1. Introduction
The failure of patients to adhere to their medication regimes is a multifaceted issue faced by all clinicians. The most thorough and well-thought-out treatment plans are ineffective if the patients do not take the medication as agreed upon. Medication adherence is a behaviour that can be defined as the degree to which the patient follows a mutually agreed upon course of treatment [
1,
2]. The literature generally accepts a person to be adherent if they take the medication as prescribed at least 80% of the time [
3,
4]. Medication adherence is a significant global issue: the World Health Organisation estimated that rates are as low as 50% in certain patient groups [
1,
3,
5]. There are a variety of reasons why individuals do not adhere to their medication: forgetfulness, lack of access, cost, or experiencing side effects are some factors identified [
1,
5]. Poor adherence contributes to treatment failure and deteriorating health outcomes for patients [
2,
6].
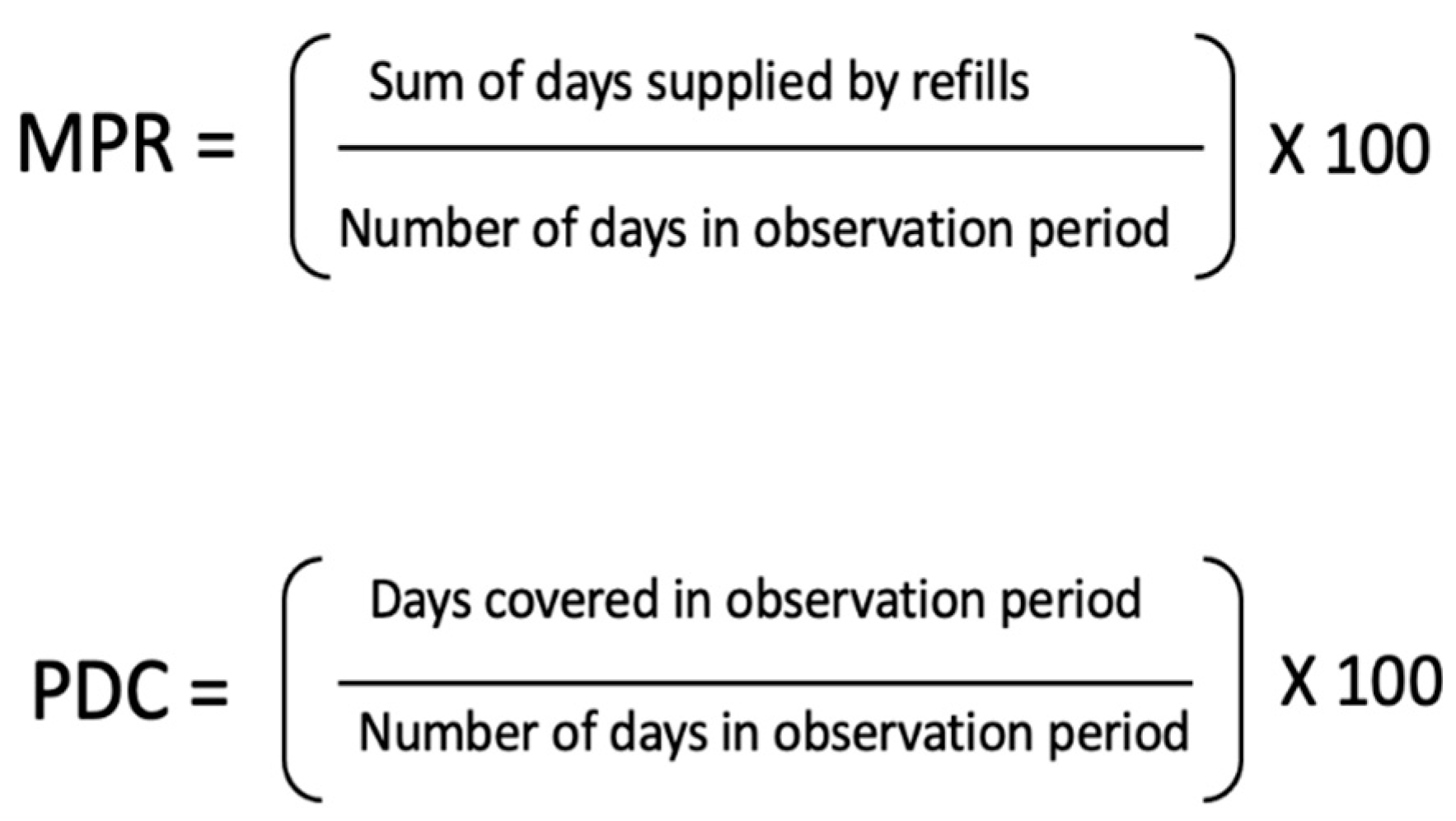
There are a range of methods used to measure medication adherence, such as measuring drug metabolites, pill counts, pharmacy dispensing records, patient reports and devices that record a pill container being opened. The most common method is to use pharmacy records in large observational cohort studies. This is because analysing dispensing or prescribing records is relatively cheap, non-invasive to participants, has less participations bias, and easy to conduct on a large-scale compared to other measures. A pharmacy records the days’ worth of a medicine dispensed over a period of time which can be used to calculate when the patient has medicine available. Medication possession ratio (MPR) and proportion of days covered (PDC) are the calculations most frequently used (
Figure 1). A subtle difference is that MPR can overestimate medication adherence if individuals collect their refills early. This is then reported as the pharmacies mean PDC or as a proportion of their patients with a PDC greater than 80% [
7].
Patients collecting their medication from a pharmacy is generally the final step in the care pathway. Research has identified that patient-pharmacist interactions at this point have the opportunity to enhance patients’ medication adherence [
5].
This review focuses on the two most studied types of pharmacies based on their ownership structure. While there is a lack of established definitions, we recognise the following.
Through their greater buying power, chain pharmacies are often able to offer lower priced medications than independent pharmacies [
10]. Evidence also suggests chain pharmacies offer more services although concern is being raised about a focus on profitability impacting service quality [
8]. The greater patient satisfaction reported by the users of independent pharmacies is believed to be a result of a greater focus on interpersonal interactions in these businesses [
11,
12]. The potential impact of patient’s pharmacy choice on their medication adherence has yet to be established.
By reviewing the literature where a variety of established pharmacy models exist, countries such as New Zealand and Australia with emerging discount pharmacy chains may be able to anticipate their impact.
Aims
This review aims to investigate if the users of chain pharmacies have greater medication adherence than the users of independent pharmacies. We will also investigate patterns in pharmacy patronage and its impact on medication adherence among patient groups, such as elderly, those with a low income, certain conditions, or those with a high medication burden. We hypothesise that the users of chain pharmacies will have greater rates of medication adherence because of the lower cost of medications.
2. Materials and Methods
A systematic narrative review was conducted using the EMBASE and MEDLINE(R) databases which we deemed suitable to capture our intended literature. Authors followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement for reporting systematic reviews and meta-analyses of studies that evaluate health-care interventions. This review was not registered.
The following search was used (“patient compliance” OR “medic* adherence” OR “medic* persistence” OR “medic* possession” OR “medic* compliance”) AND (“community pharmac*”, “dispensing channel”, “retail pharmac*”) AND (“chain”, “discount”, “mass retail*”).
The asterisks allow the search engine to include any terms which begin with that combination of letters, for example, both medicine and medication will be included in a search for medic*.
The EMBASE search window was between 1947 and the 11th of March 2022 and MEDLINE(R) was between 1946 and week 1 March 2022.
Inclusion Criteria
To be included, the study must have compared the rates of medication adherence between the users of independent and chain pharmacies. We did not exclude any papers because of the method used to measure medication adherence due to the lack of accepted definitions for the type of pharmacies, methods for measuring medication adherence, and covariates. Studies were excluded if they carried out an intervention aimed at improving medication adherence in a retail or community pharmacy without comparing it to a different type of pharmacy. Studies comparing medication adherence between specialty and community pharmacies were excluded.
We initially looked to compare mail-order pharmacies with traditional community pharmacies. However, in 2016 Fernandez et al. carried out a review that included most of the studies we had sought for retrieval for this section. As far as we are aware nothing new has been published on the topic since 2016 [
13].
J.N. removed duplicates by hand before screening titles and then abstracts. The remaining papers were fully appraised by J.N. and A.S. who had to agree on which paper meet the inclusion criteria. During the full article review, J.N. sought out studies referenced in the article that may meet our inclusion criteria. Two articles were identified and fully appraised but only Kalsekar et al. was included in our review [
14,
15]. The aims, methods, and results of included papers were then extracted by J.N. J.N. and A.S. collaborated to assess and interpret the results of each paper following the PRISMA guidelines and assess the quality and potential for bias using the Critical Appraisal Skills Programme tool (CASP) [
16]. No studies were excluded from our quality assessment.
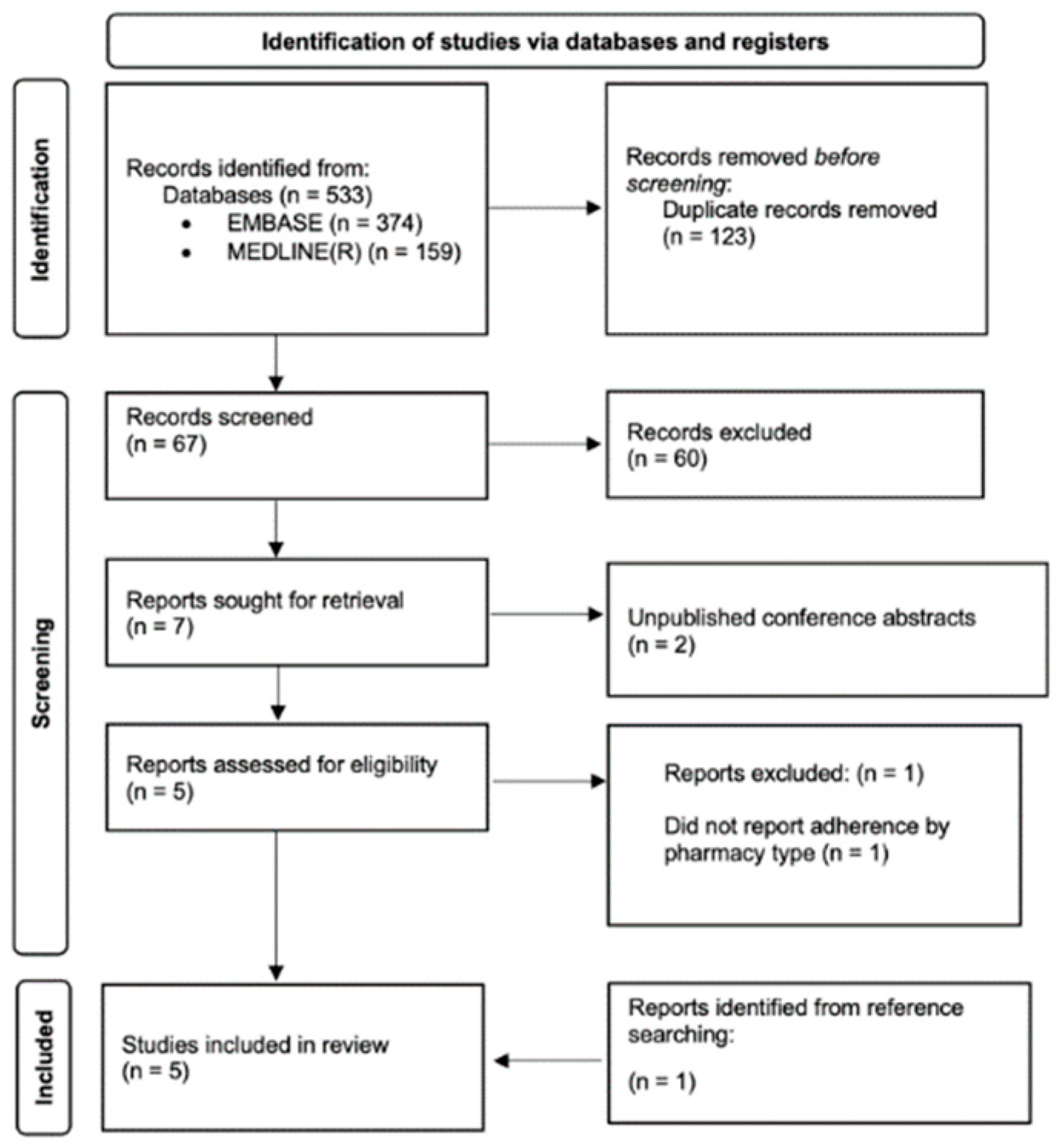
3. Results
Our search identified 410 potential articles. A total of seven were sought for full-text review, after which four articles were deemed to be eligible. Two further studies were found from reviewing the eligible papers’ references, one of which was included in this review, as shown in the PRISMA flow chart (
Figure 2). The main results are summarised below in
Table 1.
3.1. Quality Assessment
The studies were generally assessed to be of high quality; however, several areas of weakness were identified. Firstly, three studies failed to state how the type of pharmacy was defined, thus reducing the generalisability of the results [
14]. Another potential issue was the methods used to assign what type of pharmacy someone uses. By assigning someone to the type of pharmacy they collected the first prescription from, which two studies did, they do not account for people’s behaviour for the remainder of the study period [
4,
14]. Two separate studies reported the medication adherence for individual pharmacies but it is unclear how they accounted for participants using other pharmacies during the follow up period, they also the results were presented in a manner which made it difficult to interpret [
17,
18]. The completed CASP table may be viewed in the
Appendix A (
Table A1).
3.2. Summary of Findings
The majority of the included studies took place in North America, followed patients’ medication adherence for 12 months using pharmacy records data, and were all published in the past 15 years. Two of the studies reported medication adherence at a pharmacy level and one used a self-reported measure of medication adherence.
Varying rates of medication adherence were seen across the five studies. Kalsekar et al. found independent pharmacy users to have a mean MPR for oral anti diabetic medications of 0.90 (95% CI 0.89–0.91) compared to 0.88 (95% CI 0.87–0.89) for chain pharmacy users, a statistically significant difference [
14]. Urick et al. also observed that independent pharmacy users had greater medication adherence to oral anti diabetic medications as well as a custom measure of chronic medications to the average pharmacy, however, there was no significant difference for statins and renin-angiotensin system antagonists (RASA) [
18]. Urick et al. created the custom measure of chronic medicine by calculating the PDC for 71 medicine classes related to a range of common chronic diseases to assess patients overall medication adherence [
19]. Evans et al. found the proportion of new statin patients with >80% PDC over a 12 month period was 55.0% for the users of chain pharmacies and 54.1% for the users of independent pharmacies, although the observed difference was not statistically significant [
4]. Jacobs et al. were unable to detect a difference in self-reported medication adherence between different types of pharmacy [
8]. In contrast, Desai et al. found the users of chain pharmacies to have the greatest medication adherence [
17]. Desai et al. ranked pharmacies by mean PDC and categorised the top 50% as high performers and the bottom 50% to be low performers. The odds ratio of an independent pharmacy being a low performer compared to chain pharmacies was found to be 1.23 (95% CI 1.10–1.37), 1.68 (95% CI 1.56–1.80), and 1.47 (95% CI 1.37–1.58) for oral anti diabetic medications, RASA, and statins, respectively [
17].
While the included studies had comparable objectives and methods, variance in the sample populations and secondary outcomes, as shown in
Table 1, allows us to comment on the possibility that the different pharmacy types are unequally impacting certain groups of people. We have identified four themes where medication adherence is potentially being unequally affected by different types of pharmacies.
3.3. Low Income
Several studies concluded that low income could predict poor medication adherence [
4,
17]. Desai et al. reported that a pharmacy located in a county with a low median income was more likely to be categorised as a low medication adherence performer [
17]. Evans et al. found that low-income drug coverage could predict low adherence with an adjusted odds ratio of 0.81 (95% CI 0.71–0.92), compared to those without known low-income drug coverage [
4]. They also reported that a greater proportion of low-income patients used independent pharmacies over the generally cheaper chain pharmacies [
4].
Two studies took their samples from Medicaid data, a program designed to provide health coverage to low-income Americans [
14,
20]. Both found independent pharmacy users to have greater medication adherence than chain pharmacy users suggesting that low-income patients have greater medication adherence when using independent pharmacies.
3.4. Medication Burden
Medication burden can be defined as the impact of healthcare on a patient’s function and well-being [
21]. The users of independent pharmacies were found to have a greater medication burden than the users of chain pharmacies [
4,
14]. Kalsekar et al. reported that independent pharmacy users had significantly more prescriptions for chronic conditions dispensed than the users of chain pharmacies over a 12 month period [
14]. Evans et al. found that independent pharmacy users concurrently had more classes of medications dispensed in the year preceding the observation period than the users of other types of pharmacies [
4].
Evans et al. reported that patients collecting one or more medications, in addition to the statin that was studied, are more likely to be adherent to their medication regime [
4]. Similarly, Kaleskar et al. found the number of prescriptions for chronic medications someone collected to be positively associated with medication adherence [
14].
3.5. Age
Kalsekar et al. and Jacobs et al. both reported that medication adherence increases as individuals age increases [
8]. Similarly, Evans et al. also found that those over 65 years old had greater medication adherence, than those under the age of 65 years, irrespective of the type of pharmacy they use, although a greater portion of them chose to use independent pharmacies over chain pharmacies [
4].
Kalsekar et al. and Desai et al.’s sample selection gives some insight into the impact the type of pharmacy someone uses has on their medication adherence depending on their age [
14,
17]. Kalsekar et al. only included under the age of 65 years old and reported the users of independent pharmacies to have greater medication adherence than the users of chain pharmacies [
14]. In contrast to Desai et al. used Medicare data which produced a sample largely composed of over 65 year olds [
17]. To be eligible for Medicare you must be over the age of 65 years old, have a qualifying disability or permanent kidney failure [
22]. Desai et al. reported significant odds ratios of independent pharmacy users having poor medication adherence compared to the users of chain pharmacies [
17].
3.6. Medications
Oral anti diabetic medications were investigated by several papers [
14,
17,
18]. Urick et al. found patients to have greater medication adherence to this class of medications when using independent pharmacies. Kaleskar et al. only investigated oral anti diabetic medications and found adherence rates to be greater for users of independent pharmacies. Desai et al.’s findings were in contrast, reporting an odds ratio of 1.23 (95% CI 1.10–1.37) that an independent pharmacy would be a low performer for adherence to oral anti diabetic medications.
Statin adherence was reported by 3 of our studies [
4,
17,
18]. Desai et al. found independent pharmacy patrons to have worse statin adherence. The odds ratio of an independent pharmacy being a low performer for statin adherence was 1.47 (95% CI 1.37–1.58) compared to a chain pharmacy. However, Urick et al. and Evans et al.’s did not find a significant difference in statin adherence between the users of independent and chain pharmacies.
However, Urick et al. disagreed with Desai et al. regarding RASA adherence. Urick et al. found that using an independent pharmacy did not have a significant effect on RASA adherence. In contrast, Desai et al. showed chain pharmacy users to have great RASA adherence, reporting the odds ratio of an independent pharmacy being a poor performer to be 1.68 (95% CI 1.56–1.80) compared to a chain pharmacy.
4. Discussion
The five studies included in this review could not conclude that chain pharmacy users had greater rates of adherence than the users of independent pharmacies. However, those with a low income, high medication burden, increased age, or taking specific medications appear to be disproportionately impacted by the type of pharmacy they use. Exploring these themes may expand on how the type of pharmacy someone uses affects their medication adherence.
4.1. Low-Income
Those with a low-income tend to use independent pharmacies more frequently than chain pharmacies and potentially have better medication adherence when they do so. This is demonstrated by the two studies whose samples were largely composed of beneficiaries reporting that independent pharmacy users have greater medication adherence [
14,
18].
The cost of medications can be a major barrier to medication adherence and is a key difference between chain and independent pharmacies [
5]. A 2015 cross-sectional study of 60,000 pharmacies across the United States by Luo et al. found the cost of medications in independent pharmacies to be 1.61 (95% CI 1.58–1.64) times that of a large pharmacy chain [
10]. We postulated that those with a lower income would have a greater demand for low-cost medications leading them to frequent chain pharmacies. However, that is not what the findings of this review have observed.
The two studies, Evans et al. and Desai et al., which investigated the effects of income agreed with the literature that low income is a predictor of low medication adherence [
3,
5,
23,
24,
25].
Education is a variable potentially linking income and medication adherence. A lower level of education is associated with both a lower income and lower health literacy [
26,
27]. Health literacy describes a person’s ability to interpret health information and use it to make decisions about their care [
28]. Poor health literacy has been shown to lead to lower medication adherence [
5,
25,
29]. Someone with poor health literacy may experience greater improvements in their medication adherence from high quality interactions with a pharmacist, as the literature suggests occurs in independent pharmacies, than receiving cheaper medication. Hence, our studies report that low-income patients have better medication adherence in independent pharmacies [
30,
31].
4.2. Medication Burden
Two studies reported that independent pharmacy users had a greater medication burden than the users of chain pharmacies [
4,
14].
The findings of this review contrast with the literature, as our included studies reported greater medication adherence among individuals with a higher number of medications [
3,
5].
These findings were unexpected as patients with a high medication burden may be more likely to have medication changes to improve their therapy. This effect may compound if the patients are non-adherent, as the prescriber may be more likely to augment or adjust the patient’s medications furthering their medication burden and the complexity of their regime which in turn makes it harder to adhere to the medication regime. In addition, a known weakness of measuring medication adherence using pharmacy record data is that an individual starting and stopping medications throughout the follow up period will cause the patient to be recorded as non-adherent regardless of whether the prescriber leads the change or not.
By having a higher proportion of patients with a high medication burden independent pharmacies’ are facing more complex patient care demands [
5].
4.3. Age
Evans et al. reported that older individuals tend to use independent pharmacies, which is supported by the literature [
32,
33]. However, three of our studies agreed that older individuals have greater medication adherence which is met with some conjecture from the literature [
4,
8,
14]. A 2013 systematic review of 51 studies into medication adherence reported age as having an inconsistent impact on medication adherence [
1,
5,
29]. The potential for different types of pharmacies to affect adherence unevenly depending on the patient’s age is worthy of future study.
4.4. Medications
There are several medication specific differences observed in the studies we have included. Oral anti diabetic medications tended to have greater adherence at independent pharmacies while RASA and statins tended to have better adherence at chain pharmacies [
4,
14,
17,
18].
When treating uncontrolled diabetes best practice recommends augmenting therapy with another oral anti diabetic medication class creating a more complex regime [
34]. In contrast, RASA or statin therapy is less complex and would typically only involve one medication from each class [
35,
36]. Similar to the medication burden section, patients with more complex medication regimes may be benefiting from the additional pharmacist service observed in independent pharmacies [
5].
Independent pharmacy users tend to have a lower income, be older, and take more medications than the users of chain pharmacies. These themes suggest the users of independent pharmacies are biased face more barriers to medication adherence. However, that is not what is being observed which postulates that independent pharmacies are positively influencing their user’s adherence.
4.5. Limitations
The themes discussed in this review is not an exhaustive list, as many other factors affect a person’s adherence [
5]. Further research into who uses different types of pharmacies and how individuals decide which pharmacies to frequent would advance our understanding of this issue.
The lack of information describing how differ pharmacies may reduce the generalisability of this review since we do not know how the studied pharmacies compare to the those, we wish to compare them to.
Most medication adherence studies focus on chronic conditions because they generally require lifelong treatment, have serious consequences for non-adherence, and are the easiest to measure medication adherence on a large scale [
25]. There is a lack of research investigating the impact pharmacy type has on adherence to short term medication.
All of the included studies except Jacobs et al. used pharmacy records data to calculate their measures of medication adherence. An established limitation of this methodology is that it is assumed that a medication dispensed is a medication taken [
37]. However, it is possible that the portion of medication dispensed but not taken differs between independent and chain pharmacy users. Paying less for a medication may reduce the perceived value of the medication making it less likely that they take it after having it dispensed, we believe this is an area worthy of further research.
Like any review, these findings may be impacted by bias surrounding the decision to publish research, particularly due to the business implications of this area of study.
5. Conclusions
The findings of this review were unable to confirm our hypothesis that the users of chain pharmacies have greater medication adherence than those who used independent pharmacies. Patient characteristics such as low income, high medication burden, and age appear to be associated with both poor medication adherence and frequenting independent pharmacies more than chain pharmacies. However, independent pharmacy users’ medication adherence is at least comparable to those who use chain pharmacies. There may be an unknown factor that draws adherent patients to independent pharmacies or a difference in the service independent pharmacies provide which improves medication adherence. Establishing the differences between independent and chain pharmacies and investigating how different groups’ preferences drive them towards different types of pharmacies could help improve patients’ medication adherence and health outcomes.
Author Contributions
Conceptualization, J.N. and A.S.; methodology, J.N. and A.S.; validation, A.S., S.S. and C.A.M.; formal analysis, J.N.; investigation, J.N. and A.S.; data curation, J.N.; writing—original draft preparation, J.N.; writing—review and editing, J.N., A.S., S.S. and C.A.M.; visualization, J.N.; supervision, A.S.; project administration, J.N. All authors have read and agreed to the published version of the manuscript.
Funding
J.N was supported by a University of Otago doctoral scholarship.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A
Table A1.
CASP quality assessment.
Table A1.
CASP quality assessment.
| | Are the Results of the Review Valid? | What are the Results? | Will the Results Help Locally? |
|---|
| Author | Clearly Focused Issue | Cohort Recruitment | Exposure Accurately Measured to Minimise Bias | Outcome Accurately Measured to Minimise Bias | Identified and Accounted for Confounding Factors | Follow Up Was Complete and Sufficiently Long | Overall Results | Precision of Results | The Results Are Believable | Applicable to Local Population | Results Fit with Other Evidence |
|---|
Kalsekar et al.,
2007 [14] | Yes | Yes | Used index script to define user. Did not define pharmacy types | MPR | Yes | 12 months | Yes | Statistically significant | Yes | Yes | Yes |
Evans et al.,
2009 [4] | Yes | Yes | Used index script to define user. Defined pharmacy types | PDC >80% | Yes | 3 years | Yes | Statistically significant | Yes | Yes | Yes |
Desai et al.,
2016 [17] | Moderate | Yes | Type of pharmacy.
Did not define pharmacies | Mean PDC of users used to rank pharmacies | Yes | 6 months | Unusual measure used | Statistically significant | Yes | Moderately generalisable | Yes |
Urick et al.,
2020 [18] | Yes
(Pharmacy type a secondary outcome) | Yes | Did not define pharmacy type | Proportion of patients with a PDC >80% | Yes | 12 months | Hard to interpret | Some medications significant some not | Yes | Yes | Yes |
Jacobs et al.,
2020 [8] | Yes | Yes, but missed a pharmacy type which declined to participate | Yes, and clearly defined pharmacy types | Yes, self-reported adherence MARS | Yes | NA | Yes | Not statistically significant | Yes | Yes | Yes |
References
- World Health Organization. Adherence to Long-Term Therapies: Evidence for Action; World Health Organization: Geneva, Switzerland, 2003.
- Ho, P.M.; Bryson, C.L.; Rumsfeld, J.S. Medication Adherence. Circulation 2009, 119, 3028–3035. [Google Scholar] [CrossRef]
- Rolnick, S.J.; Pawloski, P.A.; Hedblom, B.D.; Asche, S.E.; Bruzek, R.J. Patient characteristics associated with medication adherence. Clin. Med. Res. 2013, 11, 54–65. [Google Scholar] [CrossRef]
- Evans, C.D.; Eurich, D.T.; Lamb, D.A.; Taylor, J.G.; Jorgenson, D.J.; Semchuk, W.M.; Mansell, K.D.; Blackburn, D.F. Retrospective observational assessment of statin adherence among subjects patronizing different types of community pharmacies in Canada. J. Manag. Care Pharm. 2009, 15, 476–484. (In English) [Google Scholar] [CrossRef]
- Kardas, P.; Lewek, P.; Matyjaszczyk, M. Determinants of patient adherence: A review of systematic reviews. Front. Pharmacol. 2013, 4, 91. [Google Scholar] [CrossRef]
- Sokol, M.C.; McGuigan, K.A.; Verbrugge, R.R.; Epstein, R.S. Impact of Medication Adherence on Hospitalization Risk and Healthcare Cost. Med. Care 2005, 43, 521–530. Available online: http://www.jstor.org/stable/3768169 (accessed on 24 March 2022). [CrossRef]
- Anghel, L.A.; Farcas, A.M.; Oprean, R.N. An overview of the common methods used to measure treatment adherence. Med. Pharm. Rep. 2019, 92, 117–122. (In English) [Google Scholar] [CrossRef]
- Jacobs, S.; Hann, M.; Bradley, F.; Elvey, R.; Fegan, T.; Halsall, D.; Hassell, K.; Wagner, A.; Schafheutle, E.I. Organisational factors associated with safety climate, patient satisfaction and self-reported medicines adherence in community pharmacies. Res. Soc. Adm. Pharm. 2020, 16, 895–903. (In English) [Google Scholar] [CrossRef]
- Perepelkin, J.; Dobson, R.T. Influence of ownership type on role orientation, role affinity, and role conflict among community pharmacy managers and owners in Canada. Res. Soc. Adm. Pharm. 2010, 6, 280–292. [Google Scholar] [CrossRef]
- Luo, J.; Kulldorff, M.; Sarpatwari, A.; Pawar, A.; Kesselheim, A.S. Variation in Prescription Drug Prices by Retail Pharmacy Type. Ann. Intern. Med. 2019, 171, 605–611. [Google Scholar] [CrossRef]
- Briesacher, B.; Corey, R. Patient satisfaction with pharmaceutical services at independent and chain pharmacies. Am. J. Health-Syst. Pharm. 1997, 54, 531–536. [Google Scholar] [CrossRef]
- Mackeigan, L.D.; Larson, L.N. Development and validation of an instrument to measure patient satisfaction with pharmacy services. Med. Care 1989, 27, 522–536. [Google Scholar] [CrossRef]
- Fernandez, E.V.; McDaniel, J.A.; Carroll, N.V. Examination of the link between medication adherence and use of mail-order pharmacies in chronic disease states. J. Manag. Care Spec. Pharm. 2016, 22, 1247–1259. [Google Scholar] [CrossRef]
- Kalsekar, I.; Sheehan, C.; Peak, A. Utilization patterns and medication adherence in patients with type 2 diabetes: Variations based on type of pharmacy (chain vs independent). Res. Soc. Adm. Pharm. 2007, 3, 378–391. (In English) [Google Scholar] [CrossRef]
- Pedan, A.; Varasteh, L.; Schneeweiss, S. Analysis of factors associated with statin adherence in a hierarchical model considering physician, pharmacy, patient, and prescription characteristics. J. Manag. Care Pharm. 2007, 13, 487–496. (In English) [Google Scholar] [CrossRef]
- Long, H.A.; French, D.P.; Brooks, J.M. Optimising the value of the critical appraisal skills programme (CASP) tool for quality appraisal in qualitative evidence synthesis. Res. Methods Med. Health Sci. 2020, 1, 31–42. [Google Scholar] [CrossRef]
- Desai, V.; Nau, D.; Conklin, M.; Heaton, P.C. Impact of Environmental Factors on Differences in Quality of Medication Use: An Insight for the Medicare Star Rating System. J. Manag. Care Spec. Pharm. 2016, 22, 779–786. (In English) [Google Scholar] [CrossRef]
- Urick, B.Y.; Bhosle, M.; Farley, J.F. Patient Medication Adherence Among Pharmacies Participating in a North Carolina Enhanced Services Network. J. Manag. Care Spec. Pharm. 2020, 26, 718–722. (In English) [Google Scholar] [CrossRef]
- Urick, B.Y.; Ferreri, S.P.; Shasky, C.; Pfeiffenberger, T.; Trygstad, T.; Farley, J.F. Lessons learned from using global outcome measures to assess community pharmacy performance. J. Manag. Care Spec. Pharm. 2018, 24, 1278–1283. [Google Scholar] [CrossRef]
- Medicaid.gov. Medicaid: Eligibility. Available online: https://www.medicaid.gov/medicaid/eligibility/index.html (accessed on 2 May 2022).
- Eton, D.T.; Ramalho de Oliveira, D.; Egginton, J.S.; Ridgeway, J.L.; Odell, L.; May, C.R.; Montori, V.M. Building a measurement framework of burden of treatment in complex patients with chronic conditions: A qualitative study. Patient Relat Outcome Meas 2012, 3, 39–49. (In English) [Google Scholar] [CrossRef]
- Social Security Administration. Medicare Benefits. Available online: https://www.ssa.gov/benefits/medicare/#anchor1 (accessed on 3 May 2022).
- Fernandez-Lazaro, C.I.; Adams, D.P.; Fernandez-Lazaro, D.; Garcia-González, J.M.; Caballero-Garcia, A.; Miron-Canelo, J.A. Medication adherence and barriers among low-income, uninsured patients with multiple chronic conditions. Res. Soc. Adm. Pharm. 2019, 15, 744–753. [Google Scholar] [CrossRef]
- Polonsky, W.H.; Henry, R.R. Poor medication adherence in type 2 diabetes: Recognizing the scope of the problem and its key contributors. Patient Prefer. Adherence 2016, 10, 1299–1307. (In English) [Google Scholar] [CrossRef] [PubMed]
- DiMatteo, M.R. Variations in Patients’ Adherence to Medical Recommendations: A Quantitative Review of 50 Years of Research. Med. Care 2004, 42, 200–209. Available online: http://www.jstor.org/stable/4640729 (accessed on 9 May 2022). [CrossRef] [PubMed]
- Muller, A. Education, income inequality, and mortality: A multiple regression analysis. BMJ 2002, 324, 23. [Google Scholar] [CrossRef] [PubMed]
- Van Der Heide, I.; Wang, J.; Droomers, M.; Spreeuwenberg, P.; Rademakers, J.; Uiters, E. The relationship between health, education, and health literacy: Results from the Dutch Adult Literacy and Life Skills Survey. J. Health Commun. 2013, 18, 172–184. [Google Scholar] [CrossRef] [PubMed]
- Berkman, N.D.; Davis, T.C.; McCormack, L. Health literacy: What is it? J. Health Commun. 2010, 15, 9–19. [Google Scholar] [CrossRef]
- Kripalani, S.; Gatti, M.E.; Jacobson, T.A. Association of age, health literacy, and medication management strategies with cardiovascular medication adherence. Patient Educ. Couns. 2010, 81, 177–181. [Google Scholar] [CrossRef]
- Fritsch, M.A.; Lamp, K.C. Low Pharmacist Counseling Rates in the Kansas City, Missouri, Metropolitan Area. Ann. Pharmacother. 1997, 31, 984–991. [Google Scholar] [CrossRef]
- Keehn, J. Independent Drug Stores Win in CR Survey. Available online: https://www.consumerreports.org/cro/news/2011/04/independent-drug-stores-win-in-cr-survey/index.htm (accessed on 27 April 2022).
- Franic, D.M.; Haddock, S.M.; Leslie Tootle, T.; Nathan, W. Pharmacy patronage: Identifying key factors in the decision making process using the determinant attribute approach. J. Am. Pharm. Assoc. 2008, 48, 71–86a. [Google Scholar] [CrossRef]
- Schommer, J.C. The Effect of Age on Pharmacy Patronage: Is Locational Convenience a Lurking Variable? J. Pharm. Mark. Manag. 1994, 9, 33–46. [Google Scholar] [CrossRef]
- National Institute for Health and Care Excellence. Type 2 Diabetes in Adults: Management. Available online: https://www.nice.org.uk/guidance/ng28 (accessed on 18 July 2022).
- National Institute for Health and Care Excellence. Cardiovascular Disease: Risk Assessment and Reduction, Including Lipid Modification. Available online: https://www.nice.org.uk/guidance/cg181 (accessed on 18 July 2022).
- National Institute for Health and Care Excellence. Hypertension in Adults: Diagnosis and Management. Available online: https://www.nice.org.uk/guidance/ng136/chapter/Recommendations#choosing-antihypertensive-drug-treatment-for-people-with-or-without-type-2-diabetes (accessed on 18 July 2022).
- Rickles, N.M.; Svarstad, B.L. Relationships between multiple self-reported nonadherence measures and pharmacy records. Res. Soc. Adm. Pharm. 2007, 3, 363–377. [Google Scholar] [CrossRef]
| Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).