Preparing Pharmacists to Care for Patients Exposed to Intimate Partner Violence
Abstract
1. Introduction
2. Materials and Methods
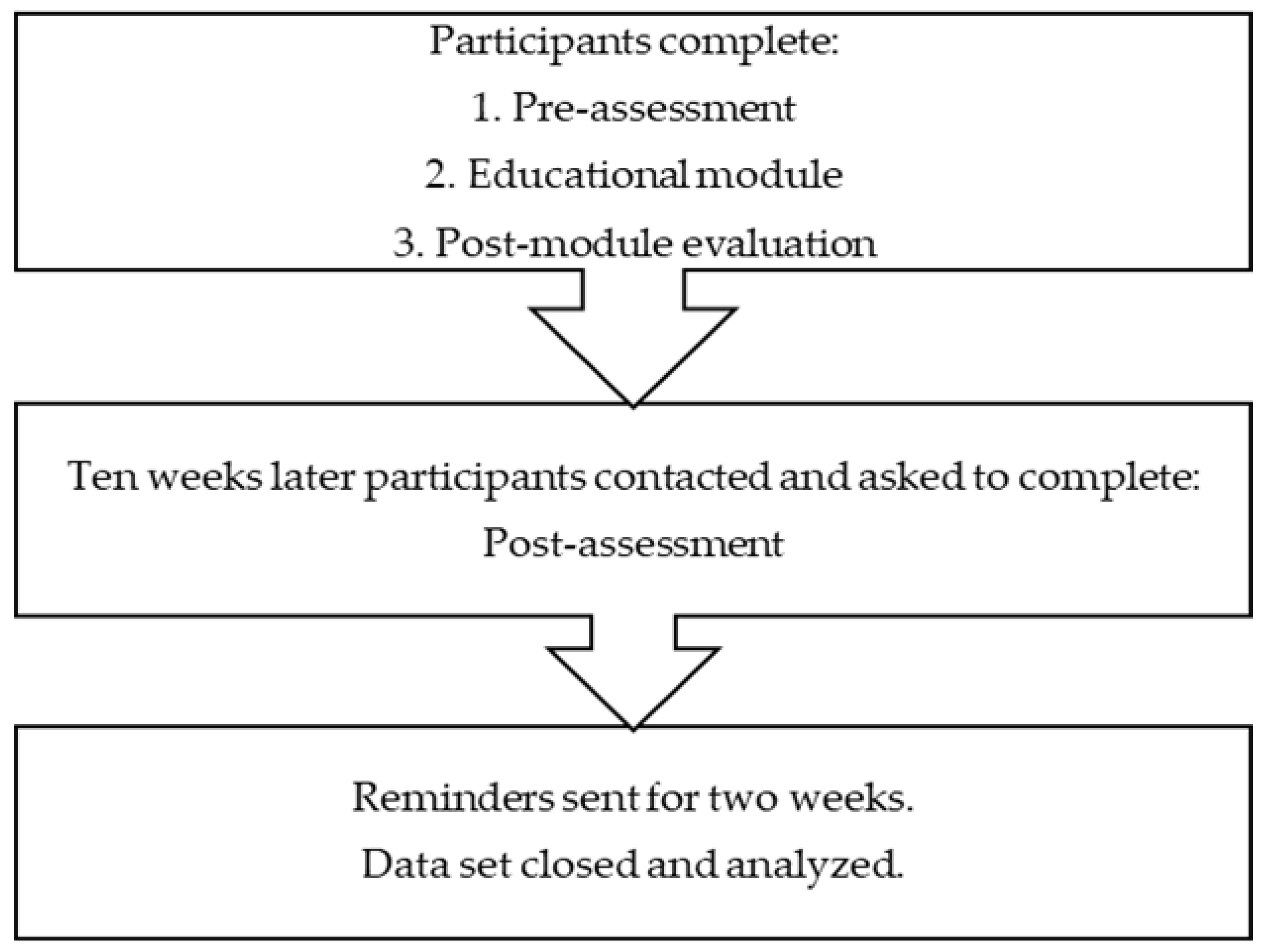
2.1. Study Design
2.2. Educational Module
- Increase knowledge and awareness of intimate partner violence (IPV).
- Identify the impact IPV has on patient health and health care utilization.
- Identify misinformation about IPV.
- Prepare for how to handle a patient who discloses IPV in the pharmacy setting.
- Identify two follow-up strategies to increase your capacity to respond to patients exposed to IPV.
2.3. Participants
2.4. Measurement Tools
2.5. Data Collection
2.6. Data Analysis
3. Results
3.1. Participant Characteristics and Prior IPV Training Experience
3.2. Module Evaluation
3.3. PREMIS for Pharmacists Scales
3.4. Pharmacists’ Perspectives on IPV and Pharmacy Practice
3.5. Positive Steps toward Change
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Breiding, M.J.; Smith, S.G.; Basile, K.C.; Walters, M.L.; Chen, J.; Merrick, M.T. Prevalence and Characteristics of Sexual Violence, Stalking, and Intimate Partner Violence Victimization—National Intimate Partner and Sexual Violence Survey, United States, 2011. MMWR Morb. Mortal. Wkly. Rep. 2014, 63, 1–18. [Google Scholar]
- Vos, T.; Astbury, J.; Piers, L.S.; Magnus, A.; Heenan, M.; Stanley, L.; Walker, L.; Webster, K. Measuring the impact of intimate partner violence on the health of women in Victoria, Australia. Bull. World Health Organ. 2006, 84, 739–744. [Google Scholar] [CrossRef] [PubMed]
- Coker, A.L.; Davis, K.E.; Arias, I.; Desai, S.; Sanderson, M.; Brandt, H.M.; Smith, P.H. Physical and mental health effects of intimate partner violence for men and women. Am. J. Prev. Med. 2002, 23, 260–268. [Google Scholar] [CrossRef]
- Coker, A.L.; Hopenhayn, C.; DeSimone, C.P.; Bush, H.M.; Crofford, L. Violence against Women Raises Risk of Cervical Cancer. J. Womens Health (Larchmt) 2009, 18, 1179–1185. [Google Scholar] [CrossRef] [PubMed]
- Corrigan, J.D.; Wolfe, M.; Mysiw, W.J.; Jackson, R.D.; Bogner, J.A. Early identification of mild traumatic brain injury in female victims of domestic violence. Am. J. Obstet. Gynecol. 2003, 188, S71–S76. [Google Scholar] [CrossRef] [PubMed]
- Drossman, D.A.; Talley, N.J.; Leserman, J.; Olden, K.W.; Barreiro, M.A. Sexual and physical abuse and gastrointestinal illness. Review and recommendations. Ann. Intern. Med. 1995, 123, 782–794. [Google Scholar] [CrossRef] [PubMed]
- Lopez, E.J.; Jones, D.L.; Villar-Loubet, O.M.; Arheart, K.L.; Weiss, S.M. Violence, coping, and consistent medication adherence in HIV-positive couples. AIDS Educ. Prev. 2010, 22, 61–68. [Google Scholar] [CrossRef] [PubMed]
- Berenson, A.B.; Wiemann, C.M.; Wilkinson, G.S.; Jones, W.A.; Anderson, G.D. Perinatal morbidity associated with violence experienced by pregnant women. Am. J. Obstet. Gynecol. 1994, 170, 1760–1766. [Google Scholar] [CrossRef]
- Bonomi, A.E.; Anderson, M.L.; Rivara, F.P.; Thompson, R.S. Health outcomes in women with physical and sexual intimate partner violence exposure. J. Womens Health (Larchmt) 2007, 16, 987–997. [Google Scholar] [CrossRef] [PubMed]
- Cokkinides, V.E.; Coker, A.L.; Sanderson, M.; Addy, C.; Bethea, L. Physical violence during pregnancy: Maternal complications and birth outcomes. Obstet. Gynecol. 1999, 93, 661–666. [Google Scholar] [CrossRef] [PubMed]
- McFarlane, J.; Parker, B.; Soeken, K.; Bullock, L. Assessing for abuse during pregnancy. Severity and frequency of injuries and associated entry into prenatal care. JAMA 1992, 267, 3176–3178. [Google Scholar] [CrossRef] [PubMed]
- Bonomi, A.E.; Anderson, M.L.; Rivara, F.P.; Thompson, R.S. Health Care Utilization and Costs Associated with Physical and Nonphysical-Only Intimate Partner Violence. Health Serv. Res. 2009, 44, 1052–1067. [Google Scholar] [CrossRef] [PubMed]
- Sterling, S.; Chi, F.; Weisner, C.; Grant, R.; Pruzansky, A.; Bui, S.; Madvig, P.; Pearl, R. Association of behavioral health factors and social determinants of health with high and persistently high healthcare costs. Prev. Med. Rep. 2018, 11, 154–159. [Google Scholar] [CrossRef] [PubMed]
- National Center for Injury Prevention and Control. Costs of Intimate Partner Violence against Women in the United States; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2003.
- Rivara, F.P.; Anderson, M.L.; Fishman, P.; Bonomi, A.E.; Reid, R.J.; Carrell, D.; Thompson, R.S. Intimate partner violence and health care costs and utilization for children living in the home. Pediatrics 2007, 120, 1270–1277. [Google Scholar] [CrossRef] [PubMed]
- Bauer, N.S.; Gilbert, A.L.; Carroll, A.E.; Downs, S.M. Associations between early exposure to intimate partner violence, parental depression and subsequent mental health outcomes. JAMA Pediatr. 2013, 167, 341–347. [Google Scholar] [CrossRef] [PubMed]
- Chai, J.; Fink, G.; Kaaya, S.; Danaei, G.; Fawzi, W.; Ezzati, M.; Lienert, J.; Smith Fawzi, M.C. Association between intimate partner violence and poor child growth: Results from 42 demographic and health surveys. Bull. World Health Organ. 2016, 94, 331–339. [Google Scholar] [CrossRef] [PubMed]
- Position statement on physical violence against women. Am. Nurse 1992, 24, 8.
- Yawn, B.P.; Yawn, R.A.; Uden, D.L. American Medical Association diagnostic and treatment guidelines on domestic violence. Arch. Fam. Med. 1992, 1, 39. [Google Scholar]
- Smith, M.A. Pharmacists and the primary care workforce. Ann. Pharmacother. 2012, 46, 1568–1571. [Google Scholar] [CrossRef] [PubMed]
- Goode, J.-V.; Owen, J.; Page, A.; Gatewood, S. Community-Based Pharmacy Practice Innovation and the Role of the Community-Based Pharmacist Practitioner in the United States. Pharmacy 2019, 7, 106. [Google Scholar] [CrossRef] [PubMed]
- Mospan, C.M. Pharmacists as women’s health providers: Increasing access to contraception and preconception care. J. Am. Pharm. Assoc. 2019. [Google Scholar] [CrossRef] [PubMed]
- Cerulli, C.; Cerulli, J.; Santos, E.J.; Lu, N.; He, H.; Kaukeinen, K.; White, A.M.; Tu, X. Does the Health Status of Intimate Partner Violence Victims Warrant Pharmacies as Portals for Public Health Promotion? J. Am. Pharm Assoc. 2010, 50, 200–206. [Google Scholar] [CrossRef] [PubMed]
- Gadomski, A.M.; Wolff, D.; Tripp, M.; Lewis, C.; Short, L.M. Changes in health care providers’ knowledge, attitudes, beliefs, and behaviors regarding domestic violence, following a multifaceted intervention. Acad. Med. 2001, 76, 1045–1052. [Google Scholar] [CrossRef] [PubMed]
- Lapidus, G.; Cooke, M.B.; Gelven, E.; Sherman, K.; Duncan, M.; Banco, L. A statewide survey of domestic violence screening behaviors among pediatricians and family physicians. Arch. Pediatr. Adolesc. Med. 2002, 156, 332–336. [Google Scholar] [CrossRef] [PubMed]
- Sugg, N.K.; Thompson, R.S.; Thompson, D.C.; Maiuro, R.; Rivara, F.P. Domestic violence and primary care. Attitudes, practices, and beliefs. Arch. Fam Med. 1999, 8, 301–306. [Google Scholar] [CrossRef] [PubMed]
- Garimella, R.; Plichta, S.B.; Houseman, C.; Garzon, L. Physician beliefs about victims of spouse abuse and about the physician role. J. Womens Health Gend. Based. Med. 2000, 9, 405–411. [Google Scholar] [CrossRef] [PubMed]
- Barnard, M.; West-Strum, D.; Holmes, E.; Yang, Y.; Swain, K.A. Community Pharmacists’ Awareness of Intimate Partner Violence: An Exploratory Study. Innov. Pharm. 2013, 4, 106. [Google Scholar] [CrossRef][Green Version]
- Hilverding, A.T.; DiPietro Mager, N.A. Pharmacists’ attitudes regarding provision of sexual and reproductive health services. J. Am. Pharm Assoc. 2017, 57, 493–497. [Google Scholar] [CrossRef] [PubMed]
- Ford, J.; Murphy, J.E. Chain pharmacists’ attitudes on and awareness of domestic abuse. J. Am. Pharm Assoc. 1996, NS36, 323–328. [Google Scholar] [CrossRef]
- McAndrew, M.; Pierre, G.C.; Kojanis, L.C. Effectiveness of an Online Tutorial on Intimate Partner Violence for Dental Students: A Pilot Study. J. Dent. Educ. 2014, 78, 1176–1181. [Google Scholar] [PubMed]
- Connor, P.D.; Nouer, S.S.; Speck, P.M.; Mackey, S.N.; Tipton, N.G. Nursing Students and Intimate Partner Violence Education: Improving and Integrating Knowledge into Health Care Curricula. J. Prof. Nurs. 2013, 29, 233–239. [Google Scholar] [CrossRef] [PubMed]
- Wood, L. Simulation as a Training Tool for Intimate Partner Violence Screenings. Clin. Simul. Nurs. 2016, 12, 8–15. [Google Scholar] [CrossRef]
- Zachor, H.; Chang, J.C.; Zelazny, S.; Jones, K.A.; Miller, E. Training reproductive health providers to talk about intimate partner violence and reproductive coercion: An exploratory study. Health Educ Res. 2018, 33, 175–185. [Google Scholar] [CrossRef] [PubMed]
- Alshammari, K.F.; McGarry, J.; Higginbottom, G.M.A. Nurse education and understanding related to domestic violence and abuse against women: An integrative review of the literature. Nurs. Open 2018, 5, 237–253. [Google Scholar] [CrossRef] [PubMed]
- Kottasova, I.; DiDonato, V. Women are Using Code Words at Pharmacies to Escape Domestic Violence. Available online: https://www.cnn.com/2020/04/02/europe/domestic-violence-coronavirus-lockdown-intl/index.html (accessed on 20 April 2020).
- Shaddish, W.; Cook, T.; Campbell, D. Experimental and Quasi-Experimental Designs for Generalized Causal Inference; Wadsworth: Belmont, CA, USA, 2002. [Google Scholar]
- Rouse, M.J. Continuing Professional Development in Pharmacy. J. Pharm. Technol. 2004, 44, 4. [Google Scholar]
- Haines, S.T. It’s Time to Dismantle CE and Build a CPI System. Am. J. Pharm. Educ. 2018, 82. [Google Scholar] [CrossRef] [PubMed]
- Kalra, N.; Tanna, G.L.D.; García-Moreno, C. Training healthcare providers to respond to intimate partner violence against women. Cochrane Database Syst. Rev. 2017. [Google Scholar] [CrossRef]
- Ambuel, B.; Trent, K.; Lenahan, P.; Cronholm, P.; Downing, D.; Jelley, M.; Lewis-O’Connor, A.; McGraw, M.; Marjavi, A.; Mouden, L.; et al. Competencies Needed by Health Professionals for Addressing Exposure to Violence and Abuse in Patient Care; Academy on Violence and Abuse: Eden Prairie, MN, USA, 2011; pp. 1–18. [Google Scholar]
- Zaher, E.; Keogh, K.; Ratnapalan, S. Effect of domestic violence training. Can. Fam. Physician 2014, 60, 618–624. [Google Scholar] [PubMed]
- Family Violence Prevention Fund. National Consensus Guidelines on Identifying and Responding to Domestic Violence Victimization in Health Care Settings; Family Violence Prevention Fund: San Francisco, CA, USA, 2004. [Google Scholar]
- Short, L.M.; Alpert, E.; Harris, J.M.; Surprenant, Z.J. A Tool for Measuring Physician Readiness to Manage Intimate Partner Violence. Am. J. Prev. Med. 2006, 30, 173–180.e19. [Google Scholar] [CrossRef] [PubMed]
- Connor, P.D.; Nouer, S.S.; Mackey, S.T.N.; Tipton, N.G.; Lloyd, A.K. Psychometric Properties of an Intimate Partner Violence Tool for Health Care Students. J. Interpers. Violence 2011, 26, 1012–1035. [Google Scholar] [CrossRef] [PubMed]
- Barnard, M.; West-Strum, D.; Yang, Y.; Holmes, E. Evaluation of a Tool to Measure Pharmacists’ Readiness to Manage Intimate Partner Violence. Pharmacy (Basel) 2018, 6, 66. [Google Scholar] [CrossRef] [PubMed]
| Scales | Total Items | Sample Items | Response Scoring |
|---|---|---|---|
| BACKGROUND | |||
| Perceived Preparation | 12 | How prepared do you feel to appropriately respond to disclosures of abuse? | Not prepared (1) to Quite well prepared (7) |
| Perceived Knowledge | 16 | How much do you feel you know about what questions to ask to identify Intimate Partner Violence (IPV)? | Nothing (1) to Very much (7) |
| Actual Knowledge | 18 | What is the strongest single risk factor for being a victim of IPV? | True/False and Multiple choice; Possible range 6–32 |
| OPINIONS | |||
| Efficacy—workplace/self | 7 | I feel comfortable discussing IPV with my patients. My practice setting allows me adequate time to response to victims of IPV. | Strong disagree (1) to Strongly agree (7) |
| Preparation | 3 | I don’t have the necessary skills to discuss abuse with an IPV victims who is female. | Strong disagree (1) to Strongly agree (7) |
| Legal Requirements | 3 | I am aware of the legal requirements in this state regarding reporting of suspected cases of IPV. | Strong disagree (1) to Strongly agree (7) |
| Alcohol & Drugs | 2 | Use of alcohol or drugs is related to IPV victimization. | Strong disagree (1) to Strongly agree (7) |
| Constraints | 3 | Pharmacists do not have the time to assist patients in addressing IPV. | Strong disagree (1) to Strongly agree (7) |
| Characteristic | % (n) |
|---|---|
| Sex | |
| Female | 52.8% (19) |
| Male | 47.2% (17) |
| Race | |
| White | 83.3% (30) |
| African American/Black | 0 |
| Asian | 11.1% (4) |
| Native Hawaiian or Pacific Islander | 0 |
| American Indian or Alaskan Native | 0 |
| Other | 5.6% (2) |
| Hispanic or Latino | 0 |
| Age, mean (SD) | 44.72 (10.48) |
| Most advanced pharmacy training | |
| B.S. Pharmacy | 52.8% (19) |
| PharmD | 41.7% (15) |
| M.S. Pharmacy | 5.6% (2) |
| Residency/Fellowship | 0 |
| Years practicing pharmacy | 20.00 (11.69) |
| Characteristic | % (n) | |
|---|---|---|
| Type of pharmacy | ||
| Chain/retail | 52.8% (19 | |
| Independent | 44.4% (16 | |
| Hospital Institutionalsetting | 5.6% (2) | |
| Specialty pharmacy | 0 | |
| Other (outpatient hospital pharmacy) | 2.8% (1) | |
| Offers advanced pharmacy services | ||
| Yes | 77.8% (28) | |
| No | 22.2% (8) | |
| Average number of fills per day in your pharmacy | 268.75 (192.94) | |
| Training Experience | % (n) |
|---|---|
| None | 80.6% (29) |
| Read institution’s protocol | 8.3% (3) |
| Watched a video | 11.1% (4) |
| Attended a lecture/talk | 8.3% (3) |
| Attended skills-based training/workshop | 2.8% (1) |
| Pharmacy/other school classroom workshop | 0 |
| Pharmacy/other school clinical training | 5.6% (2) |
| Residency/fellowship/post-grad training | 0 |
| Continuing education | 5.6% (2) |
| Other | 0 |
| Total hours of IPV-related training, Mean (SD) | 3.14 (1.8) |
| Item | % Strongly Agreed (n) | % Agreed (n) |
|---|---|---|
| I learned new information from this module | 63.9% (23) | 36.1% (13) |
| The information was presented in a logical sequence | 77.8% (28) | 22.2% (8) |
| The information presented was relevant to pharmacists | 72.2% (26) | 27.8% (10) |
| I found the module to be valuable to my general knowledge as a practitioner | 75.0% (27) | 25.0% (9) |
| PREMIS for Pharmacists Scales | PRE | POST | p Value | ||||
|---|---|---|---|---|---|---|---|
| Mean (SD) | Range | α | Mean (SD) | Range | α | ||
| BACKGROUND Scales | |||||||
| Perceived Preparation | 25.56 (13.27) | 12–56 | 0.976 | 35.86 (15.51) | 12–75 | 0.977 | <0.001 |
| Perceived Knowledge | 38.00 (18.29) | 16–100 | 0.977 | 56.81 (18.99) | 22–97 | 0.975 | <0.001 |
| Actual Knowledge | 21.11 (4.53) | 10–29 | n/a | 21.86 (5.91) | 9–30 | n/a | 0.46 |
| OPINION Scales | |||||||
| Work/Self-efficacy | 2.98 (0.96) | 1.29–5.14 | 0.770 | 3.34 (0.90) | 1.00–5.43 | 0.778 | <0.05 |
| Preparation | 2.91 (1.27) | 1–6 | 0.971 | 3.68 (1.18) | 1–6 | 0.874 | <0.05 |
| Legal Requirements | 3.42 (1.75) | 1–7 | 0.942 | 4.45 (1.39) | 1–7 | 0.910 | <0.001 |
| Alcohol and Drugs | 4.61 (0.96) | 2.5–7 | 0.653 | 4.28 (1.14) | 2.5–7 | 0.753 | 0.39 |
| Constraints | 3.82 (1.15) | 1.33–6.00 | 0.607 | 4.02 (1.10) | 1.67–5.67 | 0.678 | 0.39 |
| Item | PRE % (n) | POST % (n) |
|---|---|---|
| Practice setting has a protocol for managing IPV | 0 | 16.7% (6) |
| Provided information (phone numbers, pamphlets, other information) to patient | 8.3% (3) | 8.3% (3) |
| Counseled patient about options s/he may have | 5.6% (2) | 8.3% (3) |
| Conducted safety assessment for the victim | 2.8% (1) | 2.8% (1) |
| Conducted safety assessment for the victim’s children | 0 | 2.8% (1) |
| Helped patient develop a personal safety plan | 0 | 0 |
| Referred patient to other assistance (i.e., therapy, law enforcement, hotline, support group) | 5.6% (2) | 5.6% (2) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barnard, M.; White, A.; Bouldin, A. Preparing Pharmacists to Care for Patients Exposed to Intimate Partner Violence. Pharmacy 2020, 8, 100. https://doi.org/10.3390/pharmacy8020100
Barnard M, White A, Bouldin A. Preparing Pharmacists to Care for Patients Exposed to Intimate Partner Violence. Pharmacy. 2020; 8(2):100. https://doi.org/10.3390/pharmacy8020100
Chicago/Turabian StyleBarnard, Marie, Aaron White, and Alicia Bouldin. 2020. "Preparing Pharmacists to Care for Patients Exposed to Intimate Partner Violence" Pharmacy 8, no. 2: 100. https://doi.org/10.3390/pharmacy8020100
APA StyleBarnard, M., White, A., & Bouldin, A. (2020). Preparing Pharmacists to Care for Patients Exposed to Intimate Partner Violence. Pharmacy, 8(2), 100. https://doi.org/10.3390/pharmacy8020100





