Community Pharmacy Use by Children across Europe: A Narrative Literature Review
Abstract
1. Introduction
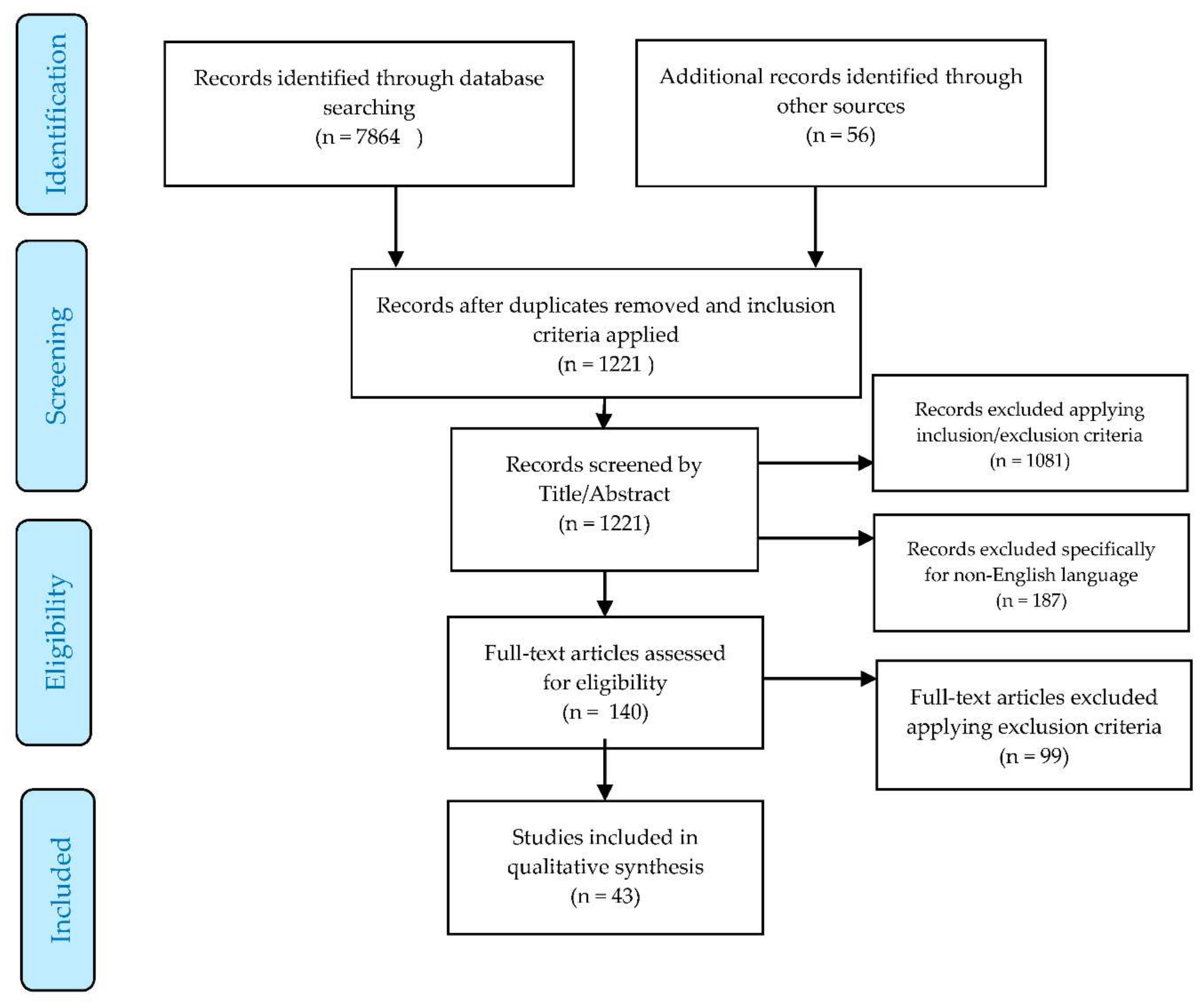
2. Materials and Methods
3. Results
3.1. Perceptions
3.1.1. Parental Perception
3.1.2. Young People
3.2. Potential Opportunities
3.2.1. Acute Minor Illness
3.2.2. Chronic Disease
3.2.3. Pregnancy and Antenatal Care
3.2.4. Pharmacovigilance
3.2.5. OTC Drug Use in Children
3.2.6. Off-Label Drug Use
3.3. Further Training Needs
3.3.1. Emergency Setting
3.3.2. Community Pharmacists as Medication Advisers
3.3.3. Drug Safety
4. Discussion
5. Conclusions
6. Limitations
7. Further Research
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Svarcaite, J. Overview of Community Pharmacy Services in Europe. 2016. Available online: https://www.oecd.org/els/health-systems/Item-2b-Overview-Community-Pharmacy-Services-Svarcaite%20.pdf (accessed on 18 December 2017).
- OECD; EU. Health at a Glance: Europe 2016, 4th ed.; Organisation for Economic Co-Operation and Development: Paris, France, 2016. [Google Scholar]
- EU. Living in the EU. 2017. Available online: https://europa.eu/european-union/about-eu/figures/living_en (accessed on 25 December 2017).
- OECD; European Observatory on Health Systems. State of Health in the EU. Slovak Republic: Country Health Profile 2017; OECD: Paris, France; European Observatory on Health Systems: Brussels, Belgium, 2017. [Google Scholar]
- Association, P. NHS Urges Parents to Use Pharmacies for Children’s Illnesses. The Guardian Online 2018. Available online: https://read.oecd-ilibrary.org/social-issues-migration-health/slovak-republic-country-health-profile-2017_9789264283541-en#page1 (accessed on 12 February 2018).
- Gill, P.; Goldacre, M.J.; Mant, D.; Heneghan, C.; Thomson, A.; Seagroatt, V.; Harnden, A. Increase in emergency admissions to hospital for children aged under 15 in England, 1999–2010: National database analysis. Arch. Dis. Child. 2013, 98, 328–334. [Google Scholar] [CrossRef] [PubMed]
- Blair, M.; Oligbu, G.; EI Tokhy, O.; Levitan, M.; Goldstone, P.; Lathlean, P. G69 how do community pharmacies support children with minor illness. Arch. Dis. Child. 2018, 103, A28–A29. [Google Scholar]
- Fraeyman, J.; Foulon, V.; Mehuys, E.; Boussery, K.; Saevels, J.; De Vriese, C.; Dalleur, O.; Housiaux, M.; Steurbaut, S.; Naegels, M.; et al. Evaluating the implementation fidelity of New Medicines Service for asthma patients in community pharmacists in Belgium. Res. Soc. Adm. Pharm. 2017, 13, 98–108. [Google Scholar] [CrossRef] [PubMed]
- Asthma UK. Asthma Facts and Statistics. 2016. Available online: https://www.asthma.org.uk/about/media/facts-and-statistics/ (accessed on 25 December 2017).
- Pharmaceutical Society of Ireland. Guidance on the Provision of Vaccination Services by Pharmacists in Retail Pharmacy Businesses; Pharmaceutical Society of Ireland: Dublin, Ireland, 2016; p. 4. [Google Scholar]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gotzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009, 6, e1000100. [Google Scholar] [CrossRef] [PubMed]
- Hammond, T.; Clatworthy, J.; Horne, R. Patients’ use of GPs and community pharmacists in minor illness: A cross-sectional questionnaire-based study. Fam. Pract. 2004, 21, 146–149. [Google Scholar] [CrossRef] [PubMed]
- Hodgson, C.; Wong, I. What do mothers of young children think of community pharmacists? A descriptive survey. J. Fam. Health Care 2004, 14, 73–74. [Google Scholar] [PubMed]
- Gray, N.J.; Boardman, H.F.; Symonds, B.S. Information sources used by parents buying non-prescription medicines in pharmacies for preschool children. Int. J. Clin. Pharm. 2011, 33, 842–848. [Google Scholar] [CrossRef] [PubMed]
- Bamford, S.; Kneale, D.; Wilson, J.; Watson, J. A New Journey to Health—Health Infrormation Seeking Behaviour Across the Ages; International Longevity Centre: London, UK, 2015; p. 1. [Google Scholar]
- Holappa, M.; Ahonen, R.; Vainio, K.; Hameen-Anttila, K. Information sources used by parents to learn about medications they are giving their children. Res. Soc. Adm. Pharm. 2012, 8, 579–584. [Google Scholar] [CrossRef] [PubMed]
- Gray, N.J.; Shaw, K.L.; Smith, F.J.; Burton, J.; Prescott, J.; Roberts, R.; Terry, D.; McDonagh, J.E. The Role of Pharmacists in Caring for Young People with Chronic Illness. J. Adolesc. Health 2017, 60, 219–225. [Google Scholar] [CrossRef] [PubMed]
- Plachouras, D.; Kavatha, D.; Antoniadou, A.; Giannitsioti, E.; Poulakou, G.; Kanellakopoulou, K.; Giamarellou, H. Dispensing of antibiotics without prescription in Greece, 2008: Another link in the antibiotic resistance chain. Euro Surveill 2010, 18, 15. [Google Scholar]
- Stakenborg, J.P.; de Bont, E.G.; Peetoom, K.K.; Nelissen-Vrancken, M.H.; Cals, J.W. Medication management of febrile children: A qualitative study on pharmacy employees’ experiences. Int. J. Clin. Pharm. 2016, 38, 1200–1209. [Google Scholar] [CrossRef] [PubMed]
- Gidman, W.; Coomber, R. Contested space in the pharmacy: Public attitudes to pharmacy harm reduction services in the West of Scotland. Res. Soc. Adm. Pharm. 2014, 10, 576–587. [Google Scholar] [CrossRef] [PubMed]
- Parsons, J.; Adams, C.; Aziz, N.; Holmes, J.; Jawad, R.; Whittlesea, C. Evaluation of a community pharmacy delivered oral contraception service. J. Fam. Plan. Reprod. Health Care 2013, 39, 97–101. [Google Scholar] [CrossRef] [PubMed]
- Guegan, E. Infection prevention and management by community pharmacists. J. Infect. Prev. 2010, 11, 106–109. [Google Scholar] [CrossRef]
- Karamanidou, C.; Dimopoulos, K. Greek health professionals’ perceptions of the HPV vaccine, state policy recommendations and their own role with regards to communication of relevant health information. BMC Public Health 2016, 16, 467. [Google Scholar] [CrossRef] [PubMed]
- Terry, D.; Petridis, K.; Aiello, M.; Sinclair, A.; Huynh, C.; Mazard, L.; Ubhi, H.; Terry, A.; Hughes, E. The Potential for Pharmacists to Manage Children Attending Emergency Departments. Arch. Dis. Child. 2016, 101, e2. [Google Scholar] [CrossRef] [PubMed]
- Carr, A.; Patel, R.; Jones, M.; Suleman, A. A pilot study of a community pharmacist intervention tp promote the effective use of emollients in childhood eczema. Pharm. J. 2007, 278, 319–322. [Google Scholar]
- Jacome, J.; Inesta Garcia, A. Prospective study about the impact of a community pharmaceutical care service in patients with asthma. Rev. Esp. Salud Publica 2003, 77, 393–403. [Google Scholar]
- Gay, C.L.; Chapuis, F.; Bendelac, N.; Tixier, F.; Treppoz, S.; Nicolino, M. Reinforced follow-up for children and adolescents with type 1 diabetes and inadequate glycaemic control: A randomized controlled trial intervention via the local pharmacist and telecare. Diabetes Metab. 2006, 32, 159–165. [Google Scholar] [CrossRef]
- Koster, E.S.; Philbert, D.; Winters, N.A.; Bouvy, M.L. Medication adherence in adolescents in current practice: Community pharmacy staff’s opinions. Int. J. Pharm. Pract. 2015, 23, 221–224. [Google Scholar] [CrossRef] [PubMed]
- Terry, D.; Sinclair, A. Prescribing for children at the interfaces of care. Arch. Dis. Child. Educ. Pract. Ed. 2012, 97, 152–156. [Google Scholar] [CrossRef] [PubMed]
- De Jong-van den Berg, L.T. Monitoring of the folic acid supplementation program in The Netherlands. Food Nutr. Bull. 2008, 29 (Suppl. 2), S210–S213. [Google Scholar] [CrossRef] [PubMed]
- Deacon, K. Epilepsy Prevalence, Incidence and Other Statistics; Epilepsy Foundation: Landover, MD, USA, 2011; p. 1. [Google Scholar]
- Bilbow, A. ADHD: Paying Enough Attention; ADDISS: Middlesex, UK, 2016; p. 1. [Google Scholar]
- Perucca, E.; Meador, K.J. Adverse effects of antiepileptic drugs. Acta Neurol. Scand. Suppl. 2005, 181, 30–35. [Google Scholar] [CrossRef] [PubMed]
- Tobaiqy, M.; Stewart, D.; Helms, P.J.; Bond, C.; Lee, A.J.; Bateman, N.; McCaig, D.; McLay, J. A pilot study to evaluate a community pharmacy-based monitoring system to identify adverse drug reactions associated with paediatric medicines use. Eur. J. Clin. Pharmacol. 2010, 66, 627–632. [Google Scholar] [CrossRef] [PubMed]
- Stewart, D.; Helms, P.; McCaig, D.; Bond, C.; McLay, J. Monitoring adverse drug reactions in children using community pharmacies: A pilot study. Br. J. Clin. Pharmacol. 2005, 59, 677–683. [Google Scholar] [CrossRef] [PubMed]
- Aston, J.; Wilson, K.A.; Terry, D.R. Children/young people taking long-term medication: A survey of community pharmacists’ experiences in England. Int. J. Pharm. Pract. 2017, 26, 104–110. [Google Scholar] [CrossRef] [PubMed]
- Lilley, A. Assessing the Benefits that Community Pharmacies can have on Childhood Asthma Outcomes. Arch. Dis. Child. 2016, 101, e2. [Google Scholar] [CrossRef] [PubMed]
- Ylinen, S.; Hameen-Anttila, K.; Sepponen, K.; Lindblad, A.K.; Ahonen, R. The use of prescription medicines and self-medication among children—A population-based study in Finland. Pharmacoepidemiol. Drug Saf. 2010, 19, 1000–1008. [Google Scholar] [CrossRef] [PubMed]
- Clavenna, A.; Sequi, M.; Bortolotti, A.; Merlino, L.; Fortino, I.; Bonati, M. Determinants of the drug utilization profile in the paediatric population in Italy’s Lombardy Region. Br. J. Clin. Pharmacol. 2009, 67, 565–571. [Google Scholar] [CrossRef] [PubMed]
- Italia, S.; Brand, H.; Heinrich, J.; Berdel, D.; von Berg, A.; Wolfenstetter, S.B. Utilization of self-medication and prescription drugs among 15-year-old children from the German GINIplus birth cohort. Pharmacoepidemiol. Drug Saf. 2015, 24, 1133–1143. [Google Scholar] [CrossRef] [PubMed]
- Koelch, M.; Prestel, A.; Singer, H.; Keller, F.; Fegert, J.M.; Schlack, R.; Hoelling, H.; Knopf, H. Psychotropic medication in children and adolescents in Germany: Prevalence, indications, and psychopathological patterns. J. Child Adolesc. Psychopharmacol. 2009, 19, 765–770. [Google Scholar] [CrossRef] [PubMed]
- Du, Y.; Knopf, H. Self-medication among children and adolescents in Germany: Results of the National Health Survey for Children and Adolescents (KiGGS). Br. J. Clin. Pharmacol. 2009, 68, 599–608. [Google Scholar] [CrossRef] [PubMed]
- Smith, S.M.; Henman, M.; Schroeder, K.; Fahey, T. Over-the-counter cough medicines in children: Neither safe or efficacious? Br. J. Gen. Pract. 2008, 58, 757–758. [Google Scholar] [CrossRef] [PubMed]
- Smith, S.M.; Schroeder, K.; Fahey, T. Over-the-counter medications for acute cough in children and adults in ambulatory settings. Cochrane Database Syst. Rev. 2008, 23, CD001831. [Google Scholar] [CrossRef]
- Holmstrom, I.K.; Bastholm-Rahmner, P.; Bernsten, C.; Roing, M.; Bjorkman, I. Swedish teenagers and over-the-counter analgesics—Responsible, casual or careless use. Res. Soc. Adm. Pharm. 2014, 10, 408–418. [Google Scholar] [CrossRef] [PubMed]
- Stewart, D.; Rouf, A.; Snaith, A.; Elliott, K.; Helms, P.J.; McLay, J.S. Attitudes and experiences of community pharmacists towards paediatric off-label prescribing: A prospective survey. Br. J. Clin. Pharmacol. 2007, 64, 90–95. [Google Scholar] [CrossRef] [PubMed]
- Mukattash, T.; Hawwa, A.F.; Trew, K.; McElnay, J.C. Healthcare professional experiences and attitudes on unlicensed/off-label paediatric prescribing and paediatric clinical trials. Eur. J. Clin. Pharmacol. 2011, 67, 449–461. [Google Scholar] [CrossRef] [PubMed]
- Hanna, H.J.; Emmanuel, J.; Naim, S.; Umasunthar, T.; Boyle, R.J. Community healthcare professionals overestimate the risk of fatal anaphylaxis for food allergic children. Clin. Exp. Allergy 2016, 46, 1588–1595. [Google Scholar] [CrossRef] [PubMed]
- Raffin, D.; Giraudeau, B.; Samimi, M.; Machet, L.; Pourrat, X.; Maruani, A. Corticosteroid Phobia Among Pharmacists Regarding Atopic Dermatitis in Children: A National French Survey. Acta Derm. Venereol. 2016, 96, 177–180. [Google Scholar] [CrossRef] [PubMed]
- Rees, P.; Edwards, A.; Powell, C.; Hibbert, P.; Williams, H.; Makeham, M.; Carter, B.; Luff, D.; Parry, G.; Avery, A.; et al. Patient Safety Incidents Involving Sick Children in Primary Care in England and Wales: A Mixed Methods Analysis. PLoS Med. 2017, 14, e1002217. [Google Scholar] [CrossRef] [PubMed]
- Bardage, C.; Westerlund, T.; Barzi, S.; Bernsten, C. Non-prescription medicines for pain and fever—A comparison of recommendations and counseling from staff in pharmacy and general sales stores. Health Policy 2013, 110, 76–83. [Google Scholar] [CrossRef] [PubMed]
- Lapeyre-Mestre, M.; Pin, M. Management of acute infantile diarrhoea: A study on community pharmacy counseling in the Midi-Pyrenees region. Arch. Pediatr. 2004, 11, 898–902. [Google Scholar] [CrossRef] [PubMed]
- Venables, R.; Stirling, H.; Batchelor, H.; Marriott, J. Problems with oral formulations prescribed to children: A focus group study of healthcare professionals. Int. J. Clin. Pharm. 2015, 37, 1057–1067. [Google Scholar] [CrossRef] [PubMed]
- Driesen, A.; Vandenplas, Y. How do pharmacists manage acute diarrhoea in an 8-month-old baby? A simulated client study. Int. J. Pharm. Pract. 2009, 17, 215–220. [Google Scholar] [CrossRef] [PubMed]
| Inclusion Criteria | Exclusion Criteria | Justification |
|---|---|---|
| At search string level: | ||
| Papers published between January 2000 and December 2017 | The role of community pharmacists compared to present day use may be significantly different | |
| Any article type | This allows for a comprehensive review | |
| Full paper available | The full paper needs to be analysed in order for the review to be robust | |
| At title/abstract level: | ||
| Paper does not specifically relate to use of community pharmacy by children | This literature review aimed to study the utilisation of community pharmacy by paediatric populations (0–18 years) in Europe | |
| English language paper | The resources were not sufficient to fully translate papers | |
| Europe | This literature review aimed to study the utilisation of community pharmacy by paediatric populations (0–18 years) in Europe | |
| At full-text level: | ||
| Paper analyses utilisation of community pharmacy by children | These articles are relevant to the study | |
| Paper only mentions community pharmacy as the location of a study | This study aims to explore the utilization of community pharmacies as a primary care service |
| Country | Number of Studies Included in Synthesis |
|---|---|
| United Kingdom (England, Scotland, Wales, Northern Ireland) | 19 |
| Sweden | 5 |
| Netherlands | 4 |
| France | 4 |
| Germany | 3 |
| Finland | 2 |
| Greece | 1 |
| Iceland | 1 |
| Belgium | 1 |
| Spain | 1 |
| Italy | 1 |
| Croatia | 1 |
| Reference as in Text | AuthorNo (Year) | Type of Paper/Study | Population Size | Main Study Finding |
|---|---|---|---|---|
| [12] | Hammond (2004) | Cross-sectional questionnaire-based study | 3984 | Pharmacists are a good source of information for unwell children |
| [13] | Hodgson (2004) | Cross-sectional questionnaire-based study | 85 | 87% of mothers find pharmacist advice for sick children helpful |
| [14] | Gray (2011) | Cross-sectional mixed methods study | 134 questionnaires, 39 interviews | 82% of parents find pharmacist advice somewhat helpful regarding medication |
| [15] | Bamford (2015) | Grey literature (Charity report) | Not applicable | Parents prioritise other information sources over pharmacists |
| [16] | Holappa (2012) | Cross-sectional questionnaire-based study | 4020 | 44% of parents seek pharmacist advice for their sick children |
| [17] | Gray (2017) | Cross-sectional mixed methods study | Not provided | Most parents prefer receiving written (50%) or spoken (29%) advice from pharmacists |
| [18] | Plachouras (2010) | Cross-sectional questionnaire-based study | 174 | Inappropriate dispensing of antibiotics by pharmacists possibly led to widespread antibiotic resistance |
| [19] | Stakenborg (2016) | Cross-sectional focus group-based study | 24 | Parents trust their own knowledge more than advice from pharmacists |
| [20] | Gidman (2014) | Cross-sectional focus group-based study | 26 | Parents did not want to bring children to pharmacies due to presence of substance misuse patients in the clinic |
| [21] | Parsons (2013) | Cross-sectional questionnaire-based study | 99 | Parents found that pharmacies lack privacy compared to other primary care services |
| [22] | Guegan (2010) | Literature review | Not provided | Pharmacists have a trusted relationship with young patients formed over multiple encounters |
| [23] | Karamanidou (2016) | Cross-sectional interview-based study | 15 | Expanded role for pharmacists in oral contraceptive pill (OCP) provision and HPV vaccine |
| [24] | Terry (2016) | Cross-sectional observational study | 1623 | 9% of ED attendances could have been dealt with in pharmacies |
| [25] | Carr (2007) | Pre-post interventional pilot study | 50 | Effective example of pharmacist led intervention in childhood eczema |
| [26] | Jacome (2003) | Pre-post interventional pilot study | 164 | Effective example of pharmacist-led intervention in childhood asthma |
| [27] | Gay (2006) | Randomised control trial | 100 | Ineffective example of pharmacist-led intervention for Type 1 Diabetes |
| [28] | Koster (2015) | Cross-sectional interview-based study | 170 | Regular attendance of children when collecting medication can improve medication adherence |
| [29] | Terry (2012) | Literature review | 24 references | Increasing the communication between pharmacies and other primary care interfaces |
| [30] | de Jong-van den berg (2008) | Explorative comparative study | Not provided | Effective example of pharmacist-led intervention in the reduction of neural tube defects (NTDs) |
| [31] | Deacon (2011) | Statistics report (Epilepsy) | Not applicable | Incidence of epilepsy in children |
| [32] | Bilbow (2016) | Grey Literature (Charity report) | Not applicable | Incidence of attention deficit hyperactivity disorder (ADHD) in children |
| [33] | Perucca (2005) | Literature review | 55 references | Medications for ADHD and epilepsy have a high rate of adverse events |
| [34] | Tobaiqy (2010) | Cross-sectional questionnaire-based pilot study | 72 | Exploring wider pharmacist involvement in the UK Yellow Card scheme |
| [35] | Stewart (2005) | Prospective questionnaire-based study | 267 | The pharmacist as a useful resource for therapeutic drug monitoring |
| [36] | Aston (2017) | Cross-sectional questionnaire-based study | 76 | 23.7% of pharmacists performed medicine use reviews (MURs) for children’s medication |
| [37] | Liley (2016) | Pre-post interventional pilot study | 15 | Increased use of MURs by pharmacists seems to improve children’s asthma control |
| [38] | Ylinen (2010) | Cross-sectional questionnaire-based study | 4032 | 50% of children use over-the-counter (OTC) medication |
| [39] | Clavenna (2009) | Retrospective cohort study | 1,542,203 | 48% of children receive 1 drug prescription a month |
| [40] | Italia (2015) | Retrospective cohort study | 3013 | 31.6% of children used an OTC drug in the last month |
| [41,42] | Koelch (2008)/Du (2009) | Retrospective cohort study | 17,450 | 30% of prescription medications for children were being used without proper prescription |
| [43,44] | Smith (2008)/Smith (2008) | Systematic literature review (searching for randomised controlled trials) | 3492 | The various causes of mortality from children using cough medicines |
| [45] | Holmstrom (2014) | Cross-sectional questionnaire-based study | 77 | Careless and casual behavior of children towards OTC use |
| [46] | Stewart (2007) | Prospective questionnaire-based study | 482 | 40% of pharmacists prescribed drugs off-label |
| [47] | Mukkatash (2011) | Cross-sectional questionnaire-based study | 563 | The need for clinical trials to change paediatric formulations, to reduce off-label prescribing |
| [48] | Hanna (2016) | Cross-sectional questionnaire-based study | 90 | Only 77% of pharmacists knew to use an adrenaline auto-injector for food anaphylaxis |
| [49] | Raffin (2016) | Cross-sectional questionnaire-based study | 500 | Pharmacist perpetuate a corticosteroid phobia in the population |
| [50] | Rees (2017) | Cross-sectional mixed methods study | 2191 | Medication errors occur at a much higher rate in community pharmacies than other primary care interfaces |
| [51] | Bardage (2013) | Cross-sectional questionnaire-based study | 1098 | 6% of pharmacists provided inappropriate medication to febrile children |
| [52] | Lapeyre-Mestre (2004) | Cross-sectional questionnaire-based study | 176 | 12.9% of pharmacists provided contra-indicated medication to children |
| [53] | Venables (2015) | Cross-sectional focus group-based study | 4 | 60% of pharmacists were very dependent on product monographs |
| [54] | Driesen (2009) | Cross-sectional questionnaire-based study | 101 | Only 30% of pharmacists prescribed oral rehydration solution (ORS) to children with severe diarrhoea |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Blair, M.; Menon, A. Community Pharmacy Use by Children across Europe: A Narrative Literature Review. Pharmacy 2018, 6, 51. https://doi.org/10.3390/pharmacy6020051
Blair M, Menon A. Community Pharmacy Use by Children across Europe: A Narrative Literature Review. Pharmacy. 2018; 6(2):51. https://doi.org/10.3390/pharmacy6020051
Chicago/Turabian StyleBlair, Mitch, and Arjun Menon. 2018. "Community Pharmacy Use by Children across Europe: A Narrative Literature Review" Pharmacy 6, no. 2: 51. https://doi.org/10.3390/pharmacy6020051
APA StyleBlair, M., & Menon, A. (2018). Community Pharmacy Use by Children across Europe: A Narrative Literature Review. Pharmacy, 6(2), 51. https://doi.org/10.3390/pharmacy6020051





