Quality of Life and Medication Adherence of Independently Living Older Adults Enrolled in a Pharmacist-Based Medication Management Program
Abstract
:1. Introduction
2. Materials and Methods
2.1. Description of the Pharmacist-Based Medication Management Service
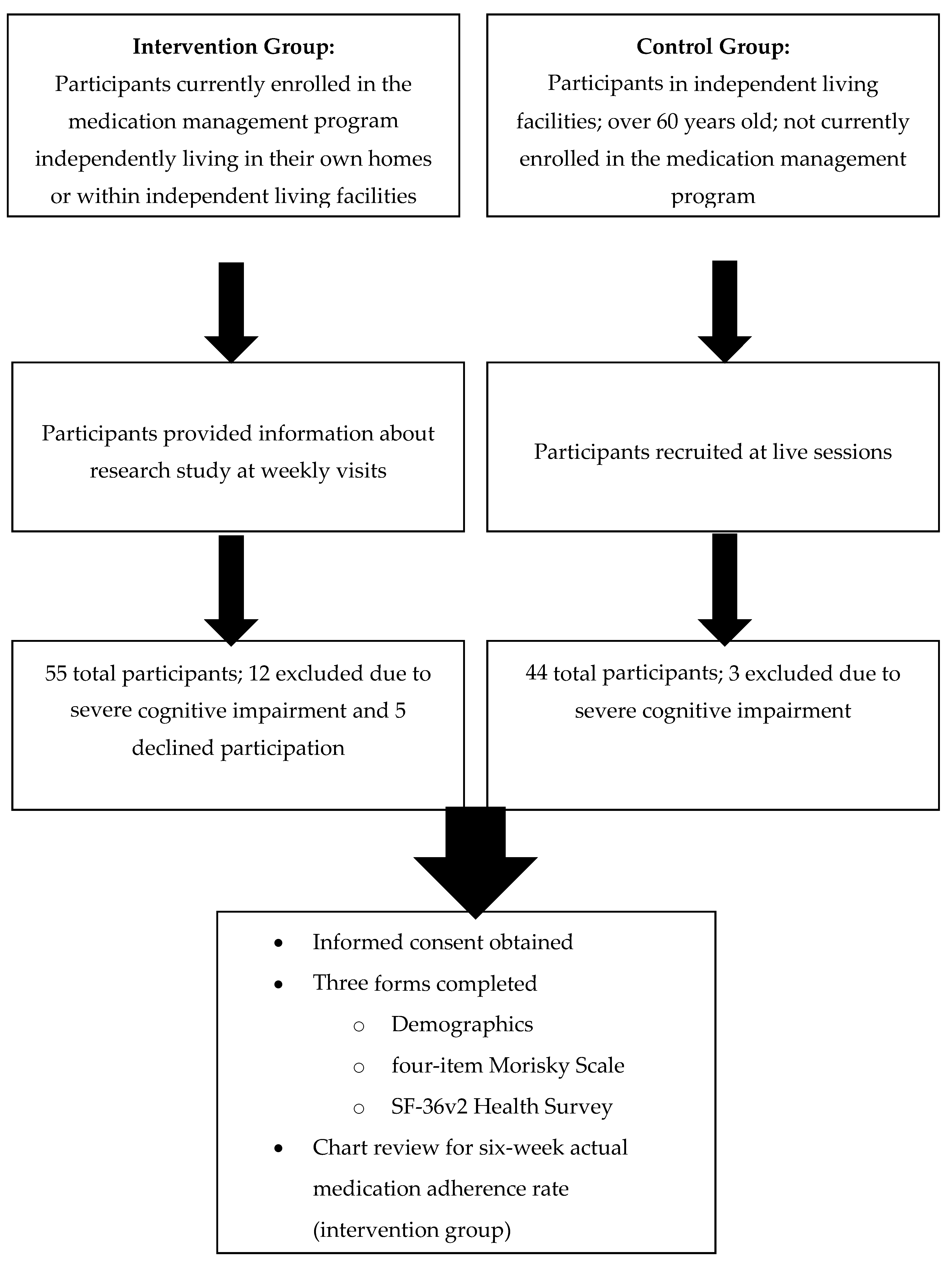
2.2. Study Design and Population
2.3. Measurements
Data Analysis
3. Results
3.1. Subjects
3.2. Medication Adherence
3.3. Quality of Life
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Holland, R.; Desborough, J.; Goodyer, L.; Hall, S.; Wright, D.; Loke, Y.K. Does pharmacist-led medication review help to reduce hospital admissions and deaths in older people? A systematic review and meta-analysis. Br. J. Clin. Pharmacol. 2007, 65, 303–316. [Google Scholar] [CrossRef] [PubMed]
- Verrue, C.L.R.; Petrovic, M.; Mehuys, E.; Remon, J.P.; Stichele, R.V. Pharmacists interventions for optimization of medication use in nursing homes. A systematic review. Drugs Aging 2009, 26, 37–49. [Google Scholar] [CrossRef] [PubMed]
- Spinewine, A.; Fialova, D.; Byrne, S. The role of the pharmacist in optimizing pharmacotherapy in older people. Drugs Aging 2012, 29, 495–510. [Google Scholar] [CrossRef] [PubMed]
- George, J.; Elliott, R.A.; Stewart, D.C. A systematic review of interventions to improve medication taking in elderly patients prescribed multiple medications. Drugs Aging 2008, 25, 307–324. [Google Scholar] [CrossRef] [PubMed]
- Cipolle, R.J.; Strand, L.M.; Morley, P.C. Pharmaceutical Care Practice: The Clinician’s Guide, 2nd ed.; McGraw-Hill: New York, NY, USA, 2004. [Google Scholar]
- Sorensen, L.; Stokes, J.A.; Purdie, D.M.; Woodward, M.; Roberts, M.S. Medication management at home: Medication-related risk factors associated with poor health outcomes. Age Ageing 2005, 34, 626–632. [Google Scholar] [CrossRef] [PubMed]
- Dorr, D.A.; Jones, S.S.; Burns, L.; Donnelly, S.M.; Brunker, C.P.; Wilcox, A.; Clayton, P.D. Use of health-related, quality of life metrics to predict mortality and hospitalizations in community-dwelling seniors. J. Am. Geriatr. Soci. 2006, 54, 667–673. [Google Scholar] [CrossRef] [PubMed]
- Fan, V.S.; Au, D.H.; McDonell, M.B.; Fihn, S.D. Intraindividual change in SF-36 in ambulatory clinic primary care patients predicted mortality and hospitalizations. J. Clin. Epidemiol. 2004, 57, 277–283. [Google Scholar] [CrossRef] [PubMed]
- Sokol, M.C.; McGuigan, K.A.; Verbrugge, R.R.; Epstein, R.S. Impact of medication adherence on hospitalization risk and healthcare cost. Med. Care 2005, 43, 521–530. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.K.; Grace, K.A.; Taylor, A.J. Effect of a pharmacy care program on medication adherence and persistence, blood pressure, and low-density lipoprotein cholesterol: A randomized controlled trial. J. Am. Med. Assoc. 2006, 296, 2563–2571. [Google Scholar] [CrossRef] [PubMed]
- Doggrell, S.A. Adherence to medicines in the older-aged with chronic conditions: Does intervention by an allied health professional help? Drugs Aging 2010, 27, 239–254. [Google Scholar] [CrossRef] [PubMed]
- Smith, H.; Hankins, M.; Hodson, A.; George, C. Measuring the adherence to medication of elderly patients with heart failure: Is there a gold standard? Int. J. Cardiol. 2009, 145, 122–123. [Google Scholar] [CrossRef] [PubMed]
- Ware, J.E.; Kosinski, M.; Dewey, J.E. How to Score Version 2 of the SF-36® Health Survey; Quality Metric Incorporated: Lincoln, RI, USA, 2000. [Google Scholar]
- Morisky, D.E.; Green, L.W.; Levine, D.M. Concurrent and predictive validity of a self-reported measure of medication adherence. Med. Care 1986, 24, 67–74. [Google Scholar] [CrossRef] [PubMed]
- Aminzadeh, F.; Dalziel, W.B. Older adults in the emergency department: A systematic review of patterns of use, adverse health outcomes, and effectiveness of interventions. Ann. Emerg. Med. 2002, 39, 238–247. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, J.J.; Stolee, P.; Hirdes, J.P.; Poss, J.W. Examining three frailty conceptualizations in their ability to predict negative outcomes for home-care clients. Age Ageing 2010, 39, 755–758. [Google Scholar] [CrossRef] [PubMed]
- Freiheit, E.A.; Hogan, D.B.; Eliasziw, M.; Meekes, M.F.; Ghali, W.A.; Partlo, L.A.; Maxwell, C.J. Development of a frailty index for patients with coronary artery disease. J. Am. Geriatr. Soc. 2010, 58, 1526–1531. [Google Scholar] [CrossRef] [PubMed]
- Rose, A.J.; Glickman, M.E.; D’Amore, M.M.; Orner, M.B.; Berlowitz, D.; Kressin, N.R. Effects of daily adherence to antihypertensive medication on blood pressure control. J. Clin. Hypertens. 2011, 13, 416–421. [Google Scholar] [CrossRef] [PubMed]
- Baroletti, S.; Dell’Orfano, H. Medication adherence in cardiovascular disease. Circulation 2010, 121, 1455–1458. [Google Scholar] [CrossRef] [PubMed]
- Zedler, B.K.; Joyce, A.; Murrelle, L.; Kakad, P.; Harpe, S.E. A pharmacoepidemiologic analysis of the impact of calendar packaging on adherence to self-administered medications for long-term use. Clin. Ther. 2011, 33, 581–597. [Google Scholar] [CrossRef] [PubMed]


| Intervention Group (n = 38) | Control Group (n = 41) | p Value | |
|---|---|---|---|
| Median Age (IQR) | 87 (83–89) | 84 (77–88) | 0.07 |
| Sex, Females (%) | 29 (76.3%) | 27 (65.9%) | 0.45 |
| Highest level of education | |||
| Some college or less | 21 (55.3%) | 15 (36.6%) | 0.22 |
| Bachelor’s degree or equivalent | 9 (23.7%) | 16 (39.0%) | |
| Masters degree or higher | 8 (21.0%) | 10 (24.4%) | |
| Median number of regularly scheduled medications (including prescription, over-the-counter, and herbal products) (IQR) | 10 (8–13) | 5 (4–8) | <0.0001 |
| Median number of disease states (IQR) | 3.5 (2–5) | 3 (2–5) | 0.17 |
| Trouble reading due to vision | 14 (36.8%) | 11 (26.8%) | 0.34 |
| Number of subjects with at least one hospital or emergency department visit in past 6 months | 16 (42.1%) | 15 (36.6%) | 0.62 |
| Median number of visits to hospital or emergency department in past 6 months (if greater than zero) (IQR) | 1.5 (1–2.5) | 1 (1–2) | 0.20 |
| Number of subjects with at least one fall in past 6 months | 13 (34.2%) | 14 (34.1%) | >0.90 |
| Median number of falls in past 6 months (if greater than zero) (IQR) | 1 (1–3) | 1 (1–2) | 0.50 |
| Duration of time in current home | |||
| 0–12 months | 11 (28.9%) | 8 (19.5%) | 0.33 |
| 1–3 years | 10 (26.3%) | 17 (41.5%) | |
| 4 or more years | 17 (44.7%) | 16 (39%) | |
| Number of people living in current household | |||
| 1 person | 30 (78.9%) | 20 (48.8%) | 0.01 |
| 2 persons | 8 (21.1%) | 21 (51.2%) | |
| Annual household income | |||
| 0–$25,000 | 8 (21.1%) | 12 (29.2%) | |
| $25,001–$50,000 | 6 (15.7%) | 17 (41.5%) | 0.0014 |
| $50,001–$100,000 | 3 (7.9%) | 8 (19.5%) | |
| Greater than $100,000 | 13 (34.2%) | 2 (4.9%) | |
| Not specified | 8 (21.1%) | 2 (4.9%) |
| Mean (SD) | 98 (0.03) |
|---|---|
| Median (Range) | 99 (88–100) |
| Intervention (n = 38) | Control (n = 41) | p Value | |
|---|---|---|---|
| Physical Component Summary (PCS) | 41.77 (11.31) | 45.37 (8.80) | 0.12 |
| Mental Component Summary (MCS) | 55.85 (48.34–59.76) | 54.67 (50.12–60.17) | 0.97 |
| Physical Functioning (PF) | 36.49 (26.92–47.97) | 46.06 (38.40–49.89) | 0.03 |
| Role-Physical (RP) | 39.19 (32.46–54.91) | 45.93 (39.19–52.66) | 0.06 |
| Bodily Pain (BP) | 51.51 (42.64–62.00) | 50.71 (42.64–55.55) | 0.69 |
| General Health (GH) | 53.19 (43.68–57.94) | 53.19 (46.05–55.56) | 0.97 |
| Vitality (VT) | 52.60 (40.72–55.57) | 52.60 (49.63–58.54) | 0.15 |
| Social Functioning (SF) | 54.84 (37.27–57.34) | 52.33 (47.31–57.34) | 0.64 |
| Role Emotional (RE) | 54.43 (38.76–56.17) | 52.69 (42.24–56.17) | 0.97 |
| Mental Health (MH) | 53.48 (48.25–58.72) | 56.10 (53.48–58.72) | 0.36 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Harlow, C.; Hanna, C.; Eckmann, L.; Gokun, Y.; Zanjani, F.; Blumenschein, K.; Divine, H. Quality of Life and Medication Adherence of Independently Living Older Adults Enrolled in a Pharmacist-Based Medication Management Program. Pharmacy 2017, 5, 20. https://doi.org/10.3390/pharmacy5020020
Harlow C, Hanna C, Eckmann L, Gokun Y, Zanjani F, Blumenschein K, Divine H. Quality of Life and Medication Adherence of Independently Living Older Adults Enrolled in a Pharmacist-Based Medication Management Program. Pharmacy. 2017; 5(2):20. https://doi.org/10.3390/pharmacy5020020
Chicago/Turabian StyleHarlow, Christopher, Catherine Hanna, Lynne Eckmann, Yevgeniya Gokun, Faika Zanjani, Karen Blumenschein, and Holly Divine. 2017. "Quality of Life and Medication Adherence of Independently Living Older Adults Enrolled in a Pharmacist-Based Medication Management Program" Pharmacy 5, no. 2: 20. https://doi.org/10.3390/pharmacy5020020
APA StyleHarlow, C., Hanna, C., Eckmann, L., Gokun, Y., Zanjani, F., Blumenschein, K., & Divine, H. (2017). Quality of Life and Medication Adherence of Independently Living Older Adults Enrolled in a Pharmacist-Based Medication Management Program. Pharmacy, 5(2), 20. https://doi.org/10.3390/pharmacy5020020





