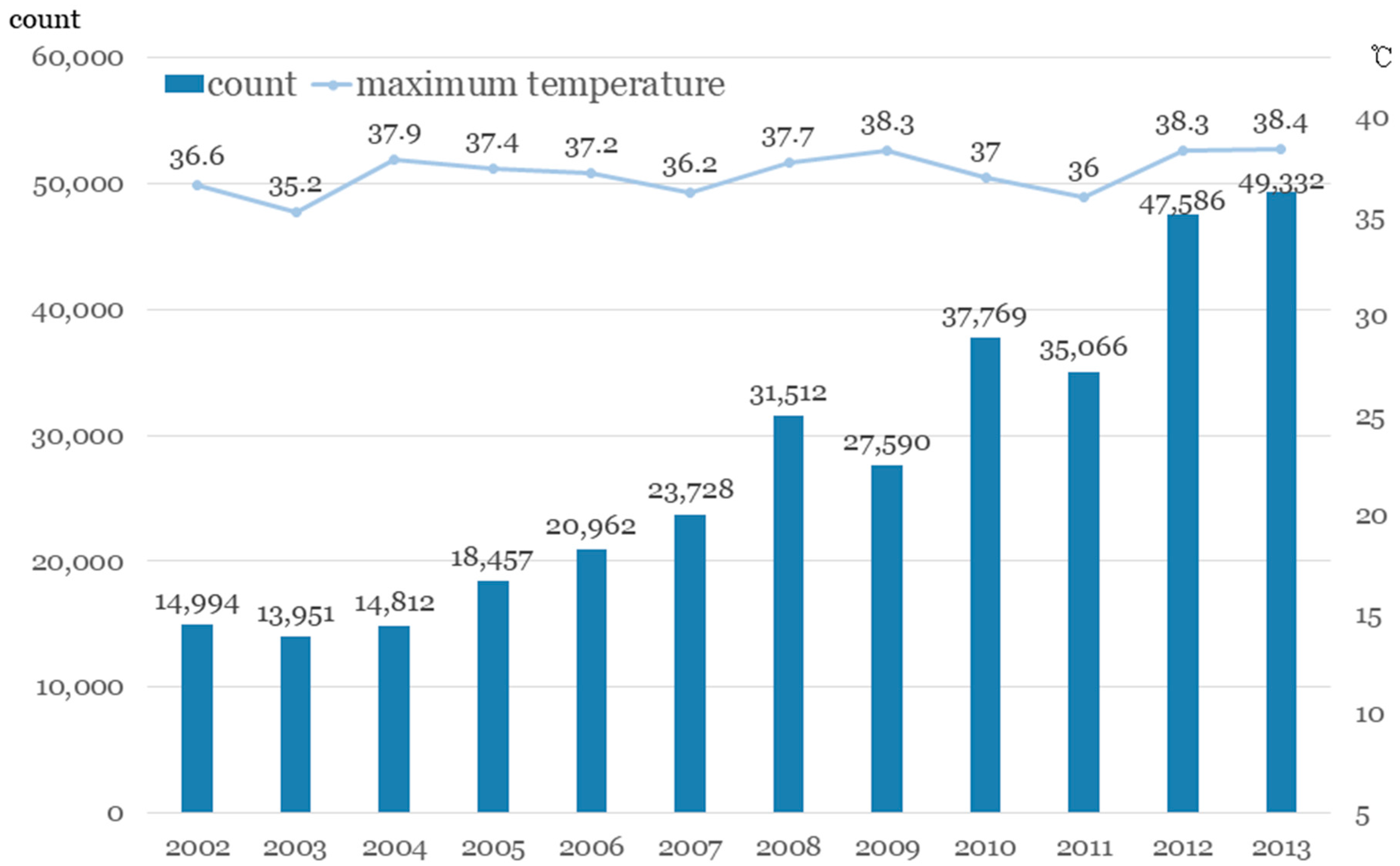
Trend of Outbreak of Thermal Illness Patients Based on Temperature 2002–2013 in Korea
Abstract
1. Introduction
2. Methods
2.1. Study Design and Setting
2.2. Data Collection and Variables
2.3. Environmental Data
2.4. Study Population
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Appendix A
| Year | Resident Population | Daily Maximum Temperature (°C) | Number of Days above Threshold (29.5 °C) |
|---|---|---|---|
| 2002 | 48,125,745 | 36.6 | 22 |
| 2003 | 48,308,386 | 35.2 | 6 |
| 2004 | 48,485,314 | 37.9 | 31 |
| 2005 | 48,683,040 | 37.4 | 32 |
| 2006 | 48,887,027 | 37.2 | 26 |
| 2007 | 49,130,354 | 36.2 | 26 |
| 2008 | 49,404,648 | 37.7 | 32 |
| 2009 | 49,656,756 | 38.3 | 16 |
| 2010 | 49,879,812 | 37.0 | 35 |
| 2011 | 50,111,476 | 36.0 | 23 |
| 2012 | 50,345,325 | 38.3 | 31 |
| 2013 | 50,558,952 | 38.4 | 43 |
References
- Woodward, A.; Smith, K.R.; Campbell-Lendrum, D.; Chadee, D.D.; Honda, Y.; Liu, Q.; Olwoch, J.; Revich, B.; Sauerborn, R.; Chafe, Z.; et al. Climate change and health: On the latest IPCC report. Lancet 2014, 383, 1185–1189. [Google Scholar] [CrossRef]
- Intergovernmental Panel on Climate Change. Climate Change 2007: The Physical Science Basis. Available online: https://www.ipcc.ch/publications_and_data/publications_ipcc_fourth_assessment_report_wg1_report_the_physical_science_basis.htm (accessed on 13 December 2016).
- Wolf, T.; Martinez, G.S.; Cheong, H.K.; Williams, E.; Menne, B. Protecting health from climate change in the WHO European Region. Int. J. Environ. Res. Public Health 2014, 11, 6265–6280. [Google Scholar] [CrossRef] [PubMed]
- Meehl, G.A.; Tebaldi, C. More intense, more frequent, and longer lasting heat waves in the 21st century. Science 2004, 305, 994–997. [Google Scholar] [CrossRef] [PubMed]
- National Institute of Meteorological Science. Climate Change Scenario Report. 2011. Available online: http://www.climate.go.kr/home/cc_data/scenario_report.pdf (accessed on 13 December 2016).
- Marto, N. Heat waves: Health impacts. Acta Med. Port. 2005, 18, 467–474. [Google Scholar] [PubMed]
- Howe, A.S.; Boden, B.P. Heat-related illness in athletes. Am. J. Sports Med. 2007, 35, 1384–1395. [Google Scholar] [CrossRef] [PubMed]
- Schmeltz, M.T.; Petkova, E.P.; Gamble, J.L. Economic Burden of Hospitalizations for Heat-Related Illnesses in the United States, 2001–2010. Int. J. Environ. Res. Public Health 2016, 13. [Google Scholar] [CrossRef] [PubMed]
- Lim, Y.H.; Kim, H.; Hong, Y.C. Variation in mortality of ischemic and hemorrhagic strokes in relation to high temperature. Int. J. Biometeorol. 2013, 57, 145–153. [Google Scholar] [CrossRef] [PubMed]
- WHO. Climate Change is Affecting Our Health. 2009. Available online: http://www.who.int/globalchange/publications/climate_change_health_brochure/en/ (accessed on 13 December 2016).
- Rossati, A. Global Warming and Its Health Impact. Int. J. Occup. Environ. Med. 2017, 8, 7–20. [Google Scholar] [CrossRef] [PubMed]
- Ahdoot, S.; Pacheco, S.E. Council on Environmental Health. Global Climate Change and Children’s Health. Pediatrics 2015, 136, 992–997. [Google Scholar] [CrossRef] [PubMed]
- Johnson, H.; Kovats, R.S.; McGregor, G.; Stedman, J.; Gibbs, M.; Walton, H.; Cook, L.; Black, E. The impact of the 2003 heat wave on mortality and hospital admissions in England. Health Stat. Q. 2005, 25, 6–11. [Google Scholar] [CrossRef]
- Semenza, J.C.; McCullough, J.E.; Flanders, W.D.; McGeehin, M.A.; Lumpkin, J.R. Excess hospital admissions during the July 1995 heat wave in Chicago. Am. J. Prev. Med. 1999, 16, 269–277. [Google Scholar] [CrossRef]
- Medina-Ramón, M.; Zanobetti, A.; Cavanagh, D.P.; Schwartz, J. Extreme temperatures and mortality: Assessing effect modification by personal characteristics and specific cause of death in a multi-city case-only analysis. Environ. Health Perspect. 2006, 114, 1331–1336. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.T.; Lim, Y.H.; Woodward, A.; Kim, H. Heat-attributable deaths between 1992 and 2009 in Seoul, South Korea. PLoS ONE 2015, 10, e0118577. [Google Scholar] [CrossRef] [PubMed]
- Ha, J.; Kim, H. Changes in the association between summer temperature and mortality in Seoul, South Korea. Int. J. Biometeorol. 2013, 57, 535–544. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.K.; Lee, H.A.; Park, H. Modifying Effect of Heat Waves on the Relationship between Temperature and Mortality. J. Korean Med. Sci. 2016, 31, 702–708. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Ha, J.S.; Park, J. High temperature, heat index, and mortality in 6 major cities in South Korea. Arch. Environ. Occup. Health 2006, 61, 265–270. [Google Scholar] [CrossRef] [PubMed]
- Wu, G.; Liu, Y.; He, B.; Bao, Q.; Duan, A.; Jin, F.F. Thermal controls on the Asian summer monsoon. Sci. Rep. 2012, 2, 404. [Google Scholar] [CrossRef] [PubMed]
- Seong, S.C.; Kim, Y.Y.; Khang, Y.H.; Heon Park, J.; Kang, H.J.; Lee, H.; Do, C.H.; Song, J.S.; Hyon Bang, J.; Ha, S.; et al. Data resource profile: The National Health Information Database of the National Health Insurance Service in South Korea. Int. J. Epidemiol. 2017, 46, 799–800. [Google Scholar]
- Korean Ministry of Environment. Annual Report of Ambient Air Quality in Korea. 2013. Available online: http://library.me.go.kr/search/DetailView.ax?sid=11&cid=5584427 (accessed on 13 December 2016).
- Kovats, R.S.; Hajat, S.; Wilkinson, P. Contrasting patterns of mortality and hospital admissions during hot weather and heat waves in Greater London, UK. Occup. Environ. Med. 2004, 61, 893–898. [Google Scholar] [CrossRef] [PubMed]
- Liang, W.M.; Liu, W.P.; Chou, S.Y.; Kuo, H.W. Ambient temperature and emergency room admissions for acute coronary syndrome in Taiwan. Int. J. Biometeorol. 2008, 52, 223–229. [Google Scholar] [CrossRef] [PubMed]
- Lin, S.; Luo, M.; Walker, R.J.; Liu, X.; Hwang, S.A.; Chinery, R. Extreme high temperatures and hospital admissions for respiratory and cardiovascular diseases. Epidemiology 2009, 20, 738–746. [Google Scholar] [CrossRef] [PubMed]
- Bayentin, L.; El Adlouni, S.; Ouarda, T.B.; Gosselin, P.; Doyon, B.; Chebana, F. Spatial variability of climate effects on ischemic heart disease hospitalization rates for the period 1989–2006 in Quebec, Canada. Int. J. Health Geogr. 2010, 9, 5. [Google Scholar] [CrossRef] [PubMed]
- Barnett, A.G.; Dobson, A.J.; McElduff, P.; Salomaa, V.; Kuulasmaa, K.; Sans, S. WHO MONICA Project. Cold periods and coronary events: An analysis of populations worldwide. J. Epidemiol. Community Health 2005, 59, 551–557. [Google Scholar] [CrossRef] [PubMed]
- Hjort, J.; Suomi, J.; Kayhko, J. Extreme urban-rural temperatures in the coastal city of Turku, Finland: Quantification and visualization based on a generalized additive model. Sci. Total Environ. 2016, 569–570, 507–517. [Google Scholar] [CrossRef] [PubMed]
- Anderson, B.G.; Bell, M.L. Weather-related mortality: How heat, cold, and heat waves affect mortality in the United States. Epidemiology 2009, 20, 205–213. [Google Scholar] [CrossRef] [PubMed]
- Chung, J.Y.; Honda, Y.; Hong, Y.C.; Pan, X.C.; Guo, Y.L.; Kim, H. Ambient temperature and mortality: An international study in four capital cities of East Asia. Sci. Total Environ. 2009, 408, 390–396. [Google Scholar] [CrossRef] [PubMed]
- Knowlton, K.; Rotkin-Ellman, M.; King, G.; Margolis, H.G.; Smith, D.; Solomon, G.; Trent, R.; English, P. The 2006 California heat wave: Impacts on hospitalizations and emergency department visits. Environ. Health Perspect. 2009, 117, 61–67. [Google Scholar] [CrossRef] [PubMed]
- Lippmann, S.J.; Fuhrmann, C.M.; Waller, A.E.; Richardson, D.B. Ambient temperature and emergency department visits for heat-related illness in North Carolina, 2007–2008. Environ. Res. 2013, 124, 35–42. [Google Scholar] [CrossRef] [PubMed]
- Sheffield, P.E.; Landrigan, P.J. Global climate change and children’s health: Threats and strategies for prevention. Environ. Health Perspect. 2011, 119, 291–298. [Google Scholar] [CrossRef] [PubMed]
- Iñiguez, C.; Schifano, P.; Asta, F.; Michelozzi, P.; Vicedo-Cabrera, A.; Ballester, F. Temperature in summer and children’s hospitalizations in two Mediterranean cities. Environ. Res. 2016, 150, 236–244. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.; Hu, W.; Su, H.; Turner, L.R.; Ye, X.; Wang, J.; Tong, S. Extreme temperatures and paediatric emergency department admissions. J. Epidemiol. Community Health 2014, 68, 304–311. [Google Scholar] [CrossRef] [PubMed]
- Oberlin, M.; Tubery, M.; Cances-Lauwers, V.; Ecoiffier, M.; Lauque, D. Heat-related illnesses during the 2003 heat wave in an emergency service. Emerg. Med. J. 2010, 27, 297–299. [Google Scholar] [CrossRef] [PubMed]
| Region | Area (km2) | Population | Agricultural Population (%) | Weather Observatories |
|---|---|---|---|---|
| Central (Region 1) | 11,818 | 25,258,000 | 0 | 9 |
| Northeast (Region 2) | 16,790 | 1,542,000 | 10.7 | 13 |
| Northwest (Region 3) | 16,615 | 5,275,000 | 9.5 | 11 |
| Southwest (Region 4) | 20,838 | 5,253,000 | 10.3 | 27 |
| Southeast (Region 5) | 32,278 | 13,218,000 | 5.7 | 29 |
| Island (Region 6) | 1849 | 593,000 | 13.9 | 4 |
| Variables | Total | Region 1 | Region 2 | Region 3 | Region 4 | Region 5 | Region 6 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | N | % | N | % | N | % | ||
| Total | 335,759 | 100.0 | 105,226 | 100.0 | 6450 | 100.0 | 65,199 | 100.0 | 68,176 | 100.0 | 86,715 | 100.0 | 3993 | 100.0 | |
| Year | 2002 | 14,994 | 4.5 | 5748 | 5.5 | 334 | 5.2 | 3281 | 5.0 | 3246 | 4.8 | 2288 | 2.6 | 97 | 2.4 |
| 2003 | 13,951 | 4.2 | 5882 | 5.6 | 324 | 5.0 | 3220 | 4.9 | 2674 | 3.9 | 1741 | 2.0 | 110 | 2.8 | |
| 2004 | 14,812 | 4.4 | 6161 | 5.9 | 341 | 5.3 | 3019 | 4.6 | 3072 | 4.5 | 2118 | 2.4 | 101 | 2.5 | |
| 2005 | 18,457 | 5.5 | 7331 | 7.0 | 418 | 6.5 | 4236 | 6.5 | 3511 | 5.1 | 2862 | 3.3 | 99 | 2.5 | |
| 2006 | 20,962 | 6.2 | 7016 | 6.7 | 382 | 5.9 | 5393 | 8.3 | 4066 | 6.0 | 3840 | 4.4 | 265 | 6.6 | |
| 2007 | 23,728 | 7.1 | 6905 | 6.6 | 546 | 8.5 | 5872 | 9.0 | 5113 | 7.5 | 4920 | 5.7 | 372 | 9.3 | |
| 2008 | 31,512 | 9.4 | 10,947 | 10.4 | 684 | 10.6 | 6578 | 10.1 | 6782 | 9.9 | 6146 | 7.1 | 375 | 9.4 | |
| 2009 | 27,590 | 8.2 | 8701 | 8.3 | 609 | 9.4 | 5624 | 8.6 | 6556 | 9.6 | 5698 | 6.6 | 402 | 10.1 | |
| 2010 | 37,769 | 11.2 | 10,485 | 10.0 | 816 | 12.7 | 7720 | 11.8 | 8417 | 12.3 | 9901 | 11.4 | 430 | 10.8 | |
| 2011 | 35,066 | 10.4 | 9286 | 8.8 | 625 | 9.7 | 6979 | 10.7 | 7175 | 10.5 | 10,500 | 12.1 | 501 | 12.5 | |
| 2012 | 47,586 | 14.2 | 13,144 | 12.5 | 719 | 11.1 | 6471 | 9.9 | 8772 | 12.9 | 17,920 | 20.7 | 560 | 14.0 | |
| 2013 | 49,332 | 14.7 | 13,620 | 12.9 | 652 | 10.1 | 6806 | 10.4 | 8792 | 12.9 | 18,781 | 21.7 | 681 | 17.1 | |
| Gender | male | 148,978 | 44.4 | 47,616 | 45.3 | 3039 | 47.1 | 28,439 | 43.6 | 27,595 | 40.5 | 40,551 | 46.8 | 1738 | 43.5 |
| female | 186,781 | 55.6 | 57,610 | 54.7 | 3411 | 52.9 | 36,760 | 56.4 | 40,581 | 59.5 | 46,164 | 53.2 | 2255 | 56.5 | |
| Age | 0–7 | 65,998 | 19.8 | 24,042 | 22.8 | 1199 | 18.6 | 10,495 | 16.1 | 5137 | 7.5 | 24,692 | 28.5 | 433 | 10.8 |
| 8–17 | 27,386 | 8.2 | 10,101 | 9.6 | 670 | 10.4 | 6399 | 9.8 | 4161 | 6.1 | 5820 | 6.7 | 235 | 5.9 | |
| 18–44 | 83,502 | 24.9 | 32,844 | 31.2 | 1432 | 22.2 | 17,797 | 27.3 | 13,314 | 19.5 | 17,333 | 20.0 | 782 | 19.6 | |
| 45–64 | 81,829 | 24.4 | 22,077 | 21.0 | 1526 | 23.7 | 15,207 | 23.3 | 19,151 | 28.1 | 22,463 | 25.9 | 1405 | 35.2 | |
| 65– | 77,044 | 22.9 | 16,162 | 15.4 | 1623 | 25.2 | 15,301 | 23.5 | 26,413 | 38.7 | 16,407 | 18.9 | 1138 | 28.5 | |
| All-Season | Warm Season (May to September) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N (Days) | Mean | SD | Min. | Max. | N (Days) | Mean | SD | Min. | Max. | |
| Daily Mean Temperature (°C) | 4383 | 12.7 | 9.4 | −10.0 | 29.5 | 1836 | 21.8 | 3.5 | 11.4 | 29.5 |
| Daily Maximum Temperature (°C) | 4383 | 17.5 | 9.4 | −6.0 | 34.5 | 1836 | 26.2 | 3.5 | 12.9 | 34.5 |
| Daily Minimum Temperature (°C) | 4383 | 8.3 | 9.9 | −14.3 | 25.9 | 1836 | 18.0 | 4.3 | 4.6 | 25.9 |
| Daily Relative Humidity (%) | 4383 | 67.8 | 12.0 | 30.1 | 92.7 | 1836 | 74.9 | 9.3 | 39.5 | 92.7 |
| Daily Mean Wind Speed | 4383 | 2.0 | 0.7 | 0.7 | 7.2 | 1836 | 1.8 | 0.5 | 0.7 | 7.2 |
| Daily Maximum Ozone (ppm) | 4383 | 0.0 | 0.0 | 0.0 | 0.1 | 1836 | 0.0 | 0.0 | 0.0 | 0.1 |
| Daily Mean PM10 (μg/m3) | 4383 | 55.1 | 32.2 | 11.7 | 653.4 | 1836 | 47.6 | 23.1 | 11.7 | 314.8 |
| RR | 95% CI | lag 1 | lag 2 | lag 3 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| RR | 95% CI | RR | 95% CI | RR | 95% CI | ||||||||
| Total | 1.06 | 1.06 | 1.06 | 1.05 | 1.05 | 1.06 | 1.05 | 1.05 | 1.05 | 1.05 | 1.05 | 1.05 | |
| Region | Region 1 | 1.03 | 1.03 | 1.03 | 1.02 | 1.02 | 1.02 | 1.02 | 1.02 | 1.02 | 1.01 | 1.01 | 1.02 |
| Region 2 | 1.14 | 1.13 | 1.15 | 1.12 | 1.12 | 1.13 | 1.11 | 1.11 | 1.12 | 1.11 | 1.10 | 1.11 | |
| Region 3 | 1.04 | 1.04 | 1.04 | 1.04 | 1.03 | 1.04 | 1.04 | 1.03 | 1.04 | 1.03 | 1.03 | 1.03 | |
| Region 4 | 1.11 | 1.10 | 1.11 | 1.10 | 1.10 | 1.10 | 1.10 | 1.09 | 1.10 | 1.09 | 1.09 | 1.09 | |
| Region 5 | 1.06 | 1.05 | 1.06 | 1.05 | 1.05 | 1.05 | 1.05 | 1.04 | 1.05 | 1.04 | 1.04 | 1.05 | |
| Region 6 | 1.23 | 1.21 | 1.25 | 1.23 | 1.21 | 1.25 | 1.23 | 1.21 | 1.24 | 1.23 | 1.21 | 1.25 | |
| Gender | male | 1.08 | 1.08 | 1.08 | 1.07 | 1.07 | 1.07 | 1.06 | 1.06 | 1.06 | 1.06 | 1.05 | 1.06 |
| female | 1.05 | 1.05 | 1.05 | 1.04 | 1.04 | 1.04 | 1.04 | 1.04 | 1.04 | 1.04 | 1.04 | 1.04 | |
| Age | 0–7 | 1.01 | 1.01 | 1.01 | 0.99 | 0.99 | 1.00 | 0.99 | 0.99 | 0.99 | 0.99 | 0.98 | 0.99 |
| 8–17 | 1.04 | 1.04 | 1.05 | 1.03 | 1.03 | 1.04 | 1.03 | 1.02 | 1.03 | 1.02 | 1.02 | 1.03 | |
| 18–44 | 1.06 | 1.06 | 1.06 | 1.05 | 1.05 | 1.05 | 1.05 | 1.05 | 1.05 | 1.04 | 1.04 | 1.05 | |
| 45–64 | 1.09 | 1.09 | 1.09 | 1.09 | 1.09 | 1.09 | 1.09 | 1.09 | 1.09 | 1.08 | 1.08 | 1.09 | |
| 65– | 1.08 | 1.08 | 1.09 | 1.08 | 1.08 | 1.09 | 1.08 | 1.08 | 1.08 | 1.08 | 1.08 | 1.08 | |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, J.; Song, K.J.; Hong, K.J.; Ro, Y.S. Trend of Outbreak of Thermal Illness Patients Based on Temperature 2002–2013 in Korea. Climate 2017, 5, 94. https://doi.org/10.3390/cli5040094
Kim J, Song KJ, Hong KJ, Ro YS. Trend of Outbreak of Thermal Illness Patients Based on Temperature 2002–2013 in Korea. Climate. 2017; 5(4):94. https://doi.org/10.3390/cli5040094
Chicago/Turabian StyleKim, Jungeun, Kyoung Jun Song, Ki Jeong Hong, and Young Sun Ro. 2017. "Trend of Outbreak of Thermal Illness Patients Based on Temperature 2002–2013 in Korea" Climate 5, no. 4: 94. https://doi.org/10.3390/cli5040094
APA StyleKim, J., Song, K. J., Hong, K. J., & Ro, Y. S. (2017). Trend of Outbreak of Thermal Illness Patients Based on Temperature 2002–2013 in Korea. Climate, 5(4), 94. https://doi.org/10.3390/cli5040094






