Climate-Sensitive Health Outcomes in Kenya: A Scoping Review of Environmental Exposures and Health Outcomes Research, 2000–2024
Abstract
1. Introduction
2. Materials and Methods
2.1. Protocol and Registration
2.2. Eligibility Criteria
2.3. Information Source
- P: Population of Kenya;
- E: Environmental exposures, including weather, hydrometeorological hazards, and air quality variables;
- C: No effect of environmental exposures on health conditions (as available, studies will not be excluded for lack of comparison groups);
- O: Disease burdens or measures of association or effect of environmental exposures on health outcomes.
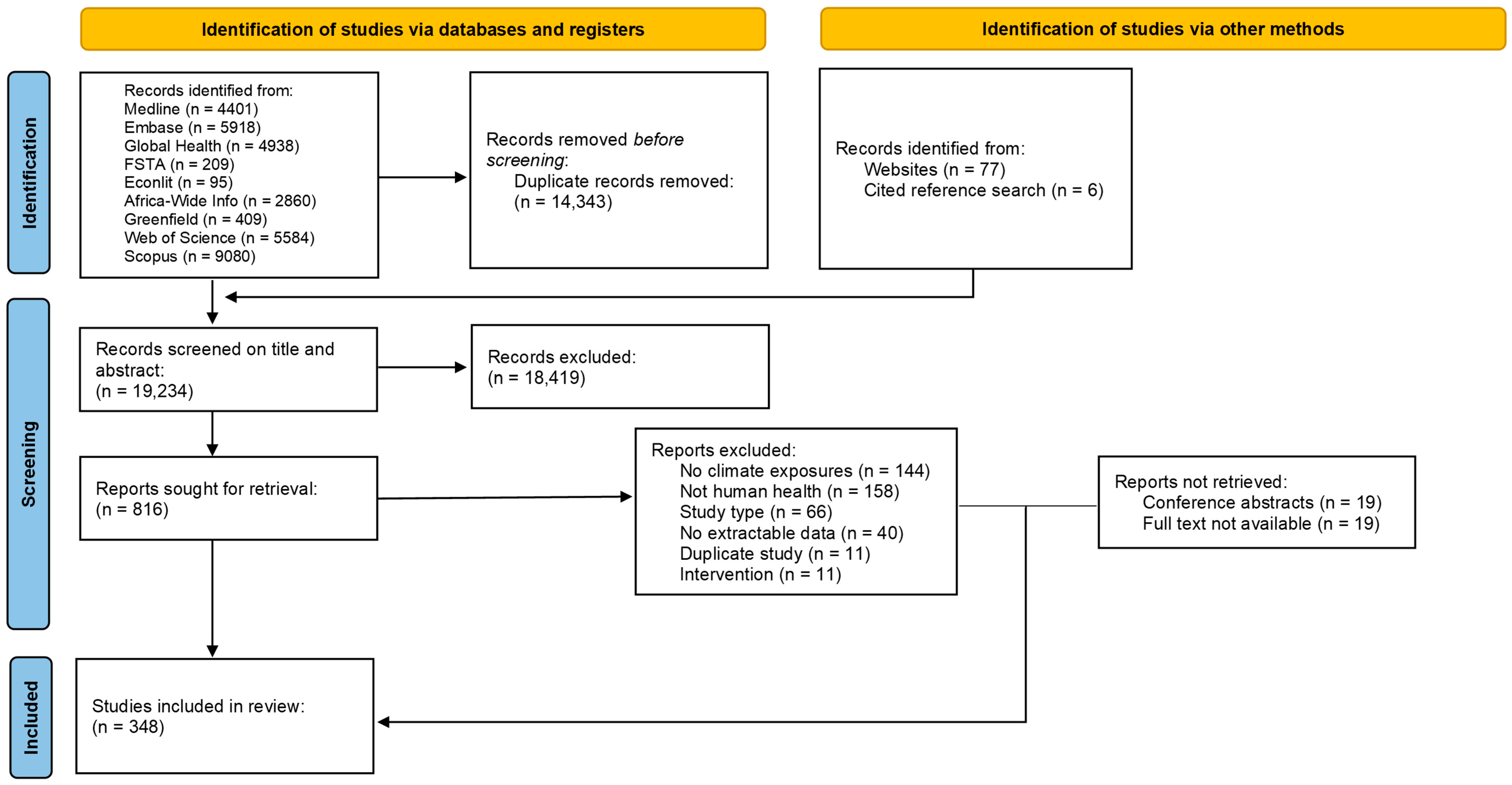
2.4. Selection Process
2.5. Data Extraction
2.6. Evidence Synthesis
2.7. Protocol Amendments
3. Results
3.1. Article Characteristics
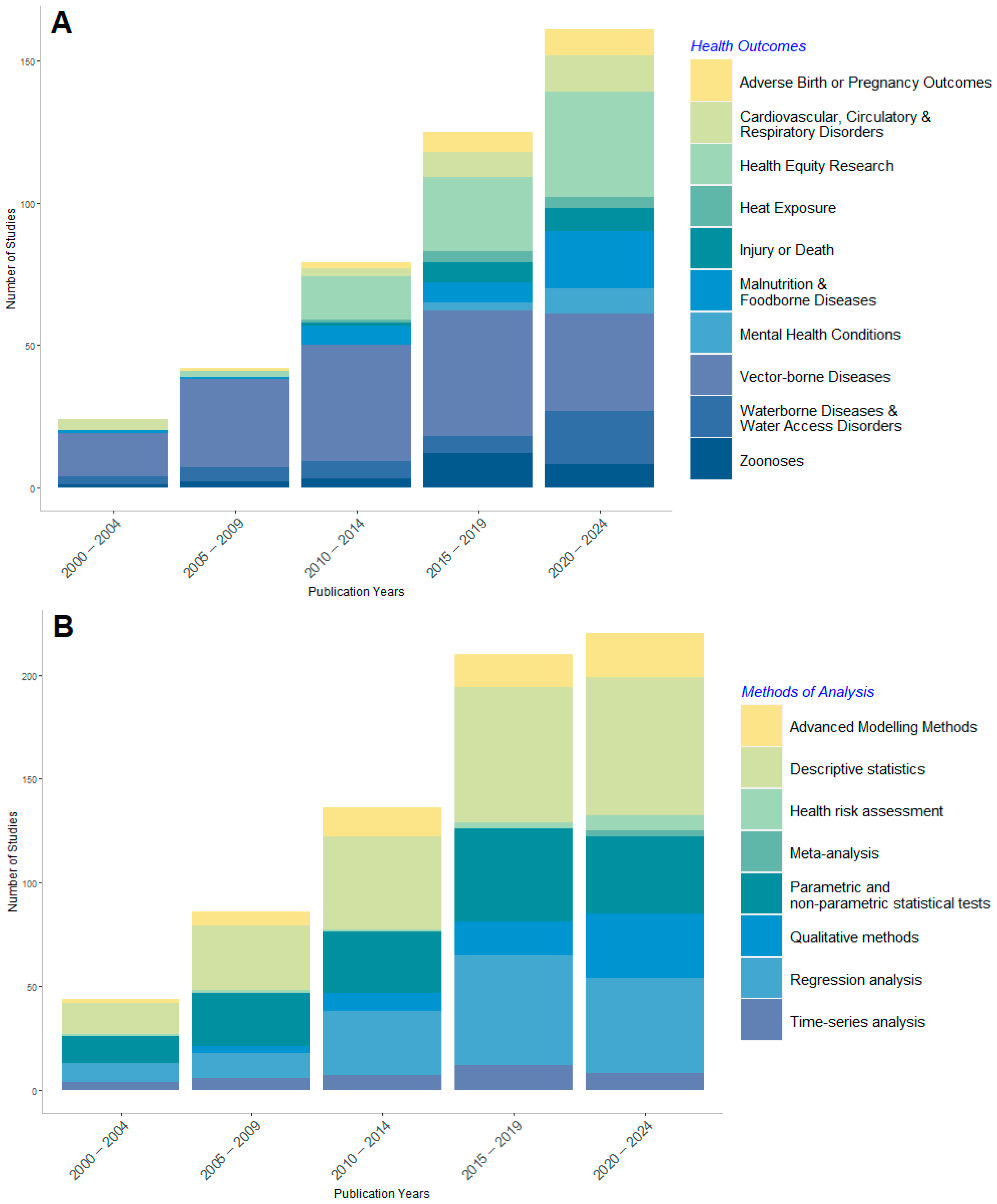
3.2. Key Trends in Health Impacts Assessments
3.3. Environmental Drivers of Health Outcomes in Kenya
3.4. Research Locations in Kenya
3.5. Health Outcome Summaries
3.5.1. Vector-Borne Diseases
3.5.2. Health Equity Research
3.5.3. Waterborne Diseases and Water Access Disorders
3.5.4. Cardiovascular, Circulatory, and Respiratory Disorders
3.5.5. Malnutrition and Foodborne Diseases
3.5.6. Zoonoses
3.5.7. Adverse Birth or Pregnancy Outcomes
3.5.8. Injury or Death
3.5.9. Mental Health Conditions
3.5.10. Heat Exposure and Skin Conditions
4. Discussion
4.1. Research Trends
4.2. Shifting Narratives
4.3. Research Gaps
4.4. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| EE | Environmental exposures |
| HO | Health outcomes |
| CCH | Climate change and health |
| SSA | Sub-Saharan Africa |
Appendix A
| Topic Category | Topic Subcategories |
|---|---|
| Climate Change and Seasonality | Climate change |
| Seasonality | |
| Solar radiation | |
| Ambient Temperature | Excess heat |
| Excess cold | |
| Temperature variation | |
| Rainfall and Humidity | Rainfall |
| Humidity | |
| Wind Characteristics | Wind speed |
| Flooding and Water Characteristics | Flooding |
| Water level change | |
| Water quality parameters | |
| Drought | Drought |
| Air Pollution | Particulate matter |
| NOx, SO2, Ozone | |
| Cooking fuel emissions | |
| Lighting emissions | |
| Second-hand tobacco smoke | |
| Other air pollutants | |
| Terrestrial and Water Pollution | Organic matter contamination |
| Inorganic compound contamination | |
| Microbial contamination | |
| Plastic pollution | |
| Topography | Soil type and moisture |
| Climate-Associated Land Use Change | Deforestation |
| Urban development | |
| Habitat and vegetation change |
| Characteristic | Included literature (n) |
|---|---|
| Health Outcome Categories | 431 |
| Vector-borne Diseases | 165 |
| Health Equity Research | 80 |
| Waterborne Diseases and Water Access Disorders | 39 |
| Cardiovascular, Circulatory, and Respiratory Disorders | 29 |
| Malnutrition and Foodborne Diseases | 36 |
| Zoonoses | 26 |
| Adverse Birth or Pregnancy Outcomes | 19 |
| Injury or Death | 16 |
| Mental Health Conditions | 12 |
| Heat Exposure | 9 |
| Methods of Analysis | 663 |
| Descriptive statistics | 214 |
| Parametric and non-parametric statistical tests | 138 |
| Regression analysis | 145 |
| Advanced modelling methods | 63 |
| Qualitative methods | 55 |
| Time-series analysis | 38 |
| Health risk assessment | 7 |
| Meta-analysis | 3 |
| Funder(s) | 402 |
| International funder(s) | 246 |
| No funding cited | 61 |
| International university funding | 48 |
| Kenya Government | 28 |
| University funding | 11 |
| Private/local funder | 8 |
| Characteristic | Included Literature (n) |
|---|---|
| Year Published | 348 |
| 2000–2004 | 21 |
| 2005–2009 | 39 |
| 2010–2014 | 64 |
| 2015–2019 | 100 |
| 2020–2024 | 124 |
| Institutional Collaborations | 348 |
| Kenyan | 59 |
| African Region | 19 |
| International | 198 |
| International without African collaborations | 72 |
| Study Type | 348 |
| Observational | 183 |
| Modelling Study | 76 |
| Mixed methods | 26 |
| Trials * | 24 |
| Qualitative | 36 |
| Meta-analysis | 3 |
| Geographic Scale | 348 |
| National | 63 |
| Regional | 195 |
| City/community | 78 |
| Not specified/relevant | 12 |
References
- World Meteorological Organization. State of the Climate in Africa 2021. 2022. Available online: https://library.wmo.int/records/item/58070-state-of-the-climate-in-africa-2021 (accessed on 31 October 2023).
- World Bank Group. Climate Risk Profile: Kenya. 2021. Available online: https://climateknowledgeportal.worldbank.org/sites/default/files/2021-05/15724-WB_Kenya%20Country%20Profile-WEB.pdf (accessed on 31 October 2023).
- Wambua, C. The Kenya Climate Change Act 2016 Emerging Lessons from a Pioneer Law. Carbon Clim. Law Rev. 2019, 13, 257–269. [Google Scholar] [CrossRef]
- Government of the Republic of Kenya. National Climate Change Action Plan (Kenya): 2018–2022; Ministry of Environment and Forestry, Ed.; Government of the Republic of Kenya: Nairobi, Kenya, 2018. Available online: https://rise.esmap.org/data/files/library/kenya/Clean%20Cooking/Kenya_NCCAP_2018-2022.pdf (accessed on 31 October 2023).
- Mora, C.; McKenzie, T.; Gaw, I.M.; Dean, J.M.; Von Hammerstein, H.; Knudson, T.A.; Setter, R.O.; Smith, C.Z.; Webster, K.M.; Patz, J.A.; et al. Over half of known human pathogenic diseases can be aggravated by climate change. Nat. Clim. Change 2022, 12, 869–875. [Google Scholar] [CrossRef]
- Sarkis-Onofre, R.; Catalá-López, F.; Aromataris, E.; Lockwood, C. How to properly use the PRISMA Statement. Syst. Rev. 2021, 10, 117. [Google Scholar] [CrossRef] [PubMed]
- Pham, M.T.; Rajić, A.; Greig, J.D.; Sargeant, J.M.; Papadopoulos, A.; McEwen, S.A. A scoping review of scoping reviews: Advancing the approach and enhancing the consistency. Res. Synth. Methods 2014, 5, 371–385. [Google Scholar] [CrossRef]
- Brunn, A.; Ray, S.; Blom, I.; Gerard, J.; Hughes, R.C.; Kibaara, T.; Onyango, B.; Abdullahi, L.; Falconer, J. Climate-Sensitive Health Outcomes in Kenya: A Protocol for a Scoping Review of the Impact of Environmental Exposures on Health Outcomes. 2023. Available online: https://doi.org/10.17605/OSF.IO/FP6SD (accessed on 31 October 2023). [CrossRef]
- Callaghan, M.W.; Minx, J.C.; Forster, P.M. A topography of climate change research. Nat. Clim. Change 2020, 10, 118–123. [Google Scholar] [CrossRef]
- Morgan, R.L.; Whaley, P.; Thayer, K.A.; Schünemann, H.J. Identifying the PECO: A framework for formulating good questions to explore the association of environmental and other exposures with health outcomes. Env. Int. 2018, 121 Pt 1, 1027–1031. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Quality Criteria for Health National Adaptation Plans; World Health Organization: Geneva, Switzerland, 2021; Available online: https://www.who.int/publications/i/item/9789240018983 (accessed on 31 October 2023).
- Falconer, J.; Brunn, A. Search Strategies for A Scoping Review of the Influence of Environmental Exposures on Health Outcomes in Kenya; London School of Hygiene & Tropical Medicine: London, UK, 2023. [Google Scholar] [CrossRef]
- Thomas, J.; Brunton, J.; Graziosi, S. EPPI-Reviewer 4.0: Software for Research Synthesis; EPPI Centre Software; Social Science Research Unit, Institute of Education, University of London: London, UK, 2010. [Google Scholar]
- Kenya Meteorological Department. State of the Climate in Kenya 2020. [Internet]. 2020. Available online: https://www.kenyaclimatedirectory.org/resources/64f21390754b0ke (accessed on 31 October 2023).
- R Core Team. R: A Language and Environment for Statistical Computing, Version 4.3.2; R Foundation for Statistical Computing: Vienna, Austria, 2024; Available online: https://www.R-project.org/ (accessed on 31 May 2024).
- Popay, J.; Roberts, H.; Sowden, A.; Petticrew, M.; Arai, L.; Rodgers, M.; Britten, N.; Roen, K.; Duffy, S. Guidance on the Conduct of Narrative Synthesis in Systematic Reviews: A product from the ESRC Methods Programme; Version 1; Lancaster University: Lancaster, UK, 2006; pp. 1–92. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Dianati, K.; Zimmermann, N.; Milner, J.; Muindi, K.; Ezeh, A.; Chege, M.; Mberu, B.; Kyobutungi, C.; Fletcher, H.; Wilkinson, P.; et al. Household air pollution in Nairobi’s slums: A long-term policy evaluation using participatory system dynamics. Sci. Total Environ. 2019, 660, 1108–1134. [Google Scholar] [CrossRef]
- Egondi, T.; Kyobutungi, C.; Ng, N.; Muindi, K.; Oti, S.; van de Vijver, S.; Ettarh, R.; Rocklöv, J. Community perceptions of air pollution and related health risks in Nairobi slums. Int. J. Environ. Res. Public Health 2013, 10, 4851–4868. [Google Scholar] [CrossRef]
- Muindi, K.; Egondi, T.; Kimani-Murage, E.; Rocklov, J.; Ng, N. “We are used to this”: A qualitative assessment of the perceptions of and attitudes towards air pollution amongst slum residents in Nairobi. BMC Public Health 2014, 14, 226. [Google Scholar] [CrossRef]
- Ngo, N.S.; Kokoyo, S.; Klopp, J. Why participation matters for air quality studies: Risk perceptions, understandings of air pollution and mobilization in a poor neighborhood in Nairobi, Kenya. Public Health 2017, 142, 177–185. [Google Scholar] [CrossRef] [PubMed]
- West, S.E.; Bowyer, C.J.; Apondo, W.; Büker, P.; Cinderby, S.; Gray, C.M.; Hahn, M.; Lambe, F.; Loh, M.; Medcalf, A.; et al. Using a co-created transdisciplinary approach to explore the complexity of air pollution in informal settlements. Humanit. Soc. Sci. Commun. 2021, 8, 285. [Google Scholar] [CrossRef]
- Lusambili, A.; Kovats, S.; Nakstad, B.; Filippi, V.; Khaemba, P.; Roos, N.; Part, C.; Luchters, S.; Chersich, M.; Hess, J.; et al. Too hot to thrive: A qualitative inquiry of community perspectives on the effect of high ambient temperature on postpartum women and neonates in Kilifi, Kenya. BMC Pediatr. 2024, 24, 36. [Google Scholar] [CrossRef]
- Dida, G.O.; Lutta, P.O.; Abuom, P.O.; Mestrovic, T.; Anyona, D.N. Factors predisposing women and children to indoor air pollution in rural villages, Western Kenya. Arch. Public Health 2022, 80, 46. [Google Scholar] [CrossRef]
- Zuurmond, M.; Nyapera, V.; Mwenda, V.; Kisia, J.; Rono, H.; Palmer, J. Childhood disability in Turkana, Kenya: Understanding how carers cope in a complex humanitarian setting. Afr. J. Disabil. 2016, 5, 277. [Google Scholar] [CrossRef] [PubMed]
- Esho, T.; Komba, E.; Richard, F.; Shell-Duncan, B. Intersections between climate change and female genital mutilation among the Maasai of Kajiado County, Kenya. J. Glob. Health 2021, 11, 04033. Available online: https://jogh.org/intersections-between-climate-change-and-female-genital-mutilation-among-the-maasai-of-kajiado-county-kenya/ (accessed on 31 October 2023).
- Allen, E.M.; Munala, L.; Henderson, J.R. Kenyan Women Bearing the Cost of Climate Change. Int. J. Environ. Res. Public Health 2021, 18, 12697. [Google Scholar] [CrossRef]
- Linke, A.M.; O’Loughlin, J.; McCabe, J.T.; Tir, J.; Witmer, F.D.W. Rainfall variability and violence in rural Kenya: Investigating the effects of drought and the role of local institutions with survey data. Glob. Environ. Change 2015, 34, 35–47. [Google Scholar] [CrossRef]
- Linke, A.M.; Witmer, F.D.W.; O’Loughlin, J. Weather variability and conflict forecasts: Dynamic human-environment interactions in Kenya. Political Geogr. 2022, 92, 102489. [Google Scholar] [CrossRef]
- Omosa, E. The Impact of Water Conflicts on Pastoral Livelihoods: The Case of Wajir District in Kenya; International Institute for Sustainable Development: Winnipeg, MB, Canada, 2005; Available online: https://www.iisd.org/publications/report/impact-water-conflicts-pastoral-livelihoods-case-wajir-district-kenya (accessed on 31 October 2023).
- McNally, K.L. Developing Risk Assessment Maps for Schistosoma Haematobium in Kenya Based on Climate Grids and Remotely Sensed Data. Master’s Thesis, Louisiana State University, Baton Rouge, LA, USA, 2003. [Google Scholar]
- McCreesh, N.; Nikulin, G.; Booth, M. Predicting the effects of climate change on Schistosoma mansoni transmission in eastern Africa. Parasites Vectors 2015, 8, 4. [Google Scholar] [CrossRef]
- Kariuki, H.C.; Clennon, J.A.; Brady, M.S.; Kitron, U.; Sturrock, R.F.; Ouma, J.H.; Ndzovu, S.T.M.; Mungai, P.; Hoffman, O.; Hamburger, J.; et al. Distribution patterns and cercarial shedding of Bulinus nasutus and other snails in the Msambweni area, Coast Province, Kenya. Am. J. Trop. Med. Hyg. 2004, 70, 449–456. [Google Scholar] [CrossRef]
- Tabo, Z.; Kalinda, C.; Breuer, L.; Albrecht, C. Exploring the interplay between climate change and schistosomiasis transmission dynamics. Infect. Dis. Model. 2024, 9, 158–176. [Google Scholar] [CrossRef] [PubMed]
- Stoltzfus, J.D.; Carter, J.Y.; Akpinar-Elci, M.; Matu, M.; Kimotho, V.; Giganti, M.J.; Langat, D.; Elci, O.C. Interaction between climatic, environmental, and demographic factors on cholera outbreaks in Kenya. Infect. Dis. Poverty 2014, 3, 37. [Google Scholar] [CrossRef]
- Muchiri, J.M.; Ascolillo, L.; Mugambi, M.; Mutwiri, T.; Ward, H.D.; Naumova, E.N.; Egorov, A.I.; Cohen, S.; Else, J.G.; Griffiths, J.K. Seasonality of Cryptosporidium oocyst detection in surface waters of Meru, Kenya as determined by two isolation methods followed by PCR. J. Water Health 2009, 7, 67–75. [Google Scholar] [CrossRef] [PubMed]
- Gatei, W.; Wamae, C.N.; Mbae, C.; Waruru, A.; Mulinge, E.; Waithera, T.; Gatika, S.M.; Kamwati, S.K.; Revathi, G.; Hart, C.A. Cryptosporidiosis: Prevalence, genotype analysis, and symptoms associated with infections in children in Kenya. Am. J. Trop. Med. Hyg. 2006, 75, 78–82. [Google Scholar] [CrossRef] [PubMed]
- Mutuku, F.M.; King, C.H.; Bustinduy, A.L.; Mungai, P.L.; Muchiri, E.M.; Kitron, U. Impact of drought on the spatial pattern of transmission of Schistosoma haematobium in coastal Kenya. Am. J. Trop. Med. Hyg. 2011, 85, 1065–1070. [Google Scholar] [CrossRef]
- Omore, R.; Tate, J.E.; O’Reilly, C.E.; Ayers, T.; Williamson, J.; Moke, F.; Schilling, K.A.; Awuor, A.O.; Jaron, P.; Ochieng, J.B.; et al. Epidemiology, Seasonality and Factors Associated with Rotavirus Infection among Children with Moderate-to-Severe Diarrhea in Rural Western Kenya, 2008–2012: The Global Enteric Multicenter Study (GEMS). PLoS ONE 2016, 11, e0160060. [Google Scholar] [CrossRef]
- Lambisia, A.W.; Onchaga, S.; Murunga, N.; Lewa, C.S.; Nyanjom, S.G.; Agoti, C.N. Epidemiological Trends of Five Common Diarrhea-Associated Enteric Viruses Pre- and Post-Rotavirus Vaccine Introduction in Coastal Kenya. Pathogens 2020, 9, 660. [Google Scholar] [CrossRef]
- Gikonyo, J.; Mbatia, B.; Okanya, P.; Obiero, G.; Sang, C.; Nyangao, J. Rotavirus prevalence and seasonal distribution post vaccine introduction in Nairobi county Kenya. Pan Afr. Med. J. 2019, 33, 269. [Google Scholar] [CrossRef]
- Dohoo, C.; Guernsey, J.R.; Critchley, K.; VanLeeuwen, J. Pilot study on the impact of biogas as a fuel source on respiratory health of women on rural Kenyan smallholder dairy farms. J. Environ. Public Health 2012, 2012, 636298. [Google Scholar] [CrossRef]
- Sikolia, D.N.; Mwololo, K.; Cherop, H.; Hussein, A.; Juma, M.; Kurui, J.; Bwika, A.; Seki, I.; Osaki, Y. The prevalence of acute respiratory infections and the associated risk factors: A study of children under five years of age in Kibera Lindi Village, Nairobi, Kenya. J. Natl. Inst. Public Health 2002, 51, 67–72. Available online: https://www.niph.go.jp/journal/data/51-1/200251010012.pdf (accessed on 31 October 2023).
- Meme, H.; Amukoye, E.; Bowyer, C.; Chakaya, J.; Das, D.; Dobson, R.; Dragosits, U.; Fuld, J.; Gray, C.; Hahn, M.; et al. Asthma symptoms, spirometry and air pollution exposure in schoolchildren in an informal settlement and an affluent area of Nairobi, Kenya. Thorax 2023, 78, 1118–1125. [Google Scholar] [CrossRef] [PubMed]
- Parvizi, K.; Menya, D.; Nix, E.; Mangeni, J.; Lorenzetti, F.; Sang, E.; de Cuevas, R.A.; Tawiah, T.; Baame, M.; Betang, E.; et al. Burden of headaches, eye irritation and respiratory symptoms among females stacking LPG with polluting cooking fuels: Modelling from peri-urban Cameroon, Ghana & Kenya. Energy Nexus 2024, 14, 100304. [Google Scholar] [CrossRef]
- Agarwal, A.; Kirwa, K.; Eliot, M.N.; Alenezi, F.; Menya, D.; Mitter, S.S.; Velazquez, E.J.; Vedanthan, R.; Wellenius, G.A.; Bloomfield, G.S. Household Air Pollution Is Associated with Altered Cardiac Function among Women in Kenya. Am. J. Respir. Crit. Care Med. 2018, 197, 958–961. [Google Scholar] [CrossRef]
- Critchley, K. Air Quality, Respiratory Health and Wood Use for Women Converting from Low- to High-Efficiency Stoves in Rural Kenya; WIT Press: Southampton, UK, 2015. [Google Scholar] [CrossRef]
- Foote, E.M.; Gieraltowski, L.; Ayers, T.; Sadumah, I.; Faith, S.H.; Silk, B.J.; Were, V.; Quick, R.E.; Hughes, J.M.; Cohen, A.L. Impact of locally-produced, ceramic cookstoves on respiratory disease in children in rural western Kenya. Am. J. Trop. Med. Hyg. 2013, 88, 132–137. [Google Scholar] [CrossRef]
- Larson, P.S.; Espira, L.; Glenn, B.E.; Larson, M.C.; Crowe, C.S.; Jang, S.; O’Neill, M.S. Long-Term PM (2.5) Exposure Is Associated with Symptoms of Acute Respiratory Infections among Children under Five Years of Age in Kenya, 2014. Int. J. Environ. Res. Public Health 2022, 19, 2525. [Google Scholar] [CrossRef] [PubMed]
- Harison, K.; Mark, B.; Imwatis, A. Spatial Variability of Malnutrition and Predictions Based on Climate Change and Other Causal Factors: A Case Study of North Rift ASAL Counties of Kenya. J. Earth Sci. Clim. Change 2017, 8, 416. [Google Scholar] [CrossRef]
- Bauer, J.M.; Mburu, S. Effects of drought on child health in Marsabit District, Northern Kenya. Econ. Human Biol. 2017, 24, 74–79. [Google Scholar] [CrossRef]
- Ongudi, S.; Thiam, D.R. Prenatal health and weather-related shocks under social safety net policy in Kenya. Econ. Res. S. Afr. 2020, 831, 17–21. Available online: https://econrsa.org/wp-content/uploads/2022/06/working_paper_831.pdf (accessed on 31 October 2023).
- Uusitalo, R.J.; Jackson, R.T.; Lunn, T.J.; Korhonen, E.M.; Ogola, J.G.; Webala, P.W.; Sironen, T.A.; Forbes, K.M. Current and future environmental suitability for bats hosting potential zoonotic pathogens in rural Kenya. Ecol. Evol. 2024, 14, e11572. [Google Scholar] [CrossRef]
- Young, H.S.; McCauley, D.J.; Dirzo, R.; Nunn, C.L.; Campana, M.G.; Agwanda, B.; Otarola-Castillo, E.R.; Castillo, E.R.; Pringle, R.M.; Veblen, K.E.; et al. Interacting effects of land use and climate on rodent-borne pathogens in central Kenya. Philos. Trans. R. Soc. B Biol. Sci. 2017, 372, 20160116. [Google Scholar] [CrossRef]
- Anyamba, A.; Chretien, J.P.; Small, J.; Tucker, C.J.; Formenty, P.B.; Richardson, J.H.; Britch, S.C.; Schnabel, D.C.; Erickson, R.L.; Linthicum, K.J. Prediction of a Rift Valley fever outbreak. Proc. Natl. Acad. Sci. USA 2009, 106, 955–959. [Google Scholar] [CrossRef]
- Campbell, L.P.; Reuman, D.C.; Lutomiah, J.; Peterson, A.T.; Linthicum, K.J.; Britch, S.C.; Anyamba, A.; Sang, R.; Iacono, G.L. Predicting Abundances of Aedes mcintoshi, a primary Rift Valley fever virus mosquito vector. PLoS ONE 2019, 14, e0226617. [Google Scholar] [CrossRef] [PubMed]
- Mosomtai, G.; Evander, M.; Sandström, P.; Ahlm, C.; Sang, R.; Hassan, O.A.; Affognon, H.; Landmann, T. Association of ecological factors with Rift Valley fever occurrence and mapping of risk zones in Kenya. Int. J. Infect. Dis. 2016, 46, 49–55. [Google Scholar] [CrossRef] [PubMed]
- McIntyre, K.M.; Setzkorn, C.; Hepworth, P.J.; Morand, S.; Morse, A.P.; Baylis, M. Systematic Assessment of the Climate Sensitivity of Important Human and Domestic Animals Pathogens in Europe. Sci. Rep. 2017, 7, 7134. [Google Scholar] [CrossRef]
- Bakhtsiyarava, M.; Grace, K.; Nawrotzki, R.J. Climate, Birth Weight, and Agricultural Livelihoods in Kenya and Mali. Am. J. Public Health 2018, 108 (Suppl. S2), S144–S150. [Google Scholar] [CrossRef] [PubMed]
- Owor, B.E.; Masankwa, G.N.; Mwango, L.C.; Njeru, R.W.; Agoti, C.N.; Nokes, D.J. Human metapneumovirus epidemiological and evolutionary patterns in Coastal Kenya, 2007–2011. BMC Infect. Dis. 2016, 16, 301. [Google Scholar] [CrossRef]
- Wambua, J.; Munywoki, P.K.; Coletti, P.; Nyawanda, B.O.; Murunga, N.; Nokes, D.J.; Hens, N.; Giorgi, E. Drivers of respiratory syncytial virus seasonal epidemics in children under 5 years in Kilifi, coastal Kenya. PLoS ONE 2022, 17, e0278066. [Google Scholar] [CrossRef]
- Sewe, M.O.; Bunker, A.; Ingole, V.; Egondi, T.; Astrom, D.O.; Hondula, D.M.; Rocklöv, J.; Schumann, B. Estimated Effect of Temperature on Years of Life Lost: A Retrospective Time-Series Study of Low-, Middle-, and High-Income Regions. Environ. Health Perspect. 2018, 126, 17004. [Google Scholar] [CrossRef]
- Egondi, T.; Kyobutungi, C.; Rocklöv, J. Temperature variation and heat wave and cold spell impacts on years of life lost among the urban poor population of Nairobi, Kenya. Int. J. Environ. Res. Public Health 2015, 12, 2735–2748. [Google Scholar] [CrossRef]
- Bherwani, H.; Kumar, S.; Musugu, K.; Nair, M.; Gautam, S.; Gupta, A.; Ho, C.-H.; Anshul, A.; Kumar, R. Assessment and valuation of health impacts of fine particulate matter during COVID-19 lockdown: A comprehensive study of tropical and sub tropical countries. Environ. Sci. Pollut. Res. Int. 2021, 28, 44522–445237. [Google Scholar] [CrossRef] [PubMed]
- Mukeka, J.M.; Ogutu, J.O.; Kanga, E.; Piepho, H.-P.; Røskaft, E. Long-term trends in elephant mortality and their causes in Kenya. Front. Conserv. Sci. 2022, 3, 975682. [Google Scholar] [CrossRef]
- Egondi, T.; Ettarh, R.; Kyobutungi, C.; Ng, N.; Rocklöv, J. Exposure to Outdoor Particles (PM2.5) and Associated Child Morbidity and Mortality in Socially Deprived Neighborhoods of Nairobi, Kenya. Atmosphere 2018, 9, 351. [Google Scholar] [CrossRef]
- Lee, K.K.; Bing, R.; Kiang, J.; Bashir, S.; Spath, N.; Stelzle, D.; Mortimer, K.; Bularga, A.; Doudesis, D.; Joshi, S.S.; et al. Adverse health effects associated with household air pollution: A systematic review, meta-analysis, and burden estimation study. Lancet Glob. Health 2020, 8, e1427–e1434. [Google Scholar] [CrossRef]
- Dianati, K.; Schäfer, L.; Milner, J.; Gómez-Sanabria, A.; Gitau, H.; Hale, J.; Langmaack, H.; Kiesewetter, G.; Muindi, K.; Mberu, B.; et al. A system dynamics-based scenario analysis of residential solid waste management in Kisumu, Kenya. Sci. Total Environ. 2021, 777, 146–200. [Google Scholar] [CrossRef]
- Owili, P.O.; Muga, M.A.; Pan, W.C.; Kuo, H.W. Cooking fuel and risk of under-five mortality in 23 Sub-Saharan African countries: A population-based study. Int. J. Environ. Health Res. 2017, 27, 191–204. [Google Scholar] [CrossRef] [PubMed]
- Jiao, X.; Walelign, S.Z.; Nielsen, M.R.; Smith-Hall, C. Protected areas, household environmental incomes and well-being in the Greater Serengeti-Mara Ecosystem. For. Policy Econ. 2019, 106, 101948. [Google Scholar] [CrossRef]
- Mwenda, P.K.; Olago, D.; Okatcha, F.; Ali, A.A. Vulnerability of Communities to Climate Change Induced Disaster Risks and Potential Mental Health Outcomes in Isiolo County, Kenya. J. Phys. Sci. 2022, 3, 37–66. [Google Scholar] [CrossRef]
- Neale, C.; Boukhechba, M.; Cinderby, S. Understanding psychophysiological responses to walking in urban settings in Asia and Africa. J. Environ. Psychol. 2023, 86, 101973. [Google Scholar] [CrossRef]
- Straight, B.; Hilton, C.E.; Naugle, A.; Olungah, C.O.; Ngo, D.; Qiao, X.; Needham, B.L. Drought, psychosocial stress, and ecogeographical patterning: Tibial growth and body shape in Samburu (Kenyan) pastoralist children. Am. J. Biol. Anthropol. 2022, 178, 574–592. [Google Scholar] [CrossRef]
- Egondi, T.; Kyobutungi, C.; Kovats, S.; Muindi, K.; Ettarh, R.; Rocklöv, J. Time-series analysis of weather and mortality patterns in Nairobi’s informal settlements. Glob. Health Action 2012, 5, 23–32. [Google Scholar] [CrossRef] [PubMed]
- Scott, A.A.; Misiani, H.; Okoth, J.; Jordan, A.; Gohlke, J.; Ouma, G.; Arrighi, J.; Zaitchik, B.F.; Jjemba, E.; Verjee, S.; et al. Temperature and heat in informal settlements in Nairobi. PLoS ONE 2017, 12, e0187300. [Google Scholar] [CrossRef]
- Asefi-Najafabady, S.; Vandecar, K.L.; Seimon, A.; Lawrence, P.; Lawrence, D. Climate change, population, and poverty: Vulnerability and exposure to heat stress in countries bordering the Great Lakes of Africa. Clim. Change 2018, 148, 561–573. [Google Scholar] [CrossRef]
- Bethancourt, H.J.; Swanson, Z.S.; Nzunza, R.; Huanca, T.; Conde, E.; Kenney, W.L.; Young, S.L.; Ndiema, E.; Braun, D.; Pontzer, H.; et al. Hydration in relation to water insecurity, heat index, and lactation status in two small-scale populations in hot-humid and hot-arid environments. Am. J. Human Biol. 2021, 33, e23447. [Google Scholar] [CrossRef] [PubMed]
- Deribe, K.; Sultani, H.M.; Okoyo, C.; Omondi, W.P.; Ngere, I.; Newport, M.J.; Cano, J. Geostatistical modelling of the distribution, risk and burden of podoconiosis in Kenya. Trans. R. Soc. Trop. Med. Hyg. 2023, 117, 72–82. [Google Scholar] [CrossRef]
- United States Agency for International Development. Climate Risk in Kenya: Country Risk Profile. 2018. Report Unavailable online.
- UK Meteorological Office. Climate: Observations, Projections and Impacts: Kenya. 2011. Available online: https://www.metoffice.gov.uk/binaries/content/assets/metofficegovuk/pdf/research/climate-science/climate-observations-projections-and-impacts/kenya.pdf (accessed on 31 October 2023).
- Kulkarni, M.A.; Duguay, C.; Ost, K. Charting the evidence for climate change impacts on the global spread of malaria and dengue and adaptive responses: A scoping review of reviews. Glob. Health 2022, 18, 1. [Google Scholar] [CrossRef] [PubMed]
- The Lancet Global Health. Climate change and NTDs: A perfect storm. Lancet Glob. Health 2025, 13, e172. [Google Scholar] [CrossRef]
- Allotey, P.; Reidpath, D.D.; Pokhrel, S. Social sciences research in neglected tropical diseases 1: The ongoing neglect in the neglected tropical diseases. Health Res. Policy Syst. 2010, 8, 32. [Google Scholar] [CrossRef]
- Charani, E.; Abimbola, S.; Pai, M.; Adeyi, O.; Mendelson, M.; Laxminarayan, R.; Rasheed, M.A. Funders: The missing link in equitable global health research? PLoS Glob. Public Health 2022, 2, e0000583. [Google Scholar] [CrossRef]
- Beran, D.; Byass, P.; Gbakima, A.; Kahn, K.; Sankoh, O.; Tollman, S.; Witham, M.; Davies, J. Research capacity building-obligations for global health partners. Lancet Glob. Health 2017, 5, e567–e568. [Google Scholar] [CrossRef]
- International Development Research Centre (IDRC). Eastern and Southern African Regional Hub for Research and Policy on Climate Change and Health. 2024. Available online: https://idrc-crdi.ca/en/project/eastern-and-southern-african-regional-hub-research-and-policy-climate-change-and-health (accessed on 31 May 2024).
- O’Neill, M.S.; McMichael, A.J.; Schwartz, J.; Wartenberg, D. Poverty, environment, and health: The role of environmental epidemiology and environmental epidemiologists. Epidemiology 2007, 18, 664–668. [Google Scholar] [CrossRef] [PubMed]
- Currie, D.J.; Smith, C.; Jagals, P. The application of system dynamics modelling to environmental health decision-making and policy—A scoping review. BMC Public Health 2018, 18, 402. [Google Scholar] [CrossRef] [PubMed]
- Hwong, A.R.; Wang, M.; Khan, H.; Chagwedera, D.N.; Grzenda, A.; Doty, B.; Benton, T.; Alpert, J.; Clarke, D.; Compton, W.M. Climate change and mental health research methods, gaps, and priorities: A scoping review. Lancet Planet. Health 2022, 6, e281–e291. [Google Scholar] [CrossRef] [PubMed]
- Government of the Republic of Kenya. Kenya National Adaptation Plan 2015–2030: Enhanced Climate Resilience Towards the Attainment of Vision 2030 and Beyond; Ministry of Environment and Natural Resources, Ed.; Government of the Republic of Kenya: Nairobi, Kenya, 2016. Available online: https://www4.unfccc.int/sites/NAPC/Documents%20NAP/Kenya_NAP_Final.pdf (accessed on 31 October 2023).
- Burrows, K.; Denckla, C.A.; Hahn, J.; Schiff, J.E.; Okuzono, S.S.; Randriamady, H.; Mita, C.; Kubzansky, L.D.; Koenen, K.C.; Lowe, S.R. A systematic review of the effects of chronic, slow-onset climate change on mental health. Nat. Ment. Health 2024, 2, 228–243. [Google Scholar] [CrossRef]
- Thompson, R.; Lawrance, E.L.; Roberts, L.F.; Grailey, K.; Ashrafian, H.; Maheswaran, H.; Toledano, M.B.; Darzi, A. Ambient temperature and mental health: A systematic review and meta-analysis. Lancet Planet. Health 2023, 7, e580–e589. [Google Scholar] [CrossRef]
- Bonell, A.; Sonko, B.; Badjie, J.; Samateh, T.; Saidy, T.; Sosseh, F.; Sallah, Y.; Bajo, K.; Murray, K.A.; Hirst, J.; et al. Environmental heat stress on maternal physiology and fetal blood flow in pregnant subsistence farmers in The Gambia, west Africa: An observational cohort study. Lancet Planet. Health 2022, 6, e968–e976. [Google Scholar] [CrossRef]
- McElroy, S.; Ilango, S.; Dimitrova, A.; Gershunov, A.; Benmarhnia, T. Extreme heat, preterm birth, and stillbirth: A global analysis across 14 lower-middle income countries. Environ. Int. 2022, 158, 106902. [Google Scholar] [CrossRef]
- Imbo, A.E.; Mbuthia, E.K.; Ngotho, D.N. Determinants of Neonatal Mortality in Kenya: Evidence from the Kenya Demographic and Health Survey 2014. Int. J. Matern. Child Health Aids 2021, 10, 287–295. [Google Scholar] [CrossRef]
- United Nations Population Fund. Demographic Dividend: Kenya; The United Nations: New York, NY, USA, 2023; Available online: https://www.unfpa.org/data/demographic-dividend/KE (accessed on 31 May 2024).
- World Health Organization. Climate Change and Health Research: Current Trends, Gaps and Perspectives for the Future; World Health Organization (WHO): Geneva, Switzerland, 2021; Available online: https://www.who.int/publications/m/item/climate-change-and-health-research-current-trends-gaps-and-perspectives-for-the-future (accessed on 31 October 2023).
- Pearse, R. Gender and climate change. WIREs Clim. Change 2017, 8, e451. [Google Scholar] [CrossRef]
- Fraser-Baxter, S.E. Without Climate Change, the Horn of Africa Drought Wouldn’t Have Happened [Internet]. 2023. Available online: https://www.imperial.ac.uk/news/244671/without-climate-change-horn-africa-drought/ (accessed on 31 May 2024).
- O’Hare, R. Somalia Drought May Have Caused More Than 20,000 Child Deaths. 2023. Available online: https://www.imperial.ac.uk/news/243879/somalia-drought-have-caused-more-than/ (accessed on 31 May 2024).
- Institute Health Metrics Evaluation. Health Research by Location—Kenya. 2023. Available online: https://www.healthdata.org/research-analysis/health-by-location/profiles/kenya (accessed on 31 May 2024).
- Schilling, J.; Werland, L. Facing old and new risks in arid environments: The case of pastoral communities in Northern Kenya. PLoS Clim. 2023, 2, e0000251. [Google Scholar] [CrossRef]
- Haider, H. Conflict Analysis of North Eastern Kenya; Institute of Development Studies: Brighton, UK, 2020; Available online: https://opendocs.ids.ac.uk/opendocs/handle/20.500.12413/15570 (accessed on 31 May 2024).
- Ebi, K.L.; Åström, C.; Boyer, C.J.; Harrington, L.J.; Hess, J.J.; Honda, Y.; Kazura, E.; Stuart-Smith, R.F.; Otto, F.E.L. Using Detection And Attribution To Quantify How Climate Change Is Affecting Health. Health Aff. 2020, 39, 2168–2174. [Google Scholar] [CrossRef] [PubMed]

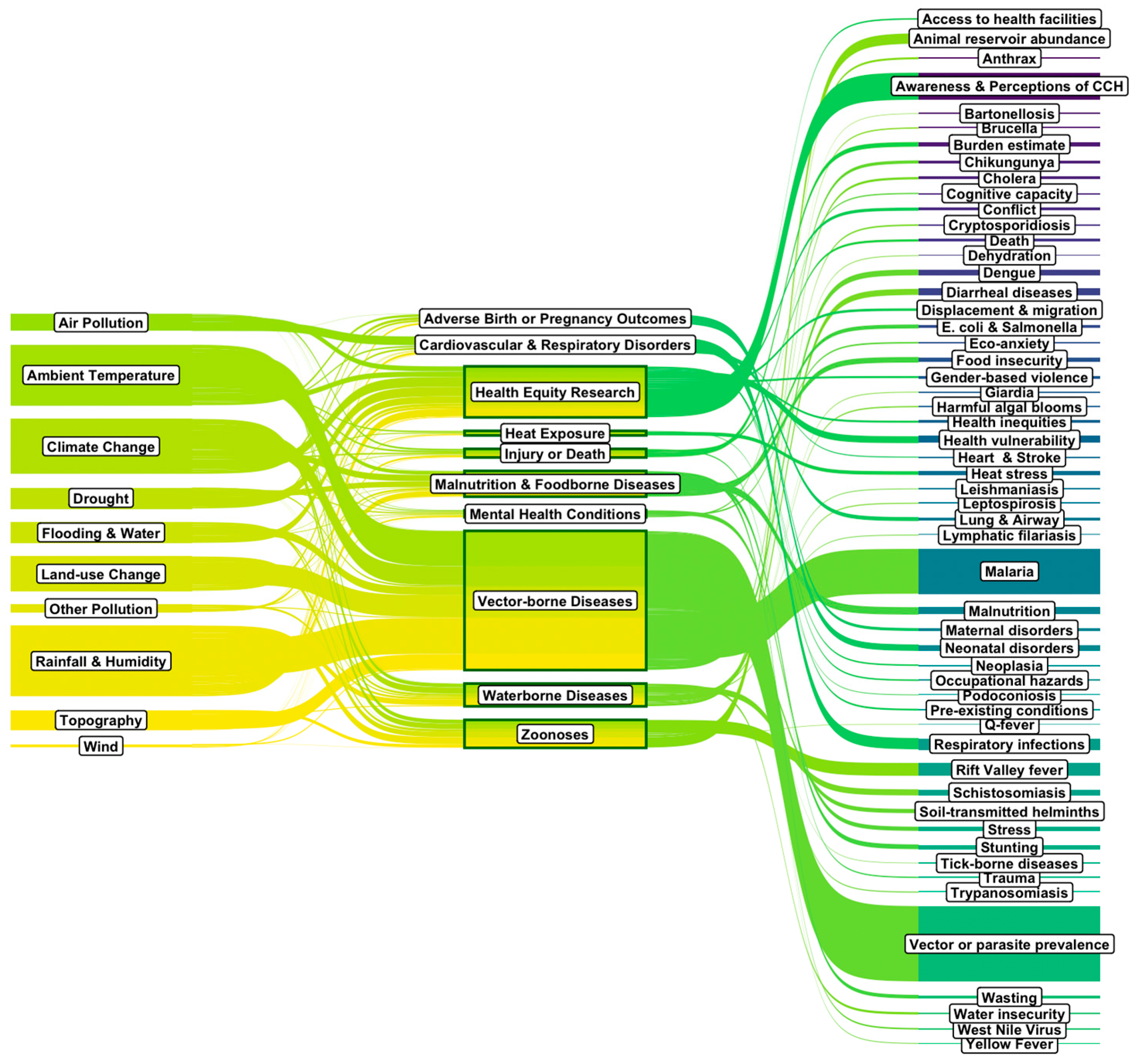

| Topic Category | Topic Subcategories | |
|---|---|---|
| Injury or Death | Trauma Death | Burden estimate |
| Heat Exposure and Skin Conditions | Heat stress | |
| Skin conditions | ||
| Cardiovascular, Circulatory, and Respiratory Disorders | Heart disease and circulatory disorders Lung and airway conditions | Respiratory infections |
| Waterborne Diseases and Water Access Disorders | Cholera Diarrheal diseases Leptospirosis Cryptosporidiosis Schistosomiasis | Giardia Dehydration and kidney disorders Water insecurity Harmful algal blooms |
| Vector-borne Diseases | Vector or parasite abundance or prevalence Malaria Dengue Trypanosomiasis Lymphatic filariasis Leishmaniasis | Tick-borne diseases Soil-transmitted helminths Yellow Fever Chikungunya West Nile Virus |
| Zoonoses | Animal reservoir abundance or zoonotic disease prevalence Anthrax Coxiella burnetti | Bartonellosis Rift Valley fever Brucellosis |
| Malnutrition and Foodborne Diseases | Stunting Wasting Malnutrition | Food insecurity Escherichia coli and Salmonella |
| Mental Health Conditions | Eco-anxiety and depression Stress and resilience | Cognitive capacity |
| Adverse Birth or Pregnancy Outcomes | Neonatal or infant outcomes | |
| Maternal health outcomes | ||
| Health Equity Research | Neoplasia Pre-existing conditions Displacement and migration Occupational hazards | Health vulnerability Awareness and Perceptions Conflict Gender-based violence Access to health facilities Health inequities |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gerard, J.; Kibaara, T.; Blom, I.M.; Falconer, J.; Mohammed, S.; Kadri-Alabi, Z.; Taylor, R.; Abdullahi, L.; Hughes, R.C.; Onyango, B.; et al. Climate-Sensitive Health Outcomes in Kenya: A Scoping Review of Environmental Exposures and Health Outcomes Research, 2000–2024. Climate 2025, 13, 133. https://doi.org/10.3390/cli13070133
Gerard J, Kibaara T, Blom IM, Falconer J, Mohammed S, Kadri-Alabi Z, Taylor R, Abdullahi L, Hughes RC, Onyango B, et al. Climate-Sensitive Health Outcomes in Kenya: A Scoping Review of Environmental Exposures and Health Outcomes Research, 2000–2024. Climate. 2025; 13(7):133. https://doi.org/10.3390/cli13070133
Chicago/Turabian StyleGerard, Jessica, Titus Kibaara, Iris Martine Blom, Jane Falconer, Shamsudeen Mohammed, Zaharat Kadri-Alabi, Roz Taylor, Leila Abdullahi, Robert C. Hughes, Bernard Onyango, and et al. 2025. "Climate-Sensitive Health Outcomes in Kenya: A Scoping Review of Environmental Exposures and Health Outcomes Research, 2000–2024" Climate 13, no. 7: 133. https://doi.org/10.3390/cli13070133
APA StyleGerard, J., Kibaara, T., Blom, I. M., Falconer, J., Mohammed, S., Kadri-Alabi, Z., Taylor, R., Abdullahi, L., Hughes, R. C., Onyango, B., & Brunn, A. A. (2025). Climate-Sensitive Health Outcomes in Kenya: A Scoping Review of Environmental Exposures and Health Outcomes Research, 2000–2024. Climate, 13(7), 133. https://doi.org/10.3390/cli13070133






