Current and Potential Roles in Sports Pharmacy: A Systematic Review
Abstract
1. Introduction
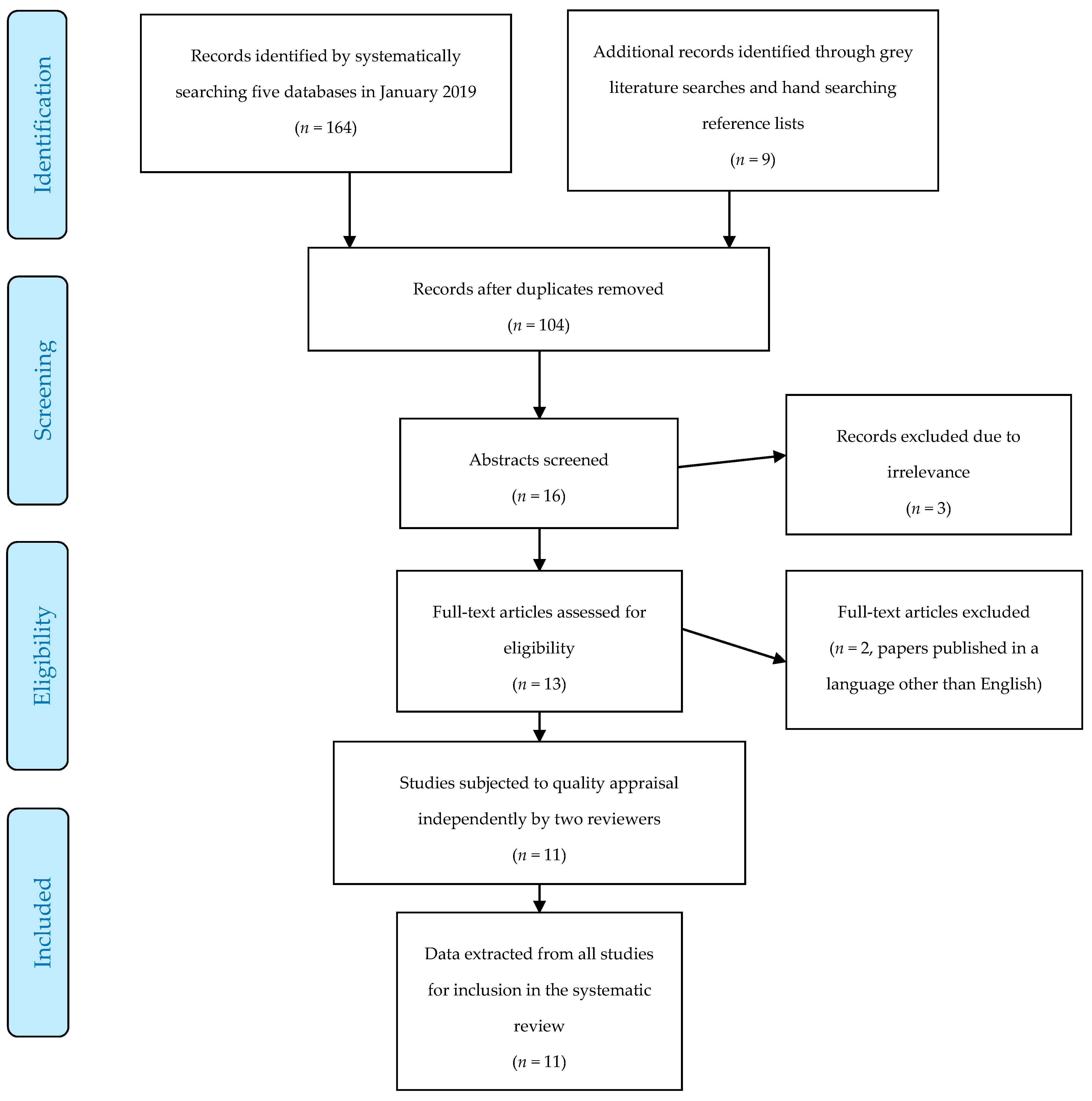
2. Methods
2.1. Search Strategy and Study Eligibility
2.2. Data Extraction and Quality Appraisal
3. Results
Quality Appraisal, Study Characteristics, and Summary of Results
4. Discussion
4.1. Doping Prevention and Control
4.1.1. Pharmacist’s Knowledge
4.1.2. Other Potential Roles for Pharmacists
4.2. Injury Management and First Aid
4.3. Opportunities for Education and Training and Recommendations Arising from This Review
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- NSW Government Department of Health NSW Pharmacist Vaccination Program. Available online: https://www.health.nsw.gov.au/immunisation/Pages/pharmacist-vaccination-expansion.aspx (accessed on 20 January 2019).
- Paudyal, V.; Watson, M.C.; Sach, T.; Porteous, T.; Bond, C.M.; Wright, D.J.; Cleland, J.; Barton, G.; Holland, R. Are pharmacy-based minor ailment schemes a substitute for other service providers? A systematic review. Br. J. Gen. Pract. 2013, 63, e472–e481. [Google Scholar] [CrossRef] [PubMed]
- Hoti, K.; Hughes, J.; Sunderland, B. An expanded prescribing role for pharmacists—An Australian perspective. Australas. Med. J. 2011, 4, 236–242. [Google Scholar] [CrossRef]
- Paola, S. Pharmacist Prescribing by 2020? What You Need to Know. Available online: https://ajp.com.au/features/professional/pharmacist-prescribing-by-2020-what-you-need-to-know/ (accessed on 13 March 2019).
- File, H.; Thomas, T.; Anderson, G. Case study of the London 2012 Olympic and Paralympic pharmacy service preparations. Int. J. Pharm. Pract. 2015, 23, 212–220. [Google Scholar] [CrossRef]
- Ambrose, P.J. Drug use in sports: A veritable arena for pharmacists. J. Am. Pharm. Assoc. 2004, 44, 501–514. [Google Scholar] [CrossRef]
- Stuart, M.; Mottram, D.; Erskine, D.; Simbler, S.; Thomas, T. Development and delivery of pharmacy services for the London 2012 Olympic and Paralympic Games. Eur. J. Hosp. Pharm. 2013, 20, 42–45. [Google Scholar] [CrossRef]
- Stuart, M.; Mottram, D.; Thomas, T. Innovations in Olympic and Paralympic pharmacy services. Br. J. Sport Med. 2013, 47, 404–406. [Google Scholar] [CrossRef] [PubMed]
- Stuart, M.; Skouroliakou, M. Pharmacy at the 2004 Olympic games. Pharm. J. 2004, 273, 319. [Google Scholar]
- Davis, S. Managing common sport injuries in the pharmacy. SA Pharm. J. 2017, 84, 35–37. [Google Scholar]
- Oltmann, C. Sports pharmacy in South Africa—Need or nonsense? SA Pharm. J. 2018, 85, 50. [Google Scholar]
- Pray, W.S. Preventing and treating summer sports injuries. Pharmacist 2010, 35, 8–15. [Google Scholar]
- Price, K.O.; Goldwire, M.A. Treatment of athletic injuries. Pharmacist 1994, 19 (Suppl. 7), 15–19. [Google Scholar]
- Thomas, T.; Mottram, D.; Waldock, C. Advising patients on prevention and management of sporting injuries. Pharm. J. 2016, 297, 102–105. [Google Scholar]
- Ciocca, M.; Stafford, H.; Laney, R. The athlete’s pharmacy. Clin. Sport Med. 2011, 30, 629–639. [Google Scholar] [CrossRef] [PubMed]
- Ivanović, D.; Jancic Stojanovic, B. Sports pharmacy—Pharmacists role in doping in sport. Arhiv za Farmaciju 2013, 63, 528–540. [Google Scholar]
- International Pharmaceutical Federation FIP Guidelines: The Role of the Pharmacist in the Fight against Doping in Sport. Available online: https://www.fip.org/www/uploads/database_file.php?id=369&table_id= (accessed on 20 January 2019).
- World Anti-Doping Agency World Anti-Doping Code. Available online: https://www.wada-ama.org/en/what-we-do/the-code (accessed on 6 January 2019).
- Howard, M.S.; DiDonato, K.L.; Janovick, D.L.; Schroeder, M.N.; Powers, M.F.; Azzi, A.G.; Lengel, A.J. Perspectives of athletes and pharmacists on pharmacist-provided sports supplement counseling: An exploratory study. J. Am. Pharm. Assoc. 2018, 58, S30–S36. [Google Scholar] [CrossRef]
- Ambrose, P.J. An advanced pharmacy practice experience in sports pharmacy. Am. J. Pharm. Educ. 2008, 72, 19. [Google Scholar] [CrossRef]
- Osborne, M.D.; Rizzo, T.D.J. Prevention and treatment of ankle sprain in athletes. Sports Med. 2003, 33, 1145–1150. [Google Scholar] [CrossRef] [PubMed]
- Pollack, A.; Bayram, C.; Miller, G. Musculoskeletal injury in Australian general practice: 2000 to 2015. Aust. Fam. Phys. 2016, 45, 462–465. [Google Scholar]
- Braund, R.; Bannerman, S.L.; Lim, C.; Moon, J.; Nicholls, J.; Straight, P.; Thompson, M. Recommendations of community pharmacists for the treatment of sprains and strains. Int. J. Pharm. Pract. 2006, 14, 271–276. [Google Scholar] [CrossRef]
- Wilcox, C.M.; Cryer, B.; Triadafilopoulos, G. Patterns of use and public perception of over-the-counter pain relievers: Focus on nonsteroidal antiinflammatory drugs. J. Rheumatol. 2005, 32, 18–24. [Google Scholar]
- Tidball, J.G. Inflammatory processes in muscle injury and repair. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2005, 288, R345–R353. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Prisma Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- University of Oxford Center for Evidence-Based Management Critical Appraisal of a Survey. Available online: https://www.cebma.org/wp-content/uploads/Critical-Appraisal-Questions-for-a-Survey.pdf (accessed on 10 January 2019).
- The Joanna Briggs Institute Critical Appraisal Checklist for Quasi-Experimental Studies (Non-Randomized Experimental Studies). Available online: http://joannabriggs.org/assets/docs/critical-appraisal-tools/JBI_Quasi-Experimental_Appraisal_Tool2017.pdf (accessed on 10 January 2019).
- Awaisu, A.; Mottram, D.; Rahhal, A.; Alemrayat, B.; Ahmed, A.; Stuart, M.; Khalifa, S. Knowledge and Perceptions of Pharmacy Students in Qatar on Anti-Doping in Sports and on Sports Pharmacy in Undergraduate Curricula. Am. J. Pharm. Educ. 2015, 79, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Bastani, P.; Nia, A.A.; Shabanpoor, M.; Mehravar, S.; Kashefian, S. Knowledge, Attitude and Practice of Iranian Pharmacists, Body Builders, and Their Coaches Regarding Sports Supplements. J. Res. Pharm. Pract. 2017, 6, 166–172. [Google Scholar] [CrossRef] [PubMed]
- Chiang, L.M.; Hatah, E.; Shamsuddin, A.F. The readiness of community pharmacists as counselors for athletes in addressing issues of the use and misuse of drugs in sports. Lat. Am. J. Pharm. 2018, 37, 1049–1055. [Google Scholar]
- Laure, P.; Kriebitzsch-Lejeune, A. Retail pharmacists and doping in sports: Knowledge and attitudes. A national survey in France. Sci. Sport 2000, 15, 141–146. [Google Scholar] [CrossRef]
- Malek, S.; Taylor, J.; Mansell, K. A questionnaire examining attitudes of collegiate athletes toward doping and pharmacists as information providers. Can. Pharm. J. 2014, 147, 352–358. [Google Scholar] [CrossRef] [PubMed]
- Mottram, D.; Khalifa, S.; Alemrayat, B.; Rahhal, A.; Ahmed, A.; Stuart, M.; Awaisu, A. Perspective of pharmacists in Qatar regarding doping and anti-doping in sports. J. Sport Med. Phys. Fit. 2016, 56, 817–824. [Google Scholar]
- Smith-Morris, A.D.; Lien, K.; Arnold, B.E. Pharmacist assessment to prevent inadvertent prohibited substance use among competitive strength athletes. Can. Pharm. J. 2018, 151, 372–376. [Google Scholar] [CrossRef]
- Doty, R.; Spinelli, A.; Stanton, M.L. Assessing the value of a pharmacy student first aid volunteer experience at a large-venue sporting event. Curr. Pharm. Teach. Learn. 2015, 7, 365–370. [Google Scholar] [CrossRef]
- Japan Anti-Doping Agency Play True 2020: Sports Pharmacist System. Available online: https://playtrue2020-sp4t.jp/static/sportspharmacist/ (accessed on 15 January 2019).
- Centre for Pharmacy Postgraduate Education. Available online: https://www.cppe.ac.uk/ (accessed on 15 January 2019).
- Brooker, C. What’s Been Happening at the Frontline at the Commonwealth Games 2018 Pharmacy, Including a Visit from Royalty. Available online: https://ajp.com.au/news/a-royal-visitation/ (accessed on 13 March 2019).
- Price, K.O.; Huff, P.S.; Isetts, B.J.; Goldwire, M.A. University-based sports pharmacy program. Am. J. Health-Syst. Pharm. 1995, 52, 302–309. [Google Scholar] [CrossRef] [PubMed]
- Braund, R. Should NSAIDs be routinely used in the treatment of sprains and strains? Pharm. J. 2006, 276, 655–656. [Google Scholar]
| Pharmacist* OR Pharmacy OR Pharmacies |
| AND |
| drug* OR ailment OR medicin* OR substance OR medical or test* OR sample or urine or urinalysis OR advise OR advice OR dispens* OR compound* OR extemporane* OR manufactur* OR inventory OR imprest OR record OR counsel* OR performance OR enhance OR enhancing OR performance-enhancing OR dope OR doping OR anti-doping OR supplement* OR non-steroidal OR anti-inflammator* OR antiinflammator* OR nonsteroidal OR NSAID* OR analgesi* OR paracetamol OR ibuprofen OR diclofenac OR naproxen OR piroxicam OR mefenamic OR topical OR rubefacient* OR CAM OR “complimentary medicine” OR “alternative medicine” OR TENS OR “transcutaneous electric* nerve stimulation” OR ultrasound OR OTC OR “over the counter” OR non-prescription OR nonprescription OR refer* OR recommend* OR RICE* OR non-pharmacological OR nonpharmacological OR lifestyle OR exercise OR assess* OR manage* OR recommend* OR approach OR strap* OR tape OR taping OR brace* OR device* OR crutch* OR “walking stick” OR wheelchair OR “mobility aid” OR orthopaedic OR orthopedic OR “first aid” OR first-aid OR amphetamine* OR stimulant* OR ephedrine OR adrenaline OR ephedra OR caffeine OR anabolic OR steroid* OR “growth hormone” OR erythropoietin OR EPO OR darbepoetin OR androstenedione OR dehydroepiandrosterone OR creatine OR “biological passport” OR vaccinat* OR immunis* OR immuniz* |
| AND |
| injury OR sprain* OR strain* OR contusion* OR “soft tissue” OR ligament OR “muscle tear” OR “torn muscle” OR tendon OR ankle OR sport* OR athlete* OR coach* OR Olympic* OR competition OR competitor OR club |
| Author (Date) | Study Location; Context; Design; Duration; Sample Size | Main Outcomes | Study Results |
|---|---|---|---|
| Ambrose (2008) [20] | California, USA; Retrospective evaluation of a six-week elective in Advanced Pharmacy Practice Experience (APPE) at two Californian universities among seven senior students. | Assessment of students’ completion and mastery of skills during APPE, and student evaluation of the APPE—satisfaction with the program and confidence in conducting drug-testing and giving drug information presentations. | All students were assessed as satisfactory for all aspects of drug collection procedures. Student evaluations of the APPE indicated a high level of satisfaction. Suggested improvements were more discussion around sports injuries/management, more drug-testing collections, presentations, and exposure to other sports-governing agencies. |
| Awaisu (2015) [29] | Qatar, 2014; Three-month cross-sectional, web-based survey of 80 female pharmacy students at Qatar University College of Pharmacy | Participants’ knowledge and perception of drugs in sports, and their views on curricular needs of Sports Pharmacy in undergraduate pharmacy programs. | 60% were unaware of WADA’s role and 85% were unaware of the FIP Statement on pharmacist’s role in anti-doping. Majority correctly classified some substances as permitted/prohibited: paracetamol (88%), amphetamines (72%), anabolic steroids (65%) antihistamines (61%); most were unable to correctly classify codeine (86%), insulin (85%) and caffeine (56%). Participants rated health professionals as the most reliable source of information. 90% favored incorporating sports pharmacy into undergraduate pharmacy curricula. |
| Bastani (2017) [30] | Iran, 2015; Five-month cross-sectional survey distributed to randomly selected bodybuilders, coaches, and pharmacists in Shiraz, South Iran. Results from 287 questionnaires included in analysis (189 body builders, 43 coaches, 55 pharmacists). | Comparison of knowledge, attitudes and practice (KAP) about sports supplements among each population, using a 5-point Likert Scale. Questions explored aspects of sports supplements and access to information, therapeutic considerations (efficacy, safety, dosage and administration), drug-supplement and disease-supplement interactions, impact on performance, involvement of health professionals, and accessing or recommending supplements. | In the three populations, mean KAP response was significantly greater than the intermediate score of 3, except pharmacists’ knowledge (not statistically significant). Younger pharmacists with less work experience had a significantly lower level of knowledge about sports supplements. Mean scores of knowledge and practice were significantly higher in the coaches group, while scores reflecting attitude were highest in the bodybuilders group. |
| Braund (2006) [23] | New Zealand, 2005; One-month cross-sectional, structured, postal questionnaire of 229 pharmacists throughout New Zealand | Frequency of presentation of sprains and strains to community pharmacies, pharmacist interventions and advice provided, and beliefs about the role of analgesics in treatment of these injuries. | An average of nine injuries were reported per month. 96% of pharmacists recommended rest, ice, compression and elevation (RICE) and 89% frequently recommended analgesics. Of these respondents, 46% recommended non-steroidal anti-inflammatory drugs (NSAIDs; oral or topical), paracetamol (36%), and codeine (8%) if required. Almost half (46%) believed that NSAIDs should not be used in the first 24–48 h post injury. Reasons for not withholding NSAIDs included belief that inflammation is a barrier to healing or that the patient is entitled to analgesia. Reasons for withholding were beliefs that inflammation was required for optimal healing, or that NSAIDs may worsen bruising, increase bleeding, or mask signs of further injury. Other advice included avoidance of heat, massage and alcohol for the 24–48 h post-injury, referral to another health professional, and arnica. |
| Chiang (2018) [31] | Malaysia, 2015; Five-month cross-sectional survey of 108 community pharmacists in Kuala Lumpur. All community pharmacists in Kuala Lumpur with at least one years’ experience in a community setting were invited to participate. | Pharmacists’ knowledge, experience, and perceptions about doping prevention in community pharmacy and factors that might influence doping. | Overall knowledge score regarding drugs in sport was low. 70% were unable to identify the official Malaysian anti-doping agency. 95% of pharmacists knew that anabolic steroids were prohibited in sport. Only 25% were aware of the prohibited status of beta blockers. Most respondents considered doping prevention initiatives important and believed pharmacists can play a role in doping prevention. Only 25% felt equipped to counsel athletes. 50% felt that athletes source performance-enhancing substances over the internet. 10% of respondents could recall requests for information about doping agents and 55% for performance enhancing supplements. Nutritional supplements most commonly sold were whey protein, weight gain powders, and multivitamins. 38% reported dispensing medicines for performance enhancing or body image purposes. Only six pharmacists had attended a course on drugs in sports, while a larger proportion (31%) had read educational materials. |
| Doty (2015) [36] | USA, 2011; Twelve-month pre-test and post-test evaluating the experiences of 26 and 27 (respectively) pharmacy students from University of Florida’s College of Pharmacy in assisting Alachua County Fire Rescue personnel provide first aid at football games. | Students’ perceptions including self-reported changes in confidence and perceptions of first aid personnel about the student’s presence. Median scores on a Likert Scale were used to compare pre- and post-assessment responses to the survey, and quantitative data was expressed in means to indicate the direction of change. | Significant improvements were seen in the post-survey for all survey criteria. The greatest improvements in student confidence were in relation to communicating and assisting first aid providers and in recognizing a dehydrated patient. Other improvements were in using interview techniques to obtain information from a patient, obtaining accurate accident information from the patient to evaluate risk to the public, documenting accident events, assisting in dispensing OTC 1 products, and recognizing heat exhaustion, alcohol intoxication, a patient in distress, or the need to transfer a patient to the hospital. |
| Howard (2018) [19] | USA, 2017; Two separate cross-sectional surveys delivered over a one-month period to either 129 athletes at Northwestern fitness centers in Ohio, or to 143 pharmacists in chain pharmacies. | Athletes’ interest in pharmacist-delivered advice about sports supplements, including perceptions of pharmacists providing counseling on sports supplements. Pharmacist survey: pharmacists’ knowledge, confidence, and enthusiasm about sports supplement counseling and perceptions on benefits and barriers to providing the service. Pharmacist knowledge, confidence and enthusiasm was measured on a 5-point Likert Scale. | Most athletes obtained supplements from a grocery store or online. Pharmacists were consulted only 2% of the time. 52% indicated that they would consider seeking a pharmacist’s advice. A doctor was consulted 9% of the time, as was a dietician. More commonly accessed sources of information were supplement stores (44%), friends (32%), or other resources (34%, primarily the internet). Information from advertisements, commercials, endorsements, or websites was not considered trustworthy by 71% of athletes. Supplements most commonly used were protein (75%), vitamins (50%), amino acids (25%), creatine (23%) and caffeine (20%). Pharmacists generally disagreed with statements concerning knowledge or confidence in their ability to counsel on sports supplements. Responses about enthusiasm for this type of service were positive—92% of pharmacists believed providing counseling on sports supplements would be beneficial. Perceived barriers were time (22%), lack of evidence (14%), and lack of knowledge (64%). In addition, 31% of pharmacists recalled no education about sports supplements at university, knowledge stemmed from self-interest in 28% of respondents cases, and 26% recalled some university-provided education. |
| Laure (2000) [32] | France, 1997; Cross-sectional questionnaire administered via scripted telephone interview among 198 French retail (community) pharmacists who reported having been either involved in programs or questioned by athletes about drugs in sports. | Pharmacists’ knowledge about doping in sports, frequency and contexts in which pharmacists are faced with doping, their attitudes toward doping in sport, and the desire of pharmacists to participate in doping control. | Doping was considered a public health problem by 88% of pharmacists. In addition, 25% reported having been confronted with doping in the previous 12 months, either to provide a product or information. Additionally, 6% recalled having been offered proposals (e.g., financial) to supply performance enhancing substances to an organization (e.g., a sporting club). While 91% of pharmacists believe pharmacists can play a role in doping prevention, 74% felt inadequately prepared to do so. Of the eight classes of drugs prohibited in sport in France in 1997, respondents only correctly identified an average of 1.7 ± 1 (most frequently mentioned were stimulants identified by 24.3% of pharmacists, anabolic steroids 20.6%, and narcotics 8.4%). Furthermore, 82.3% reported having a list of banned products in their pharmacy even though 100% had the Vidal dictionary, which contains the list in the opening pages. While only 6% of pharmacists recalled having been taught about doping control during undergraduate training, 91% had ‘seen’ articles and 62% had read some. |
| Malek (2014) [33] | Canada, 2012; Three-month cross-sectional questionnaire among 307 athletes who were part of an athletic team for the University of Saskatchewan competing in the Canadian Interuniversity Sport program. | Attitudes of athletes about doping, medication use, sources of information about doping, and whether pharmacists play a role as drug-information-providers for athletes. | Athletes did not feel pressured to dope (96.7%) and did not consider it prevalent or necessary (84.5%), or a risk worth taking (95.4%). Furthermore, 82.9% felt that most of their competitors and colleagues do not use performance-enhancing substances. Conversely, 32.9% believed that some high performance student athletes use anabolic steroids. The majority felt they had good knowledge about banned substances. Medication and supplement use was not affected by fear of doping violations with the exception of cough and cold products (avoided by 20% of athletes). An online doping education program administered by the Canadian Center for Ethics in Sport was most frequently accessed (used 74.5% of the time). In addition, 75.6% of athletes considered pharmacists a good source of information about doping, but only 35% reported speaking to a pharmacist when purchasing an OTC 1 medicine. Other reliable sources were physicians (accessed by 48.5% of athletes), physiotherapists (42.5%), and other health professionals (30.2%). Additionally, 86.8% of athletes believed they receive adequate information about doping. |
| Mottram (2016) [34] | Qatar, 2014; Three-month cross-sectional survey of 300 hospital and community pharmacists in Qatar. | Participants’ knowledge and awareness regarding doping and anti-doping, perception of information sources on drug use in sport, and attitudes toward educational needs in sports pharmacy. | While most pharmacists were aware of WADA, most were unaware of the FIP Statement. Respondents achieved an average score (53.2%) concerning knowledge about drugs in sports. Pharmacists scored higher in their knowledge of the prohibited status of OTC 1 cough and cold medicines, and dietary and ergogenic supplements, than for miscellaneous substances (e.g., anabolic steroids, amphetamines, insulin, and cannabis). Respondents perceived all potential information sources as being used equally. Their assessment of sources that should be accessed rated healthcare professionals highest when compared with other athletes, coaches, team managers, and the Internet. Sports medicine doctors were considered the most appropriate source of health-professional-delivered information, followed by pharmacists. Pharmacists had limited awareness of doping and anti-doping but most respondents (81.7%) were interested in receiving certified education or training programs in sports pharmacy. |
| Smith-Morris (2018) [35] | Canada, 2016–2017; Two-year retrospective, comprehensive analysis of medication and supplements performed by a pharmacist on 27 Canadian athletes competing at the International Powerlifting Federation Classic World Championships. | Descriptive data was reported on the findings of the pharmacist-administered assessment. | Athletes reported use of an average of 11 substances including non-prescription and prescription medicines as well as herbal and sports supplements. Overall, 15 substances were identified as being on the WADA Prohibited List or Monitoring Program and 48% of athletes (n = 13) were taking at least one WADA banned substance. The most commonly identified banned substance was pseudoephedrine. Most prohibited products were taken “as needed”, two were administered between three and five times a week, and two were taken daily. |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hooper, A.D.; Cooper, J.M.; Schneider, J.; Kairuz, T. Current and Potential Roles in Sports Pharmacy: A Systematic Review. Pharmacy 2019, 7, 29. https://doi.org/10.3390/pharmacy7010029
Hooper AD, Cooper JM, Schneider J, Kairuz T. Current and Potential Roles in Sports Pharmacy: A Systematic Review. Pharmacy. 2019; 7(1):29. https://doi.org/10.3390/pharmacy7010029
Chicago/Turabian StyleHooper, Alison D., Joyce M. Cooper, Jennifer Schneider, and Therése Kairuz. 2019. "Current and Potential Roles in Sports Pharmacy: A Systematic Review" Pharmacy 7, no. 1: 29. https://doi.org/10.3390/pharmacy7010029
APA StyleHooper, A. D., Cooper, J. M., Schneider, J., & Kairuz, T. (2019). Current and Potential Roles in Sports Pharmacy: A Systematic Review. Pharmacy, 7(1), 29. https://doi.org/10.3390/pharmacy7010029






