Development of a Platform to Align Education and Practice: Bridging Academia and the Profession in Portugal
Abstract
1. Introduction
- on the academic side, aiming to influence the innovation in teaching methods; and
- on the professional side, aiming to collect information about key competences for each practice area that need to be ensured through life-long learning, in order to have a competent pharmaceutical workforce.
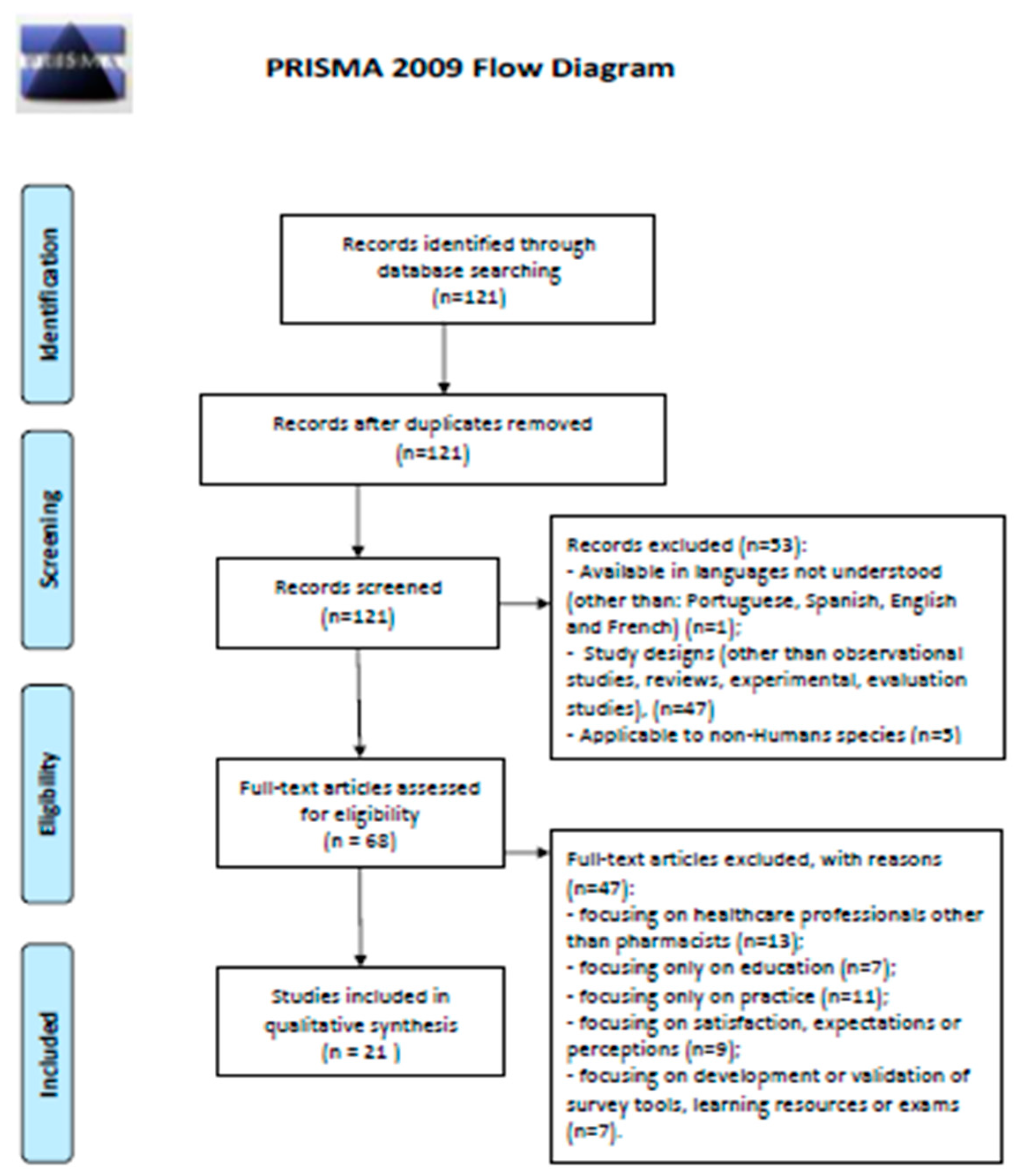
2. Materials and Methods
2.1. Narrative Review
2.2. Workshop Activities
2.3. Involvement in International Events
2.4. Answering to Global Requests
2.5. Answering to National Needs
3. Results
3.1. Literature Review
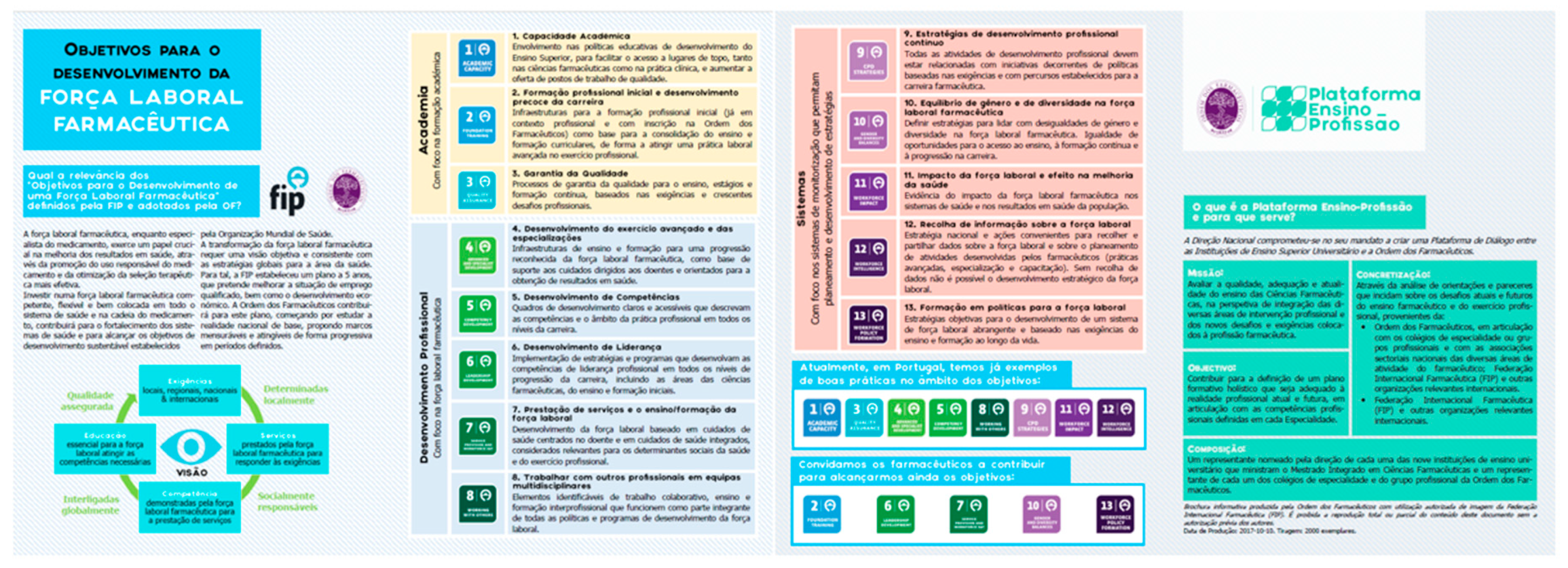
3.2. Establishing the Platform
3.3. Workshop Activities
3.4. Involvement in International Events
3.5. Answering to Global Requests
3.6. Answering to National Needs
4. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| Author, Year | Focus | Summary Description | |
|---|---|---|---|
| 1 | Bulkley, 2017 [22] | Internship/ Residency | Literature review led to identify thre strategies to improve residency training. Of highlight is the formatting of training for use across all residency programs. |
| 2 | Kim, 2017 [23] | Evaluation methods for competency assurance | Survey study suggesting skills tests are necessary to evaluate professional competencies, and that the assessor should be an academic with clinical experience. |
| 3 | Katajavuori, 2017 [17] | Curriculum shaping to professional needs | Describes a curricular reform (Big Wheel) undertaken in 2015 in Helsinki, based on the identification on relevant learning outcomes for professional activities by experts from various fields of practice. Innovative teaching practices were generated in cooperation with all stakeholders, including students. |
| 4 | Gallagher, 2010 [8] | Curriculum shaping to professional needs | Defends how changes in professional practice and accountability must inform the undergraduate curriculum so that they are fit for new challenges when they graduate. This is the approach taken by the Council of the Pharmaceutical Society of Ireland, and which led to the inclusion of vaccination in undergraduate education subsequent to practice changes led by legislation. |
| 5 | Wilbur, 2017 [24] | Identification of gaps | Identifies chart documentation as one of the skills pharmacists are poorer at, aiming to align education with practice needs. |
| 6 | Karim, 2015 [25] | Identification of gaps | Through a knowledge-based survey, it is shown that although most were “average”, only 30% execute the task of interest on admission and 50% during hospitalization (nutrition) |
| 7 | Jacobs, 2013 [26] | Failures in revalidation process | Through interviews with regulatory agencies and pharmacy commissioners, it is demonstrated that during the monitoring and inspection needed for revalidation, the main focus is out on the premises, and not the individual pharmacist. |
| 8 | Wittman, 2017 [27] | Targeting training for pharmaceutical industry | Describes a program set to improve critical appraisal skills based on needs identified by the pharmaceutical industry for their workforce. |
| 9 | Tchen, 2018 [28] | Internship/ Residency | Describes an online resource to facilitate transition from classroom to internships; considered by 70% to have impacted on their performance. |
| 10 | Bellottie, 2018 [29] | Targeting training for laboratory | Focuses on assessment models that may be used incorporating practice laboratories to demonstrate readiness for Advanced Pharmacy Practice Experiences, a standard compulsory level for this practice area. |
| 11 | Kennedy, 2018 [30] | Identification of gaps | Identifies pharmacogenomics as a specific area for which pharmacists are not completely ready for current challenges, suggesting a transformative journey needed in education in training. |
| 12 | Aucoin, 2005 [31] | Identification of gaps | Suggests specific targets in education (≥25 hours) and training (min one rotation) for core pediatric areas to be fit for practice in this area. |
| 13 | Brown, 2013 [32] | Health System Failures | Focuses on workforce challenges and how new pedagogical approaches are needed to train other professionals involved in essential medicines supply, particularly in areas where 80% of access cannot ensure a pharmacist present. Sets up principles for the pharmaceutical training of such professionals. |
| 14 | Dean, 2014 [33] | Specific competences | Reviews the development of interprofessional educational diabetes teams achieved over 6 years in Canada, suggesting as key elements: collaborative practice as part of the curriculum, having teams involving students and preceptors, and strong institutional support. |
| 15 | Buna, 2011 [34] | Internship/ Residency | Assesses the effect of residency training on pharmacy careers, and concludes that for a majority, these allowed hospital pharmacists to acquire core competencies, highlighting the development of direct patient care skills. |
| 16 | O’Neil, 2007 [35] | Internship/ Residency | Describes how experiential rotations were perceived to significantly enhance students’ preparedness for practice and even self-confidence in their skills. |
| 17 | Fowler, 2018 [36] | Improving quality in practice while teaching students | Used students as observers for the quality improvement of a set of tasks developed by a hospital-based team, showing an improvement in the observational capacity of students, whilst contributing to improved practice, i.e., a win-win situation. |
| 18 | Cardiff, 2018 [37] | Specific competences | Describes a prescribing program complemented with mandatory supervised training developed to meet national competency standards. |
| 19 | Kassam, 2006 [38] | Internship/ Residency | Analyzes the learning opportunities of students during their community pharmacy internships, concluding that they were all involved in prescription refill and in consultations for non-prescription drugs, although there were limited experiences in pharmaceutical care (monitoring patients), or even in shadowing other healthcare professionals. |
| 20 | Pelly, 2010 [39] | Specific competences | Assessing the immunization curriculum content in various schools, Pelly et al. found a wide variability in time spent between and within disciplines; moreover, during training, only 20% perceived that their teaching had been adequate, highlighting important gaps that impact on practice. |
| 21 | Sihavong, 2007 [40] | Specific competences | Competencies of community pharmacists in rural Laos were evaluated using written clinical scenarios to describe management of reproductive tract infections. Results suggest that over 85% provided inadequate health education, leaving it clear that to improve practice continuous education must be made available. |
References
- Anderson, S. The state of the world’s pharmacy: A portrait of the pharmacy profession. J. Interprof. Care 2002, 16, 391–404. [Google Scholar] [CrossRef] [PubMed]
- Albanese, N.P.; Rouse, M.J.; Schlaifer, M.; Council on Credentialing in Pharmacy. Scope of contemporary pharmacy practice: Roles, responsibilities, and functions of pharmacists and pharmacy technicians. J. Am. Pharm. Assoc. 2010, 50, e35–e69. [Google Scholar] [CrossRef] [PubMed]
- Soares, I.B.; Imfeld-Isenegger, T.L.; Makovec, U.N.; Horvat, N.; Kos, M.; Arnet, I.; Hersberger, K.E.; Costa, F.A. A survey to assess the availability, implementation rate and remuneration of pharmacist-led cognitive services throughout Europe. Res. Soc. Admin. Pharm. 2020, 16, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Aldeen, A.Z.; Quattromani, E.N.; Williamson, K.; Hartman, N.D.; Wheaton, N.B.; Branzetti, J.B. Faculty Prediction of In-Training Examination Scores of Emergency Medicine Residents: A Multicenter Study. J. Emerg. Med. 2015, 49, 64–69. [Google Scholar] [CrossRef]
- Bruno, A.; Bates, I.; Brock, T.; Anderson, C. Towards a Global Competency Framework. Am. J. Pharm. Educ. 2010, 74, 56. [Google Scholar] [CrossRef]
- Competency Development Evaluation Group. GLF–General Level Framework. A Framework for Pharmacist Development in General Pharmacy Practice, 2nd ed.; Competency Development Evaluation Group: London, UK, 2007. [Google Scholar]
- Competency Development and Evaluation Group. Advanced to Consultant Level Framework: A Developmental Framework for Pharmacists Progressing to Advanced Levels of Practice; CoDEG: London, UK, 2009; Available online: http://www.codeg.org/fileadmin/codeg/pdf/ACLF.pdf (accessed on 15 February 2019).
- Gallagher, H.C. New fitness-to-practice requirements for pharmacists in Ireland: Implications for undergraduate pharmacy education. Med. Teach. 2010, 32, e71–e77. [Google Scholar] [CrossRef]
- Kirton, S.B.; Kravitz, L. Objective Structured Clinical Examinations (OSCEs) compared with traditional assessment methods. Am. J. Pharm. Educ. 2011, 75, 111. [Google Scholar] [CrossRef] [PubMed]
- Competências Farmacêuticas e Atribuição de Especialidades. Modelo de Competências Farmacêuticas. V12. Lisboa, 16 October 2014. Available online: https://www.ordemfarmaceuticos.pt/fotos/documentos/competencias_e_especia_18767615595bc99d944a3.pdf (accessed on 16 February 2019).
- Competências Farmacêuticas para Assuntos Regulamentares. Versão 23.11.15. Available online: https://www.ordemfarmaceuticos.pt/fotos/documentos/ar_677588552595bc9ba2a8c2.pdf (accessed on 16 February 2019).
- Competências Farmacêuticas para Farmácia Hospitalar. Versão 2.2.16. Available online: https://www.ordemfarmaceuticos.pt/fotos/documentos/fh_2046040655595bc9e9e089d.pdf (accessed on 16 February 2019).
- Competências Farmacêuticas para Farmácia Comunitária. Versão 11. 2.2.16. Available online: https://www.ordemfarmaceuticos.pt/fotos/documentos/fc_975194071595bc9d3b6579.pdf (accessed on 16 February 2019).
- Competências Farmacêuticas para Indústria Farmacêutica. Versão 23.11.15. Available online: https://www.ordemfarmaceuticos.pt/fotos/documentos/if_267124854595bca01812f6.pdf (accessed on 16 February 2019).
- Regulamento para Atribuição de Competências Farmacêuticas. January 2019. Available online: https://www.ordemfarmaceuticos.pt/fotos/documentos/regulamento_atribuicyayo_de_competeyncias_20464593465c51d2c366566.pdf (accessed on 16 February 2019).
- European Pharmaceutical Students’ Association. The Methodology Booklet. October 2018. Available online: https://www.epsa-online.org/methodology-booklet/ (accessed on 18 February 2019).
- Postma, T.C.; White, J.G. Students’ perceptions of vertical and horizontal integration in a discipline-based dental school? Eur. J. Dent. Educ. 2017, 21, 101–107. [Google Scholar] [CrossRef] [PubMed]
- Federação Internacional Farmacêutica (FIP). Transformar a Formação e Educação em Farmácia e Ciências Farmacêuticas no Contexto da Força Laboral Farmacêutica; Federação Mundial Farmacêutica: Haia, The Netherlands, 2017; Available online: https://fip.org/files/fip/PharmacyEducation/FIPEd_Nanjing_Report_2017_PT.pdf (accessed on 18 February 2019).
- Katajavuori, N.; Salminen, O.; Vuorensola, K.; Huhtala, H.; Vuorela, P.; Hirvonen, J. Competence-based pharmacy education in the University of Helsinki. Pharmacy 2017, 5, 29. [Google Scholar] [CrossRef]
- Gubbins, P.O.; Micek, S.T.; Badowski, M.; Cheng, J.; Gallagher, J.; Johnson, S.G.; Karnes, J.H.; Lyons, K.; Moore, K.G.; Strnad, K. Innovation in clinical pharmacy practice and opportunities for academic—Practice partnership. Pharmacotherapy 2014, 34, e45–e54. [Google Scholar] [PubMed]
- Health Education England. Advancing Pharmacy Education and Training: A Review. 2019. Available online: https://www.hee.nhs.uk/our-work/pharmacy/review-education-training (accessed on 4 January 2020).
- Bulkley, C.F.; Miller, M.J.; Draugalis, J.R. Developing and improving residency research training. Am. J. Health Syst. Pharm. 2017, 74, 152–161. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Lee, J.Y.; Lee, Y.S.; Yong, C.S.; Han, N.; Gwak, H.S.; Oh, J.; Lee, B.K.; Lee, S. Attitudes to proposed assessment of pharmacy skills in Korean pharmacist licensure examination. J. Educ. Eval. Health Prof. 2017, 14, 6. [Google Scholar] [CrossRef] [PubMed]
- Wilbur, K.; El-Awaisi, A.; Paravattil, B.; Zolezzi, M.; Pawluk, S. Contemporary Professional Skills Development for Pharmacists in the Middle East. Am. J. Pharm. Educ. 2017, 81, 6042. [Google Scholar] [CrossRef] [PubMed]
- Karim, S.A.; Ibrahim, B.; Tangiisuran, B.; Davies, J.G. What do healthcare providers know about nutrition support? A survey of the knowledge, attitudes, and practice of pharmacists and doctors toward nutrition support in Malaysia. J. Parenter Enter. Nutr. 2015, 39, 482–488. [Google Scholar] [CrossRef]
- Jacobs, S.; Schafheutle, E.I.; Jee, S.D.; Elvey, R.; Hassell, K.; Noyce, P.R. Existing arrangements for monitoring community pharmacies in England: Can they have a role in the revalidation of pharmacists? Res. Soc. Admin. Pharm. 2013, 9, 166–177. [Google Scholar] [CrossRef]
- Wittman, D.; Kovera, C.; Sullivan, M.; Rumore, M.M. Incorporating a Drug Information Consult into a Pharmacy Practice Course to Build Literature Search and Evaluation Skills Through a 3-Stage Model. J. Pharm. Pract. 2017, 30, 306–312. [Google Scholar] [CrossRef]
- Tchen, P.; Leung, L.; Simpson, F.; Kim-Sing, A.; Pearson, M.L. Bridging the gap: An evaluation of self-paced online transition modules for advanced pharmacy practice experience students. Curr. Pharm. Teach. Learn. 2018, 10, 1375–1383. [Google Scholar] [CrossRef]
- Bellottie, G.D.; Kirwin, J.; Allen, R.A.; Anksorus, H.N.; Bartelme, K.M.; Bottenberg, M.M.; Dula, C.C.; Kane, T.H.; Lee, P.H.; McMillan, A.; et al. Suggested pharmacy practice laboratory activities to align with pre-APPE domains in the Doctor of Pharmacy curriculum. Curr. Pharm. Teach. Learn. 2018, 10, 1303–1320. [Google Scholar] [CrossRef]
- Kennedy, M.J. Personalized medicines—Are pharmacists ready for the challenge? Integr. Pharm. Res. Pract. 2018, 7, 113–123. [Google Scholar] [CrossRef]
- Aucoin, R.G.; Buck, M.L.; Dupuis, L.L.; Dominguez, K.D.; Smith, K.P. Pediatric pharmacotherapeutic education: Current status and recommendations to fill the growing need. Pharmacotherapy 2005, 25, 1277–1282. [Google Scholar] [CrossRef]
- Brown, A.N.; Ward-Panckhurst, L.; Cooper, G. Factors affecting learning and teaching for medicines supply management training in Pacific Island Countries—A realist review. Rural Remote Health 2013, 13, 2327. [Google Scholar] [PubMed]
- Dean, H.J.; MacDonald, L.; Alessi-Severini, S.; Halipchuk, J.A.; Sellers, E.A.; Grymonpre, R.E. Elements and enablers for interprofessional education clinical placements in diabetes teams. Can. J. Diabetes. 2014, 38, 273–278. [Google Scholar] [CrossRef] [PubMed]
- Buna, D.K.; McGloin, R.; Loewen, P.S.; Thornhill, A.K.; Dillon, E.D.; Hawkes, J. Survey of graduates of the British Columbia pharmacy practice residency programs, 1973–2009. Can. J. Hosp. Pharm. 2011, 64, 419–425. [Google Scholar] [CrossRef] [PubMed]
- O’Neil, C.; Berdine, H. Experiential education at a university-based wellness center. Am. J. Pharm. Educ. 2007, 71, 49. [Google Scholar] [CrossRef][Green Version]
- Fowler, T.O.; Wise, H.H.; Mauldin, M.P.; Ragucci, K.R.; Scheurer, D.B.; Su, Z.; Mauldin, P.D.; Bailey, J.R.; Borckardt, J.J. Alignment of an interprofessional student learning experience with a hospital quality improvement initiative. J. Interprof. Care 2018, 1–10. [Google Scholar] [CrossRef]
- Cardiff, L.M.; Lum, E.P.; Mitchell, C.; Nissen, L.M.; Patounas, M.P.; McBride, L.J. Teaching the principles of safe prescribing to a mixed profession postgraduate cohort: Program development. J. Multidiscip Healthc. 2018, 11, 635–644. [Google Scholar] [CrossRef]
- Kassam, R. Evaluation of pharmaceutical care opportunities within an advanced pharmacy practice experience. Am. J. Pharm. Educ. 2006, 70, 49. [Google Scholar] [CrossRef]
- Pelly, L.P.; Pierrynowski Macdougall, D.M.; Halperin, B.A.; Strang, R.A.; Bowles, S.K.; Baxendale, D.M.; McNeil, S.A. THE VAXED PROJECT: An assessment of immunization education in Canadian health professional programs. BMC Med. Educ. 2010, 10, 86. [Google Scholar] [CrossRef]
- Sihavong, A.; Lundborg, C.S.; Syhakhang, L.; Vernby, A.; Panyanouvong, A.; Marions, L.; Wahlström, R. Health providers’ competence in the management of reproductive tract infections in Vientiane, Lao People’s Democratic Republic. Int. J. STD AIDS 2007, 18, 774–781. [Google Scholar] [CrossRef]

| Domain | KPI Set | Period of Monitoring |
|---|---|---|
| Workshop activities | Number of workshops held Proportion of invited participants present Satisfaction of participants (stratified per area of activity, i.e., academia vs practice) | 2016–2021, with an internal evaluation in 2019 |
| Involvement in international events | Number of events identified as particularly relevant for the EPP’s aims where work is presented | |
| Answering to global requests | Number of organizations/events/tasks with whom the EPP cooperated | |
| Answering to national needs | Creation of a common training framework for hospital internships (met/unmet) Creation of a common training framework for community pharmacy internships (met/unmet) Report by Boards of Pharmacy Practice describing their view on the advantages of these common training frameworks. This report will be made by area (hospital pharmacy and community pharmacy) and will include a section with the remaining areas, which will be structured as desired training delivered through undergraduate and postgraduate education. Development of a roadmap identifying postgraduate education available in all faculties, including those needed for less common areas of practice (e.g., research methods; pharmacogenetics) Establishment of a protocol between the nine higher education institutions and the PPS for Continuous Professional Development (CPD) (met/unmet) |
| Institution | # Semesters | # Contact Hours/Semester | # ECTS/Semester | % Practical Teaching |
|---|---|---|---|---|
| 1 | 3 | 56 | 5 | 73 |
| 2 | 1 | 60 | 5 | 43 |
| 3 | 2 | 60 | 4 | 33 |
| 4 | 2 | 112 | 9 | 68 |
| 5 | 1 | 60 | 5 | 50 |
| 6 | 3 | 52 | 5 | 67 |
| 7 | 2 | 49 | 4 | 60 |
| 8 | 1 | 75 | 6 | 60 |
| 9 | 1 | 52 | 4 | 50 |
| Core Areas | ECTS Conferred MSc | Area with Strongest Component | Proportion of Employed Graduates | Post-Graduate Offer | Particularities |
|---|---|---|---|---|---|
| Institution 1 | 300 | Pharmaceutical Sciences | 94.8% | 6 MSc; 1 PG; 1 PhD | Various international partners Unique center for monitoring drug-herbal interactions |
| Institution 2 | 300 | Pharmaceutical Sciences | 99.4% | 7 MSc; 3 PG; 5 PhD | Various partnerships with other faculties for PhD |
| Institution 3 | 300 | Health Sciences | 95.0% | 0 MSc; 0 PG; 6 PhD | Various partnerships with other faculties for PhD |
| Institution 4 | 300 | Biology and Biochemistry | 94.9% | 3 MSc; 0 PG; 0 PhD | Compulsory internships throughout the degree in various areas |
| Institution 5 | 300 | Pharmaceutical Sciences | 95.0% | 4 MSc; 14 PG, 0 PhD | Summer internships throughout the degree in various areas |
| Institution 6 | 300 | Pharmaceutical Sciences | 98.1% | 1 MSc; 0 PG; 1 PhD | Sole institution with growing number of students |
| Institution 7 | 300 | Pharmaceutical Sciences | 95.7% | 0 MSc; 10 PG; 1 PhD | Teacher practitioner concept (integrated with local community). Interprofessional collaboration in teaching (e.g., clinical cases) |
| Institution 8 | 300 | Pharmaceutical Sciences | Not Available | 0 MSc; 0 PG; 0 PhD | Has own hospital to ensure internships |
| Institution 9 | 300 | Pharmaceutical Sciences | 95.0% | 1 MSc; 0 PG; 1 PhD | International partnerships for PhD. Teaching organized in trimesters |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alves da Costa, F.; Martins, A.P.; Veiga, F.; Ramalhinho, I.; Sousa Lobo, J.M.; Rodrigues, L.; Granadeiro, L.; Castro, M.; Barata, P.; Gomes, P.; et al. Development of a Platform to Align Education and Practice: Bridging Academia and the Profession in Portugal. Pharmacy 2020, 8, 11. https://doi.org/10.3390/pharmacy8010011
Alves da Costa F, Martins AP, Veiga F, Ramalhinho I, Sousa Lobo JM, Rodrigues L, Granadeiro L, Castro M, Barata P, Gomes P, et al. Development of a Platform to Align Education and Practice: Bridging Academia and the Profession in Portugal. Pharmacy. 2020; 8(1):11. https://doi.org/10.3390/pharmacy8010011
Chicago/Turabian StyleAlves da Costa, Filipa, Ana Paula Martins, Francisco Veiga, Isabel Ramalhinho, José Manuel Sousa Lobo, Luís Rodrigues, Luiza Granadeiro, Matilde Castro, Pedro Barata, Perpétua Gomes, and et al. 2020. "Development of a Platform to Align Education and Practice: Bridging Academia and the Profession in Portugal" Pharmacy 8, no. 1: 11. https://doi.org/10.3390/pharmacy8010011
APA StyleAlves da Costa, F., Martins, A. P., Veiga, F., Ramalhinho, I., Sousa Lobo, J. M., Rodrigues, L., Granadeiro, L., Castro, M., Barata, P., Gomes, P., Seabra, V., & Caramona, M. M. (2020). Development of a Platform to Align Education and Practice: Bridging Academia and the Profession in Portugal. Pharmacy, 8(1), 11. https://doi.org/10.3390/pharmacy8010011








