Doxorubicin Is Key for the Cardiotoxicity of FAC (5-Fluorouracil + Adriamycin + Cyclophosphamide) Combination in Differentiated H9c2 Cells
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Methods
2.2.1. Cell Culture Experimental Protocols
2.2.2. Experimental Protocol Paradigm
- -
- the drugs per se in different concentrations (DOX (0.13–5 µM), 5-FU (0.13–5 µM), CYA (0.13–5 µM));
- -
- equimolar mixtures of the parent drugs (FAC (0.2; 1 or 5 µM));
- -
- FAC mixture with concentrations based in the plasma levels of treated patients (50 µM 5-FU + 1 µM DOX + 50 µM CYA) (Table 1).
2.2.3. Cytotoxicity Tests
MTT Reduction Assay
Lysosomal Neutral Red Uptake Assay
2.2.4. Microscopic Observation of the Cells
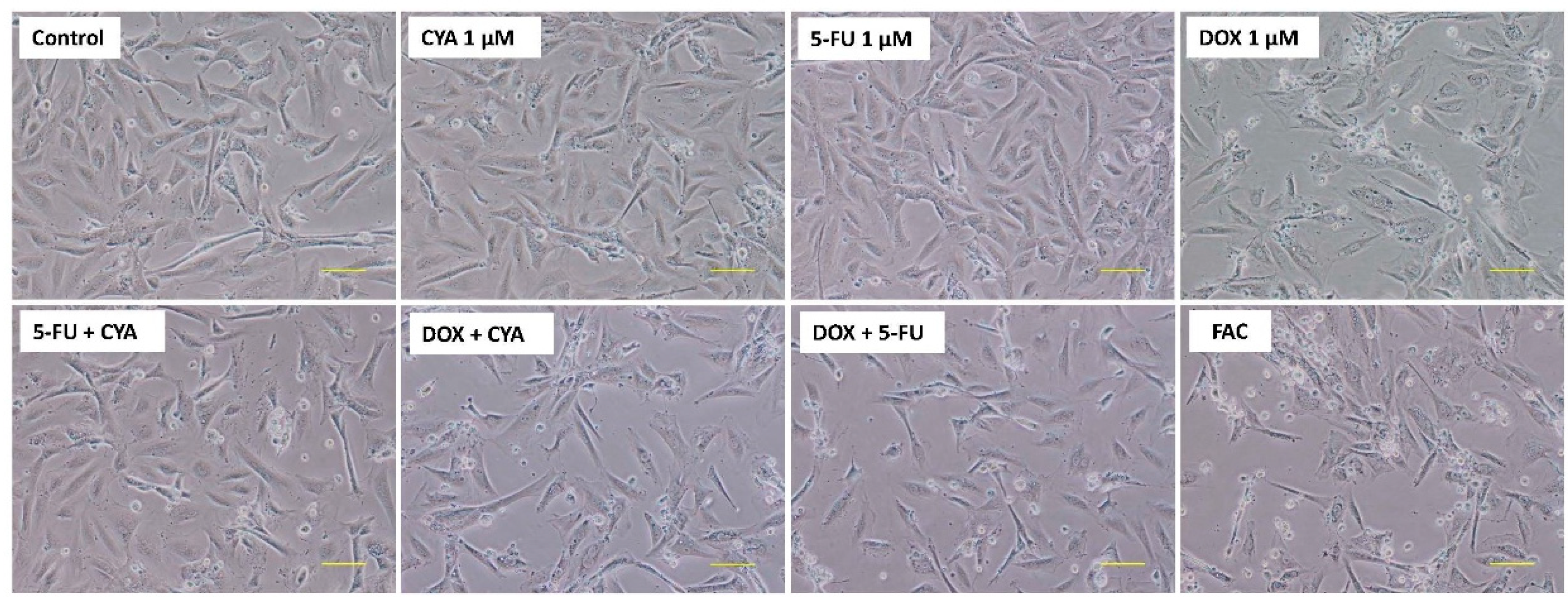
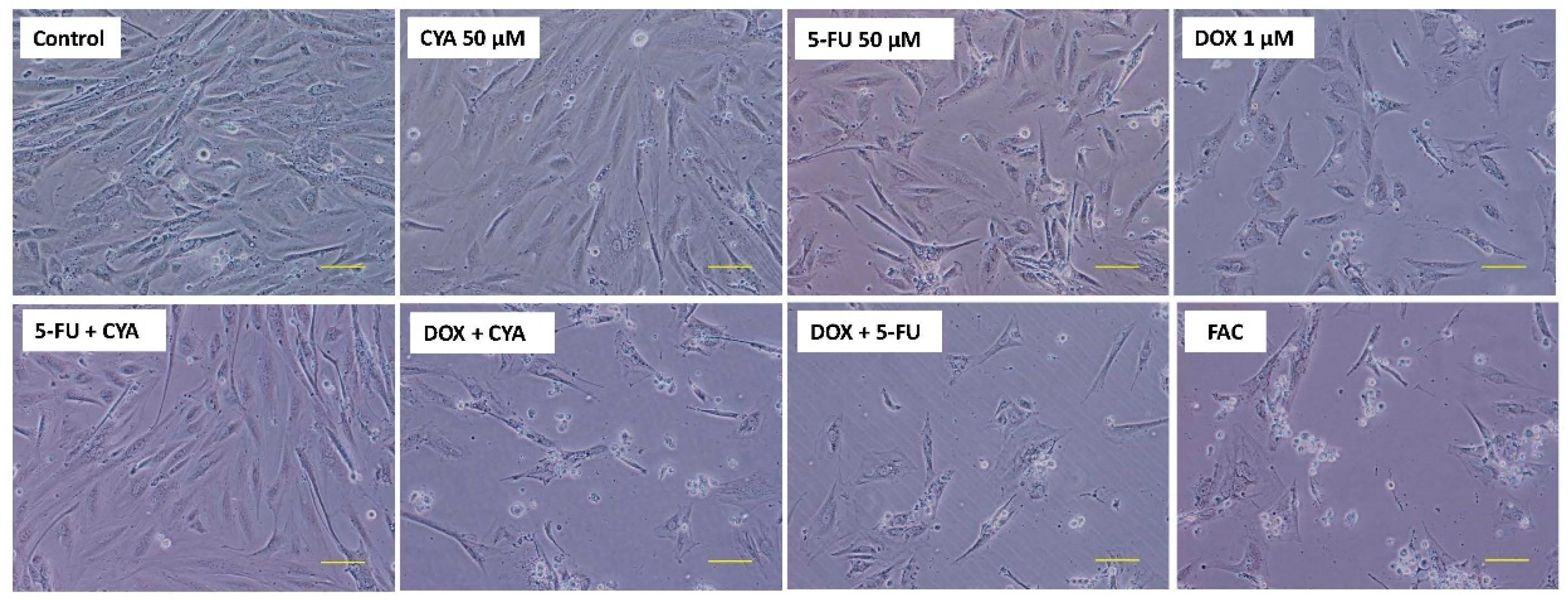
Contrast Phase Microscopy
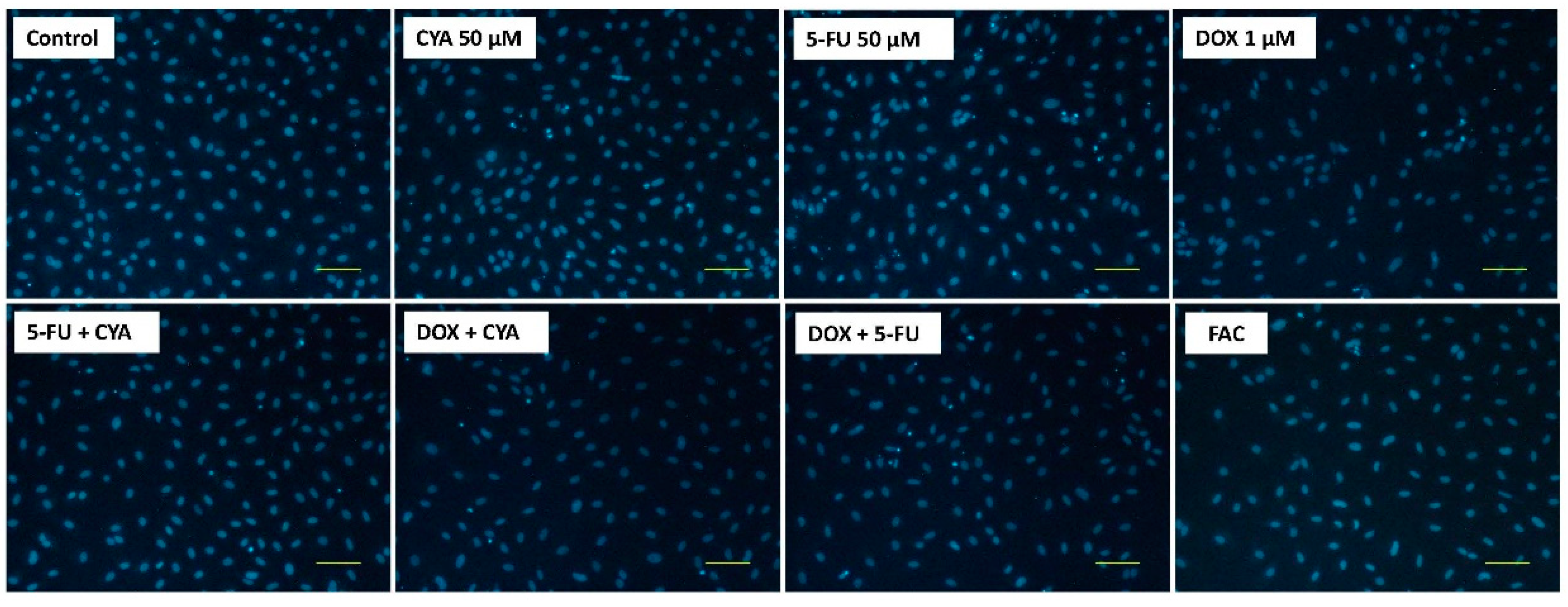
Hoechst Nuclear Staining
2.2.5. Mitochondrial Membrane Potential
2.2.6. Statistical Analysis
3. Results
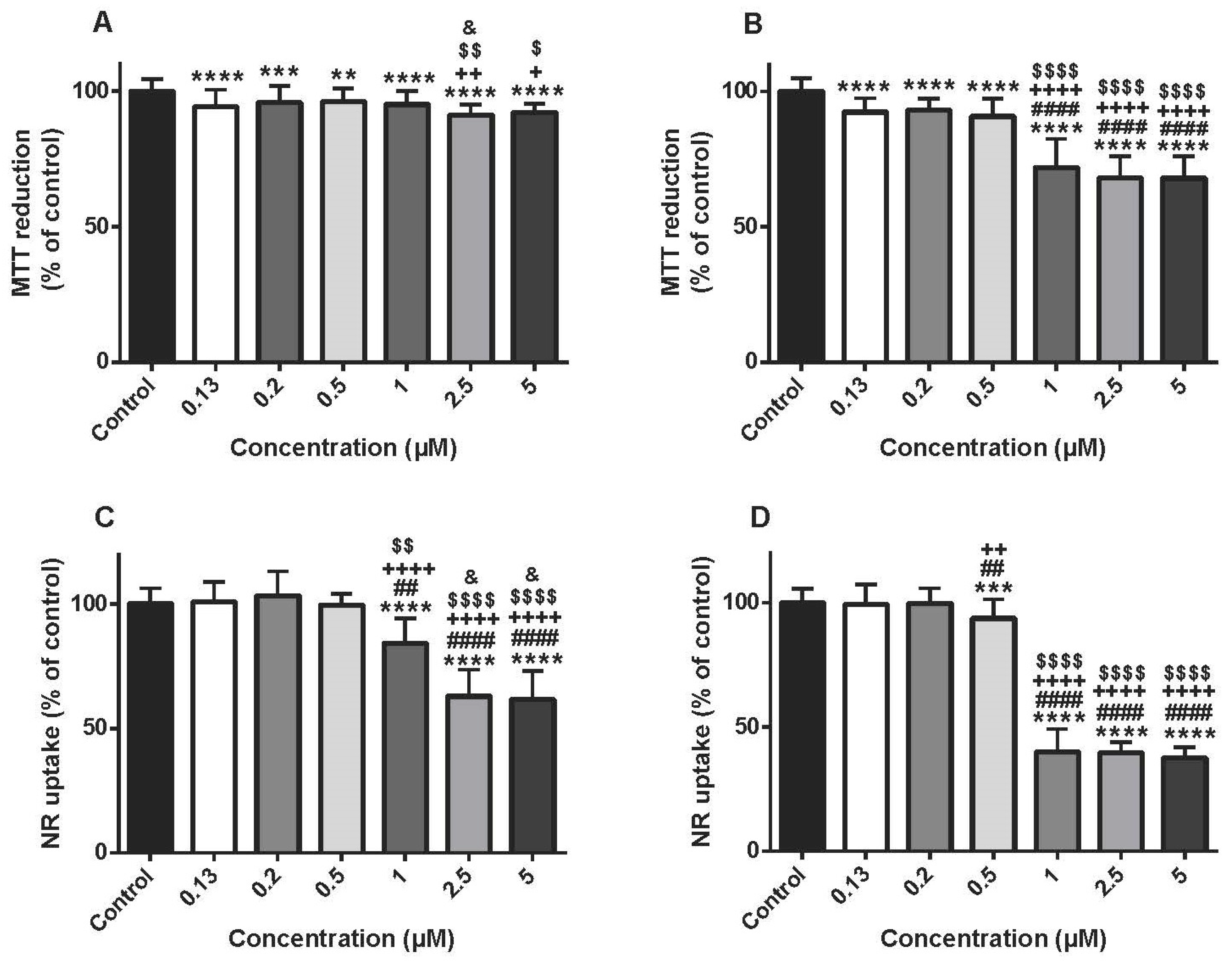
3.1. Doxorubicin Caused A Time-Dependent Mitochondrial And Lysosomal Impairment In Differentiated H9c2 Cells
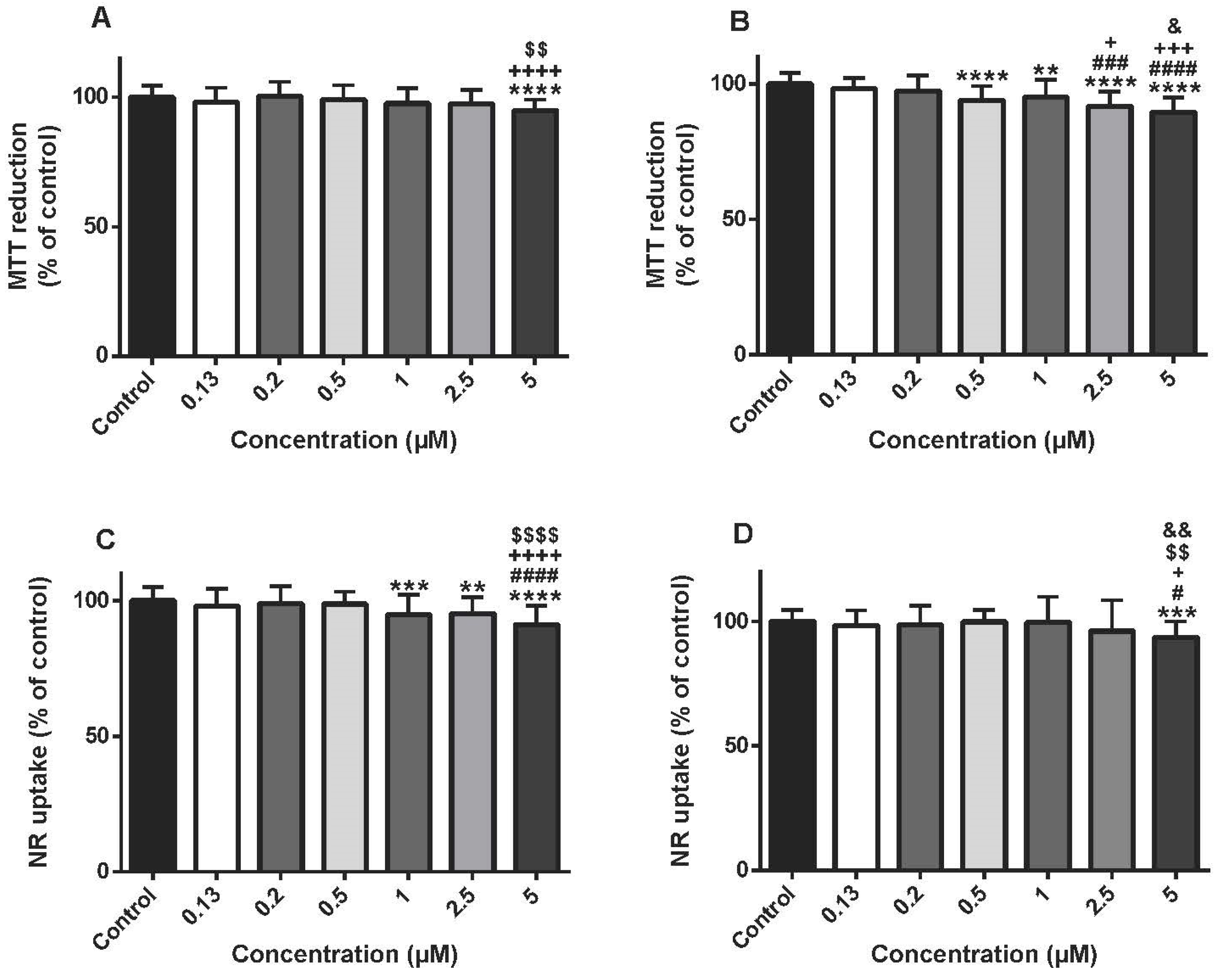
3.2. The Highest Concentrations Of 5-Fluorouracil Lead To Cytotoxicity In Differentiated H9c2 Cells
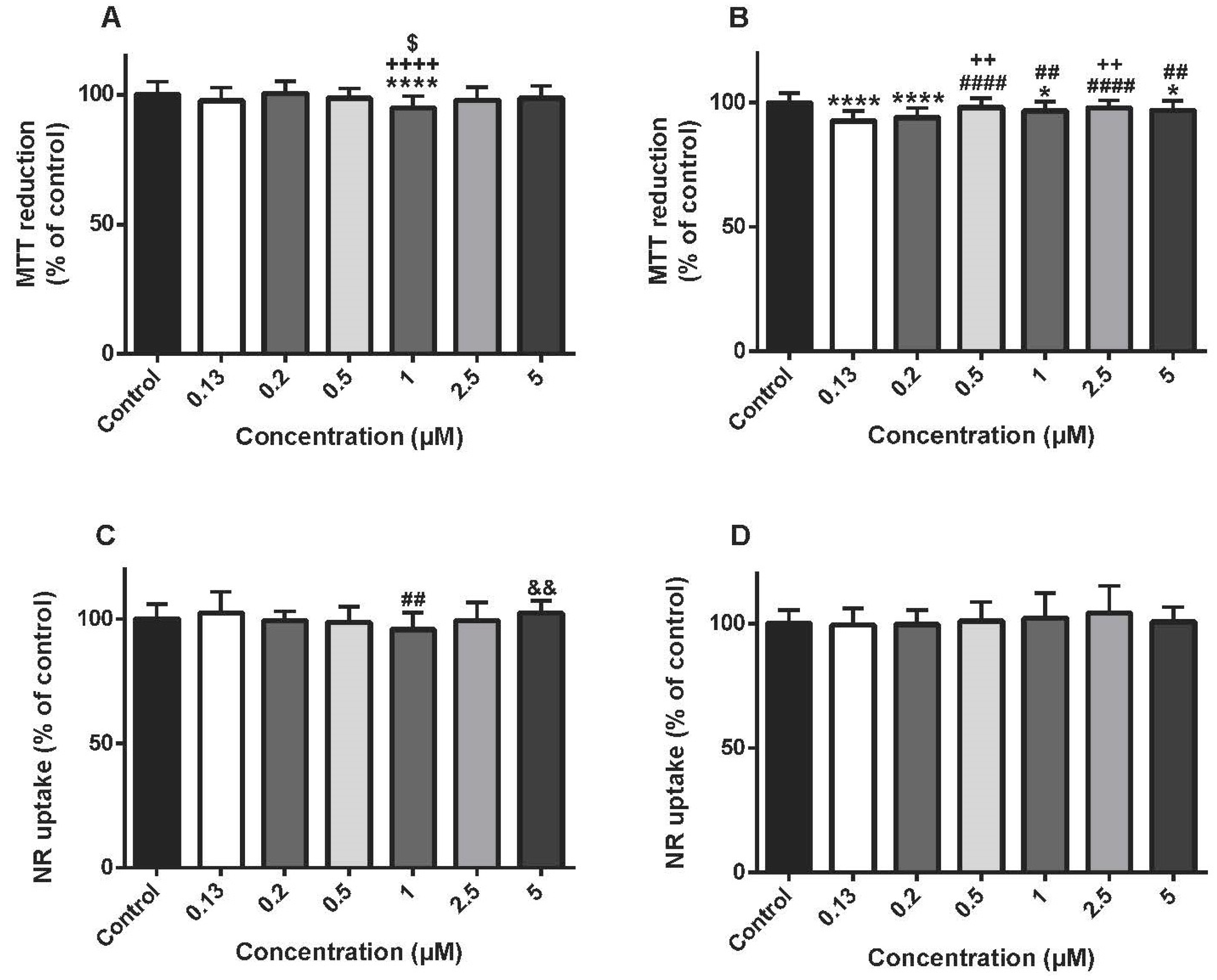
3.3. Cyclophosphamide Was Not Cytotoxic In Differentiated H9c2 Cells In The Majority Of The Concentrations Tested
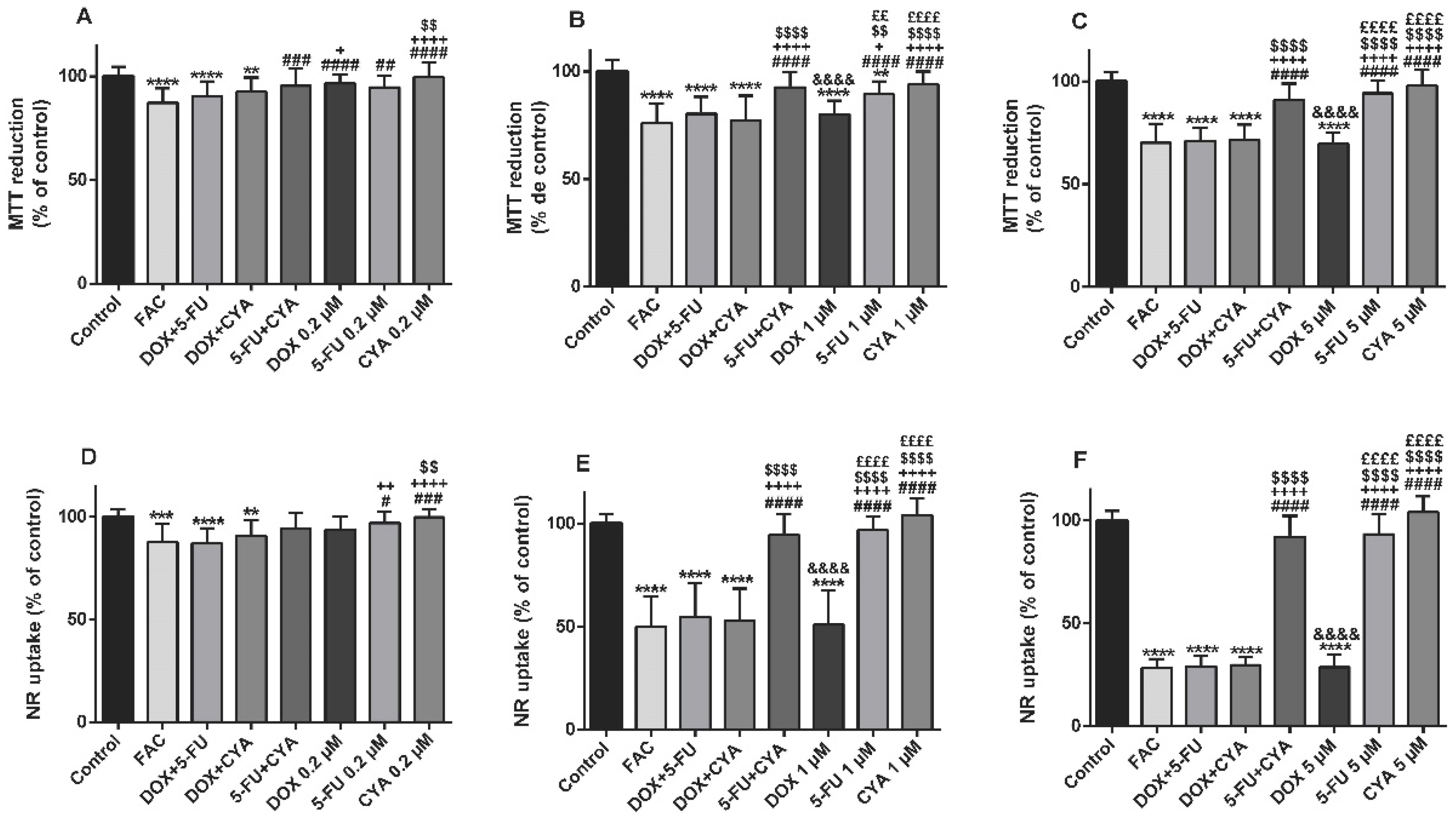
3.4. The FAC Mixture Caused Similar Cytotoxicity In The Concentration Of 1 Or 5 µM In Differentiated H9c2 Cells When Compared To Doxorubicin Per Se
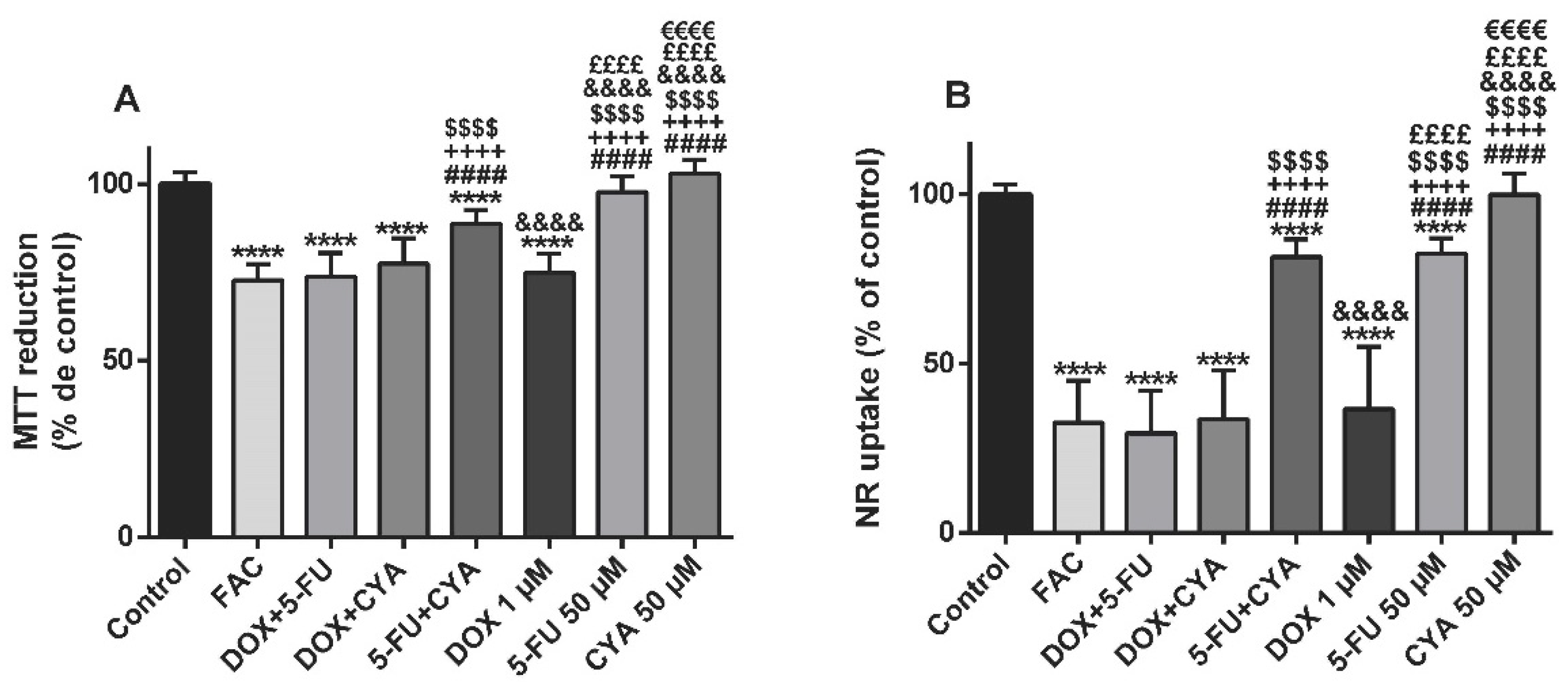
3.5. The FAC Mixture Caused Similar Cytotoxicity To Doxorubicin Alone, When Using Concentrations Based In The Plasma Levels Found In FAC-Treated Patients
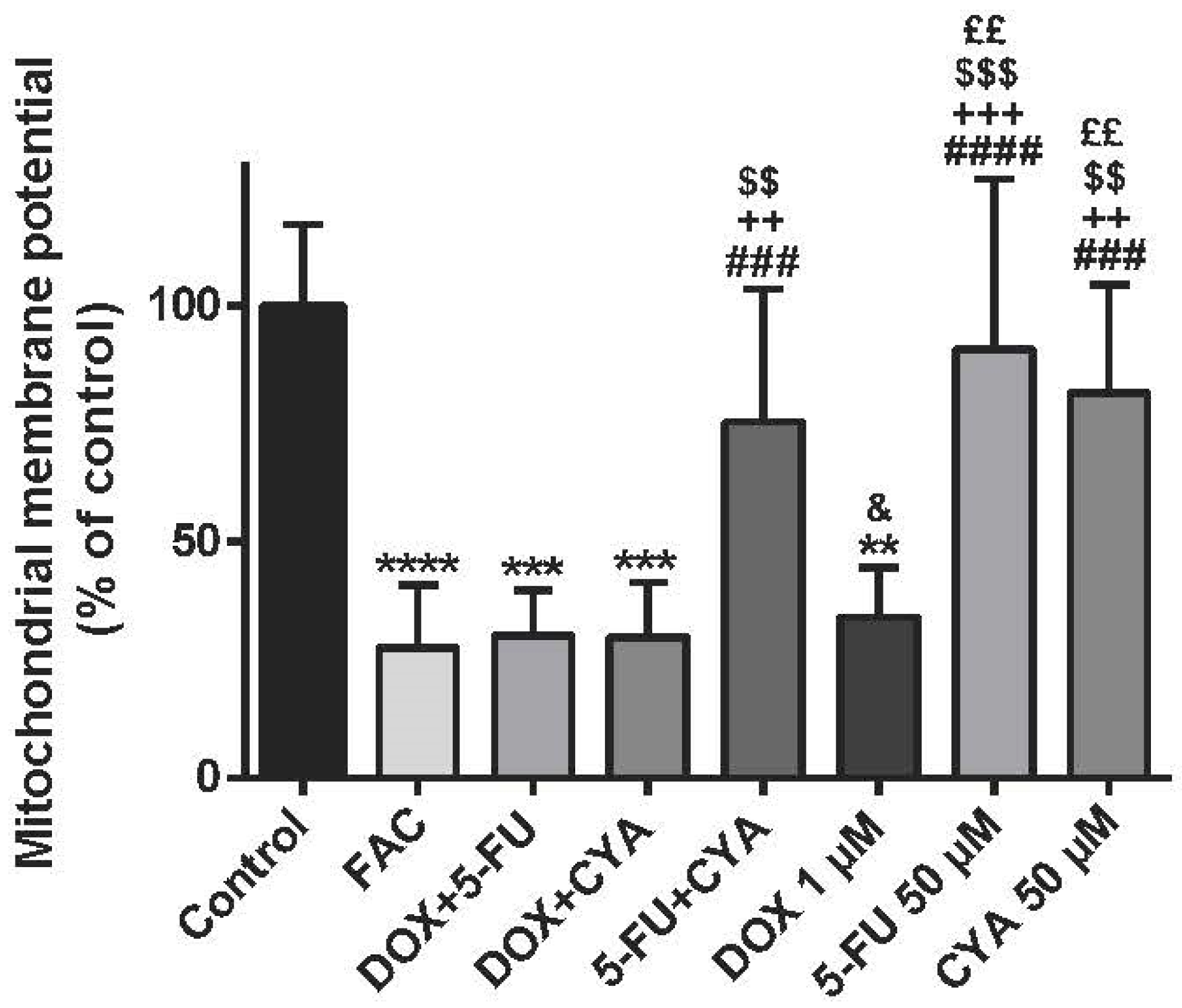
3.6. The FAC Mixture Caused Similar Mitochondrial Membrane Potential Depolarization To Doxorubicin Alone, When Using Concentrations Based In The Plasma Levels Found In FAC-Treated Patients
4. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| CYA | Cyclophosphamide |
| DMEM | Dulbecco’s modified Eagle medium |
| DOX | Doxorubicin |
| FAC | 5-Fluorouracil + Adriamycin + Cyclophosphamide |
| FBS | Fetal bovine serum |
| 5-FU | 5-Fluorouracil |
| i.v. | Intravenous |
| HBSS | Hanks’ balanced salt solution |
| MTT | 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl tetrazolium bromide |
| NR | Neutral red |
| PBS | Phosphate buffered saline |
| RA | Retinoic acid |
| SD | Standard deviation |
| SDS | Sodium dodecyl sulfate |
References
- Frei, E.I.; Eder, J.P. Combination chemotherapy. In Holland-Frei Cancer Medicine, 6th ed.; Kufe, D.W., Pollock, R.E., Bast, R.C., Weichselbaum, R.R., Eds.; BC Decker: Hamilton, ON, Canada, 2003; Available online: https://www.ncbi.nlm.nih.gov/books/NBK13955/ (accessed on 1 September 2018).
- Shih, Y.C.; Smieliauskas, F.; Geynisman, D.; Kelly, R.; Smith, T. Trends in the cost and use of targeted cancer therapies for the privately insured noneldery: 2001 to 2011. J. Clin. Oncol. 2015, 33, 2190–2199. [Google Scholar] [CrossRef] [PubMed]
- Hrynchak, I.; Sousa, E.; Pinto, M.; Costa, V.M. The importance of drug metabolites synthesis: The case-study of cardiotoxic anticancer drugs. Drug Metab. Rev. 2017, 49, 158–196. [Google Scholar] [CrossRef] [PubMed]
- Herskovic, A.; Martz, K.; al-Sarraf, M.; Leichman, L.; Brindle, J.; Vaitkevicius, V.; Cooper, J.; Byhardt, R.; Davis, L.; Emami, B. Combined chemotherapy and radiotherapy compared with radiotherapy alone in patients with cancer of the esophagus. N. Engl. J. Med. 1992, 326, 1593–1598. [Google Scholar] [CrossRef] [PubMed]
- Devita, V.T., Jr.; Serpick, A.A.; Carbone, P.P. Combination chemotherapy in the treatment of advanced Hodgkin’s disease. Ann. Intern. Med. 1970, 73, 881–895. [Google Scholar] [CrossRef] [PubMed]
- Ferlay, J.; Steliarova-Foucher, E.; Lortet-Tieulent, J.; Rosso, S.; Coebergh, J.W.; Comber, H.; Forman, D.; Bray, F. Cancer incidence and mortality patterns in Europe: Estimates for 40 countries in 2012. Eur. J. Cancer 2013, 49, 1374–1403. [Google Scholar] [CrossRef] [PubMed]
- Anampa, J.; Makower, D.; Sparano, J.A. Progress in adjuvant chemotherapy for breast cancer: An overview. BMC Med. 2015, 13, 195. [Google Scholar] [CrossRef] [PubMed]
- Bonadonna, G.; Brusamolino, E.; Valagussa, P.; Rossi, A.; Brugnatelli, L.; Brambilla, C.; De Lena, M.; Tancini, G.; Bajetta, E.; Musumeci, R.; et al. Combination chemotherapy as an adjuvant treatment in operable breast cancer. N. Engl. J. Med. 1976, 294, 405–410. [Google Scholar] [CrossRef]
- Martin, M.; Villar, A.; Sole-Calvo, A.; Gonzalez, R.; Massuti, B.; Lizon, J.; Camps, C.; Carrato, A.; Casado, A.; Candel, M.T.; et al. Doxorubicin in combination with fluorouracil and cyclophosphamide (i.v. FAC regimen, day 1, 21) versus methotrexate in combination with fluorouracil and cyclophosphamide (i.v. CMF regimen, day 1, 21) as adjuvant chemotherapy for operable breast cancer: A study by the GEICAM group. Ann. Oncol. 2003, 14, 833–842. [Google Scholar]
- Costa, V.M.; Carvalho, F.; Duarte, J.A.; Bastos Mde, L.; Remiao, F. The heart as a target for xenobiotic toxicity: The cardiac susceptibility to oxidative stress. Chem. Res. Toxicol. 2013, 26, 1285–1311. [Google Scholar] [CrossRef]
- Reis-Mendes, A.F.; Sousa, E.; de Lourdes Bastos, M.; Costa, V.M. The role of the metabolism of anticancer drugs in their induced-cardiotoxicity. Curr. Drug Metab. 2015, 17, 75–90. [Google Scholar] [CrossRef]
- Praga, C.; Beretta, G.; Vigo, P.L.; Lenaz, G.R.; Pollini, C.; Bonadonna, G.; Canetta, R.; Castellani, R.; Villa, E.; Gallagher, C.G.; et al. Adriamycin cardiotoxicity: A survey of 1273 patients. Cancer Treat. Rep. 1979, 63, 827–834. [Google Scholar] [PubMed]
- Kolaric, K.; Bradamante, V.; Cervek, J.; Cieslinska, A.; Cisarz-Filipcak, E.; Denisov, L.E.; Donat, D.; Drosik, K.; Gershanovic, M.; Hudziec, P.; et al. A phase II trial of cardioprotection with cardioxane (ICRF-187) in patients with advanced breast cancer receiving 5-fluorouracil, doxorubicin and cyclophosphamide. Oncology 1995, 52, 251–255. [Google Scholar] [CrossRef] [PubMed]
- Buzdar, A.U.; Kau, S.W.; Smith, T.L.; Hortobagyi, G.N. Ten-year results of FAC adjuvant chemotherapy trial in breast cancer. Am. J. Clin. Oncol. 1989, 12, 123–128. [Google Scholar] [CrossRef] [PubMed]
- Buyukunal, E.; Derman, U.; Serdengecti, S.; Berkarda, B. A clinical trial of mitoxantrone (novantrone) versus doxorubicin (adriamycin) in combination chemotherapy for metastatic breast cancer. Chemioterapia 1987, 6, 377–379. [Google Scholar] [PubMed]
- Bustova, I. Risk of cardiotoxicity of combination treatment radiotherapy and chemotherapy of locally advanced breast carcinoma stage III. Klin. Onkol. 2009, 22, 17–21. [Google Scholar] [PubMed]
- Mackey, J.R.; Martin, M.; Pienkowski, T.; Rolski, J.; Guastalla, J.P.; Sami, A.; Glaspy, J.; Juhos, E.; Wardley, A.; Fornander, T.; et al. Adjuvant docetaxel, doxorubicin, and cyclophosphamide in node-positive breast cancer: 10-year follow-up of the phase 3 randomised BCIRG 001 trial. Lancet Oncol. 2013, 14, 72–80. [Google Scholar] [CrossRef]
- Kimes, B.W.; Brandt, B.L. Properties of a clonal muscle cell line from rat heart. Exp. Cell Res. 1976, 98, 367–381. [Google Scholar] [CrossRef]
- Ruiz, M.; Courilleau, D.; Jullian, J.C.; Fortin, D.; Ventura-Clapier, R.; Blondeau, J.P.; Garnier, A. A cardiac-specific robotized cellular assay identified families of human ligands as inducers of PGC-1alpha expression and mitochondrial biogenesis. PLoS ONE 2012, 7, e46753. [Google Scholar] [CrossRef]
- Pereira, S.L.; Ramalho-Santos, J.; Branco, A.F.; Sardao, V.A.; Oliveira, P.J.; Carvalho, R.A. Metabolic remodeling during H9c2 myoblast differentiation: Relevance for in vitro toxicity studies. Cardiovasc. Toxicol. 2011, 11, 180–190. [Google Scholar] [CrossRef]
- Menard, C.; Pupier, S.; Mornet, D.; Kitzmann, M.; Nargeot, J.; Lory, P. Modulation of l-type calcium channel expression during retinoic acid-induced differentiation of H9c2 cardiac cells. J. Biol. Chem. 1999, 274, 29063–29070. [Google Scholar] [CrossRef]
- Reis-Mendes, A.; Gomes, A.S.; Carvalho, R.A.; Carvalho, F.; Remiao, F.; Pinto, M.; Bastos, M.L.; Sousa, E.; Costa, V.M. Naphthoquinoxaline metabolite of mitoxantrone is less cardiotoxic than the parent compound and it can be a more cardiosafe drug in anticancer therapy. Arch. Toxicol. 2017, 91, 1871–1890. [Google Scholar] [CrossRef] [PubMed]
- Soares, A.S.; Costa, V.M.; Diniz, C.; Fresco, P. Potentiation of cytotoxicity of paclitaxel in combination with CL-IB-MECA in human C32 metastatic melanoma cells: A new possible therapeutic strategy for melanoma. Biomed. Pharmacother. 2013, 67, 777–789. [Google Scholar] [CrossRef] [PubMed]
- Green, P.S.; Leeuwenburgh, C. Mitochondrial dysfunction is an early indicator of doxorubicin-induced apoptosis. Biochim. Biophys. Acta 2002, 1588, 94–101. [Google Scholar] [CrossRef]
- Zhang, Y.Y.; Meng, C.; Zhang, X.M.; Yuan, C.H.; Wen, M.D.; Chen, Z.; Dong, D.C.; Gao, Y.H.; Liu, C.; Zhang, Z. Ophiopogonin d attenuates doxorubicin-induced autophagic cell death by relieving mitochondrial damage in vitro and in vivo. J. Pharmacol. Exp. Ther. 2015, 352, 166–174. [Google Scholar] [CrossRef] [PubMed]
- Lamberti, M.; Porto, S.; Marra, M.; Zappavigna, S.; Grimaldi, A.; Feola, D.; Pesce, D.; Naviglio, S.; Spina, A.; Sannolo, N.; et al. 5-Fluorouracil induces apoptosis in rat cardiocytes through intracellular oxidative stress. J. Exp. Clin. Cancer Res. 2012, 31, 60. [Google Scholar] [CrossRef]
- Branco, A.F.; Sampaio, S.F.; Moreira, A.C.; Holy, J.; Wallace, K.B.; Baldeiras, I.; Oliveira, P.J.; Sardao, V.A. Differentiation-dependent doxorubicin toxicity on H9c2 cardiomyoblasts. Cardiovasc. Toxicol. 2012, 12, 326–340. [Google Scholar] [CrossRef] [PubMed]
- Deus, C.M.; Zehowski, C.; Nordgren, K.; Wallace, K.B.; Skildum, A.; Oliveira, P.J. Stimulating basal mitochondrial respiration decreases doxorubicin apoptotic signaling in H9c2 cardiomyoblasts. Toxicology 2015, 334, 1–11. [Google Scholar] [CrossRef]
- Sardao, V.A.; Oliveira, P.J.; Holy, J.; Oliveira, C.R.; Wallace, K.B. Morphological alterations induced by doxorubicin on H9c2 myoblasts: Nuclear, mitochondrial, and cytoskeletal targets. Cell Biol. Toxicol. 2009, 25, 227–243. [Google Scholar] [CrossRef]
- Nishikawa, T.; Miyahara, E.; Kurauchi, K.; Watanabe, E.; Ikawa, K.; Asaba, K.; Tanabe, T.; Okamoto, Y.; Kawano, Y. Mechanisms of fatal cardiotoxicity following high-dose cyclophosphamide therapy and a method for its prevention. PLoS ONE 2015, 10, e0131394. [Google Scholar] [CrossRef]
- Martin, M.; Ruiz, A.; Ruiz Borrego, M.; Barnadas, A.; Gonzalez, S.; Calvo, L.; Margeli Vila, M.; Anton, A.; Rodriguez-Lescure, A.; Segui-Palmer, M.A.; et al. Fluorouracil, doxorubicin, and cyclophosphamide (fac) versus fac followed by weekly paclitaxel as adjuvant therapy for high-risk, node-negative breast cancer: Results from the GEICAM/2003-02 study. J. Clin. Oncol. 2013, 31, 2593–2599. [Google Scholar] [CrossRef]
- Barrett-Lee, P.J.; Dixon, J.M.; Farrell, C.; Jones, A.; Leonard, R.; Murray, N.; Palmieri, C.; Plummer, C.J.; Stanley, A.; Verrill, M.W. Expert opinion on the use of anthracyclines in patients with advanced breast cancer at cardiac risk. Ann. Oncol. 2009, 20, 816–827. [Google Scholar] [CrossRef]
- Chatterjee, K.; Zhang, J.; Honbo, N.; Karliner, J.S. Doxorubicin cardiomyopathy. Cardiology 2010, 115, 155–162. [Google Scholar] [CrossRef] [PubMed]
- Dalley, D.N.; Levi, J.A.; Aroney, R.S. Combination chemotherapy with cyclophosphamide, adriamycin, and 5-fluorouracil (CAF) in advanced breast carcinoma. Med. J. Aust. 1980, 1, 216–218. [Google Scholar] [PubMed]
- Palle, J.; Frost, B.-M.; Peterson, C.; Gustafsson, G.; Hellebostad, M.; Kanerva, J.; Schmiegelow, K.; Lönnerholm, G.; Nordic Society for Pediatric Hematology and Oncology. Doxorubicin pharmacokinetics is correlated to the effect of induction therapy in children with acute myeloid leukemia. Anticancer Drugs 2006, 17, 385–392. [Google Scholar] [CrossRef] [PubMed]
- Frost, B.M.; Eksborg, S.; Björk, O.; Abrahamsson, J.; Behrendtz, M.; Castor, A.; Forestier, E.; Lönnerholm, G. Pharmacokinetics of doxorubicin in children with acute lymphoblastic leukemia: Multi-institutional collaborative study. Med. Pediatr. Oncol. 2002, 38, 329–337. [Google Scholar] [CrossRef]
- Barpe, D.R.; Rosa, D.D.; Froehlich, P.E. Pharmacokinetic evaluation of doxorubicin plasma levels in normal and overweight patients with breast cancer and simulation of dose adjustment by different indexes of body mass. Eur. J. Pharm. Sci. 2010, 41, 458–463. [Google Scholar] [CrossRef] [PubMed]
- Joerger, M.; Huitema, A.D.; Meenhorst, P.L.; Schellens, J.H.; Beijnen, J.H. Pharmacokinetics of low-dose doxorubicin and metabolites in patients with AIDS-related Kaposi sarcoma. Cancer Chemother. Pharmacol. 2005, 55, 488–496. [Google Scholar] [CrossRef]
- Voon, P.J.; Yap, H.L.; Ma, C.Y.; Lu, F.; Wong, A.L.; Sapari, N.S.; Soong, R.; Soh, T.I.; Goh, B.C.; Lee, H.S.; et al. Correlation of aldo-ketoreductase (akr) 1c3 genetic variant with doxorubicin pharmacodynamics in asian breast cancer patients. Br. J. Clin. Pharmacol. 2013, 75, 1497–1505. [Google Scholar] [CrossRef]
- Büchel, B.; Rhyn, P.; Schürch, S.; Bühr, C.; Amstutz, U.; Largiadèr, C.R. LC-MS/MS method for simultaneous analysis of uracil, 5,6-dihydrouracil, 5-fluorouracil and 5-fluoro-5,6-dihydrouracil in human plasma for therapeutic drug monitoring and toxicity prediction in cancer patients. Biomed. Chromatogr. 2013, 27, 7–16. [Google Scholar] [CrossRef]
- Veal, G.J.; Cole, M.; Chinnaswamy, G.; Sludden, J.; Jamieson, D.; Errington, J.; Malik, G.; Hill, C.R.; Chamberlain, T.; Boddy, A.V. Cyclophosphamide pharmacokinetics and pharmacogenetics in children with b-cell non-hodgkin’s lymphoma. Eur. J. Cancer 2016, 55, 56–64. [Google Scholar] [CrossRef]
- Joerger, M.; Huitema, A.D.; Richel, D.J.; Dittrich, C.; Pavlidis, N.; Briasoulis, E.; Vermorken, J.B.; Strocchi, E.; Martoni, A.; Sorio, R.; et al. Population pharmacokinetics and pharmacodynamics of doxorubicin and cyclophosphamide in breast cancer patients: A study by the EORTC-PAMM-NDDG. Clin. Pharmacokinet. 2007, 46, 1051–1068. [Google Scholar] [CrossRef] [PubMed]
- Damiani, R.M.; Moura, D.J.; Viau, C.M.; Caceres, R.A.; Henriques, J.A.; Saffi, J. Pathways of cardiac toxicity: Comparison between chemotherapeutic drugs doxorubicin and mitoxantrone. Arch. Toxicol. 2016, 90, 2063–2076. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, R.A.; Sousa, R.P.; Cadete, V.J.; Lopaschuk, G.D.; Palmeira, C.M.; Bjork, J.A.; Wallace, K.B. Metabolic remodeling associated with subchronic doxorubicin cardiomyopathy. Toxicology 2010, 270, 92–98. [Google Scholar] [CrossRef] [PubMed]
- Palmeira, C.M.; Serrano, J.; Kuehl, D.W.; Wallace, K.B. Preferential oxidation of cardiac mitochondrial DNA following acute intoxication with doxorubicin. Biochim. Biophys. Acta 1997, 1321, 101–106. [Google Scholar] [CrossRef]
- Kluza, J.; Marchetti, P.; Gallego, M.A.; Lancel, S.; Fournier, C.; Loyens, A.; Beauvillain, J.C.; Bailly, C. Mitochondrial proliferation during apoptosis induced by anticancer agents: Effects of doxorubicin and mitoxantrone on cancer and cardiac cells. Oncogene 2004, 23, 7018–7030. [Google Scholar] [CrossRef] [PubMed]
- Sardao, V.A.; Oliveira, P.J.; Holy, J.; Oliveira, C.R.; Wallace, K.B. Doxorubicin-induced mitochondrial dysfunction is secondary to nuclear p53 activation in H9c2 cardiomyoblasts. Cancer Chemother. Pharmacol. 2009, 64, 811–827. [Google Scholar] [CrossRef] [PubMed]
- Azim, H.A., Jr.; de Azambuja, E.; Colozza, M.; Bines, J.; Piccart, M.J. Long-term toxic effects of adjuvant chemotherapy in breast cancer. Ann. Oncol. 2011, 22, 1939–1947. [Google Scholar] [CrossRef]
- Youn, H.J.; Kim, H.S.; Jeon, M.H.; Lee, J.H.; Seo, Y.J.; Lee, Y.J.; Lee, J.H. Induction of caspase-independent apoptosis in H9c2 cardiomyocytes by adriamycin treatment. Mol. Cell. Biochem. 2005, 270, 13–19. [Google Scholar] [CrossRef]
- Fernandes, B.J.; Silva Cde, M.; Andrade, J.M.; Matthes Ado, C.; Coelho, E.B.; Lanchote, V.L. Pharmacokinetics of cyclophosphamide enantiomers in patients with breast cancer. Cancer Chemother. Pharmacol. 2011, 68, 897–904. [Google Scholar] [CrossRef]
- Yang, L.; Zhang, X.C.; Yu, S.F.; Zhu, H.Q.; Hu, A.P.; Chen, J.; Shen, P. Pharmacokinetics and safety of cyclophosphamide and docetaxel in a hemodialysis patient with early stage breast cancer: A case report. BMC Cancer 2015, 15, 917. [Google Scholar] [CrossRef]
- Gamelin, E.C.; Danquechin-Dorval, E.M.; Dumesnil, Y.F.; Maillart, P.J.; Goudier, M.J.; Burtin, P.C.; Delva, R.G.; Lortholary, A.H.; Gesta, P.H.; Larra, F.G. Relationship between 5-fluorouracil (5-FU) dose intensity and therapeutic response in patients with advanced colorectal cancer receiving infusional therapy containing 5-FU. Cancer 1996, 77, 441–451. [Google Scholar] [CrossRef]
- Grem, J.L.; Quinn, M.; Ismail, A.S.; Takimoto, C.H.; Lush, R.; Liewehr, D.J.; Steinberg, S.M.; Balis, F.M.; Chen, A.P.; Monahan, B.P.; et al. Pharmacokinetics and pharmacodynamic effects of 5-fluorouracil given as a one-hour intravenous infusion. Cancer Chemother. Pharmacol. 2001, 47, 117–125. [Google Scholar] [CrossRef] [PubMed]
- Jamieson, D.; Lee, J.; Cresti, N.; Jackson, R.; Griffin, M.; Sludden, J.; Verrill, M.; Boddy, A.V. Pharmacogenetics of adjuvant breast cancer treatment with cyclophosphamide, epirubicin and 5-fluorouracil. Cancer Chemother. Pharmacol. 2014, 74, 667–674. [Google Scholar] [CrossRef] [PubMed]
- Murayama, Y.; Nagashima, M. Systemic chemotherapy of mammary carcinoma: Plasma and tissue concentrations of 5-fluorouracil and adriamycin, and result of CAF and CMF therapy of breast cancer. Gan To Kagaku Ryoho 1984, 11, 415–419. [Google Scholar] [PubMed]
- Afsar, N.A.; Ufer, M.; Haenisch, S.; Remmler, C.; Mateen, A.; Usman, A.; Ahmed, K.Z.; Ahmad, H.R.; Cascorbi, I. Relationship of drug metabolizing enzyme genotype to plasma levels as well as myelotoxicity of cyclophosphamide in breast cancer patients. Eur. J. Clin. Pharmacol. 2012, 68, 389–395. [Google Scholar] [CrossRef] [PubMed]

| Drug | Patients and Dose | Plasma Concentrations | Reference |
|---|---|---|---|
| Cyclophosphamide (CYA) | 644 plasma samples collected over a 5-year period, from 49 B-cell non-Hodgkin’s lymphoma patients 18 years receiving CYA. CYA (250 mg/m2) was administered as a 15-min infusion twice daily on days 2, 3 and 4 of treatment (six doses in total) (1.5 g/m2 total dose). | After dose 1: 37.54–438.94 μM After dose 5: 32.67–205.68 μM | [41] |
| 15 patients with breast cancer with previously removal of the tumor and then treated with 4 to 6 doses of injectable racemic CYA (900 or 1000 mg/m2 administered at intervals of 21 days, i.v.). | 75.5 μM | [50] | |
| Patient with early stage breast cancer received CYA 600 mg/m2 i.v., day 1 and docetaxel 75 mg/m2 i.v., day 1; treatment repeated every three weeks, for 4 cycles. | 187.6 μM | [51] | |
| Doxorubicin (DOX) | 107 children >1 year of age, with newly diagnosed acute lymphoblastic leukemia received a 24-h infusion of DOX 40 mg/m2. | 0.04–0.61 μM | [36] |
| 41 children treated for newly diagnosed acute myeloid leukemia. DOX, 75 mg/m2 body surface area, was administered by constant i.v. infusion over 8 h. | 0.32–0.60 μM | [35] | |
| 10 female patients [normal (n = 3) and overweight (n = 7)] with breast cancer received adjuvant therapy with CYA and DOX. DOX, 60 mg/m2 body surface area, was administered by i.v. infusion for 40 min. | Normal: 0.07–1.16 μM Overweight: 0.08–0.68 μM | [37] | |
| 151 Asian breast cancer patients treated with DOX-containing chemotherapy. DOX was administered at 75 mg/m2 as a slow bolus and docetaxel at 75 mg/m2 over 1 h. | 0.68–1.05 μM | [39] | |
| 5-Fluorouracil (5-FU) | 10 colorectal cancer patients were treated with 5-FU bolus doses ranging from 600 to 800 mg followed by a 48-h continuous infusion of 3000 to 4800 mg of FU. Blood samples were collected in the first cycle of treatment, 2 h after the start of 5-FU infusion. | 1.4–6.7 μM | [40] |
| 40 patients with advanced colorectal cancer were treated with 5-FU plus leucovorin (LV). 5-FU was administered weekly by 8-h continuous infusion. The initial dose of 1000 mg/m2 was individually increased every 3 weeks by 250 mg/m2 steps, potentiated by 400 mg/m2 LV. | 15.4– 23.1 μM | [52] | |
| 22 adults with advanced gastrointestinal tract cancers and no prior systemic chemotherapy for advanced disease received interferon alpha-2a (5 MU/m2 subcutaneous administration, days 1–7), leucovorin (500 mg/m2 i.v. over 30 min, days 2–6) and 5-FU (370 mg/m2 i.v. over 1 h, days 2–6). | 21.53–52.28 µM | [53] | |
| FAC | 51 patients breast cancer treated with CYA (n = 51) and epirubicin (n = 35), with or without 5-FU. The women received between 3 and 6 cycles of either 5-FU, epirubicin (EPI) and CYA (FEC) (n = 32), EPI and CYA (EC) (n = 3), DOX and CYA (AC) (n = 13) or 5-FU, DOX and CYA (FAC) (n = 3) adjuvant chemotherapy. Dose of 5-FU and CYA were 500–600 mg/m2. Each of the drugs was administered as a short infusion (3–20 min). | FU: 22.3–203 μM CYA: 71.4–172 μM | [54] |
| 28 patients with recurrent breast cancers were treated with a combination chemotherapy consisting of 5-FU (200 mg/m2/day P 0 days 1–28), DOX (27 mg/m2 i.v. at days 1 and 8), and CYA (67 mg/m2/day P 0 days 1–28). On the other hand, 15 patients with recurrent breast cancer were treated with a combination chemotherapy consisting of 5-FU (200 mg/m2/day P 0 days 1–28), CYA (67 mg/m2/day P 0 days 1–28) and DOX (27 mg/m2 i.v. at days 1 and 8). | DOX: 0.24–1.36 μM | [55] | |
| 68 breast cancer patients received six cycles of FAC chemotherapy containing 5-FU 500 mg/m2, doxorubicin 50 mg/m2, and CYA 500 mg/m2 administered on the same day, every 21 days. DOX and CYA were given as “infusion-1” over 30 min followed by 5-FU as “infusion-2” over 2 h. | CYA: 9–20.2 μM | [56] |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pereira-Oliveira, M.; Reis-Mendes, A.; Carvalho, F.; Remião, F.; Bastos, M.d.L.; Costa, V.M. Doxorubicin Is Key for the Cardiotoxicity of FAC (5-Fluorouracil + Adriamycin + Cyclophosphamide) Combination in Differentiated H9c2 Cells. Biomolecules 2019, 9, 21. https://doi.org/10.3390/biom9010021
Pereira-Oliveira M, Reis-Mendes A, Carvalho F, Remião F, Bastos MdL, Costa VM. Doxorubicin Is Key for the Cardiotoxicity of FAC (5-Fluorouracil + Adriamycin + Cyclophosphamide) Combination in Differentiated H9c2 Cells. Biomolecules. 2019; 9(1):21. https://doi.org/10.3390/biom9010021
Chicago/Turabian StylePereira-Oliveira, Maria, Ana Reis-Mendes, Félix Carvalho, Fernando Remião, Maria de Lourdes Bastos, and Vera Marisa Costa. 2019. "Doxorubicin Is Key for the Cardiotoxicity of FAC (5-Fluorouracil + Adriamycin + Cyclophosphamide) Combination in Differentiated H9c2 Cells" Biomolecules 9, no. 1: 21. https://doi.org/10.3390/biom9010021
APA StylePereira-Oliveira, M., Reis-Mendes, A., Carvalho, F., Remião, F., Bastos, M. d. L., & Costa, V. M. (2019). Doxorubicin Is Key for the Cardiotoxicity of FAC (5-Fluorouracil + Adriamycin + Cyclophosphamide) Combination in Differentiated H9c2 Cells. Biomolecules, 9(1), 21. https://doi.org/10.3390/biom9010021








