Exploring Robotic Technologies for Upper Limb Rehabilitation: Current Status and Future Directions
Abstract
1. Introduction
- Expand market awareness beyond niche perception;
- Remove entry barriers for industry participants;
- Establish dedicated funding mechanisms;
- Focus on underserved populations;
- Implement universal access strategies;
- Ensure user-centered design processes.
- Exoskeleton: A wearable mechanical structure that aligns with the anatomical joints of the wearer, providing direct actuation of specific joints.
- Exosuit: A soft or partially soft wearable system that applies forces through flexible materials (fabrics, cables, elastomers) without rigid joint alignment.
- End-effector: A robotic system where the user interacts with the device only at the distal segment (e.g., hand or forearm), without joint-by-joint alignment.
2. Background
Upper Limb Rehabilitation Robots
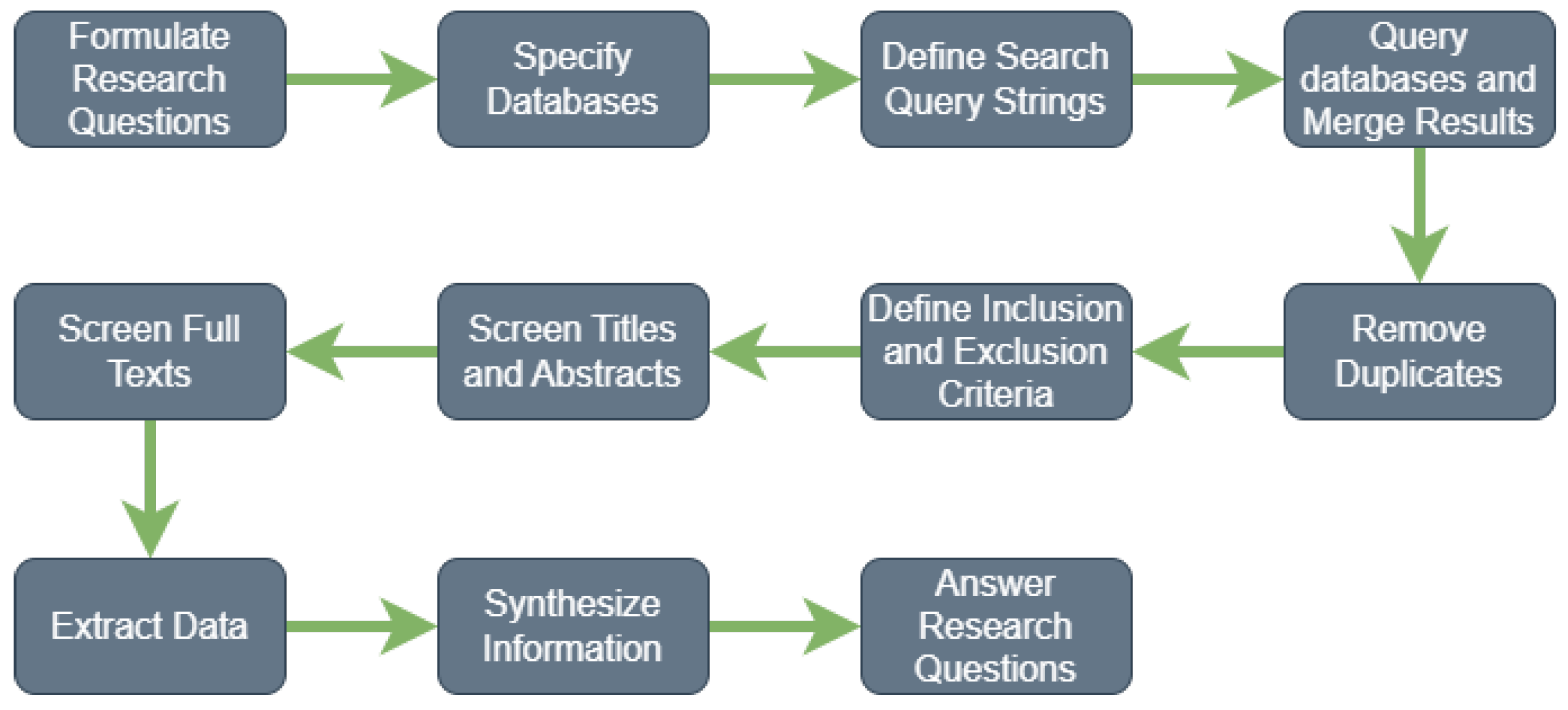
3. Method
- RQ1: What technologies have been used for upper extremity rehabilitation in robotics, especially regarding myoelectric sensors, neural network-based control, and exoskeletons?
- RQ2: What are the most common approaches in control algorithms used for exoskeleton control in rehabilitation?
- RQ3: What specific applications of rehabilitation robotics for the upper extremity have been evaluated, and how do they vary in terms of effectiveness and ease of use?
- RQ4: What research gaps exist in the field of upper extremity rehabilitation robotics that have not yet been addressed?
4. Discussion
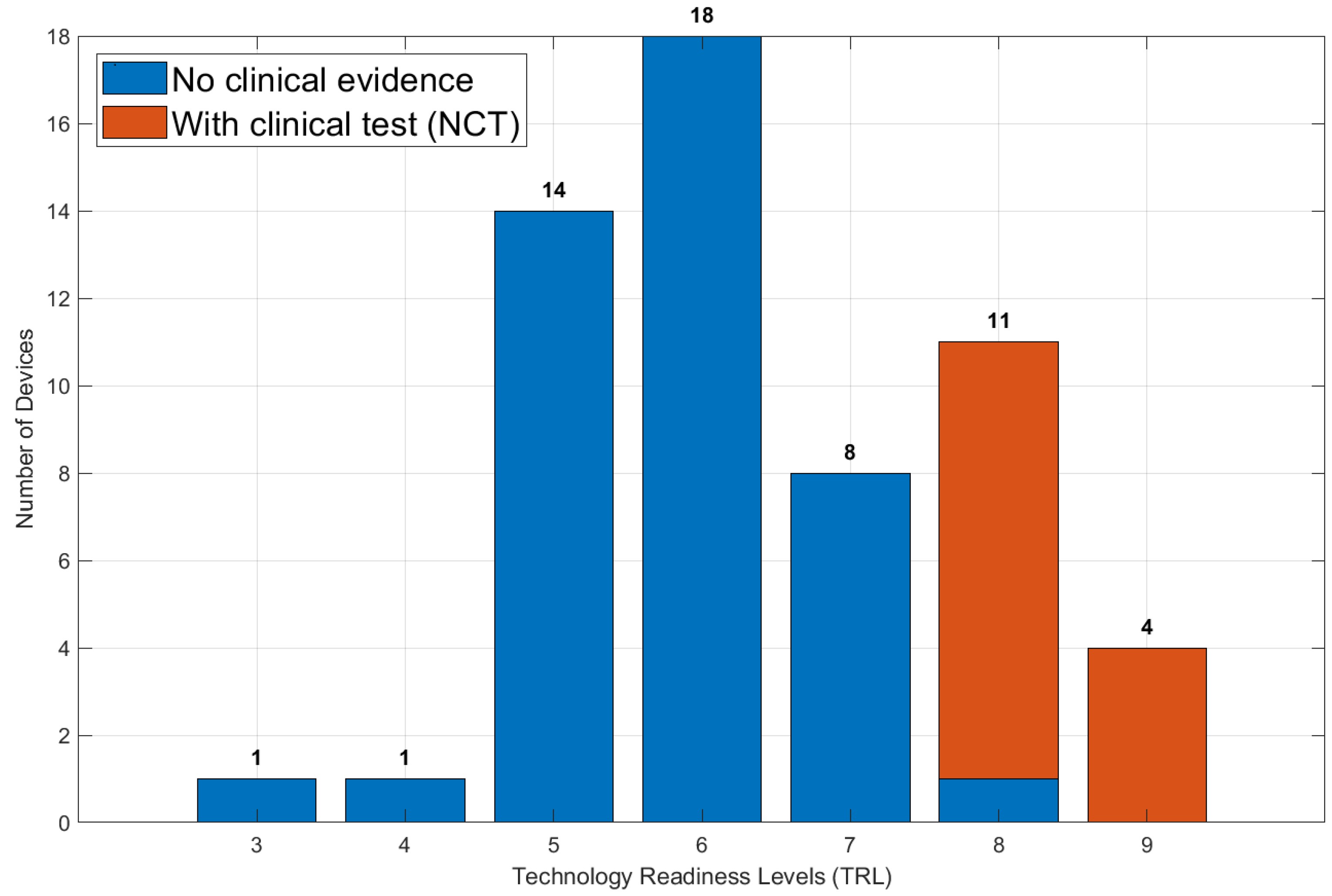
- TRL 1–3 (research phase): Conceptual studies, laboratory testing without human subjects;
- TRL 4–6 (Development phase): Testing with healthy subjects (TRL 4: n < 10, TRL 5: n ≥ 10), preliminary patient studies (TRL 6: n ≥ 5);
- TRL 7–8 (Clinical validation): Registered clinical trials (TRL 7: single-center trials, TRL 8: multi-center trials with n ≥ 20);
- TRL 9 (Commercial deployment): Regulatory approval obtained, commercial availability with post-market surveillance.
- Clinical validation: Registration in clinical trial databases (e.g., NCT number), patient sample size, published clinical outcomes;
- Technical validation: Peer-reviewed publications on performance metrics, mechanical specifications, control system validation;
- Development status: Current stage (prototype, pre-commercial, commercial product).
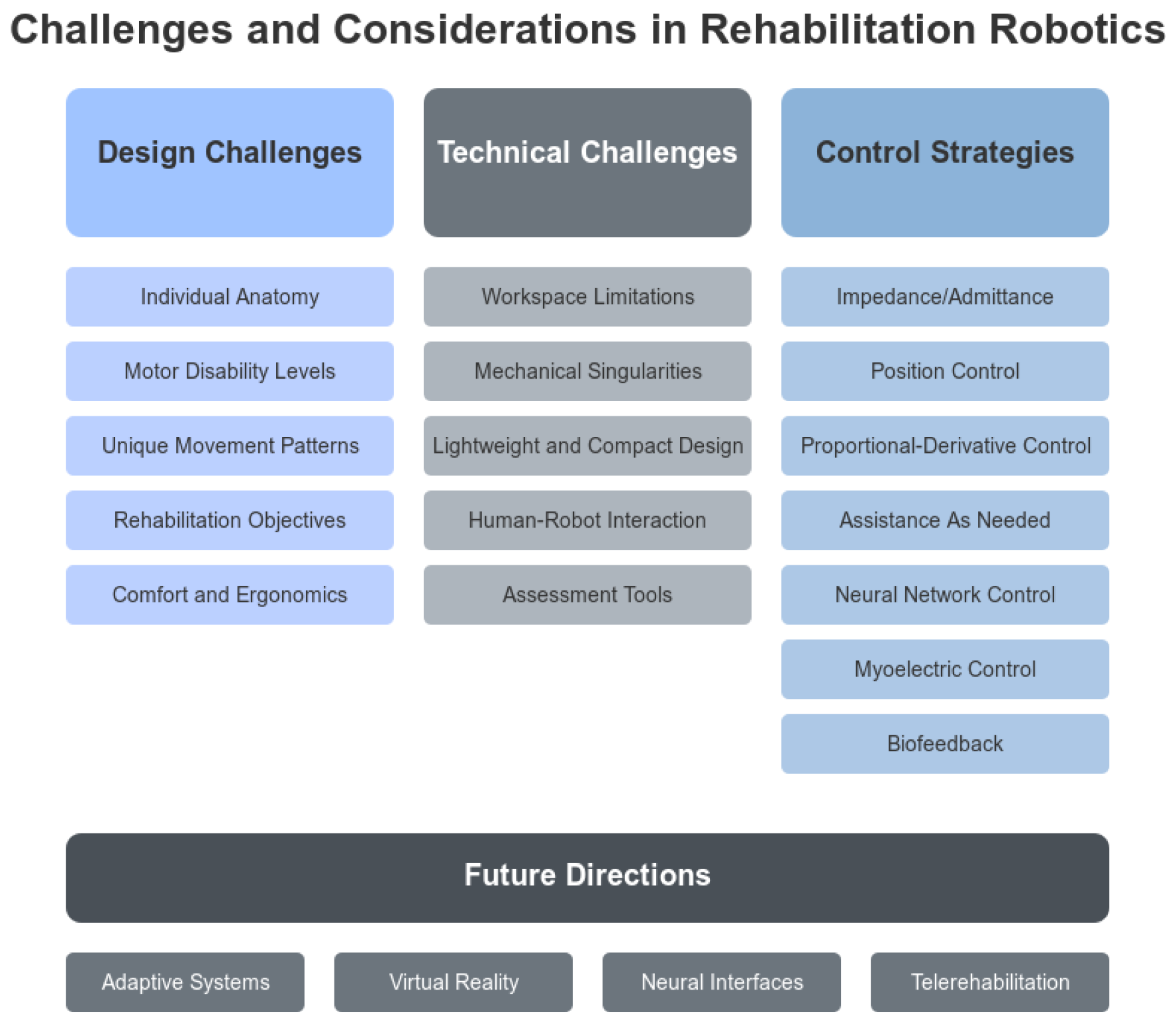
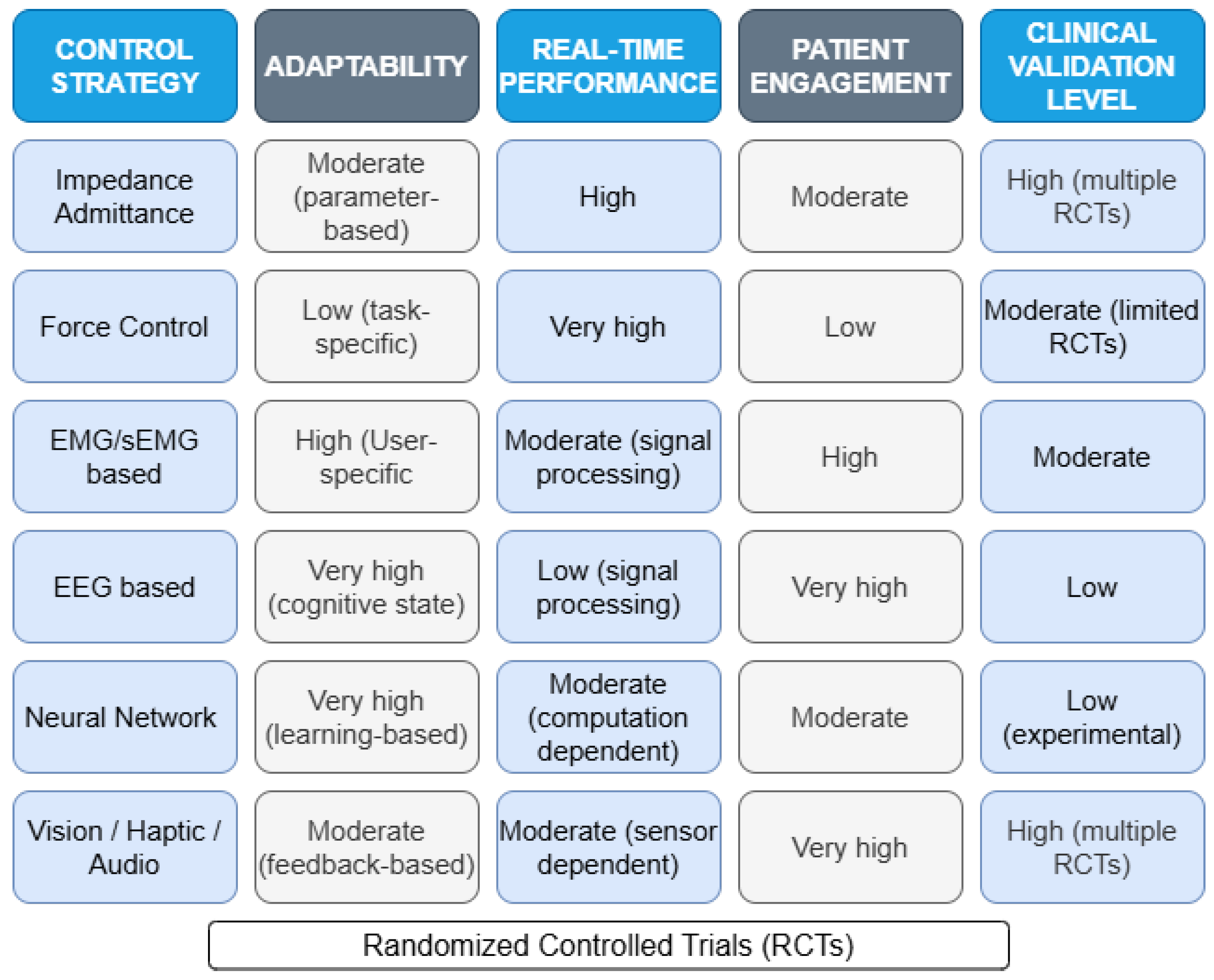
- Impedance/Admittance Control: Enables the exoskeleton to behave as a “virtual” mechanical system with desired stiffness or compliance characteristics, facilitating more natural interaction between the robot and the user. While offering excellent stability and safety for patient interaction, these methods face challenges in personalizing assistance levels without explicit models of patient capability. Advanced implementations now incorporate adaptive parameters that evolve based on performance metrics (completion time, movement smoothness).
- Position Control: Primarily used in the early stages of rehabilitation, where the patient requires full assistance in movement.
- Proportional–Derivative (PD) Control: Provides precise movement control, suitable for specific tasks requiring high precision.
- Assist-as-Needed Strategy: Adjusts the level of assistance based on the patient’s performance, encouraging active participation.
- Neural Network Control: Models the complex dynamics of human–robot interactions and adapts in real-time to the user’s movements.
- Myoelectric Control: Uses electromyography (EMG) signals to infer intended movements, promoting a high level of user engagement. These systems provide intuitive control but suffer from signal variability due to electrode placement, muscle fatigue, and cross-talk between muscle groups. Recent advances employ deep learning techniques to improve signal classification accuracy.
- Biofeedback Control: Provides feedback to the user through sensory channels, such as visual, haptic, or auditory, enhancing motivation and learning. Although offering the advantage of direct brain–computer interfaces, these systems face significant challenges in signal reliability and classification accuracy.
- Force Control: Applies force directly to the limb, enabling strength training and precise control of interaction.
- Hybrid Systems: Combine various control strategies, such as position control and myoelectric control, to maximize therapeutic effectiveness.
- Patient-Cooperative Control: Modulates the robot’s behavior in response to patient-initiated movements, promoting active participation and motor learning.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ibrahim, H.A.; Ammar, H.H.; Shalaby, R. A review of upper limb robot-assisted therapy techniques and virtual reality applications. IAES Int. J. Artif. Intell. 2022, 11, 613–623. [Google Scholar] [CrossRef]
- Saadatzi, M.; Long, D.C.; Celik, O. Comparison of Human-Robot Interaction Torque Estimation Methods in a Wrist Rehabilitation Exoskeleton. J. Intell. Robot. Syst. Theory Appl. 2019, 94, 565–581. [Google Scholar] [CrossRef]
- Hatem, S.M.; Saussez, G.; Faille, M.D.; Prist, V.; Zhang, X.; Dispa, D.; Bleyenheuft, Y. Rehabilitation of motor function after stroke: A multiple systematic review focused on techniques to stimulate upper extremity recovery. Front. Hum. Neurosci. 2016, 10, 442. [Google Scholar] [CrossRef] [PubMed]
- Mao, Z.; Kobayashi, R.; Nabae, H.; Suzumori, K. Multimodal Strain Sensing System for Shape Recognition of Tensegrity Structures by Combining Traditional Regression and Deep Learning Approaches. IEEE Robot. Autom. Lett. 2024, 9, 10050–10056. [Google Scholar] [CrossRef]
- Islam, M.R.; Spiewak, C.; Rahman, M.H.; Fareh, R. A Brief Review on Robotic Exoskeletons for Upper Extremity Rehabilitation to Find the Gap between Research Prototype and Commercial Type. Adv. Robot. Autom. 2017, 6, 1000177. [Google Scholar] [CrossRef]
- Pehlivan, A.U.; Losey, D.P.; Omalley, M.K. Minimal Assist-as-Needed Controller for Upper Limb Robotic Rehabilitation. IEEE Trans. Robot. 2016, 32, 113–124. [Google Scholar] [CrossRef]
- Maciejasz, P.; Jörg, E.; Gerlach-Hahn, K.; Jansen-Troy, A.; Leonhardt, S. A survey on robotic devices for upper limb rehabilitation. J. Neuroeng. Rehabil. 2014, 74, 841–849. [Google Scholar] [CrossRef] [PubMed]
- Gull, M.A.; Bai, S.; Bak, T. A review on design of upper limb exoskeletons. Robotics 2020, 9, 16. [Google Scholar] [CrossRef]
- Cheng, G.; Xu, L. Compliance Control of a Lower Limb Rehabilitation Robot in Mirror Therapy. In Proceedings of the 2021 7th International Conference on Mechatronics and Robotics Engineering (ICMRE 2021), Budapest, Hungary, 3–5 February 2021; pp. 77–82. [Google Scholar] [CrossRef]
- Colombo, R.; Sanguineti, V. Chapter 5—Assistive controllers and modalities for robot-aided neurorehabilitation. In Rehabilitation Robotics; Colombo, R., Sanguineti, V., Eds.; Academic Press: Cambridge, MA, USA, 2018; pp. 63–74. [Google Scholar] [CrossRef]
- Vatan, H.M.F.; Nefti-Meziani, S.; Davis, S.; Saffari, Z.; El-Hussieny, H. A review: A Comprehensive Review of Soft and Rigid Wearable Rehabilitation and Assistive Devices with a Focus on the Shoulder Joint. J. Intell. Robot. Syst. Theory Appl. 2021, 102, 9. [Google Scholar] [CrossRef]
- Cardona, M.; Destarac, M.; Cena, C.G. Robotics for Rehabilitation: A State of the Art. In Exoskeleton Robots for Rehabilitation and Healthcare Devices; Springer: Singapore, 2020; pp. 1–11. [Google Scholar] [CrossRef]
- Kapsalyamov, A.; Hussain, S.; Jamwal, P.K. State-of-the-art assistive powered upper limb exoskeletons for elderly. IEEE Access 2020, 8, 178991–179001. [Google Scholar] [CrossRef]
- Brackenridge, J.; Bradnam, L.V.; Lennon, S.; Costi, J.J.; Hobbs, D.A. A review of rehabilitation devices to promote upper limb function following stroke. Neurosci. Biomed. Eng. 2016, 4, 25–42. [Google Scholar] [CrossRef]
- Gasperina, S.D.; Roveda, L.; Pedrocchi, A.; Braghin, F.; Gandolla, M. Review on Patient-Cooperative Control Strategies for Upper-Limb Rehabilitation Exoskeletons. Front. Robot. AI 2021, 8, 745018. [Google Scholar] [CrossRef] [PubMed]
- Ofner, P.; Schwarz, A.; Pereira, J.; Müller-Putz, G.R. Upper limb movements can be decoded from the time-domain of low-frequency EEG. PLoS ONE 2017, 12, e0182578. [Google Scholar] [CrossRef] [PubMed]
- Freeman, C. Control System Design for Electrical Stimulation in Upper Limb Rehabilitation; Springer International Publishing: Berlin/Heidelberg, Germany, 2016. [Google Scholar] [CrossRef]
- Proietti, T.; Crocher, V.; Roby-Brami, A.; Jarrasse, N. Upper-limb robotic exoskeletons for neurorehabilitation: A review on control strategies. IEEE Rev. Biomed. Eng. 2016, 9, 4–14. [Google Scholar] [CrossRef] [PubMed]
- De Marzi, L.; Peixoto, N. EEG-EMG-Based Interface for Upper Limb Exoskeleton—A Review. Online Resource. Available online: https://mars.gmu.edu/server/api/core/bitstreams/2a2f28cf-552d-40b1-8b57-91a5b802ee60/content (accessed on 13 January 2025).
- Fu, J.; Choudhury, R.; Hosseini, S.M.; Simpson, R.; Park, J.-H. Myoelectric Control Systems for Upper Limb Wearable Robotic Exoskeletons and Exosuits—A Systematic Review. Sensors 2022, 22, 8134. [Google Scholar] [CrossRef]
- Losey, D.P.; McDonald, C.G.; Battaglia, E.; O’Malley, M.K. A review of intent detection, arbitration, and communication aspects of shared control for physical human–robot interaction. Appl. Mech. Rev. 2018, 70, 010804. [Google Scholar] [CrossRef]
- Liu, J.; Ren, Y.; Xu, D.; Kang, S.H.; Zhang, L.Q. EMG-Based Real-Time Linear-Nonlinear Cascade Regression Decoding of Shoulder, Elbow, and Wrist Movements in Able-Bodied Persons and Stroke Survivors. IEEE Trans. Biomed. Eng. 2020, 67, 1272–1281. [Google Scholar] [CrossRef]
- Murakami, Y.; Honaga, K.; Kono, H.; Haruyama, K.; Yamaguchi, T.; Tani, M.; Isayama, R.; Takakura, T.; Tanuma, A.; Hatori, K.; et al. New Artificial Intelligence-Integrated Electromyography-Driven Robot Hand for Upper Extremity Rehabilitation of Patients With Stroke: A Randomized, Controlled Trial. Neurorehabil. Neural Repair 2023, 37, 298–306. [Google Scholar] [CrossRef]
- Qian, W.; Liao, J.; Lu, L.; Ai, L.; Li, M.; Xiao, X.; Guo, Z. CURER: A Lightweight Cable-Driven Compliant Upper Limb Rehabilitation Exoskeleton Robot. IEEE/ASME Trans. Mechatron. 2023, 28, 1730–1741. [Google Scholar] [CrossRef]
- Zahedi, A.; Wang, Y.; Lau, N.; Ang, W.T.; Zhang, D. A Bamboo-Inspired Exoskeleton (BiEXO) Based on Carbon Fiber for Shoulder and Elbow Joints. IEEE Trans. Med. Robot. Bionics 2023, 5, 375–386. [Google Scholar] [CrossRef]
- Verdel, D.; Sahm, G.; Bruneau, O.; Berret, B.; Vignais, N. A Trade-Off between Complexity and Interaction Quality for Upper Limb Exoskeleton Interfaces. Sensors 2023, 23, 4122. [Google Scholar] [CrossRef] [PubMed]
- Niu, L.; Guo, S.; Song, M.; Wu, Y.; Qu, H. Design and Analysis of a Novel Shoulder Exoskeleton Based on a Parallel Mechanism. Chin. J. Mech. Eng. (Engl. Ed.) 2023, 36, 65. [Google Scholar] [CrossRef]
- Simbaña, E.D.O.; Baeza, P.S.; Huete, A.J.; Balaguer, C. Review of automated systems for upper limbs functional assessment in neurorehabilitation. IEEE Access 2019, 7, 32352–32367. [Google Scholar] [CrossRef]
- Niyetkaliyev, A.S.; Hussain, S.; Ghayesh, M.H.; Alici, G. Review on Design and Control Aspects of Robotic Shoulder Rehabilitation Orthoses. IEEE Trans. Hum.-Mach. Syst. 2017, 47, 1134–1145. [Google Scholar] [CrossRef]
- Qassim, H.M.; Wan Hasan, W.Z. A review on upper limb rehabilitation robots. Appl. Sci. 2020, 10, 6976. [Google Scholar] [CrossRef]
- Frisoli, A.; Barsotti, M.; Sotgiu, E.; Lamola, G.; Procopio, C.; Chisari, C. A randomized clinical control study on the efficacy of three-dimensional upper limb robotic exoskeleton training in chronic stroke. J. Neuroeng. Rehabil. 2022, 19, 14. [Google Scholar] [CrossRef] [PubMed]
- Rahman, M.H.; Ouimet, T.K.; Saad, M.; Kenné, J.P.; Archambault, P.S. Development and control of a wearable robot for rehabilitation of elbow and shoulder joint movements. In Proceedings of the IECON 2010—36th Annual Conference on IEEE Industrial Electronics Society, Glendale, AZ, USA, 7–10 November 2010; pp. 1506–1511. [Google Scholar] [CrossRef]
- Fitle, K.D.; Pehlivan, A.U.; O’Malley, M.K. A robotic exoskeleton for rehabilitation and assessment of the upper limb following incomplete spinal cord injury. In Proceedings of the 2015 IEEE international conference on robotics and automation (ICRA), Seattle, WA, USA, 26–30 May 2015; pp. 4960–4966. [Google Scholar] [CrossRef]
- Lessard, S.; Pansodtee, P.; Robbins, A.; Baltaxe-Admony, L.B.; Trombadore, J.M.; Teodorescu, M.; Agogino, A.; Kurniawan, S. CRUX: A compliant robotic upper-extremity exosuit for lightweight, portable, multi-joint muscular augmentation. In Proceedings of the 2017 International Conference on Rehabilitation Robotics (ICORR), London, UK, 17–20 July 2017; pp. 1633–1638. [Google Scholar] [CrossRef]
- Jarrett, C.; McDaid, A.J. Robust control of a cable-driven soft exoskeleton joint for intrinsic human-robot interaction. IEEE Trans. Neural Syst. Rehabil. Eng. 2017, 25, 976–986. [Google Scholar] [CrossRef] [PubMed]
- Barria, P.; Riquelme, M.; Reppich, H.; Cisnal, A.; Fraile, J.C.; Pérez-Turiel, J.; Sierra, D.; Aguilar, R.; Andrade, A.; Nuñez-Espinosa, C. Hand rehabilitation based on the RobHand exoskeleton in stroke patients: A case series study. Front. Robot. AI 2023, 10, 1146018. [Google Scholar] [CrossRef]
- Oguntosin, V.W.; Mori, Y.; Kim, H.; Nasuto, S.J.; Kawamura, S.; Hayashi, Y. Design and Validation of exoskeleton actuated by soft modules toward neurorehabilitation-vision-based control for precise reaching motion of upper limb. Front. Neurosci. 2017, 11, 352. [Google Scholar] [CrossRef]
- Ferguson, P.W.; Dimapasoc, B.; Shen, Y.; Rosen, J. Design of a hand exoskeleton for use with upper limb exoskeletons. Biosyst. Biorobot. 2019, 22, 276–280. [Google Scholar] [CrossRef]
- Mahdavian, M.; Toudeshki, A.G.; Yousefi-Koma, A. Design and Fabrication of a 3DoF Upper Limb Exoskeleton. In Proceedings of the 2015 3rd RSI International Conference on Robotics and Mechatronics (ICROM), Tehran, Iran, 7–9 October 2015. [Google Scholar] [CrossRef]
- Rocon, E.; Ruiz, A.F.; Manto, M.; Moreno, J.C.; Pons, J.L. Design and Validation of a Rehabilitation Robotic Exoskeleton for Tremor Assessment and Suppression. IEEE Trans. Neural Syst. Rehabil. Eng. 2007, 15, 367–378. [Google Scholar] [CrossRef] [PubMed]
- Gopura, R.; Kiguchi, K.; Li, Y. SUEFUL-7: A 7DOF upper-limb exoskeleton robot with muscle-model-oriented EMG-based control. In Proceedings of the 2009 IEEE/RSJ International Conference on Intelligent Robots and Systems, St. Louis, MO, USA, 11–15 October 2009; pp. 1126–1131. [Google Scholar] [CrossRef]
- Kim, B.; Deshpande, A.D. An upper-body rehabilitation exoskeleton Harmony with an anatomical shoulder mechanism: Design, modeling, control, and performance evaluation. Int. J. Robot. Res. 2017, 36, 414–435. [Google Scholar] [CrossRef]
- de Oliveira, A.C.; Rose, C.G.; Warburton, K.; Ogden, E.M.; Whitford, B.; Lee, R.K.; Deshpande, A.D. Exploring the Capabilities of Harmony for Upper-Limb Stroke Therapy. In Proceedings of the 2019 IEEE 16th International Conference on Rehabilitation Robotics (ICORR), Toronto, ON, Canada, 24–28 June 2019; pp. 637–643. [Google Scholar] [CrossRef]
- Ghonasgi, K.; Oliveira, A.C.D.; Shafer, A.; Rose, C.G.; Deshpande, A.D. Estimating the Effect of Robotic Intervention on Elbow Joint Motion. In Proceedings of the 2019 28th IEEE International Conference on Robot and Human Interactive Communication (RO-MAN), New Delhi, India, 14–18 October 2019. [Google Scholar] [CrossRef]
- Klein, J.; Spencer, S.; Allington, J.; Bobrow, J.E.; Reinkensmeyer, D.J. Optimization of a parallel shoulder mechanism to achieve a high-force, low-mass, robotic-arm exoskeleton. IEEE Trans. Robot. 2010, 26, 710–715. [Google Scholar] [CrossRef]
- Garrec, P.; Friconneau, J.P.; Méasson, Y.; Perrot, Y. ABLE, an innovative transparent exoskeleton for the upper-limb. In Proceedings of the 2008 IEEE/RSJ International Conference on Intelligent Robots and Systems, Nice, France, 22–26 September 2008; pp. 1483–1488. [Google Scholar] [CrossRef]
- Rahman, M.; Saad, M.; Jean-Pierre, K.; Archambault, P. Control of an Exoskeleton Robot Arm with Sliding Mode Exponential Reaching Law. Int. J. Control Autom. Syst. 2013, 11, 92–104. [Google Scholar] [CrossRef]
- Rahman, M.H.; Rahman, M.J.; Cristobal, O.L.; Saad, M.; Kenné, J.P.; Archambault, P.S. Development of a whole arm wearable robotic exoskeleton for rehabilitation and to assist upper limb movements. Robotica 2015, 33, 19–39. [Google Scholar] [CrossRef]
- Ebrahimi, A.; Groninger, D.; Singer, R.; Schneider, U. Control parameter optimization of the actively powered upper body exoskeleton using subjective feedbacks. In Proceedings of the 2017 3rd International Conference on Control, Automation and Robotics (ICCAR), Nagoya, Japan, 22–24 April 2017; pp. 432–437. [Google Scholar] [CrossRef]
- Hsieh, H.-C.; Chen, D.-F.; Chien, L.; Lan, C.-C. Design of a Parallel Actuated Exoskeleton for Adaptive and Safe Robotic Shoulder Rehabilitation. IEEE/ASME Trans. Mechatron. 2017, 22, 2034–2045. [Google Scholar] [CrossRef]
- Hadi, A.; Alipour, K.; Kazeminasab, S.; Elahinia, M. ASR glove: A wearable glove for hand assistance and rehabilitation using shape memory alloys. J. Intell. Mater. Syst. Struct. 2017, 29, 1045389X1774272. [Google Scholar] [CrossRef]
- Sale, P.; Stellin, G.; Masiero, S.; Becchi, F.; Sieklicki, W. FEX a Fingers Extending eXoskeleton for Rehabilitation and Regaining Mobility. In Advances in Service and Industrial Robotics: Proceedings of the 26th International Conference on Robotics in Alpe-Adria-Danube Region, RAAD 2017; Springer International Publishing: Berlin/Heidelberg, Germany, 2018; pp. 813–824. [Google Scholar] [CrossRef]
- Sandoval-Gonzalez, O.; Jacinto-Villegas, J.; Herrera-Aguilar, I.; Portillo-Rodiguez, O.; Tripicchio, P.; Hernandez-Ramos, M.; Flores-Cuautle, A.; Avizzano, C. Design and Development of a Hand Exoskeleton Robot for Active and Passive Rehabilitation. Int. J. Adv. Robot. Syst. 2016, 13, 66. [Google Scholar] [CrossRef]
- Sutapun, A.; Sangveraphunsiri, V. A 4-DOF Upper Limb Exoskeleton for Stroke Rehabilitation: Kinematics Mechanics and Control. Int. J. Mech. Eng. Robot. Res. 2015, 4, 269–272. [Google Scholar] [CrossRef]
- Ripel, T.; Krejsa, J.; Hrbacek, J.; Cizmar, I. Active Elbow Orthosis. Int. J. Adv. Robot. Syst. 2014, 11, 143. [Google Scholar] [CrossRef]
- Bundy, D.T.; Souders, L.; Baranyai, K.; Leonard, L.; Schalk, G.; Coker, R.; Moran, D.W.; Huskey, T.; Leuthardt, E.C. Contralesional Brain-Computer Interface Control of a Powered Exoskeleton for Motor Recovery in Chronic Stroke Survivors. Stroke 2017, 48, 1908–1915. [Google Scholar] [CrossRef]
- Genna, C.; Dosen, S.; Paredes, L.; Turolla, A.; Graimann, B.; Farina, D. A novel robot-aided therapy for shoulder rehabilitation after stroke: Active-assisted control of the rehaarm robot using electromyographic signals. Biosyst. Biorobot. 2014, 7, 383–391. [Google Scholar] [CrossRef]
- Accogli, A.; Grazi, L.; Crea, S.; Panarese, A.; Carpaneto, J.; Vitiello, N.; Micera, S. EMG-Based Detection of User’s Intentions for Human-Machine Shared Control of an Assistive Upper-Limb Exoskeleton. 2017. Available online: https://api.semanticscholar.org/CorpusID:114960887 (accessed on 13 January 2025).
- Hosseini, M.; Meattini, R.; Palli, G.; Melchiorri, C. A Wearable Robotic Device Based on Twisted String Actuation for Rehabilitation and Assistive Applications. J. Robot. 2017, 2017, 3036468. [Google Scholar] [CrossRef]
- Rong, W.; Tong, K.Y.; Hu, X.L.; Ho, S.K. Effects of electromyography-driven robot-aided hand training with neuromuscular electrical stimulation on hand control performance after chronic stroke. Disabil. Rehabil. Assist. Technol. 2015, 10, 149–159. [Google Scholar] [CrossRef]
- Ben, I.A.; Bouteraa, Y.; Rekik, C. Design and development of 3d printed myoelectric robotic exoskeleton for hand rehabilitation. Int. J. Smart Sens. Intell. Syst. 2017, 10, 341–366. [Google Scholar] [CrossRef]
- Hu, X.L.; Tong, K.Y.; Song, R.; Zheng, X.J.; Lui, K.H.; Leung, W.W.F.; Ng, S.; Au-Yeung, S.S.Y. Quantitative evaluation of motor functional recovery process in chronic stroke patients during robot-assisted wrist training. J. Electromyogr. Kinesiol. Off. J. Int. Soc. Electrophysiol. Kinesiol. 2009, 19, 639–650. [Google Scholar] [CrossRef] [PubMed]
- Lambelet, C.; Lyu, M.; Woolley, D.; Gassert, R.; Wenderoth, N. The eWrist—A wearable wrist exoskeleton with sEMG-based force control for stroke rehabilitation. In Proceedings of the 2017 International Conference on Rehabilitation Robotics (ICORR), London, UK, 17–20 July 2017; pp. 726–733. [Google Scholar] [CrossRef]
- Nam, C.; Rong, W.; Li, W.; Cheung, C.; Ngai, W.; Cheung, T.; Pang, M.; Li, L.; Hu, J.; Wai, H.; et al. An Exoneuromusculoskeleton for Self-Help Upper Limb Rehabilitation after Stroke. Soft Robot. 2022, 9, 14–35. [Google Scholar] [CrossRef] [PubMed]
- Montaño, J.; Garcia Cena, C.; Chamorro, L.; Destarac, M.; Saltaren, R. Mechanical Design of a Robotic Exoskeleton for Upper Limb Rehabilitation. In Advances in Automation and Robotics Research in Latin America: Proceedings of the 1st Latin American Congress on Automation and Robotics, Panama City, Panama 2017; Springer International Publishing: Berlin/Heidelberg, Germany, 2017; pp. 297–308. [Google Scholar] [CrossRef]
- Destarac, M.A.; Garcia, C.E.; Garcia, J.; Espinoza, R.; Saltaren, R.J. ORTE: Robot for upper limb rehabilitation. biomechanical analysis of human movements. IEEE Lat. Am. Trans. 2018, 16, 1638–1643. [Google Scholar] [CrossRef]
- Hunt, J.; Lee, H.; Artemiadis, P. A novel shoulder exoskeleton robot using parallel actuation and a passive slip interface. J. Mech. Robot. 2017, 9, 011002. [Google Scholar] [CrossRef]
- Crea, S.; Cempini, M.; Mazzoleni, S.; Carrozza, M.C.; Posteraro, F.; Vitiello, N. Phase-II clinical validation of a powered exoskeleton for the treatment of elbow spasticity. Front. Neurosci. 2017, 11, 261. [Google Scholar] [CrossRef]
- Shao, Z.; Tang, X.; Yi, W. Optimal Design of a 3-DOF Cable-Driven Upper Arm Exoskeleton. Adv. Mech. Eng. 2015, 6, 157096. [Google Scholar] [CrossRef]
- Wu, Q.; Wang, X.; Du, F. Development and analysis of a gravity-balanced exoskeleton for active rehabilitation training of upper limb. Proc. Inst. Mech. Eng. Part C J. Mech. Eng. Sci. 2015, 230, 3777–3790. [Google Scholar] [CrossRef]
- Copaci, D.; Flores-Caballero, A.; Molina-Rueda, F.; Alguacil, I.; Blanco, D.; Moreno, L. Wearable Elbow Exoskeleton Actuated with Shape Memory Alloy. Biosyst. Biorobot. 2016, 15, 477–481. [Google Scholar] [CrossRef]
- Lessard, S.; Pansodtee, P.; Robbins, A.; Trombadore, J.M.; Kurniawan, S.; Teodorescu, M. A Soft Exosuit for Flexible Upper-Extremity Rehabilitation. IEEE Trans. Neural Syst. Rehabil. Eng. 2018, 26, 1604–1617. [Google Scholar] [CrossRef]
- Sarac, M.; Solazzi, M.; Leonardis, D.; Sotgiu, E.; Bergamasco, M.; Frisoli, A. Design of an Underactuated Hand Exoskeleton with Joint Estimation. In Advances in Italian Mechanism Science: Proceedings of the First International Conference of IFToMM Italy; Springer International Publishing: Berlin/Heidelberg, Germany, 2017; Volume 47. [Google Scholar] [CrossRef]
- Sharma, M.K.; Ordonez, R. Design and fabrication of an intention based upper-limb exo-skeleton. In Proceedings of the 2016 IEEE International Symposium on Intelligent Control (ISIC), Buenos Aires, Argentina, 19–22 September 2016; pp. 2–7. [Google Scholar] [CrossRef]
- Cui, X.; Chen, W.; Jin, X.; Agrawal, S.K. Design of a 7-DOF Cable-Driven Arm Exoskeleton (CAREX-7) and a Controller for Dexterous Motion Training or Assistance. IEEE/ASME Trans. Mechatron. 2017, 22, 161–172. [Google Scholar] [CrossRef]
- Mao, Y.; Agrawal, S.K. Design of a cable-driven arm exoskeleton (CAREX) for neural rehabilitation. IEEE Trans. Robot. 2012, 28, 922–931. [Google Scholar] [CrossRef]
- Khan, A.M.; Yun, D.; Ali, M.A.; Zuhaib, K.M.; Yuan, C.; Iqbal, J.; Han, J.; Shin, K.; Han, C. Passivity based adaptive control for upper extremity assist exoskeleton. Int. J. Control Autom. Syst. 2016, 14, 291–300. [Google Scholar] [CrossRef]
- Rosales, Y.; López, R.; Diaz, I.R.; Salazar, S.; Lozano, R. Design and modeling of an upper limb exoskeleton. In Proceedings of the 2015 19th International Conference on System Theory, Control and Computing (ICSTCC), Cheile Gradistei, Romania, 14–16 October 2015; pp. 266–272. [Google Scholar] [CrossRef]
- Lin, C.H.; Lien, W.M.; Wang, W.W.; Chen, S.H.; Lo, C.H.; Lin, S.Y.; Fu, L.C.; Lai, J.S. NTUH-II robot arm with dynamic torque gain adjustment method for frozen shoulder rehabilitation. In Proceedings of the 2014 IEEE/RSJ International Conference on Intelligent Robots and Systems, Chicago, IL, USA, 14–18 September 2014; pp. 3555–3560. [Google Scholar] [CrossRef]
- Perry, J.C.; Rosen, J.; Burns, S. Upper-limb powered exoskeleton design. IEEE/ASME Trans. Mechatron. 2007, 12, 408–417. [Google Scholar] [CrossRef]
- Gunasekara, M.; Gopura, R.; Jayawardena, S. 6-REXOS: Upper Limb Exoskeleton Robot with Improved pHRI. Int. J. Adv. Robot. Syst. 2015, 12, 47. [Google Scholar] [CrossRef]
- Kawasaki, H.; Ito, S.; Nishimoto, Y.; Ueki, S.; Ishigure, Y.; Mouri, T. Hand motion assist robot for rehabilitation therapy. J. Robot. Mechatron. 2014, 26, 103–104. [Google Scholar] [CrossRef]
- Mihelj, M.; Podobnik, J.; Munih, M. HEnRiE-Haptic Environment for Reaching and Grasping Exercise. In Proceedings of the 2008 2nd IEEE RAS & EMBS International Conference on Biomedical Robotics and Biomechatronics, Scottsdale, AZ, USA, 19–22 October 2008; pp. 907–912. [Google Scholar] [CrossRef]
- Tomić, T.J.D.; Savić, A.M.; Vidaković, A.S.; Rodić, S.Z.; Isaković, M.S.; Rodríguez-de-Pablo, C.; Keller, T.; Konstantinović, L.M. ArmAssist robotic system versus matched conventional therapy for poststroke upper limb rehabilitation: A randomized clinical trial. Biomed Res. Int. 2017, 2017, 7659893. [Google Scholar] [CrossRef] [PubMed]
- Dehem, S.; Montedoro, V.; Brouwers, I.; Edwards, M.G.; Detrembleur, C.; Stoquart, G.; Renders, A.; Heins, S.; Dehez, B.; Lejeune, T. Validation of a robot serious game assessment protocol for upper limb motor impairment in children with cerebral palsy. NeuroRehabilitation 2019, 45, 137–149. [Google Scholar] [CrossRef]
- Kubota, S.; Kadone, H.; Shimizu, Y.; Hara, Y.; Kubo, T.; Watanabe, H.; Hada, Y.; Ochiai, N.; Yamazaki, M. Robotic rehabilitation training with a newly developed upper limb single-joint Hybrid Assistive Limb (HAL-SJ) for elbow flexor reconstruction after brachial plexus injury: A report of two cases. J. Orthop. Surg. 2018, 26, 2309499018777887. [Google Scholar] [CrossRef]
- Villafañe, J.H.; Taveggia, G.; Galeri, S.; Bissolotti, L.; Mullè, C.; Imperio, G.; Valdes, K.; Borboni, A.; Negrini, S. Efficacy of Short-Term Robot-Assisted Rehabilitation in Patients With Hand Paralysis After Stroke: A Randomized Clinical Trial. Hand 2018, 13, 95–102. [Google Scholar] [CrossRef]
- Krebs, H.I.; Hogan, N.; Aisen, M.L.; Volpe, B.T. Robot-Aided Neurorehabilitation. IEEE Trans. Rehabil. Eng. 1998, 6, 75–87. [Google Scholar] [CrossRef] [PubMed]
- Mazzoleni, S.; Sale, P.; Franceschini, M.; Bigazzi, S.; Carrozza, M.C.; Dario, P.; Posteraro, F. Effects of proximal and distal robot-assisted upper limb rehabilitation on chronic stroke recovery. NeuroRehabilitation 2013, 33, 33–39. [Google Scholar] [CrossRef] [PubMed]
- Adomavičienė, A.; Daunoravičienė, K.; Kubilius, R.; Varžaitytė, L.; Raistenskis, J. Influence of New Technologies on Post-Stroke Rehabilitation: A Comparison of Armeo Spring to the Kinect System. Medicina 2019, 55, 98. [Google Scholar] [CrossRef]
- Trent, L.; Intintoli, M.; Prigge, P.; Bollinger, C.; Walters, L.S.; Conyers, D.; Miguelez, J.; Ryan, T. A narrative review: Current upper limb prosthetic options and design. Disabil. Rehabil. Assist. Technol. 2020, 15, 604–613. [Google Scholar] [CrossRef]
- Cardona, M.; Solanki, K.S.; García Cena, C.E. Springer Briefs In Applied Sciences And Technology: Exoskeleton Robots for Rehabilitation and Healthcare Devices. 2020. Available online: http://www.springer.com/series/8884 (accessed on 13 January 2025).
- Sui, D.; Fan, J.; Jin, H.; Cai, X.; Zhao, J.; Zhu, Y. Design of a wearable upper-limb exoskeleton for activities assistance of daily living. In Proceedings of the 2017 IEEE International Conference on Advanced Intelligent Mechatronics (AIM), Munich, Germany, 3–7 July 2017; pp. 845–850. [Google Scholar] [CrossRef]
- Hartopanu, S.; Poboroniuc, M.; Florin, S.; Irimia, D.; Livint, G. Design of a hybrid FES-mechanical intelligent haptic robotic glove. In Proceedings of the 2013 17th International Conference on System Theory, Control and Computing (ICSTCC), Sinaia, Romania, 11–13 October 2013; pp. 687–692. [Google Scholar] [CrossRef]
- ISO 13485:2016; Medical Devices—Quality Management Systems—Requirements for Regulatory Purposes. International Organization for Standardization: Geneva, Switzerland, 2016.
- IEC 60601-1:2005+AMD1:2012; Medical Electrical Equipment—Part 1: General Requirements for Basic Safety and Essential Performance. International Electrotechnical Commission: Geneva, Switzerland, 2012.
- IEC 60601-1-2:2014; Medical Electrical Equipment—Part 1–2: General Requirements for Basic Safety and Essential Performance—Collateral Standard: Electromagnetic Disturbances—Requirements and Tests. International Electrotechnical Commission: Geneva, Switzerland, 2014.

| Company Category | Manufacturers and Country of Origin | Clinical Application |
|---|---|---|
| Global Leading Companies | Hocoma (Switzerland) | Lokomat (gait training systems) |
| Ekso Bionics (USA) | EksoNR (rehabilitation exoskeletons) | |
| Tyromotion (Austria) | Physical and cognitive rehabilitation systems | |
| InMotion Robots/Bionik Laboratories (USA) | Robots for neurorehabilitation | |
| Cyberdyne (Japan) | HAL (exoskeleton based on bio-signals) | |
| ReWalk Robotics (Israel/USA/Germany) | Exoskeletons for assisted mobility | |
| Specialized Manufacturers | Motorika Medical (Israel) | Devices for motor rehabilitation |
| Myomo (USA) | Lightweight arm exoskeletons | |
| Rex Bionics (New Zealand/Australia) | Full-body exoskeletons | |
| Honda (Japan) | Walking Assist Device | |
| Toyota Motor Corporation (Japan) | Robots for rehabilitation | |
| AlterG (USA) | Anti-gravity treadmills | |
| European Companies | Technaid (Spain) | Motion analysis systems |
| Gogoa Mobility Robots (Spain) | Exoskeletons for mobility rehabilitation | |
| ABLE Human Motion (Spain) | Affordable exoskeletons | |
| KUKA Robotics (Germany) | Collaborative robots for rehabilitation | |
| Ottobock (Germany) | Advanced prosthetics and mobility solutions | |
| Japanese Companies | Fourier Intelligence (China) | Adaptive robots for rehabilitation |
| Yaskawa Electric (Japan) | Industrial and medical exoskeletons | |
| Panasonic (Japan) | Robotic solutions for medical care | |
| ATOUN (Japan) | Robots for assistance and mobility | |
| Startups and Emerging Companies | Wandercraft (France/Spain) | Atalante (autonomous exoskeleton) |
| Marsi Bionics (Spain) | Pediatric exoskeletons | |
| SuitX/US Bionics (USA) | Accessible exoskeletons for various applications | |
| Axosuits (Romania) | Affordable exoskeletons | |
| B-Temia (Canada) | Mobility assistance devices | |
| ExoAtlet (Luxembourg/Russia) | Clinical exoskeletons | |
| Companies with Medical Robotics Divisions | Össur (Iceland) | Robotic prosthetics |
| Kinova Robotics (Canada) | Robots for assistance and personal care | |
| Barrett Technology (USA) | Medical robots for neurorehabilitation | |
| Meditouch (Israel) | Technologies for physical therapy | |
| Rehab-Robotics (Hong Kong) | Robots for extremity rehabilitation | |
| Focal Meditech (Netherlands) | Customized robotic solutions | |
| Research and Development Companies | Corindus (USA) | Robots for cardiovascular procedures |
| Medexo Robotics (Hong Kong) | Robots for clinical rehabilitation | |
| Curexo (South Korea) | Robots for orthopedic rehabilitation | |
| Instead Technologies (Spain) | Innovative solutions in assistive technology |
| Query | Keywords | IEEE Xplore | Science Direct | Scopus | Springer Link | Total |
|---|---|---|---|---|---|---|
| 1 | “rehabilitation robotics” AND “exoskeleton” AND “upper limb” | 157 | 605 | 369 | 389 | 1520 |
| Total | 1520 | |||||
| Total duplicates removed | 972 | |||||
| Total titles screened | 359 | |||||
| Total abstracts screened | 131 | |||||
| Total full text screened | 18 | |||||
| Total full text selection | 40 | |||||
| No. | Inclusion Criteria |
|---|---|
| 1 | The article focuses on upper limb rehabilitation robotics. |
| 2 | The article focuses on myoelectric control research. |
| 3 | The article focuses on neural network-based or predictive control for exoskeletons. |
| No. | Exclusion Criteria |
|---|---|
| 1 | The article is not published in English or Spanish. |
| 2 | The article describes only prosthetics without control systems. |
| 3 | The article is not focused on upper limb rehabilitation. |
| Main Control Method | Robotic Device | TRL | Targeted Joint | DoFs | Type of Actuators | Sample Testing |
|---|---|---|---|---|---|---|
| Admittance control | MAHI [33] | 8 | Forearm, wrist. | 5 | Frameless DC motor | Yes, Clinical trial NCT01948739 |
| Hand exoskeleton [38] | 4 | Fingers. | 6 | Cable-driven | Not given | |
| Impedance control | Upper limb exoskeleton [39] | 3 | Shoulder, forearm. | 3 | EC motor | Not given |
| WOTAS [40] | 5 | Forearm, wrist. | 3 | Brushless DC motor | Yes | |
| SUEFUL-7 [41] | 7 | Shoulder, elbow, forearm, wrist. | 7 | DC motor | Yes | |
| Harmony [42,43,44] | 7 | Shoulder, elbow. | 7 | Series Elastic Actuator | Yes | |
| Force control | BONES [45] | 6 | Shoulder, elbow. | 4 | Pneumatic actuators | Yes |
| ABLE [46] | 6 | Shoulder, elbow. | 4 | Screw-cable | Yes | |
| MARSE-7 [47,48] | 7 | Shoulder, elbow, forearm, wrist. | 7 | Brushless DC motor | Yes | |
| Stuttgart Exo Jacket [49] | 7 | Shoulder, elbow. | 12 | EC Motor with Spring mechanism | Yes | |
| Exo for the shoulder joint [50] | 5 | Shoulder. | 6 | DC motor | Not given | |
| ASR Glove [51] | 6 | Fingers. | 3 for each finger | Shape memory alloy | Yes | |
| Yes | ||||||
| FEX [52] | 6 | Fingers. | 4 | DC motor | Yes | |
| ExoK’ab 2016 [53] | 6 | Fingers. | 6 | DC motor | Yes | |
| Upper limb exoskeleton [54] | 6 | Shoulder, elbow. | 4 | DC motor | Yes | |
| Upper limb exoskeleton [34] | 6 | Shoulder, forearm. | 6 | DC motor | Yes | |
| Active elbow orthosis [55] | 6 | Elbow. | 1 | DC motor | Yes | |
| Electroencephalography (EEG) based control | BCI powered exoskeleton [56] | 8 | Fingers. | 1 | DC motor | Yes, Clinical trial NCT02552368 |
| EMG and sEMG based control | RehaArm [57] | 8 | Shoulder. | 3 | Artificial muscle | Yes, Clinical trial NCT02321254 |
| NESM [58] | 7 | Elbow, wrist. | 4 | Brushless DC motor | Yes | |
| Wearable robotic [59] | 7 | Elbow. | 1 | Twisted string | Yes | |
| NMES-Robot [60] | 7 | Fingers. | 2 for each finger | Linear actuator | Yes | |
| Myoelectric Hand Exoskeleton [61] | 7 | Fingers. | 3 for each finger | Servo motor | Yes | |
| Robot-assisted wrist [62] | 6 | Wrist. | 1 | DC motor | Yes | |
| The eWrist [63] | 6 | Wrist. | 1 | DC motor | Yes | |
| Exoneuromusculoskeleton [64] | 8 | Elbow, wrist. | 2 | Soft pneumatic muscles | Yes, Clinical trial NCT03752775 | |
| Joint angle control | Elbow and wrist Exoskeleton [65] | 6 | Elbow, wrist. | 2 | DC motor | Yes |
| ORTE [66] | 8 | Shoulder, elbow, forearm. | 6 | Servo motor | Yes | |
| Upper limb Robotic Exo [67] | 6 | Shoulder, elbow, forearm. | 6 | Servo motor | Yes | |
| Parallel actuated shoulder exoskeleton [68] | 5 | Shoulder. | 5 | DC motor | Not given | |
| NEURO-Exos [69] | 5 | Elbow. | 1 | DC motor | Yes | |
| Upper arm exoskeleton [70] | 5 | Shoulder, elbow. | 3 | Cable-driven | Not given | |
| Gravity balanced exoskeleton [71] | 5 | Shoulder, elbow. | 5 | Brushless Servo motor | Not given | |
| Wearable elbow exoskeleton [72] | 5 | Elbow. | 2 | SMA | Not given | |
| Hand exoskeleton [73] | 5 | Fingers. | 5 | DC motor | Not given | |
| Wearable upper limb exoskeleton [74] | 6 | Shoulder, elbow. | 5 | Cable-driven mechanism | Yes | |
| Upper limb exoskeleton [75] | 5 | Shoulder, forearm. | 3 | DC motor | Not given | |
| Cable-driven soft exoskeleton [35] | 6 | Elbow. | 1 | Cable-driven | Yes | |
| CAREX [76] | 8 | Shoulder, elbow, wrist. | 7 | Cable-driven by motor | Yes, Clinical trial NCT02726204 | |
| CRUX [77] | 6 | Shoulder, forearm. | 3 | DC motor | Yes | |
| Upper limb exoskeleton [78] | 6 | Shoulder, elbow. | 2 | DC motor | Yes | |
| NTUH-II [79] | 8 | Shoulder, elbow, wrist | 8 | DC motor | Yes, Clinical trial NCT06113380 | |
| CADEN-7 [80] | 6 | Shoulder, elbow, forearm, wrist. | 7 | Brushed motors with cable-driven reduction pulleys | Yes | |
| 6-REXOS [81] | 5 | Elbow, forearm, wrist. | 6 | DC motor | Not given | |
| ExoRob [32] | 5 | Forearm, wrist. | 2 | Maxon EC-45 | Not given | |
| Master-slave control | Hand motion assist robot for therapy [82] | 5 | Wrist, fingers. | 18 | DC motor | Not given |
| Visual, haptic, and auditory-based control | HEnRiE [83] | 5 | Shoulder, elbow, wrist. | 5 | DC motor | Not given |
| Haptic robotic glove [36] | 5 | Fingers. | 3 for each finger | Pneumatic drive | Not given | |
| RobHand [37] | 8 | Fingers. | 5 | Linear actuator | Yes, Clinical trial NCT05598892. | |
| EAsoftM exoskeleton [84] | 6 | Elbow, wrist. | 4 | Pneumatic actuator | Yes | |
| Arm Assist (AA) [85] | 8 | Shoulder, elbow. | 2 | DC motor Cable-driven | Yes, Clinical trial NCT02729649 | |
| REAPlan [86] | 8 | Shoulder, elbow. | 2 | DC motor | Yes, Clinical trial NCT02543424 | |
| HAL-SJ [87] | 8 | Elbow. | 2 | DC motor | Yes, Clinical trial UMIN000014336 | |
| Gloreha-hand [88] | 9 | Wrist, fingers. | 1 for each fingers | Cable-driven | Yes, Clinical trial NCT02711787 | |
| InMotion 2 [89,90] | 9 | Shoulder, elbow. | 2 | Brushless DC motor | Yes, Clinical trial NCT00453843 | |
| RH-UL-LEXOS-10 [31] | 9 | Shoulder, elbow, wrist. | 7 | Cable-driven | Yes, Clinical trial NCT03319992 | |
| Armeo power [91] | 9 | Shoulder, elbow, forearm, wrist. | 5 | DC motor | Yes, Clinical trial NCT01485354 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Diaz, F.H.; Borrás Pinilla, C.; García Cena, C.E. Exploring Robotic Technologies for Upper Limb Rehabilitation: Current Status and Future Directions. J. Sens. Actuator Netw. 2025, 14, 48. https://doi.org/10.3390/jsan14030048
Diaz FH, Borrás Pinilla C, García Cena CE. Exploring Robotic Technologies for Upper Limb Rehabilitation: Current Status and Future Directions. Journal of Sensor and Actuator Networks. 2025; 14(3):48. https://doi.org/10.3390/jsan14030048
Chicago/Turabian StyleDiaz, Fabian Horacio, Carlos Borrás Pinilla, and Cecilia E. García Cena. 2025. "Exploring Robotic Technologies for Upper Limb Rehabilitation: Current Status and Future Directions" Journal of Sensor and Actuator Networks 14, no. 3: 48. https://doi.org/10.3390/jsan14030048
APA StyleDiaz, F. H., Borrás Pinilla, C., & García Cena, C. E. (2025). Exploring Robotic Technologies for Upper Limb Rehabilitation: Current Status and Future Directions. Journal of Sensor and Actuator Networks, 14(3), 48. https://doi.org/10.3390/jsan14030048







