P.; Gerlach, A.T. Polypharmacy and medication errors: Stop, listen, look, and analyze. Opus 2009, 12, 6–10. [Google Scholar]
- Chau, S.H.; Jansen, A.P.; van de Ven, P.M.; Hoogland, P.; Elders, P.J.; Hugtenburg, J.G. Clinical medication reviews in elderly patients with polypharmacy: A cross-sectional study on drug-related problems in the Netherlands. Int. J. Clin. Pharm. 2016, 38, 46–53. [Google Scholar] [CrossRef]
- Government of Ontario. Improving Health Care in Ontario. Available online: https://www.ontario.ca/page/improving-health-care-ontario#:~:text=One%20agency,oversee%20the%20health%20care%20system (accessed on 22 June 2020).
- Thompson, J.F.; McGhan, W.F.; Ruffalo, R.L.; Cohen, D.A.; Adamcik, B.; Segal, J.L. Clinical pharmacists prescribing drug therapy in a geriatric setting: Outcome of a trial. J. Am. Geriatr. Soc. 1984, 32, 154–159. [Google Scholar] [CrossRef]
- Jameson, J.; VanNoord, G.; Vanderwoud, K. The impact of a pharmacotherapy consultation on the cost and outcome of medical therapy. J. Fam. Pract. 1995, 41, 469–472. [Google Scholar]
- Lim, W.S.; Low, H.N.; Chan, S.P.; Chen, H.N.; Ding, Y.Y.; Tan, T.L. Impact of a pharmacist consult clinic on a hospital-based geriatric outpatient clinic in Singapore. Ann. Acad. Med. Singap. 2004, 33, 220–227. [Google Scholar] [PubMed]
- Chumney, E.C.; Robinson, L.C. The effects of pharmacist interventions on patients with polypharmacy. Pharm. Prac. 2006, 4, 103. [Google Scholar]
- Riordan, D.O.; Walsh, K.A.; Galvin, R.; Sinnott, C.; Kearney, P.M.; Byrne, S. The effect of pharmacist-led interventions in optimising prescribing in older adults in primary care: A systematic review. SAGE Open Med. 2016, 4, 2050312116652568. [Google Scholar] [CrossRef] [PubMed]
- Hazen, A.C.; De Bont, A.A.; Boelman, L.; Zwart, D.L.; De Gier, J.J.; De Wit, N.J.; Bouvy, M.L. The degree of integration of non-dispensing pharmacists in primary care practice and the impact on health outcomes: A systematic review. Res. Soc. Adm. Pharm. 2018, 14, 228–240. [Google Scholar] [CrossRef] [PubMed]
- Steele, K.M.; Ruisinger, J.F.; Bates, J.; Prohaska, E.S.; Melton, B.L.; Hipp, S. Home-Based Comprehensive Medication Reviews: Pharmacist’s Impact on Drug Therapy Problems in Geriatric Patients. Consult. Pharm. 2016, 31, 598–605. [Google Scholar] [CrossRef] [PubMed]
- McDonough, R.P.; Doucette, W.R. Drug therapy management: An empirical report of drug therapy problems, pharmacists’ interventions, and results of pharmacists’ actions. J. Am. Pharm. Assoc. 2003, 43, 511–518. [Google Scholar] [CrossRef]
- Freeman, C.R.; Cottrell, W.N.; Kyle, G.; Williams, I.D.; Nissen, L. An evaluation of medication review reports across different settings. Int. J. Clin. Pharm. 2013, 35, 5–13. [Google Scholar] [CrossRef]
- Sorensen, L.; Stokes, J.A.; Purdie, D.M.; Woodward, M.; Elliott, R.; Roberts, M.S. Medication reviews in the community: Results of a randomized, controlled effectiveness trial. Br. J. Clin. Pharmacol. 2004, 58, 648–664. [Google Scholar] [CrossRef] [PubMed]
- Butterworth, J.; Sansom, A.; Sims, L.; Healey, M.; Kingsland, E.; Campbell, J. Pharmacists’ perceptions of their emerging general practice roles in UK primary care: A qualitative interview study. Br. J. Gen. Pract. 2017, 67, e650–e658. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | Mean (SD) N: % (N = 237) |
|---|---|
| Age (in years) | 67.9 (13.9) |
| Female | 54.8% |
| Number of Prescription Medications | 9.2 (4.7) |
| History of MedsCheck in the past year | 11.4% |
| History of Health Service Utilization, Past Month (ER visit or hospital discharge) | 21% |
| Mean | Standard Deviation | Max Value | Min Value | |
|---|---|---|---|---|
| Prescription | 9.2 | 4.7 | 25 | 3 |
| Over the Counter | 2.1 | 2.3 | 20 | 0 |
| Natural or Herbal Products | 0.4 | 0.9 | 7 | 0 |
| Other | 0.1 | 0.8 | 9 | 0 |
| Type of Discrepancy | Number of Patients with at least One Discrepancy Identified * | % (of Total Patients with at least One Discrepancy Identified) |
|---|---|---|
| Drug Name | 74 | 31.2 |
| Drug Dose | 51 | 21.5 |
| Drug Frequency | 31 | 13.1 |
| Other | 20 | 8.4 |
| Type of DTPs | Number of DTPs Identified | % (of Total DTPs) | |
|---|---|---|---|
| Type 1 | Receiving/taking drug with no valid indication | 114 | 13.3 |
| Type 2 | Requires drug therapy for an indication and is not receiving/taking therapy | 194 | 22.6 |
| Type 3 | Not receiving/taking appropriate drug or drug product | 121 | 14.1 |
| Type 4 | Receiving/taking too little drug | 75 | 8.7 |
| Type 5 | Receiving/taking too much drug | 93 | 10.8 |
| Type 6 | Not receiving/taking prescribed drugs appropriately | 105 | 12.2 |
| Type 7 | Experiencing an adverse drug reaction (not dose-related) | 91 | 10.6 |
| Type 8 | Experiencing a drug–drug, drug–food, or drug–laboratory reaction | 29 | 3.4 |
| Type 99 (Other) i | Other | 38 | 4.4 |
| TOTAL | 860 | 100 |
| Type of DTP | Number of Patients with at least One DTP Identified * | % (of Total Patients with at least One DTP Identified) |
|---|---|---|
| Type 1 | 65 | 27.4 |
| Type 2 | 124 | 52.3 |
| Type 3 | 60 | 25.3 |
| Type 4 | 55 | 23.2 |
| Type 5 | 66 | 27.9 |
| Type 6 | 63 | 26.6 |
| Type 7 | 61 | 25.7 |
| Type 8 | 20 | 8.4 |
| Other | 26 | 11.0 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Benny Gerard, N.; Mathers, A.; Laeer, C.; Lui, E.; Kontio, T.; Patel, P.; Dolovich, L. A Descriptive Quantitative Analysis on the Extent of Polypharmacy in Recipients of Ontario Primary Care Team Pharmacist-Led Medication Reviews. Pharmacy 2020, 8, 110. https://doi.org/10.3390/pharmacy8030110
Benny Gerard N, Mathers A, Laeer C, Lui E, Kontio T, Patel P, Dolovich L. A Descriptive Quantitative Analysis on the Extent of Polypharmacy in Recipients of Ontario Primary Care Team Pharmacist-Led Medication Reviews. Pharmacy. 2020; 8(3):110. https://doi.org/10.3390/pharmacy8030110
Chicago/Turabian StyleBenny Gerard, Nichelle, Annalise Mathers, Christoph Laeer, Eric Lui, Tom Kontio, Payal Patel, and Lisa Dolovich. 2020. "A Descriptive Quantitative Analysis on the Extent of Polypharmacy in Recipients of Ontario Primary Care Team Pharmacist-Led Medication Reviews" Pharmacy 8, no. 3: 110. https://doi.org/10.3390/pharmacy8030110
APA StyleBenny Gerard, N., Mathers, A., Laeer, C., Lui, E., Kontio, T., Patel, P., & Dolovich, L. (2020). A Descriptive Quantitative Analysis on the Extent of Polypharmacy in Recipients of Ontario Primary Care Team Pharmacist-Led Medication Reviews. Pharmacy, 8(3), 110. https://doi.org/10.3390/pharmacy8030110






